Abstract
Introduction
Throughout the years, a decreasing trend in mortality rate has been demonstrated in patients suffering severe trauma. This increases the relevance of documentation of other outcomes for this population, including patient-reported outcome measures (PROMs), such as health-related quality of life (HRQoL). The aim of this review was to summarize the results of the studies that have been conducted regarding HRQoL in severely injured patients (as defined by the articles’ authors). Also, we present the instruments that are used most frequently to assess HRQoL in patients suffering severe trauma.
Methods
A literature search was conducted in the Cochrane Library, EMBASE, PubMed, and Web of Science for articles published from inception until the 1st of January 2022. Reference lists of included articles were reviewed as well. Studies were considered eligible when a population of patients with major, multiple or severe injury and/or polytrauma was included, well-defined by means of an ISS-threshold, and the outcome of interest was described in terms of (HR)QoL. A narrative design was chosen for this review.
Results
The search strategy identified 1583 articles, which were reduced to 113 after application of the eligibility criteria. In total, nineteen instruments were used to assess HRQoL. The SF-36 was used most frequently, followed by the EQ-5D and SF-12. HRQoL in patients with severe trauma was often compared to normative population norms or pre-injury status, and was found to be reduced in both cases, regardless of the tool used to assess this outcome. Some studies demonstrated higher scoring of the patients over time, suggesting improved HRQoL after considerable time after severe trauma.
Conclusion
HRQoL in severely injured patients is overall reduced, regardless of the instrument used to assess it. The instruments that were used most frequently to assess HRQoL were the SF-36 and EQ-5D. Future research is needed to shed light on the consequences of the reduced HRQoL in this population. We recommend routine assessment and documentation of HRQoL in severely injured patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, traumatic injury is one of the three leading causes of death in patients between the ages of 5 to 44 years [1]. For patients categorized as having severe or profound injuries defined as an Injury Severity Score (ISS) that is equal or above 16, a higher risk of mortality is predicted [2]. The number of patients that do not survive severe trauma, however, is decreasing, due to improvements in surgical procedures, centralization of trauma care and reduction in number of trauma incidents [3,4,5,6,7,8,9,10,11,12]. This increases the importance of documentation of outcomes other than mortality of severely injured patients on the short- and long-term, since not much is known about these patients’ way to recovery and the quantification of the impact of the trauma on the whole population (e.g., by means of Disability Adjusted Life Years). Furthermore, since patients have an increased chance of survival, they will have to face the consequences of their trauma for a longer period which might influence their health-related quality of life (HRQoL). In his dissertation, Lansink et al. [13] suggested that monitoring of quality of life should be the focus of research from now on. Based on the relatively low numbers of preventable deaths, further reduction in mortality is after all expected to be small. Hence, what is now increasingly of more relevance, is life after severe trauma.
The World Health Organization (WHO) defines quality of life (QoL) as the individuals’ perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns [14]. Although often—incorrectly—interchangeably used in literature, health-related QoL (HRQoL) forms a separate construct, which is defined by the Centres for Disease Control and Prevention (CDC) as an individual’s’ perception on physical and mental health and its impact on QoL [15]. Both definitions clarify that (HR)QoL is an individual, subjective perception, which can only be assessed by numerous questionnaires that are either generic or disease-specific; the former facilitate the possibility to compare different diseases with each other, whereas the latter identify the specific effects of, for example, traumatic injuries and allow comparisons with healthy individuals. HRQoL-measurement is valuable, as it enables caregivers to offer tailor-made aftercare to patients. Not only does this benefit the individual patient, but also the policy makers and the general society, since trauma injuries cause substantial medical and societal costs [16, 17].
The terms polytrauma, major trauma, and severe injury, which are commonly used interchangeably in literature, refer to the situation in which patients experience multiple injuries, often leading to impairments in physiologic state [18,19,20]. Although the cut-off value of ≥ 16 is used most often internationally for identifying polytrauma due to its ability of predicting the risk of mortality [26], multiple definitions in terms of ISS values are reported in literature for terms as ‘severe trauma’ or ‘major injury’ [21,22,23,24,25], leaving no consensus regarding ISS thresholds for these populations. Regardless, not only a high risk of mortality (> 10%) [26] is to be expected for those patients, but studies also demonstrate higher morbidity rates in comparison to patients suffering minor trauma [27, 28], leading to the hypothesis that HRQoL is probably significantly impacted.
To our knowledge, there have been only a few reviews of the literature published to summarize evidence regarding HRQoL after severe traumatic injuries [29, 30]. Since patients with an ISS > 15 were excluded in one review [29], studies on injury-specific HRQoL in the other [30], and emphasis was placed on instruments and methods used to measure HRQoL in both [29, 30], we aim in this review to summarize the study results discussing the HRQoL of patients with severe trauma, as defined by an article’s given ISS-threshold. Furthermore, available patients reported outcome measures (PROMs) will be presented.
Methods
Search strategy
An exhaustive search was conducted in the Cochrane Library, EMBASE, PubMed, and Web of Science covering the population of patients with severe trauma and the outcome of interest (i.e., HRQoL) defined in the introduction. All articles published from inception to the 1st of January 2022 were included and imported in Rayyan QCRI [31]. In addition to database-searched articles, references of (Cochrane) reviews and included articles and excluded reviews were checked and screened for title and abstract by two reviewers.
The used search strategies that were applied were adjusted to the syntax appropriate for that database and are reported as full texts in Electronic supplementary material (ESM) Appendix A. There were no restrictions with regard to the year of publication.
Eligibility criteria
Studies that met all of the following criteria were included:
-
I.
Studies have the objective to describe QoL or HRQoL (since both terms are used interchangeably in literature) of patients that, according to their own given definition that is well-described by means of an ISS-threshold value, have suffered major trauma, severe injury or polytrauma (e.g., defined as a population ISS ≥ 16—other thresholds as adopted by authors defining major or severe trauma, however, were accepted as well, since we aimed to cover literature’s HRQoL data on severe trauma patients, taking into account the different ISS thresholds that exist for severely injured patients) or have the objective to describe instruments used to assess QoL or HRQoL in patients with severe trauma;
-
II.
The publication is an original article;
-
III.
The article is published in English, German, French, Arabic or Dutch (selection of languages is based on the authors’ language skills);
-
IV.
The full text of the article is available.
Studies on general injury populations and injury-specific studies were both included. Multiple independent populations included in one study were considered separately.
The following articles were excluded:
-
I.
Studies that included exclusively patients described as having suffered mild or minor trauma;
-
II.
Studies using exclusively trauma severity indices scores other than ISS;
-
III.
Studies not defining the patient reported outcome (PRO) explicitly in terms of (HR)QoL (but in less standardized terms such as disability, (dis)function or (dis)satisfaction);
-
IV.
Books, commentaries, letters, reports, (conference) abstracts, posters, presentations, discussion papers, (systematic) reviews, editorials.
Data extraction
Data-extraction from the included studies was done in duplicate to avoid errors and missing relevant data.
From each eligible study, the following data-elements were extracted into a Microsoft Excel sheet:
-
Study characteristics: first author’s last name, year of publication, geographical location, study design, number of participants;
-
Population characteristics: age at baseline, gender, median/mean ISS, general population description (e.g., mechanism of injury), duration of ICU and hospital stay;
-
PRO characteristics: reported PRO, instrument used to assess PRO, elements observed with instrument, follow-up duration/time point of outcome assessment;
-
Outcome: results summarization, author conclusion.
Synthesis of results
A narrative design was chosen for this review since a meta-analysis could not be produced due to the heterogeneity of the included studies. HRQoL will be discussed per instrument used to assess it in a separate manner.
Results
Literature search
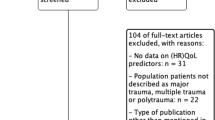
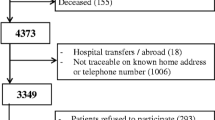
The search strategy identified 1550 articles of potentially relevant articles, while reference checking yielded an additional 33 articles (in total n = 1583 articles). Removal of duplicates and screening of titles and abstracts resulted in a selection of 239 articles that appeared to be relevant to the review subject; after applying the eligibility criteria on the full text papers, 113 articles were included for the final analysis. The main reasons for exclusion of publications were lack of data on this review’s desired outcomes, and inclusion of populations that were not necessarily identified as having suffered major trauma (e.g., populations with general trauma). The study flow diagram is shown in Fig. 1.
General study characteristics
In total, 113 studies were included, all published between January 1994 and January 2022. The general characteristics of the studies are presented in Table 1 (ESM Appendix B). In all studies, the outcomes were defined in terms of HRQoL or QoL. The majority of studies were conducted prospectively (n = 65) [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72, 158, 161,162,163, 166,167,168,169, 171, 173, 176, 177, 181,182,183, 185, 186, 189,190,191,192,193, 196, 197] and in Germany (n = 26) [33, 36, 39, 41, 45, 46, 49, 51, 53, 57, 58, 67, 69, 70, 73, 75,76,77,78,79,80,81,82,83, 189, 191]. Investigated populations were identified as having suffered major trauma, severe and/or multiple injury or polytrauma, as defined by the eligibility criteria; studies’ average ISS ranged from 9 to 57.
Sample sizes ranged between 8 [84] and 1482 [188], with the majority of patients being male (> 50% in 98 articles [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52, 54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83, 86,87,88,89,90,91,92,93,94,95,96,97, 158, 159, 161, 163, 165,166,167,168, 170,171,172,173,174,175,176,177,178,179,180,181,182,183, 185,186,187,188,189,190,191,192,193,194, 197,198,199]). Age of the participants in the included studies ranged between 2 [192] and 92 [44, 48] years. Five studies [85, 163, 167, 192, 199] assessed HRQoL in children and/or adolescents (≤ 18 years) only.
Methods to measure QoL
Nineteen instruments were used to assess HRQoL (an overview of characteristics and descriptions of each instrument is presented in Table 2 (ESM Appendix C)). Of those instruments, the 36-item Short-Form (SF-36) was used most frequently (n = 40) [37, 39, 41,42,43,44, 47, 50, 52, 61,62,63,64,65, 68, 71,72,73, 76, 77, 81, 90, 95, 97,98,99, 160, 161, 165, 168,169,170, 173, 176, 181,182,183, 186, 195, 196] followed by the EuroQoL-5 Dimension Questionnaire (EQ-5D, n = 39) [38, 40, 44, 47, 53, 55,56,57, 60, 64, 65, 68, 76, 77, 84, 88, 91, 92, 94, 96, 100, 167, 171, 176,177,178, 180,181,182, 185, 186, 190,191,192,193,194,195, 198, 199] and 12-itemed Short-Form (SF-12) (n = 17) [45, 46, 66, 67, 69, 70, 79, 80, 82, 83, 89, 172, 174, 175, 177, 187, 188]. A substantial number of studies (n = 32) used multiple tools to measure the HRQoL [38, 44,45,46,47, 64,65,66,67,68,69,70, 76, 77, 79, 80, 82, 83, 96, 161, 167, 169, 176,177,178, 181, 182, 186, 192, 195, 196, 199]. The Polytrauma Outcome (POLO) chart, which combines the Trauma Outcome Profile (TOP), Glasgow Outcome Scale (GOS), EQ-5D and SF-36, has been validated recently by multiple studies, and was used in 6 articles [49, 58, 74, 75, 78, 189]. The remaining studies used the TOP (n = 11) [47, 48, 51, 65, 68, 76, 77, 93, 179, 181, 182], Hannover Score for Polytrauma Outcome (HASPOC, n = 10) [45, 46, 66, 67, 69, 70, 79, 80, 82, 83], a subjective scale (n = 5) [33, 36, 38, 59, 61], the Sickness Impact Profile (SIP, n = 5) [38, 54, 87, 159, 161], the Quality-of-Wellbeing scale (QWB scale, n = 4) [34, 158, 162, 163], the Paediatric Quality of Life Inventory (PedsQL) (n = 3) [167, 192, 199], the Nottingham Health Profile (NHP, n = 3) [35, 47, 196], the Life satisfaction checklist (LiSat9 and LiSat11, n = 2) [86, 169], The Quality of Life after Brain Injury (QOLIBRI, n = 2) [65, 181], the Trauma-specific QoL questionnaire (T-QoL) (n = 2) [184, 197], the Classification of disability by the International Classification of Impairment, Disabilities and Handicaps (n = 1) [164], the Hadorn’s QoL and health questionnaire (n = 1) [101], the Quality-of-Life-questionnaire (n = 1) [32], the St. George’s Respiratory questionnaire (n = 1) [166], and the RAND-36 (n = 1) [85]. The latter tool includes the same item-set as the SF-36 but differs in scoring; it will therefore be discussed separately.
Overall QoL
The results are presented per instrument measuring HRQoL and in order of frequency of usage. In Table 1 (ESM Appendix B) the results are summarized and presented mostly per HRQoL domain or subscale.
SF-36
HRQoL as measured by the SF-36 was overall reduced [37, 42, 47, 50, 61,62,63,64, 68, 71, 76, 77, 81, 95, 97, 98, 160, 168,169,170, 173, 176, 183, 186, 196] when compared to pre-injury status or population norms. In some studies SF-36 scores of certain domains (e.g., physical and social functioning) improved significantly over time, although remaining significantly below population norms [37, 39, 42, 50, 52, 61, 63, 71, 161, 183, 186] up to one to fifteen years after the traumatic event [42, 47, 50, 52, 61,62,63,64, 68, 71, 77, 81, 97, 161, 183, 186].
Although HRQoL was reduced generally in all polytrauma patients, traumatic brain injury (TBI) impacted HRQoL significantly more when present, in comparison to patients with an ISS ≥ 16 without TBI [39, 47, 61, 62, 65]. Again, time had a beneficial effect on SF-scores of most domains, as shown by an increasing trend, indicating an overall improvement of HRQoL over time (i.e., 12 months [39]).
Severe trauma resulted in early retirement up to 20% of the population [170], and reduced ability to resume employment up to 30% [176, 182, 186, 196]. Moreover, scores in certain SF-36 domains resulted in approximately half of patients losing their ability to return to work after 5 years [71]. Although both patients returning and patients not returning to work report lower HRQoL scores in some of the SF-36 domains compared to the general population, patients not returning to work tend to show lower scores for all subscales. A higher percentage of TBI patients showed a decrease in their capacity to work when compared to non-TBI patients [47].
Furthermore, lower HRQoL in patients with severe trauma results in reported fatigue, reduced activity, reduced motivation, less frequent participation in and satisfaction with social activities, and the feeling of being more restricted in daily activities [42, 97]. The number of patients with depression and/or anxiety after polytrauma decreased after at least 6 months in patients receiving cognitive behavioural therapy shortly after the event leading to injury [41].
No comparisons were made in some studies [43, 73, 165, 181, 182, 195], hence making it impossible to compare HRQoL between populations, pre-injury status and between time points.
EQ-5D
HRQoL of patients suffering severe trauma was below population norms [40, 53, 57, 64, 76, 88, 97, 167, 171, 176, 178, 185, 191, 194, 198] and lower than pre-injury HRQoL [44, 47, 55, 56, 185, 186, 192,193,194] in most studies. Furthermore, patients with an ISS ≥ 16 reported a lower HRQoL than did patients with an ISS < 16 [53, 55]. The majority of patients reports having problems regarding HRQoL up to several years after the traumatic incident [40, 44, 47, 53, 55,56,57, 59, 60, 64, 76, 77, 84, 91, 96, 177, 180,181,182, 190, 195, 199]. Some studies report an improvement in HRQoL-scores over time [53, 57, 176, 177, 185, 192, 193]. Children and teenagers with major trauma reported both similar [167] and reduced [199] HRQoL compared to healthy peers in different studies.
Patients with a flail chest and/or rib fractures show comparable HRQoL scores to control groups with healthy adults [92]. Patients with Lisfranc and/or Chopart injuries report significantly lower HRQoL compared to the general (non-trauma) population, but similar HRQoL to general trauma patients [178].
Patients with a femoral fracture with a pelvic or acetabular fracture (i.e., floating hip) reported reduced HRQoL, although no significant difference was found when compared to patients with isolated acetabular or femoral fractures. However, depending on the location of the fracture in floating hip patients, significant differences in HRQoL can be detected within a minimum of 7 years post-trauma [100].
SF-12 and HASPOC
Ten studies [45, 46, 66, 67, 69, 70, 79, 80, 82, 83] used both the SF-12 and HASPOC as a measurement of QoL.
Polytrauma patients presented with reduced HRQoL when compared to normative values [46]. No difference in HRQoL between TBI and non-TBI patients was found [46, 80]; spinal injuries, however, had deleterious effects on HRQoL, especially in paraplegic patients [69]. Also, mentally impaired patients presented with worse HRQoL after severe trauma in comparison to mentally healthy patients [79].
Although no difference in HRQoL between athletes and non-athletes could be demonstrated, the impairments were serious and of long-term influence [66].
Patients with and without upper extremity trauma reported comparable HRQoL [67, 80], but involvement of the brachial plexus in the polytrauma resulted in significantly lower scores [67]. Worse HRQoL-scores were present in patients with lower extremity injury [69], especially when present below the knee joint [83].
In studies that used SF-12 exclusively, comparable HRQoL-scores in polytrauma patients and the general population were found in one study [89], although impairment in some domains were present in others [172, 174, 177]; significant HRQoL-differences between TBI and non-TBI patients, however, could be demonstrated after more than ten years follow-up, especially in mental and psychological domains [89]. In spine polytrauma patients significantly higher satisfaction on mental domains were found than on physical domains [174]. PCS- and MCS-scores improved, although little, up to 24 months after injury [172, 177], although in populations with multiple fractured ribs [175, 188] and midfoot and/or hindfoot fractures [187] population norms could not be achieved [175].
POLO and TOP
Most studies [47,48,49, 51, 58, 74,75,76,77,78, 93, 179, 181, 182, 189] demonstrated reduced HRQoL in severely injured patients several months post-injury (up to several years), defined as reduced scores in at least one of the domains.
Subjective scale
In patients with a suicidal origin of polytrauma, overall outcome was good in half of the patients according to the subjective scale by means of which HRQoL was measured, despite the double adverse influence of severe multiple blunt trauma and psychiatric disorder [33, 36].
Patients surviving trauma resulting in an ISS ≥ 25 had significantly lower HRQoL [54]. A study including military service members experiencing polytrauma revealed reduced QoL as well [59].
Sickness impact profile (SIP)
Most adult patients ≤ 65 years presented with good QoL after severe trauma; the majority showed no disablement according to the SIP. Approximately one tenth of the patients showed severe disablement (defined as a SIP ≥ 20). Two years after the injury, however, only a slight difference in QoL was found when compared to the general population. Also, SIP-scores did not differ significantly between patients with no, mild-moderate and severe TBI [87]. In another study [54], with inclusion of patients > 65 years as well, however, most patients (63%) reported severe disability (SIP ≥ 20), which was defined as a low QoL. SIP work scores remained significantly higher compared to baseline up to 12 months post-trauma, indicating worse employment status in patients suffering major trauma [161].
Patients sustaining pelvic ring fractures reported mild disability after one year [159].
Quality of well-being (QWB) scale
While healthy adults usually score between 0.830 and 0.900 on the QWB-scale, patients with an ISS ≥ 16 scored 0.400 on average. HRQoL improved after 3, 6, 12, 18 and 24 months but remained low [34, 158, 162]; even in adolescent populations, QWB-scores remained below scores of uninjured adolescents [163].
PedsQL
Psychosocial health, although improving over time, was reduced in children one-year post-trauma, whereas baseline physical health scores were achieved eventually [192, 199]. Severely injured children showed comparable mean score on the PedsQL to population norm values 6 to 8 years post-trauma [167].
Nottingham health profile (NHP)
Most patients showed problems in at least one QoL-domain, as well as disability in undertaking daily activities up to 5 years post-trauma [35, 196]. Almost half of the patients was unable to work afterwards [35]. In a population with severe trauma, TBI patients presented with lower HRQoL than non-TBI patients [47].
Life satisfaction checklist (LiSat 9/11)
Three years after severe trauma several domains of HRQoL according to the LiSat9 were affected; 87% of the patients reported lower life satisfaction in at least one domain [86].
After two years, patients with surgically treated pelvic fractured reported poorer HRQoL according to all eleven items of the LiSat 11 compared to a matched normative population, despite good radiologic results [169].
QOLIBRI
Although total QOLIBRI score is similar in both major and non-major TBI inflicted polytrauma patients, polytrauma patients with major TBI are cognitively more impaired than do patients with mild or no TBI. In total, approximately one fifth of the patients met the study’s definition of impaired HRQoL [65]. Elderly (≥ 80 years) with TBI presented with the poorest HRQoL in one of the studies [181].
Trauma-specific QoL questionnaire (T-QoL)
Impairments in everyday daily living activities were found in approximately one third of patients with severe trauma; almost half did not return to work and was diagnosed with PTSD [197]. Up to 12 months post-injury approximately half of the patients reported daily pain [184, 197].
The classification of disability by the international classification of impairment, disabilities and handicaps
QoL was reduced as a result of disability in approximately half of the patients sustaining multiple injuries. Significant improvement occurred over time [164].
Hadorn's QoL and health questionnaire
Bicycle trauma patients with an ISS ≥ 16 experienced significantly more impairments in several QoL-domains [101] (see Table 1, ESM Appendix B).
Quality of life questionnaire score
Quality of life as measured by the QoL questionnaire indicated that polytrauma patients show a significant reduction of capacity for physical effort, which affects work and other activities that are appropriate to age (see Table 1, ESM Appendix B). Half of the patients had normal QoL after 2 years, which suggests an improvement when compared to QoL one year post-polytrauma [32].
St. George’s respiratory questionnaire
Patients admitted with multiple traumas including chest trauma presented with reduced HRQoL, possibly related to pulmonary function limitation [166].
RAND-36
Nine years post-trauma, paediatric patients (≤ 15 years) surviving polytrauma had no different HRQoL than the healthy reference population [85].
Discussion
This review aimed to provide a comprehensive insight into the health-related quality of life of patients surviving severe trauma, including the tools used to assess this outcome.
Summary of main results
In this review, 113 articles were included that evaluated the health-related quality of life in patients with severe trauma. HRQoL in populations with adult patients sustaining severe trauma (e.g., defined as an ISS ≥ 16) is generally reduced when compared to the general population or pre-injury HRQoL, regardless of the tool used to assess this outcome. Interestingly, only paediatric patients (< 16 years) seem to have a similar HRQoL when compared to normative population values [85, 167, 192]. In a substantial number of studies [32, 34, 37, 39, 42, 50, 52, 53, 57, 61, 63, 71, 87, 158, 161, 162, 164, 172, 176, 177, 183, 185, 186, 192, 193, 199] scores in the used HRQoL-instruments increased over time in some domains, suggesting improvement in HRQoL after severe trauma in the months or years to follow after the event leading to the injuries; HRQoL, however, remained generally reduced when compared to population norms or pre-injury status.
The most commonly applied instruments were the SF-36 and EQ-5D; both are so-called generic instruments, suitable for assessing HRQoL in a broad range of patient populations. Of these instruments, the validity is well recognized [102,103,104,105,106,107], leading to extensive use in trauma populations for baseline and follow up assessment of HRQoL; available country specific population norms for all subscales make meaningful comparisons possible. The TOP, QOLIBRI, HASPOC, T-QoL and St. George’s Respiratory Questionnaire were the only disease-specific instruments that were used in the included articles, the first four assessing specifically the impact of trauma on HRQoL. Although these have not been extensively validated until recently, comparisons to the more validated SF-36 and EQ-5D show comparable and hence promising results [48, 65, 70, 75, 108,109,110,111,112].
Strengths and weaknesses of the review
There are certain limitations adherent to this review that need to be addressed.
First, no assessment of methodological quality of the included studies was made. Information on the risk of bias in the included studies is therefore lacking. Some studies, however, are expected to be of lesser methodological quality, for example due to the small sample size (e.g., one study [84] had included only eight patients), retrospective nature of analysis [64, 73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92, 94,95,96,97,98,99,100,101, 159, 160, 164, 165, 172, 174, 175, 178, 180, 184, 187, 188, 194, 195, 198, 199], but especially the lack of a control group or comparison with pre-injury QoL. The latter studies, however, were useful for identification of possible predictors and instruments to assess HRQoL.
Second, all studies that were included in this review, presented results of populations that were identified as having sustained either major, severe, multiple injuries and/or polytrauma, hence allowing patients with varying ISS-cut-off values to be included—the average ISS of populations included in this review ranged from 9 to 57. Therefore, we cannot conclude that this review did include polytrauma patients (often defined as an ISS ≥ 16 [27]) exclusively. Of patients with lower trauma severity scores one can expect better HRQoL, although some studies [37, 43, 54, 64, 77, 79, 87, 98, 170] did not find a significant correlation between injury severity and HRQoL. This suggests that the ISS is primarily useful to predict the life-threatening potential of the injury, which is in accordance with the initial design of ISS, which did not include prediction of HRQoL after trauma [113]. Interestingly, Brasel et al. [43] has indeed demonstrated how objective ISS differed significantly from perceived injury severity and how patients often overestimate the severity of their injuries, possibly as a consequence of the PTSD they suffered post-injury. Nevertheless, a substantial number of studies [32, 34, 35, 37, 41, 45, 53, 55,56,57,58, 60, 61, 68, 81, 101, 163,164,165, 171, 173, 174, 176, 177, 185, 189, 192, 194, 195, 199] demonstrated how polytrauma patients do have significantly worse QoL than do patients with an ISS below 16, and how increasing ISS correlates with reduced HRQoL, which is in line with our expectations. Evidence regarding this issue is therefore rather conflicting. The aim of this review, however, was to summarize the HRQoL of patients with severe trauma or major injury, terms that are ill-defined but nevertheless used frequently and interchangeably in literature with varying definitions; in our review, ISS-thresholds differed between articles describing the same population, and most commonly ISS cut-offs of 9, 12 and 16 were used to identify these patients. The fact that the results of patients presenting with an ISS less than 16 were included in this review, is therefore not considered to be necessarily a major methodological limitation, since there’s no consensus (yet) regarding a strict threshold for severe trauma or major injury in literature. Moreover, several studies suggest that the use of an ISS ≥ 16 as a threshold excludes relevant data relating to morbidity and QoL and suggest that lower cut-off values should be adopted to allow for evaluation of other outcomes than survival [20, 114, 115]. The ISS-threshold is after all chosen arbitrarily and is primarily correlated with mortality [116,117,118,119,120], and studies have demonstrated that an ISS ≥ 12 functions similarly to the ISS ≥ 16 cut-off [205, 206].
Third, we chose to only include studies using the Injury Severity Score (ISS) as an indicator of trauma severity and hence as the only tool to identify severely injured patients by. It is possible that studies examining HRQoL using other severity scoring systems [e.g., the Revised Trauma Score (RTS) or Abbreviated Injury Scale (AIS)] were excluded, hence making this review not exhaustive regarding included articles.
Despite these limitations, this review can be considered to be the most extensive to date, with inclusion of 113 unique publications, the majority of which being conducted prospectively. Furthermore, this review has included publications from 1994 to 2022, providing sufficient information on the health-related quality of life patients suffering severe trauma throughout the years. Finally, this is the first systematic review to be conducted aimed at patients with severe trauma in specific (to our knowledge), that provides information on their HRQoL as well as on instruments that may assist in assessing this outcome in this specific population.
Implications for practice and research
The results of this review, which encompasses studies published more than two decades ago and studies published more recently, are sending the alarming message that the health-related quality of life in patients with severe trauma is significantly reduced in comparison to healthy control groups and pre-injury status. This implies that despite the improvements and advances that have been made in the field of trauma surgery, which have benefited outcomes such as survival and mortality, these did not have its beneficial effects on the HRQoL of severely injured patients. Therefore, future research is urgently needed on at least the following topics:
-
I.
The POLO-chart, which includes the trauma-specific Trauma Outcome Profile (TOP) as an instrument to measure HRQoL, has been validated and used in some, but obviously a minority of studies, as is presented in Table 1 (ESM Appendix B); therefore, further research is needed to explore the reasons and motivations of researchers behind selection of HRQoL-instruments. Variation in selection of instruments across studies decreases the potential to compare studies with each other; therefore, we agree with Polinder et al. [30] recommending the use of the same instrument in studies, which encompasses all dimensions relevant for trauma patients and is easy to use, both for surgeons and patients.
-
II.
Further research is needed on the HRQoL of children surviving severe trauma. In this review, only five studies [85, 163, 167, 192, 199] investigated this outcome in paediatric and adolescent patients exclusively. Recently, Martin-Herz [121] has published a review on this topic, presenting that HRQoL was reduced in four out of six studies; however, studies included in the review were limited (n = 16), and average ISS in the studies included was below 16 in the majority (n = 14) of studies. Therefore, research on HRQoL in severely injured paediatric patients, including suitable, child-friendly instruments needs to receive more attention in the research field.
-
III.
Future research should focus more on the consequences of reduced QoL in patients suffering severe trauma. In this review, we have demonstrated how those patients may be suffering more often from psychiatric comorbidities including depression, anxiety, and PTSD, and how they show reduced capacity to work. This list, however, is not exhaustive; therefore, more focus needs to be placed on the possibly detrimental effects of reduced HRQoL on the patient himself/herself and, not irrelevant, also the consequences for his/her direct environment and general society (e.g., in terms of economic problems).
-
IV.
More information is needed on the parameters that influence HRQoL the most. This might facilitate personalized patient care and prediction of long-term outcomes for incoming patients with severe trauma, which might possibly benefit the patients.
-
V.
Future studies should explore the methods of delivery of the various discussed tools assessing HRQoL, as well as discuss their feasibility in clinical practice.
Conclusions
Health-related quality of life in patients with severe trauma is overall reduced. Instruments used most frequently to assess HRQoL were the SF-36 and EQ-5D. Assessment and documentation of HRQoL in patients with severe trauma should happen on a routine basis in daily clinical practice to make follow-up of those patients possible, which enables detection of changes in terms of improvement or deterioration.
References
World Health Organization. (2014). Injuries and violence: the facts 2014. World Health Organization. https://apps.who.int/iris/handle/10665/149798
Bolorunduro OB, Villegas C, Oyetunji TA, Haut ER, Stevens KA, Chang DC, et al. Validating the Injury Severity Score (ISS) in different populations: ISS predicts mortality better among Hispanics and females. J Surg Res. 2011;166(1):40–4.
The World Health Organization, Geneva, Switzerland. http://www.who.int
Nicholl J, Turner J. Effectiveness of a regional trauma system in reducing mortality from major trauma: before and after study 7. BMJ. 1997;315:1349–54.
Nathens AB, Brunet FP, Maier RV. Development of trauma systems and effect on outcomes after injury. Lancet. 2004;363:1794–801.
Osterwalder JJ. Could a regional trauma system in eastern Switzerland decrease the mortality of blunt polytrauma patients? A prospective cohort study. J Trauma. 2002;52:1030–6.
Mann NC, Mullins RJ, Mackenzie EJ, et al. Systematic review of published evidence regarding trauma system effectiveness. J Trauma. 1999;47:S25–33.
Celso B, Tepas J, Langland-Orban B, Pracht E, Papa L, Lottenberg L, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60(2):371–8 (discussion 378).
Utter GH, Maier RV, Rivara FP, Mock CN, Jurkovich GJ, Nathens AB. Inclusive trauma systems: do they improve triage or outcomes of the severely injured? J Trauma. 2006;60:529–35.
Papa L, Langland-Orban B, Kallenborn C, Tepas JJ 3rd, Lottenberg L, Celso B, et al. Assessing effectiveness of a mature trauma system: Association of trauma center presence with lower injury mortality rate. J Trauma. 2006;61:261–6.
MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366–78. https://doi.org/10.1056/NEJMsa052049.
Durham R, Pracht E, Orban B, Lottenburg L, Tepas J, Flint L. Evaluation of a mature trauma system. Ann Surg. 2006;243(6):775–83. https://doi.org/10.1097/01.sla.0000219644.52926.f1 (discussion 783–5).
Lansink KW, Leenen LP. Do designated trauma systems improve outcome? Curr Opin Crit Care. 2007;13(6):686–90.
The World Health Organization Quality of Life Assessment (WHOQOL). Position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–9.
CDC Gov. HRQOL concepts. https://www.cdc.gov/hrqol/concept.htm
Polinder S, Meerding WJ, Mulder S, Petridou E, van Beeck E, EUROCOST Reference Group. Assessing the burden of injury in six European countries. Bull World Health Organ. 2007;85(1):27–34. https://doi.org/10.2471/blt.06.030973.
Polinder S, Meerding WJ, van Baar ME, Toet H, Mulder S, van Beeck EF, EUROCOST Reference Group. Cost estimation of injury-related hospital admissions in 10 European countries. J Trauma. 2005;59(6):1283–90. https://doi.org/10.1097/01.ta.0000195998.11304.5b (discussion 1290–1).
Tscherne H. The treatment of the seriously injured at an emergency station. Chirurg. 1966;37:249–52.
Border JR, LaDuca J, Seibel R. Priorities in the management of the patient with polytrauma. Prog Surg. 1975;14:84–120.
Thompson L, Hill M, Shaw G. Defining major trauma: a literature review. Br Paramed J. 2019;4(1):22–30. https://doi.org/10.29045/14784726.2019.06.4.1.22.
Sikand M, Williams K, White C, Moran CG. The financial cost of treating polytrauma: implications for tertiary referral centres in the United Kingdom. Injury. 2005;36:733–7. https://doi.org/10.1016/j.injury.2004.12.026.
Biewener A, Aschenbrenner U, Rammelt S, Grass R, Zwipp H. Impact of helicopter transport and hospital level on mortality of polytrauma patients. J Trauma. 2004;56:94–8. https://doi.org/10.1097/01.TA.0000061883.92194.50.
Hildebrand F, Giannoudis P, Kretteck C, Pape HC. Damage control: Extremities. Injury. 2004;35:678–89. https://doi.org/10.1016/j.injury.2004.03.004.
Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: Development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496–504. https://doi.org/10.1097/00005373-200009000-00018.
McLain RF. Functional outcomes after surgery for spinal fractures: return to work and activity. Spine (Phila Pa 1976). 2004;29:470–7. https://doi.org/10.1097/01.BRS.0000092373.57039.FC.
Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma. 1987;27:370–8. https://doi.org/10.1097/00005373-198704000-00005.
Rau CS, Wu SC, Kuo PJ, Chen YC, Chien PC, Hsieh HY. Polytrauma defined by the new Berlin definition: a validation test based on propensity-score matching approach. Int J Environ Res Publ Health. 2017;14:E1045.
Butcher N, Balogh ZJ. The definition of polytrauma: the need for international consensus. Injury. 2009;40(S4):S12–22.
Scholten AC, Haagsma JA, Steyerberg EW, van Beeck EF, Polinder S. Assessment of pre-injury health-related quality of life: a systematic review. Popul Health Metr. 2017;15(1):10. https://doi.org/10.1186/s12963-017-0127-3.
Polinder S, Haagsma JA, Belt E, et al. A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health. 2010;10(1):783.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Vazquez Mata G, Rivera Fernandez R, Perez Aragon A, Gonzalez Carmona A, Fernandez Mondejar E, Navarrete NP. Analysis of quality of life in polytraumatized patients two years after discharge from an intensive care unit. J Trauma. 1996;41(2):326–32.
Ruchholtz S, Pajonk FG, Waydhas C, Lewan U, Nast-Kolb D, Schweiberer L. Long-term results and quality of life after parasuicidal multiple blunt trauma. Crit Care Med. 1999;27(3):522–30. https://doi.org/10.1097/00003246-199903000-00029.
Holbrook TL, Hoyt DB. The impact of major trauma: quality-of-life outcomes are worse in women than in men, independent of mechanism and injury severity. J Trauma. 2004;56(2):284–90.
Dimopoulou I, Anthi A, Mastora Z, Theodorakopoulou M, Konstandinidis A, Evangelou E, et al. Health-related quality of life and disability in survivors of multiple trauma one year after intensive care unit discharge. Am J Phys Med Rehabil. 2004;83(3):171–6.
Pajonk FG, Ruchholtz S, Waydhas C, Schneider-Axmann T. Long-term follow-up after severe suicide attempt by multiple blunt trauma. Eur Psychiatry. 2005;20(2):115–20. https://doi.org/10.1016/j.eurpsy.2004.10.003.
Kiely JM, Brasel KJ, Weidner KL, Guse CE, Weigelt JA. Predicting quality of life six months after traumatic injury. J Trauma. 2006;61(4):791–8.
Lichtveld RA, Spijkers AT, Panhuizen IF, Holtslag HR, van der Werken C. Achtergronden en gevolgen van het missen van letsels in de ambulancezorg bij ernstig gewonde ongevalspatiënten die vervoerd werden naar het Universitair Medisch Centrum Utrecht, 1999–2000 [Background and consequences of injuries missed when diagnosing severely injured accident victims in prehospital care in patients transported by ambulance to the University Medical Centre in Utrecht, 1999–2000]. Ned Tijdschr Geneeskd. 2006;150(40):2197–202.
Lippert-Grüner M, Maegele M, Haverkamp H, Klug N, Wedekind C. Health-related quality of life during the first year after severe brain trauma with and without polytrauma. Brain Inj. 2007;21(5):451–5. https://doi.org/10.1080/02699050701343961.
Holtslag HR, van Beeck EF, Lindeman E, Leenen LP. Determinants of long-term functional consequences after major trauma. J Trauma. 2007;62(4):919–27.
Pirente N, Blum C, Wortberg S, Bostanci S, Berger E, Lefering R, et al. Quality of life after multiple trauma: the effect of early onset psychotherapy on quality of life in trauma patients. Langenbecks Arch Surg. 2007;392(6):739–45.
Soberg HL, Finset A, Bautz-Holter E, Sandvik L, Roise O. Return to work after severe multiple injuries: a multidimensional approach on status 1 and 2 years postinjury. J Trauma. 2007;62(2):471–81.
Brasel KJ, Deroon-Cassini T, Bradley CT. Injury severity and quality of life: whose perspective is important? J Trauma. 2010;68(2):263–8.
Gross T, Attenberger C, Huegli RW, Amsler F. Factors associated with reduced longer-term capacity to work in patients after polytrauma: a Swiss trauma center experience. J Am Coll Surg. 2010;211(1):81–91. https://doi.org/10.1016/j.jamcollsurg.2010.02.042.
Probst C, Zelle B, Panzica M, Lohse R, Sitarro NA, Krettek C, et al. Clinical re-examination or more years after polytrauma: is there a gender related difference? J Trauma. 2010;68(3):706–11.
Zeckey C, Hildebrand F, Pape HC, Mommsen P, Panzica M, Zelle BA, et al. Head injury in polytrauma-Is there an effect on outcome more than 10 years after the injury? Brain Inj. 2011;25(6):551–9.
Gross T, Schüepp M, Attenberger C, Pargger H, Amsler F. Outcome in polytraumatized patients with and without brain injury. Acta Anaesthesiol Scand. 2012;56(9):1163–74. https://doi.org/10.1111/j.1399-6576.2012.02724.x.
Attenberger C, Amsler F, Gross T. Clinical evaluation of the Trauma Outcome Profile (TOP) in the longer-term follow-up of polytrauma patients. Injury. 2012;43(9):1566–74. https://doi.org/10.1016/j.injury.2011.01.002.
Kaske S, Lefering R, Trentzsch H, Driessen A, Bouillon B, Maegele M, et al. Quality of life two years after severe trauma: a single-centre evaluation. Injury. 2014;45(Suppl 3):S100–5.
Soberg HL, Bautz-Holter E, Finset A, Roise O, Andelic N. Physical and mental health 10 years after multiple trauma: a prospective cohort study. J Trauma Acute Care Surg. 2015;78(3):628–33. https://doi.org/10.1097/TA.0000000000000541.
Kaske S, Lefering R, Bouillon B, Maegele M, Driessen A, Probst C, et al. Bestandsaufnahme der Schmerzsituation von Schwerstverletzten zwei Jahre nach Trauma [Pain assessment of severely injured patients 2 years after trauma]. Schmerz. 2016;30(3):273–8.
Bouman AI, Hemmen B, Evers SM, van de Meent H, Ambergen T, Vos PE, et al. Effects of an integrated “fast track” rehabilitation service for multi-trauma patients: a non-randomized clinical trial in the Netherlands. PLoS ONE. 2017;12(1): e0170047. https://doi.org/10.1371/journal.pone.0170047.
Angerpointner K, Ernstberger A, Bosch K, Zeman F, Koller M, Kerschbaum M. Quality of life after multiple trauma: results from a patient cohort treated in a certified trauma network. Eur J Trauma Emerg Surg. 2021;47(1):121–7. https://doi.org/10.1007/s00068-019-01160-y.
DePalma JA, Fedorka P, Simko LC. Quality of life experienced by severely injured trauma survivors. AACN Clin Issues. 2003;14(1):54–63. https://doi.org/10.1097/00044067-200302000-00007.
Wad MS, Laursen T, Fruergaard S, Morgen SS, Dahl B. Survival and health related quality of life after severe trauma - a 15 years follow up study. Injury. 2018;49(2):191–4.
Ulvik A, Kvåle R, Wentzel-Larsen T, Flaatten H. Quality of life 2–7 years after major trauma. Acta Anaesthesiol Scand. 2008;52(2):195–201.
Fleischhacker E, Trentzsch H, Kuppinger D, Meigel F, Beyer F, Hartl WH. Long-term changes of patient-reported quality of life after major trauma: the importance of the time elapsed after injury. Injury. 2018;49(2):195–202.
Christensen MC, Banner C, Lefering R, Vallejo-Torres L, Morris S. Quality of life after severe trauma: results from the global trauma trial with recombinant Factor VII. J Trauma. 2011;70(6):1524–31.
Brickell TA, Lange RT, French LM. Health-related quality of life within the first 5 years following military-related concurrent mild traumatic brain injury and polytrauma. Mil Med. 2014;179(8):827–38. https://doi.org/10.7205/MILMED-D-13-00506.
Holtslag HR, van Beeck EF, Lichtveld RA, Leenen LP, Lindeman E, van der Werken C. Individual and population burdens of major trauma in the Netherlands. Bull World Health Organ. 2008;86(2):111–7. https://doi.org/10.2471/blt.06.033803.
Scholten AC, Haagsma JA, Andriessen TM, Vos PE, Steyerberg EW, van Beeck EF, et al. Health-related quality of life after mild, moderate and severe traumatic brain injury: patterns and predictors of suboptimal functioning during the first year after injury. Injury. 2015;46(4):616–24.
Forslund MV, Roe C, Sigurdardottir S, Andelic N. Predicting health-related quality of life 2 years after moderate-to-severe traumatic brain injury. Acta Neurol Scand. 2013;128(4):220–7.
Soberg HL, Finset A, Roise O, Bautz-Holter E. The trajectory of physical and mental health from injury to 5 years after multiple trauma: a prospective, longitudinal cohort study. Arch Phys Med Rehabil. 2012;93(5):765–74.
Bott A, Odutola A, Halliday R, Acharya MR, Ward A, Chesser TJS. Long-term patient-reported functional outcome of polytraumatized patients with operatively treated pelvic fractures. J Orthop Trauma. 2019;33(2):64–70.
Born K, Amsler F, Gross T. Prospective evaluation of the Quality of Life after Brain Injury (QOLIBRI) score: minor differences in patients with major versus no or mild traumatic brain injury at one-year follow up. Health Qual Life Outcomes. 2018;16(1):136. https://doi.org/10.1186/s12955-018-0966-z.
Weber CD, Horst K, Nguyen AR, Bader MJ, Probst C, Zelle B, et al. Return to sports after multiple trauma: which factors are responsible?-Results from a 17-year follow-up. Clin J Sport Med. 2017;27(5):481–6. https://doi.org/10.1097/JSM.0000000000000373.
Macke C, Winkelmann M, Mommsen P, Probst C, Zelle B, Krettek C, et al. Injuries to the upper extremities in polytrauma: limited effect on outcome more than ten years after injury—a cohort study in 629 patients. Bone Jt J. 2017;99-B(2):255–60. https://doi.org/10.1302/0301-620X.99B2.37999.
Gross T, Amsler F. Prevalence and incidence of longer term pain in survivors of polytrauma. Surgery. 2011;150(5):985–95.
Pape HC, Probst C, Lohse R, Zelle BA, Panzica M, Stalp M, et al. Predictors of late clinical outcome following orthopedic injuries after multiple trauma. J Trauma. 2010;69(5):1243–51. https://doi.org/10.1097/TA.0b013e3181ce1fa1.
Zelle B, Stalp M, Weihs CH, Müller F, Reiter FO, Krettek CH, et al. Arbeitsgemeinschaft “Polytrauma” der Deutschen Gesellschaft für Unfallchirurgie. Hannover Score for Polytrauma Outcome (HASPOC). Validierung am Beispiel von 170 Polytrauma-Patienten und Vergleich mit dem SF-12 [Validation of the Hannover Score for Polytrauma Outcome (HASPOC) in a sample of 170 polytrauma patients and a comparison with the 12-Item Short-Form Health Survey]. Chirurg. 2003;74(4):361–9. https://doi.org/10.1007/s00104-003-0621-y.
Soberg HL, Roise O, Bautz-Holter E, Finset A. Returning to work after severe multiple injuries: multidimensional functioning and the trajectory from injury to work at 5 years. J Trauma. 2011;71(2):425–34. https://doi.org/10.1097/TA.0b013e3181eff54f.
Turchin DC, Schemitsch EH, McKee MD, Waddell JP. Do foot injuries significantly affect the functional outcome of multiply injured patients? J Orthop Trauma. 1999;13(1):1–4. https://doi.org/10.1097/00005131-199901000-00001.
Janssen C, Ommen O, Neugebauer E, Lefering R, Pfaff H. How to improve satisfaction with hospital stay of severely injured patients. Langenbecks Arch Surg. 2007;392(6):747–60. https://doi.org/10.1007/s00423-007-0186-1.
Wurm S, Röse M, von Rüden C, Woltmann A, Bühren V. Das schwere Polytrauma mit einem ISS ≥ 50 [Severe polytrauma with an ISS ≥ 50]. Z Orthop Unfall. 2012;150(3):296–301. https://doi.org/10.1055/s-0031-1280415.
Lefering R, Tecic T, Schmidt Y, Pirente N, Bouillon B, Neugebauer E, POLO Chart Study Group. Quality of life after multiple trauma: validation and population norm of the Polytrauma Outcome (POLO) chart. Eur J Trauma Emerg Surg. 2012;38(4):403–15. https://doi.org/10.1007/s00068-011-0149-7.
Simmel S, Drisch S, Haag S, Bühren V. Langzeitergebnisse nach Polytrauma mit ISS ≥25. Outcome und Prädiktoren der Lebensqualität [Long-term results after multiple trauma with ISS ≥ 25. Outcome and predictors of quality of life]. Chirurg. 2013;84(9):771–9.
Zwingmann J, Hagelschuer P, Langenmair E, Bode G, Herget G, Südkamp NP, et al. Lower health-related quality of life in polytrauma patients: long-term follow-up after over 5 years. Medicine (Baltimore). 2016;95(19): e3515. https://doi.org/10.1097/MD.0000000000003515.
von Rüden C, Woltmann A, Röse M, Wurm S, Rüger M, Hierholzer C, et al. Outcome after severe multiple trauma: a retrospective analysis. J Trauma Manag Outcomes. 2013;7(1):4. https://doi.org/10.1186/1752-2897-7-4.
Falkenberg L, Zeckey C, Mommsen P, Winkelmann M, Zelle BA, Panzica M, et al. Longterm outcome in 324 polytrauma patients: what factors are associated with posttraumatic stress disorder and depressive disorder symptoms? Eur J Med Res. 2017;22(1):44. https://doi.org/10.1186/s40001-017-0282-9.
Andruszkow H, Probst C, Grün O, Krettek C, Hildebrand F. Does additional head trauma affect the long-term outcome after upper extremity trauma in multiple traumatized patients: is there an additional effect of traumatic brain injury? Clin Orthop Relat Res. 2013;471(9):2899–905. https://doi.org/10.1007/s11999-013-3031-6.
Janssen C, Ommen O, Neugebauer E, Lefering R, Pfaff H. Predicting health-related quality of life of severely injured patients: sociodemographic, economic, trauma, and hospital stay-related determinants. Eur J Trauma Emerg Surg. 2008;34(3):277–86.
Zelle BA, Panzica M, Vogt MT, Sittaro NA, Krettek C, Pape HC. Influence of workers’ compensation eligibility upon functional recovery 10 to 28 years after polytrauma. Am J Surg. 2005;190(1):30–6.
Zelle BA, Brown SR, Panzica M, Lohse R, Sittaro NA, Krettek C, et al. The impact of injuries below the knee joint on the long-term functional outcome following polytrauma. Injury. 2005;36(1):169–77. https://doi.org/10.1016/j.injury.2004.06.004.
Gribnau AJ, van Hensbroek PB, Haverlag R, Ponsen KJ, Been HD, Goslings JC. U-shaped sacral fractures: surgical treatment and quality of life. Injury. 2009;40(10):1040–8. https://doi.org/10.1016/j.injury.2008.11.027.
Van der Sluis CK, Kingma J, Eisma WH, ten Duis HJ. Pediatric polytrauma: short-term and long-term outcomes. J Trauma. 1997;43(3):501–6. https://doi.org/10.1097/00005373-199709000-00019.
Anke AG, Fugl-Meyer AR. Life satisfaction several years after severe multiple trauma—a retrospective investigation. Clin Rehabil. 2003;17(4):431–42. https://doi.org/10.1191/0269215503cr629oa.
Post RB, van der Sluis CK, Ten Duis HJ. Return to work and quality of life in severely injured patients. Disabil Rehabil. 2006;28(22):1399–404.
Giannoudis PV, Chalidis BE, Roberts CS. Internal fixation of traumatic diastasis of pubic symphysis: is plate removal essential? Arch Orthop Trauma Surg. 2008;128(3):325–31.
Steel J, Youssef M, Pfeifer R, Ramirez JM, Probst C, Sellei R, et al. Health-related quality of life in patients with multiple injuries and traumatic brain injury 10+ years postinjury. J Trauma. 2010;69(3):523–30. https://doi.org/10.1097/TA.0b013e3181e90c24 (discussion 530–1).
Baranyi A, Leithgöb O, Kreiner B, Tanzer K, Ehrlich G, Hofer HP, et al. Relationship between posttraumatic stress disorder, quality of life, social support, and affective and dissociative status in severely injured accident victims 12 months after trauma. Psychosomatics. 2010;51(3):237–47. https://doi.org/10.1176/appi.psy.51.3.237.
van der Vliet QMJ, Sweet AAR, Bhashyam AR, Ferree S, van Heijl M, Houwert RM, et al. Polytrauma and high-energy injury mechanisms are associated with worse patient-reported outcomes after distal radius fractures. Clin Orthop Relat Res. 2019;477(10):2267–75. https://doi.org/10.1097/CORR.0000000000000757.
Beks RB, de Jong MB, Houwert RM, Sweet AAR, De Bruin IGJM, Govaert GAM, et al. Longterm follow-up after rib fixation for flail chest and multiple rib fractures. Eur J Trauma Emerg Surg. 2019;45(4):645–54. https://doi.org/10.1007/s00068-018-1009-5.
Saengniam W, Jitpanya C. Quality of life and its predictors in Thai patients following multiple trauma. J Health Res. 2019;33(4):314–22. https://doi.org/10.1108/JHR-09-2018-0091.
Martino C, Russo E, Santonastaso DP, Gamberini E, Bertoni S, Padovani E, et al. Long-term outcomes in major trauma patients and correlations with the acute phase. World J Emerg Surg. 2020;15:6. https://doi.org/10.1186/s13017-020-0289-3.
Jackson JC, Obremskey W, Bauer R, Greevy R, Cotton BA, Anderson V, et al. Long-term cognitive, emotional, and functional outcomes in trauma intensive care unit survivors without intracranial hemorrhage. J Trauma. 2007;62(1):80–8. https://doi.org/10.1097/TA.0b013e31802ce9bd.
Karhof S, Hietbrink F, Boot R, van Wessem KJP, Leenen LPH, Simmermacher RKJ. Management strategies and outcome of blunt traumatic abdominal wall defects: a single centre experience. Injury. 2019;50(9):1516–21. https://doi.org/10.1016/j.injury.2019.06.028.
Leijdesdorff HA, Krijnen P, Van Rooyen L, Marang-van de Mheen P, Rhemrev S, Schipper IB. Reduced quality of life, fatigue, and societal participation after polytrauma. Int Surg. 2018;103(3–4):158–66.
Tuchner M, Meiner Z, Parush S, Hartman-Maeir A. Health-related quality of life two years after injury due to terrorism. Isr J Psychiatry Relat Sci. 2010;47(4):269–75.
Renovell-Ferrer P, Bertó-Martí X, Diranzo-García J, Barrera-Puigdorells L, Estrems-Díaz V, Silvestre-Muñoz A, et al. Functional outcome after calcaneus fractures: a comparison between polytrauma patients and isolated fractures. Injury. 2017;48(Suppl 6):S91–5. https://doi.org/10.1016/S0020-1383(17)30801-X.
Zamora-Navas P, Estades-Rubio FJ, Cano JR, Guerado E. Floating hip and associated injuries. Injury. 2017;48(Suppl 6):S75–80. https://doi.org/10.1016/S0020-1383(17)30798-2.
Zibung E, Riddez L, Nordenvall C. Impaired quality of life after bicycle trauma. Injury. 2016;47(5):1078–82.
Brenneman FD, Redelmeier DA, Boulanger BR, McLellan BA, Culhane JP. Long-term outcomes in blunt trauma: who back to work? J Trauma. 1997;42:778–81.
MacKenzie EJ, McCarthy ML, Ditunno JF, Forrester-Staz C, Gruen GS, Marion DW, et al. Using the SF36 for characterising outcome after multiple trauma involving head injury. J Trauma. 2002;52:527–34.
Brooks R, Rabin R, de Charro F. The measurement and valuation of health status using EQ-5D: a European perspective: evidence from the EuroHRQL BIO MED research programme. Dordrecht: Kluwer Academic Publishers; 2003.
Rossaint R, Christensen MC, Choong PIT, et al. on behalf of the NovoSeven® Trauma Study Group. Cost-effectiveness of recombinant activated factor VII as adjunctive therapy for bleeding control in severely injured trauma patients in Germany. Eur J Trauma Emerg Surg. 2007;33:528–38.
Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D2 valuation model. Med Care. 2005;43:203–20.
Luo N, Johnson JA, Shaw JW, Feeny D, Coons SJ. Self-reported health status of the general adult U.S. population as assessed by the EQ-5D and Health Utilities Index. Med Care. 2005;43:1078–86.
Pirente N, Bouillon B, Schäfer B, Raum M, Helling HJ, Berger E, et al. The polytrauma-outcome-(POLO-)chart. Unfallchirurg. 2002;105(Suppl 5):413–22.
Von Steinbuechel N, Wilson L, Gibbons H, Hawthorne G, Höfer S, Schmidt S, et al. Quality of Life after brain injury (QOLIBRI): Scale validity and correlates of quality of life. J Neurotrauma. 2010;27:1157–65.
Von Steinbuechel N, Petersen C, Bullinger M. Assessment of health-related quality of life in persons after traumatic brain injury—development of the Qolibri, a specific measure. Acta Neurochir Suppl. 2005;93:43–9.
Von Steinbuechel N, Wilson L, Gibbons H, Hawthorne G, Höfer S, Schmidt S, Bullinger M, Maas A, Neugebauer E, Powell J, et al. Quality of Life after brain injury (QOLIBRI): Scale development and metric properties. J Neurotrauma. 2010;27:1167–85.
Truelle JL, Koskinen S, Hawthorne G, Sarajuuri J, Formisano R, von Wild K, et al. Quality of life after traumatic brain injury: the clinical use of the QOLIBRI, a novel disease-specific instrument. Brain Inj. 2010;24:1272–91.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187.
Palmer C. Major trauma and the injury severity score—where should we set the bar? Annu Proc Assoc Adv Automot Med. 2007;51:13–29.
Somers RL. The probability of death score: an improvement of the injury severity score. Accid Anal Prev. 1983;15(4):247–57.
Osler T, Baker SP, Long W. A modification of the Injury Severity Score that both improves accuracy and simplifies scoring. J Trauma. 1997;43(6):922–5.
Osler T, Glance L, Buzas JS, Mukamel D, Wagner J, Dick A. A trauma mortality prediction model based on the anatomic injury scale. Ann Surg. 2008;247(6):1041–8.
Frankema SPG, Steyerberg EW, Edwards MJR, van Vugt AB. Comparison of Current Injury Scales for survival chance estimation: an evaluation comparing the predictive performance of the ISS, NISS, and AP Scores in a Dutch local trauma registration. J Trauma Inj Infect Crit Care. 2005;58(3):596–604.
Baxt WG, Upenieks V. The lack of full correlation between the Injury Severity Score and the resource needs of injured patients. Ann Emerg Med. 1990;19(12):1396–400. https://doi.org/10.1016/s0196-0644(05)82606-x.
Valenzuela TD. What is “major trauma?” Ann Emerg Med. 1990;19(12):1470–1. https://doi.org/10.1016/s0196-0644(05)82624-1.
Martin-Herz SP, Zatzick DF, McMahon RJ. Health-related quality of life in children and adolescents following traumatic injury: a review. Clin Child Fam Psychol Rev. 2012;15(3):192–214. https://doi.org/10.1007/s10567-012-0115-x.
Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33.
Larson CO. Use of the SF-12 instrument for measuring the health of homeless persons. Health Serv Res. 2002;37(3):733–50. https://doi.org/10.1111/1475-6773.00046.
Brazier J, Jones N, Kind P. Testing the validity of the Euroqol and comparing it with the SF-36 health survey questionnaire. Qual Life Res. 1993;2(3):169–80. https://doi.org/10.1007/BF00435221.
Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016;4:2050312116671725. https://doi.org/10.1177/2050312116671725.
Rabin R, Gudex C, Selai C, Herdman M. From translation to version management: a history and review of methods for the cultural adaptation of the EuroQol five-dimensional questionnaire. Value Health. 2014;17(1):70–6. https://doi.org/10.1016/j.jval.2013.10.006.
Schrag A, Selai C, Jahanshahi M, Quinn NP. The EQ-5D—a generic quality of life measure is a useful instrument to measure quality of life in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2000;69(1):67–73. https://doi.org/10.1136/jnnp.69.1.67.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36. https://doi.org/10.1007/s11136-011-9903-x.
EuroQuol Research Foundation, EQ-5D. 2017. http://www.euroqol.org/home.html. Accessed 26 Mar 2020
The EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72.
Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35:1095–108.
Hadorn DC, Sorensen J, Holte J. Large-scale health outcomes evaluation: how should quality of life be measured? Part II—questionnaire validation in a cohort of patients with advanced cancer. J Clin Epidemiol. 1995;48:619–29.
Stalp M, Koch C, Krettek C, Pape HC, der Polytrauma DGUAG. Entwicklung eines standardisierten Instruments zur quantitativen und reproduzierbaren Rehabilitationserfassung nach Polytrauma (HASPOC). Chirurg. 2001;72:312.
Stalp M, Koch C, Ruchholtz S, Regel G, Panzica M, Krettek C, et al. Standardized outcome evaluation after blunt multiple injuries by scoring systems: a clinical follow-up investigation 2 years after injury. J Trauma. 2002;52(6):1160–8. https://doi.org/10.1097/00005373-200206000-00023.
Stalp M, Koch C, Regel G, Krettek C. Pape HC [Development of a standardized instrument for quantitative and reproducible rehabilitation data assessment after polytrauma (HASPOC)]. Chirurg. 2001;72:312–8.
Black NA, Jenkinson C, Hayes JA, Young D, Vella K, Rowan KM, et al. Review of outcome measures used in adult critical care. Crit Care Med. 2001;29(11):2119–24. https://doi.org/10.1097/00003246-200111000-00012.
Hurel D, Loirat P, Saulnier F, Nicolas F, Brivet F. Quality of life 6 months after intensive care: results of a prospective multicenter study using a generic health status scale and a satisfaction scale. Intensive Care Med. 1997;23:331–7.
Gopal I, Bhonagiri S, Ronco C, Bellomo R. Out of hospital outcome and quality of life in survivors of combined acute multiple organ and renal failure treated with continuous venovenous hemofiltration/hemodiafiltration. Intensive Care Med. 1997;23(7):766–72. https://doi.org/10.1007/s001340050407.
Dimopoulou I, Anthi A, Michalis A, Tzelepis GE. Functional status and quality of life in long-term survivors of cardiac arrest after cardiac surgery. Crit Care Med. 2001;29(7):1408–11. https://doi.org/10.1097/00003246-200107000-00018.
Hinz A, Klaiberg A, Schumacher J, Brähler E. The psychometric quality of the Nottingham Health Profile (NHP) in the general population. Psychother Psych Med. 2003;53:353–8.
Vazquez Mata G, Rivera Fernandez R, Gonzalez Carmona A, Delgado-Rodriguez M, Torres Ruiz JM, Raya Pugnaire A, Aguayo de Hoyos E. Factors related to quality of life 12 months after discharge from an intensive care unit. Crit Care Med. 1992;20(9):1257–62. https://doi.org/10.1097/00003246-199209000-00012.
Rivera Fernandez R, Vazquez Mata G, Conzalez Carmona A, Torres Ruiz JM, Delgado-Rodriguez M, Abizanda Campos R, et al. Descripción de una encuesta de calidad de vida en medicina intensiva. Med Intensiva. 1991;15:313.
Kaplan RM, Bush JW. Health-related quality of life measurement for evaluation research and policy analysis. Health Psychol. 1982;1:61–80.
Kaplan RM, Bush JW, Berry CC. The reliability, stability and generalizability of a health status index. In: Proceedings of the American Statistical Association, Social Statistics Section, 1978:704–9.
Anderson JP, Bush JW, Berry CC. Classifying function for health outcome and quality of life evaluation: self versus interviewer modes. Med Care. 1986;24:454–69.
Anderson JP, Bush JW, Berry CC. Internal consistency analysis. J Chronic Dis. 1988;41:127–37.
Prcic A, Aganovic D, Hadziosmanovic O. Sickness impact profile (SIP) score, a good alternative instrument for measuring quality of life in patients with ileal urinary diversions. Acta Inform Med. 2013;21(3):160–5. https://doi.org/10.5455/aim.2013.21.160-5.
Jurkovich G, Mock C, MacKenzie E, Burgess A, Cushing B, deLateur B, et al. The Sickness Impact Profile as a tool to evaluate functional outcome in trauma patients. J Trauma. 1995;39:625–31.
Carter WB, Bobbitt RA, Bergner M, Gilson BS. Validation of an interval scaling: the sickness impact profile. Health Serv Res. 1976;11(4):516–28.
Pollard WE, Bobbitt RA, Bergner M, Martin DP, Gilson BS. The Sickness Impact Profile: reliability of a health status measure. Med Care. 1976;14(2):146–55.
Bergner M, Bobbitt RA, Pollard WE, Martin DP, Gilson BS. The sickness impact profile: validation of a health status measure. Med Care. 1976;14(1):57–67.
Jacobs HM, Luttik A, Touw-Otten FW, de Melker RA. De ‘sickness impact profile’; resultaten van een valideringsonder- zoek van de Nederlandse versie. [The sickness impact profile; results of an evaluation study of the Dutch version]. Ned Tijdschr Geneeskd. 1990;134:1950–4.
Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care. 1981;19:787–805.
Gruen GS, Leit ME, Gruen RJ, Garisson HG, Auble TE, Peitzman AB. Functional outcome of patients with unstable pelvic ring fractures stabilized with open reduction and internal fixation. J Trauma. 1995;39:838–44.
Morris S, Lenihan B, Duddy L, O’Sullivan M. Outcome after musculoskeletal trauma treated in a regional hospital. J Trauma. 2000;49:461–9.
Gilson BS, Gilson JS, Bergner M, Bobbit RA, Kressel S, Pollard WE, et al. The sickness impact profile. Development of an outcome measure of health care. Am J Public Health. 1975;65:1304–10.
Holbrook TL, Hoyt DB, Anderson JP, Hollingsworth-Fridlund P, Shackford SR. Functional limitation after major trauma: a more sensitive assessment using the Quality of Well-being scale–the trauma recovery pilot project. J Trauma. 1994;36(1):74–8.
Gruen GS, Leit ME, Gruen RJ, Garrison HG, Auble TE, Peitzman AB. Functional outcome of patients with unstable pelvic ring fractures stabilized with open reduction and internal fixation. J Trauma. 1995;39(5):838–44. https://doi.org/10.1097/00005373-199511000-00006 (discussion 844–5).
Fern KT, Smith JT, Zee B, Lee A, Borschneck D, Pichora DR. Trauma patients with multiple extremity injuries: resource utilization and long-term outcome in relation to injury severity scores. J Trauma. 1998;45(3):489–94. https://doi.org/10.1097/00005373-199809000-00010.
Michaels AJ, Michaels CE, Smith JS, Moon CH, Peterson C, Long WB. Outcome from injury: general health, work status, and satisfaction 12 months after trauma. J Trauma. 2000;48(5):841–8. https://doi.org/10.1097/00005373-200005000-00007 (discussion 848–50).
Holbrook TL, Hoyt DB, Stein MB, Sieber WJ. Perceived threat to life predicts posttraumatic stress disorder after major trauma: risk factors and functional outcome. J Trauma. 2001;51(2):287–92. https://doi.org/10.1097/00005373-200108000-00010 (discussion 292–3).
Holbrook TL, Hoyt DB, Coimbra R, Potenza B, Sise MJ, Sack DI, et al. Trauma in adolescents causes long-term marked deficits in quality of life: adolescent children do not recover preinjury quality of life or function up to two years postinjury compared to national norms. J Trauma. 2007;62(3):577–83. https://doi.org/10.1097/TA.0b013e318031aa97 (discussion 583).
Hładki W, Lorkowski J, Brongel L, Trybus M, Nazimek R, Kuliś M, et al. Quality of life and disability as a result of multiple injuries. Polish J Surg. 2007. https://doi.org/10.2478/v10035-007-0032-8.
Harris IA, Young JM, Rae H, Jalaludin BB, Solomon MJ. Predictors of general health after major trauma. J Trauma. 2008;64(4):969–74. https://doi.org/10.1097/01.ta.0000245972.83948.1a.
Leone M, Brégeon F, Antonini F, Chaumoître K, Charvet A, Ban LH, et al. Long-term outcome in chest trauma. Anesthesiology. 2008;109(5):864–71. https://doi.org/10.1097/ALN.0b013e31818a4009.
Janssens L, Gorter JW, Ketelaar M, Kramer WL, Holtslag HR. Long-term health-related quality of life in major pediatric trauma: a pilot study. Eur J Trauma Emerg Surg. 2009;35(4):371–7. https://doi.org/10.1007/s00068-009-8217-y.
Bilén K, Ponzer S, Castrén M, Pettersson H, Ottosson C. The impact of trauma mechanism on outcome: a follow-up study on health-related quality of life after major trauma. Eur J Trauma Emerg Surg. 2010;36(5):449–55. https://doi.org/10.1007/s00068-010-0003-3.
Borg T, Berg P, Fugl-Meyer K, Larsson S. Health-related quality of life and life satisfaction in patients following surgically treated pelvic ring fractures. A prospective observational study with two years follow-up. Injury. 2010;41(4):400–4. https://doi.org/10.1016/j.injury.2009.11.006.
Overgaard M, Høyer CB, Christensen EF. Long-term survival and health-related quality of life 6 to 9 years after trauma. J Trauma. 2011;71(2):435–41. https://doi.org/10.1097/TA.0b013e31820e7ec3.
Ringburg AN, Polinder S, van Ierland MC, Steyerberg EW, van Lieshout EM, Patka P, et al. Prevalence and prognostic factors of disability after major trauma. J Trauma. 2011;70(4):916–22. https://doi.org/10.1097/TA.0b013e3181f6bce8.
Gabbe BJ, Simpson PM, Sutherland AM, Wolfe R, Lyons RA, Cameron PA. Evaluating time points for measuring recovery after major trauma in adults. Ann Surg. 2013;257(1):166–72. https://doi.org/10.1097/SLA.0b013e31825d7422.
Rainer TH, Yeung JH, Cheung SK, Yuen YK, Poon WS, Ho HF, et al. Assessment of quality of life and functional outcome in patients sustaining moderate and major trauma: a multicentre, prospective cohort study. Injury. 2014;45(5):902–9. https://doi.org/10.1016/j.injury.2013.11.006.
Tee JW, Chan CH, Gruen RL, Fitzgerald MC, Liew SM, Cameron PA, et al. Early predictors of health-related quality of life outcomes in polytrauma patients with spine injuries: a level 1 trauma center study. Global Spine J. 2014;4(1):21–32. https://doi.org/10.1055/s-0033-1358617.
Marasco S, Lee G, Summerhayes R, Fitzgerald M, Bailey M. Quality of life after major trauma with multiple rib fractures. Injury. 2015;46(1):61–5. https://doi.org/10.1016/j.injury.2014.06.014.
Larsen P, Goethgen CB, Rasmussen S, Iyer AB, Elsoe R. One-year development of QOL following orthopaedic polytrauma: a prospective observational cohort study of 53 patients. Arch Orthop Trauma Surg. 2016;136(11):1539–46. https://doi.org/10.1007/s00402-016-2550-5.
Dinh MM, Cornwall K, Bein KJ, Gabbe BJ, Tomes BA, Ivers R. Health status and return to work in trauma patients at 3 and 6 months post-discharge: an Australian major trauma centre study. Eur J Trauma Emerg Surg. 2016;42(4):483–90. https://doi.org/10.1007/s00068-015-0558-0.
van der Vliet QMJ, Esselink TA, Heng M, Houwert RM, Leenen LPH, Hietbrink F. Functional outcomes of traumatic midfoot injuries. Injury. 2018;49(11):2087–92. https://doi.org/10.1016/j.injury.2018.09.021.
Spreadborough S, Radford K, das Nair R, Brooks A, Duffy M. A study of outcomes of patients treated at a UK major trauma centre for moderate or severe injuries one to three years after injury. Clin Rehabil. 2018;32(3):410–8. https://doi.org/10.1177/0269215517730862.
Spijker EE, Jones K, Duijff JW, Smith A, Christey GR. Psychiatric comorbidities in adult survivors of major trauma: findings from the Midland Trauma Registry. J Prim Health Care. 2018;10(4):292–302. https://doi.org/10.1071/HC17091.
Gross T, Amsler F. One-year outcome following brain injury: a comparison of younger versus elderly major trauma patients. Arch Orthop Trauma Surg. 2018;138(10):1375–87. https://doi.org/10.1007/s00402-018-2974-1.
Gross T, Morell S, Amsler F. Longer-term quality of life following major trauma: age only significantly affects outcome after the age of 80 years. Clin Interv Aging. 2018;30(13):773–85. https://doi.org/10.2147/CIA.S158344.
Rainer TH, Hung KKC, Yeung JHH, Cheung SKC, Leung YK, Leung LY, et al. Trajectory of functional outcome and health status after moderate-to-major trauma in Hong Kong: a prospective 5 year cohort study. Injury. 2019;50(5):1111–7. https://doi.org/10.1016/j.injury.2019.02.017.
Velmahos CS, Herrera-Escobar JP, Al Rafai SS, Chun Fat S, Kaafarani H, Nehra D, et al. It still hurts! Persistent pain and use of pain medication one year after injury. Am J Surg. 2019;218(5):864–8. https://doi.org/10.1016/j.amjsurg.2019.03.022.
Llaquet Bayo H, Montmany S, Rebasa P, Secanella M, Alberich M, Navarro S. Analysis of quality of life after major trauma: a spanish follow-up cohort study. Eur J Trauma Emerg Surg. 2019;45(2):289–97. https://doi.org/10.1007/s00068-018-0920-0.
Gross T, Morell S, Amsler F. Gender-specific improvements in outcome 1 and 2 years after major trauma. J Surg Res. 2019;235:459–69. https://doi.org/10.1016/j.jss.2018.10.024.
Diacon AL, Kimmel LA, Hau RC, Gabbe BJ, Edwards ER. Outcomes of midfoot and hindfoot fractures in multitrauma patients. Injury. 2019;50(2):558–63. https://doi.org/10.1016/j.injury.2018.11.021.
Marasco SF, Martin K, Niggemeyer L, Summerhayes R, Fitzgerald M, Bailey M. Impact of rib fixation on quality of life after major trauma with multiple rib fractures. Injury. 2019;50(1):119–24. https://doi.org/10.1016/j.injury.2018.11.005.
Simmel S, Wurm S, Drisch S, Woltmann A, Coenen M. Prädiktion des Return to Work nach Polytrauma bei Patienten mit einem ISS von 25 und höher [Prediction of Return to Work following Multiple Trauma in Patients with ISS of at least 25]. Rehabilitation (Stuttg). 2020;59(2):95–103. https://doi.org/10.1055/a-0977-6853.
Tipping CJ, Bilish E, Harrold M, Holland AE, Chan T, Hodgson CL. The impact of frailty in critically ill patients after trauma: a prospective observational study. Aust Crit Care. 2020;33(3):228–35. https://doi.org/10.1016/j.aucc.2019.11.001.
Freigang V, Müller K, Ernstberger A, Kaltenstadler M, Bode L, Pfeifer C, et al. Reduced recovery capacity after major trauma in the elderly: results of a prospective multicenter registry-based cohort study. J Clin Med. 2020;9(8):2356. https://doi.org/10.3390/jcm9082356.
Curtis K, Kennedy B, Lam MK, Mitchell RJ, Black D, Jan S, et al. Predictors of 12 month functional outcomes and length of stay of severely injured children in NSW, Australia. A longitudinal multi-centre study. Injury. 2020;51(9):2066–75.
Gabbe BJ, Stewart I, Veitch W, Beck B, Cameron P, Russ M, et al. Long-term outcomes of major trauma with unstable open pelvic fractures: a population-based cohort study. Trauma. 2020;23:111–9. https://doi.org/10.1177/1460408620933203.
van Ditshuizen JC, van Lieshout EMM, van Beeck EF, Verhofstad MHJ, den Hartog D, Dutch Trauma Registry Southwest. Health-related quality of life and return to work 1 year after major trauma from a network perspective. Eur J Trauma Emerg Surg. 2021. https://doi.org/10.1007/s00068-021-01781-2.
Zeelenberg ML, Den Hartog D, Halvachizadeh S, Pape HC, Verhofstad MHJ, Van Lieshout EMM. The impact of upper-extremity injuries on polytrauma patients at a level 1 trauma center. J Shoulder Elbow Surg. 2021. https://doi.org/10.1016/j.jse.2021.10.005.
Vardon-Bounes F, Gracia R, Abaziou T, Crognier L, Seguin T, Labaste F, et al. A study of patients’ quality of life more than 5 years after trauma: a prospective follow-up. Health Qual Life Outcomes. 2021;19(1):18. https://doi.org/10.1186/s12955-020-01652-1.
Castillo-Angeles M, Herrera-Escobar JP, Toppo A, Sanchez SE, Kaafarani HM, Salim A, et al. Patient reported outcomes 6 to 12 months after interpersonal violence: a multicenter cohort study. J Trauma Acute Care Surg. 2021;91(2):260–4. https://doi.org/10.1097/TA.0000000000003272.
Giummarra MJ, Dipnall JF, Gibson G, Beck B, Gabbe BJ. Health status after penetrating major trauma in Victoria, Australia: a registry-based cohort study. Qual Life Res. 2021;30(12):3511–21. https://doi.org/10.1007/s11136-021-02876-4.
Curtis K, Kennedy B, Lam MK, Mitchell RJ, Black D, Jan S, et al. Predictors of 12 month functional outcomes and length of stay of severely injured children in NSW, Australia. A longitudinal multi-centre study. Injury. 2022. https://doi.org/10.1016/j.injury.2021.12.057.
Varni JW, Seid M, Kurtin PS. Reliability and validity of the pediatric quality of life inventory Version4.0 generic core scales in healthy patient populations. Med Care. 2001;39(8):800–12.
Oliveira AL, Marques AS. Outcome measures used in pulmonary rehabilitation in patients with acute exacerbation of chronic obstructive pulmonary disease: a systematic review. Phys Ther. 2018;98(3):191–204. https://doi.org/10.1093/ptj/pzx122.
Spinou A, Fragkos KC, Lee KK, Elston C, Siegert RJ, Loebinger MR, et al. The validity of health-related quality of life questionnaires in bronchiectasis: a systematic review and meta-analysis. Thorax. 2016;71(8):683–94. https://doi.org/10.1136/thoraxjnl-2015-207315.
Swigris JJ, Wilson H, Esser D, Conoscenti CS, Stansen W, Kline Leidy N, et al. Psychometric properties of the St George’s Respiratory Questionnaire in patients with idiopathic pulmonary fibrosis: insights from the INPULSIS trials. BMJ Open Respir Res. 2018;5(1): e000278. https://doi.org/10.1136/bmjresp-2018-000278.
Schuntermann MF. Die internationale Klassifikation der Impairments, Disabilities und Handicaps ICIDH–Ergebnisse und Probleme [International Classification of Impairments, Disabilities and Handicaps ICIDH–results and problems]. Rehabilitation (Stuttg). 1996;35(1):6–13.
Van Ditshuizen JC, Sewalt CA, Palmer CS, Van Lieshout EMM, Verhofstad MHJ, Den Hartog D, Dutch Trauma Registry Southwest. The definition of major trauma using different revisions of the abbreviated injury scale. Scand J Trauma Resusc Emerg Med. 2021;29(1):71. https://doi.org/10.1186/s13049-021-00873-7.
Palmer CS, Gabbe BJ, Cameron PA. Defining major trauma using the 2008 Abbreviated Injury Scale. Injury. 2016;47(1):109–15. https://doi.org/10.1016/j.injury.2015.07.003.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Annesimone Lotfalla, dr. Tim Schepers, dr. Jens Halm, dr. Georgios Giannakópoulos declare that they have no financial or personal relationships with other people or organisations that could inappropriately influence (bias) the work of the four authors. There are no conflicts of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lotfalla, A., Halm, J., Schepers, T. et al. Health-related quality of life after severe trauma and available PROMS: an updated review (part I). Eur J Trauma Emerg Surg 49, 747–761 (2023). https://doi.org/10.1007/s00068-022-02178-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02178-5