Abstract
Purpose
The aim of this review was to evaluate the existing evidence for radiotherapy for brain metastases in breast cancer patients and provide recommendations for the use of radiotherapy for brain metastases and leptomeningeal carcinomatosis.
Materials and methods
For the current review, a PubMed search was conducted including articles from 01/1985 to 05/2023. The search was performed using the following terms: (brain metastases OR leptomeningeal carcinomatosis) AND (breast cancer OR breast) AND (radiotherapy OR ablative radiotherapy OR radiosurgery OR stereotactic OR radiation).
Conclusion and recommendations
Despite the fact that the biological subtype of breast cancer influences both the occurrence and relapse patterns of breast cancer brain metastases (BCBM), for most scenarios, no specific recommendations regarding radiotherapy can be made based on the existing evidence. For a limited number of BCBM (1–4), stereotactic radiosurgery (SRS) or fractionated stereotactic radiotherapy (SRT) is generally recommended irrespective of molecular subtype and concurrent/planned systemic therapy. In patients with 5–10 oligo-brain metastases, these techniques can also be conditionally recommended. For multiple, especially symptomatic BCBM, whole-brain radiotherapy (WBRT), if possible with hippocampal sparing, is recommended. In cases of multiple asymptomatic BCBM (≥ 5), if SRS/SRT is not feasible or in disseminated brain metastases (> 10), postponing WBRT with early reassessment and reevaluation of local treatment options (8–12 weeks) may be discussed if a HER2/Neu-targeting systemic therapy with significant response rates in the central nervous system (CNS) is being used. In symptomatic leptomeningeal carcinomatosis, local radiotherapy (WBRT or local spinal irradiation) should be performed in addition to systemic therapy. In patients with disseminated leptomeningeal carcinomatosis in good clinical condition and with only limited or stable extra-CNS disease, craniospinal irradiation (CSI) may be considered. Data regarding the toxicity of combining systemic therapies with cranial and spinal radiotherapy are sparse. Therefore, no clear recommendations can be given, and each case should be discussed individually in an interdisciplinary setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the leading cause of cancer-related death in women worldwide [1]. However, due to advances in medical treatment, mortality rates have been declining in western countries in the last few decades [1].
Despite good extracranial disease control, physicians are increasingly faced with long-term survivors developing brain metastases or leptomeningeal spread [2]. Patients with breast cancer brain metastases (BCBM) require special attention, as adequate treatment can lead to improved prognosis and long-term survival [3, 4].
The reported incidence of brain metastases in breast cancer patients ranges from 5.1% in patients with newly diagnosed breast cancer to up to 33% in patients with metastatic breast cancer [5,6,7]. Asymptomatic breast cancer patients are not routinely screened for brain metastases with magnetic resonance imaging (MRI). Hence, BCBM are mostly diagnosed due to emerging neurologic symptoms and the actual incidence of BCBM is expected to be even higher [8]. The median overall survival after diagnosis of BCBM ranges from 3 to > 26 months [2]. However, prognosis of patients with BCBM depends on several factors such as biological subtype, age, general condition, number and size of brain metastases, and control of systemic disease [7, 9,10,11].
Traditionally, local therapies such as neurosurgery and radiotherapy were considered as the only treatment option for BCBM due to the limited effectiveness of systemic therapies due to the blood–brain barrier. However, newer systemic therapies such as HER2-targeted therapies have shown promising central nervous system response rates. Nonetheless, local control rates achieved with radiotherapy (with or without resection) remain unrevealed [12, 13].
The appropriate use of radiation techniques such as stereotactic radiosurgery (SRS), fractionated stereotactic radiotherapy (SRT), whole-brain radiotherapy (WBRT), or craniospinal irradiation (CSI) is essential for the oncological treatment of patients and preservation of quality of life. However, with the increasing central nervous system (CNS) response rates of especially HER2-targeted therapies, there is a need to reassess the current literature to make evidence-based recommendations.
Methods
For the current review, a PubMed search was conducted including articles from 01/1985 to 05/2023. The search was performed using the following terms: (brain metastases OR leptomeningeal carcinomatosis) AND (breast cancer OR breast) AND (radiotherapy OR ablative radiotherapy OR radiosurgery OR stereotactic OR radiation). We report results of reviews, randomized trials, and high-quality retrospective studies.
Results
Prognosis of BCBM in dependence of biological subtype
The incidence of BCBM in HER2+ and triple-negative breast cancers (TNBC) is twice as high compared to hormone receptor (HR)-positive HER2− tumors [7]. Furthermore, patients with HR+ breast cancer have a significantly longer median interval until the development of brain metastases [14]. While BCBM in TNBC occur often in case of systemic/extracranial disease progression, in HER2+ tumors, BMBC develop more frequently without evidence of extracranial disease progression. There are several prognostic scores for breast cancer patients with brain metastases. In 2012, Sperduto and Kased et al. [15] published a summary report on the graded prognostic assessment (GPA) for patients with brain metastases, which was updated in 2020. The prognostic factors in breast GPA are tumor subtype, general condition (Karnofsky performance score), age, presence of extracranial disease, and number (1 vs. > 1) of brain metastases (Sperduto, Mesko et al. 2020). Luminal A/B and HER2+ tumors are associated with a significantly better outcome compared to TNBC, and patients with a single brain metastasis had superior survival compared to patients with multiple BCBM [16]. However, there was no further prognostic stratification according to the number of brain metastases for patients with more than one BCBM.
HR+/HER2− tumors can be associated with a better intracranial control rate after brain-directed radiotherapy (WBRT, SRS, or SRT) in comparison to HER2+ and TNBC brain metastases [14]. While HER2+ brain metastases are associated with a lower local control, TNBC are at higher risk of developing distant recurrences in the previously untreated brain [17]. Nevertheless, local treatment including surgery and SRS significantly improves local control rates in both HER2+ and triple-negative BCBM [18].
The microenvironment in the CNS differs from the breast and other extracranial sites [19]. Hence, breast cancer tumor cells that have the ability to cross the brain–blood barrier and proliferate effectively in the CNS need specific characteristics, which are not yet fully understood. Interestingly, in earlier studies, a discordance between primary tumor and BCBM receptors of > 40% was reported (Sperduto, Mesko et al. 2020, [9]). This further impedes treatment decisions based on molecular subtype but also emphasizes the value of local treatment as the biological subtype of BCBM often remains unknown and systemic therapies may not be adapted to the biological subtype of brain metastases (Table 1).
Radiotherapy in BCBM
The randomized studies found in literature on radiotherapy for brain metastases mostly included patients with various tumor entities and were not specifically focused on breast cancer. Even though breast cancer is the second most common primary tumor type in patients with brain metastases [21] and a significant proportion of patients included in the randomized studies had breast cancer (Tables 2 and 3), specific conclusions for the subgroup of breast cancer patients or even for individual molecular subtypes are difficult to draw. Therefore, the following statements and recommendations are based on the general literature for radiotherapy of brain metastases.
Limited brain metastases in breast cancer (≤ 4)
The definition of “limited brain metastases” differs among studies and recommendations (Table 2). Most studies focusing on local therapy in limited brain metastases included patients with up to four metastases.
In randomized trials, surgery followed by WBRT for single brain metastases resulted in an overall survival benefit with fewer local recurrences compared to WBRT alone [39,40,41]. Hence, for many years, surgery has been considered as the preferred treatment option for these patients [42]. However, a subgroup analysis of RTOG 9508 also demonstrated an improvement in overall survival for patients with 1–3 brain metastases and a high GPA when SRS was added to WBRT [23, 43]. Further studies that have applied more modern imaging and treatment techniques have demonstrated that SRS and surgery have similar outcomes [13, 24]. On the other hand, WBRT after surgery or SRS did not show any improvement in quality of life or overall survival [24, 44]. Therefore, SRS has increasingly gained importance.
SRS is less invasive than surgery and generally well tolerated [42, 45]. According to a tumor control probability (TCP) model based on pooled data of > 56 manuscripts, local 1‑year control rates of up to 95% are achievable with SRS only [22]. Meanwhile, based on a randomized phase III trial, the addition of WBRT to SRS does not improve overall survival for patients with 1–3 brain metastases despite a reduced intracranial recurrence rate [12, 25, 46]. Given the reduced neurocognitive function and quality of life and lack of an overall survival benefit, radiosurgery alone should be considered as standard of care for 1–4 brain metastases [24,25,26, 46].
In certain cases, surgery might be necessary for brain metastases, such as for immediate decompression in the presence of symptomatic brain metastases, or for large metastases that are not suitable for SRS/SRT. Surgery may also be recommended for histological verification, particularly after a long recurrence-free interval. After surgery, postoperative radiotherapy is generally indicated to improve local control rates. In a randomized phase III trial, postoperative SRS (or SRT) was shown to have the same overall survival but improved neurocognitive function compared with postoperative WBRT [28, 30]. Therefore, if postoperative radiation is planned, SRS or SRT should be favored whenever possible with respect to tumor volume.
In case of limited brain metastases, SRS/SRT can be generally be recommended regardless of molecular subtype and systemic therapy (see sections “Combination of radiotherapy with systemic therapy” and “Recommendations”). However, for SRS/SRT in TNBC, a higher intracranial distant recurrence rate should be taken into account, indicating the necessity of close follow-up.
Local therapy of multiple (≥ 5) brain metastases
For patients with multiple (≥ 5) brain metastases, WBRT has been the standard of care over the past decades [47]. In historical trials, it demonstrated a reduction of neurological symptoms and complications as well as an improvement in PFS compared to best supportive care [48]. However, WBRT also carries the risk of significant additional neurocognitive impairment during the remaining lifetime [48]. Up to two thirds of patients undergoing WBRT suffer from neurocognitive deterioration 2–6 months after treatment [49]. Although associated with less neurocognitive impairment, the value of using SRS in patients with more than four metastases has been discussed controversially [34, 48]. Recently, however, studies have demonstrated equivalence in overall survival (OS) when comparing patients with 2–4 and multiple (5–10) metastases after SRS [50]. Li et al. compared SRS to WBRT in a randomized manner including 72 patients with 4–15 brain metastases [37]. Even though SRS was associated with significantly worse intracranial distant control, no difference in OS and inferior cognitive function after WBRT was observed. A Dutch randomized phase III trial comparing SRS to WBRT in 4–10 BM was closed early due to poor accrual [51]. Observational studies suggest that patients with 5–10 metastases have similar outcomes compared to patients with 2–4 metastases after SRS [32, 33]. The treatment-related toxicity was low, with neurocognitive function being similar between the groups when cumulative tumor volume was < 15 ml [52]. In a retrospective multicenter analysis of 471 patients with 1–10 BCBM, the number of BCBM and the use of WBRT had no impact on OS [38].
Thus, SRS can be recommended as an efficient and safe treatment option even for multiple BCBM. Even in the case of in-field recurrence after prior SRS, a second course of SRS is often feasible with acceptable toxicity, and can be considered as a salvage treatment option for selected patients with good performance status and a time interval of > 12 months to initial SRS [53, 54].
In selected cases of HER2+ disseminated brain metastases and/or if SRS/SRT is technically infeasible, WBRT can be deferred with early follow-up and reevaluation of local treatment (see sections “Combination of radiotherapy with systemic therapy” and “Recommendations”).
Focal radiotherapy and craniospinal axis irradiation in leptomeningeal carcinomatosis
Leptomeningeal tumor involvement represents a very advanced tumor stage with numerous complications [55]. In recent years, the incidence of leptomeningeal carcinomatosis (LC) in breast cancer has increased sharply, mainly due to improved treatment and thus a prolonged survival of patients [56]. Due to the difficulty of diagnosis, it is likely that the reported incidence of approximately 5% in breast cancer patients is an underestimation [57]. Compared with parenchymal involvement of the central nervous system, patients with leptomeningeal carcinomatosis generally have a worse prognosis [58]. Median overall survival is 4–6 weeks when untreated and reportedly up to 30.3 weeks when treated. However, the treated and untreated patients are difficult to compare and selection bias may play an important role [56, 59, 60]. Diffuse leptomeningeal spread should be differentiated from nodular involvement, which may occur more frequently after resection of brain metastases treated with postoperative SRS/SRT compared to WBRT and is more common in patients with BCBM compared to other entities [61, 62]. It remains uncertain whether the two types of leptomeningeal carcinomatosis require distinct treatment approaches, and whether the recently proposed new approach of preoperative stereotactic radiosurgery/stereotactic radiation therapy can effectively prevent the occurrence of nodular leptomeningeal carcinomatosis after surgery. Several ongoing trials aim to address these questions [63].
The work-up and treatment options for leptomeningeal carcinomatosis are summarized in the EANO-ESMO guideline on leptomeningeal metastasis [64].
To date, despite the existence of guidelines, treatment concepts still vary widely between centers and physicians [65], as scientific evidence is sparse [56, 66]. Possible treatment options for leptomeningeal carcinomatosis include intrathecal chemotherapy, radiotherapy, systemic therapy, and best supportive care.
Intrathecal chemotherapy is a controversial therapeutic approach for leptomeningeal carcinomatosis [55, 67,68,69] and is associated with severe side effects. The evidence regarding oncologic benefit is weak and based only on retrospective observational studies from more than 20 years ago, and is considered controversial in more recent studies, particularly with regard to OS [56, 59, 66, 70]. In contrast, systemic therapy has been shown to improve overall survival from 2 to 6 months [66, 70]. Recent data from small phase I/II studies suggest that the use of intrathecal trastuzumab potentially improves the outcomes for HER2-positive breast cancer patients with leptomeningeal disease [71, 72].
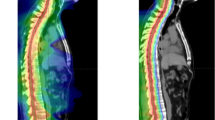
Another therapeutic option is radiotherapy [55]), which can be applied as involved-field irradiation (WBRT vs. spinal IFRT) to improve neurological systems and prevent complication, or as craniospinal irradiation (CSI), which additionally aims to improve the oncologic outcome by eradicating tumor cells in the entire craniospinal axis [73]. For selected patients with isolated nodular lesions, SRS/SRT may represent an option [74].
In 2022, the results of a randomized phase II trial (n = 62 patients) were published evaluating the oncological benefit of CSI [75]. The study enrolled patients with leptomeningeal carcinomatosis from solid tumors. A total of 63 patients were enrolled, of whom 43% had breast cancer. They were randomized 2:1 to receive either proton CSI (pCSI) or photon involved-field radiotherapy (IFRT). The primary endpoint was central nervous system progression-free survival (CNS PFS), with secondary endpoints including overall survival and treatment-related adverse events (TAEs). The results showed significant benefits regarding CNS PFS and OS after pCSI compared to IFRT, with no increase in serious TAEs. The findings of this trial reveal the potential of CSI in patients with leptomeningeal metastasis. Nevertheless, it should be noted that proton therapy for CSI is very rarely available, and the more widely available option of photon therapy results in a higher dose exposure to the bone marrow and other organs at risk (Table 4).
Irradiation techniques and follow-up
The optimal use of SRT, SRS, and WBRT is discussed in detail in the EANO-ESTRO and ASTRO guidelines as well as in the HyTEC recommendations for the treatment of brain metastases [22, 76, 77].
The question of the optimal fractionation regimen is dependent on the size and location of the metastases/resection cavity. For smaller lesions (≤ 20–25 mm), SRS is usually performed with a dose ranging between 18 and 24 Gy prescribed to the 60–80% isodose. In larger metastases (> 20–25 mm) or in critical locations, SRT is typically given in 3–7 fractions with a total dose of 27–35 Gy prescribed to the 60–80% isodose.
Depending on the irradiation technique and the location of the metastases, prescription and normalization can differ (e.g., Gamma Knife with prescription to lower isodoses).
The total dose of WBRT is typically 30 Gy given in 10 fractions (prescribed to the median dose). In frail patients, a dose regimen of 20 in 5 fractions can be used. The use of N‑methyl-D-aspartate (NMDA) receptor antagonists such as memantine in combination with hippocampal avoidance (HA) has been shown to improve cognitive function, particularly memory, in patients undergoing WBRT [78]. Several studies have demonstrated that HA during WBRT with or without memantine or donepezil (acetylcholinesterase selective inhibitor) can effectively reduce the risk of cognitive decline in patients without compromising tumor control [79,80,81,82]. It should be noted that in Germany, the use of donepezil and memantine is off label and patients need to be informed about potential side effects such as blurred vision, dizziness, and headache (Table 5).
After SRS/SRT of BCBM, regular follow-up by a radiation oncologist with additional MRI (e.g., every 3 months) is recommended, whereas follow-up after WBRT may be guided by clinical factors. For diagnosis and treatment of radionecrosis, we refer to the DEGRO practical guideline for central nervous system radiation necrosis [87].
Combination of radiotherapy with systemic therapy
There are two essential questions that arise in the context of combining radiotherapy and systemic therapy for BCBM:
1) Are there concerns regarding increased toxicity when combining these treatments?
As most patients with BCBM are treated with systemic therapy and interruption of systemic therapy may be critical due to extracranial metastatic burden, the question of the safety of concurrent treatment combination is highly relevant. The evidence regarding toxicity of combined systemic therapy and CNS radiotherapy is sparse. Whereas the combination of endocrine therapy and SRS/WBRT is considered as safe [88]), preclinical studies have shown that the HER2-targeted antibody–drug conjugate trastuzumab emtansine (T‑DM1) may increase radiosensitivity. In a recent study involving 98 patients, Lebow et al. [89] observed that administering antibody drug–conjugates (ADC; specifically trastuzumab emtansine, trastuzumab deruxtecan [T-DXd], and sacituzumab govitecan [SG]) concurrently with stereotactic radiotherapy (either up to 7 days before or within 21 days after ADC treatment) resulted in a higher incidence of grade 4–5 higher radiation necrosis compared to non-concurrent treatments (7.1% vs. 0.7%). For previously irradiated lesions the 24-month risk of severe radionecrosis was 42.0% with and 9.4% without concurrent ADC. In univariable analysis, T‑DM1 and T‑DXd were associated with an increased risk of symptomatic radiation necrosis compared with no concurrent ADC. For the subgroup receiving SG, there was only a trend (HR 5.18, ranging from 0.64 to 42.11, p = 0.12) [90]. However, this subgroup was the smallest and had the broadest confidence interval. The limitations of this study include the small patient cohort, its retrospective nature, and the difficulty in distinguishing between local treatment failure and radionecrosis. While an increased risk for radiation necrosis has already been described for the combination of SRS and T‑DM1, further data are needed for T‑TXd and SG.
In other retrospective studies, SRS was well tolerated alongside CDK4/6 inhibitors [91]. Similar reports exist for immunotherapy and PARP inhibitors administered in combination with SRS [92, 93]. Data regarding the combination of trastuzumab and pertuzumab with SRS/SRT are sparse, but according to reviews and census recommendations, the combination with stereotactic radiotherapy is generally considered as safe [94, 95].
In a systematic review by Kroeze et al. investigating the toxicity of targeted therapies and stereotactic radiotherapy, high-dose SRT concurrent with targeted therapy (TT) was characterized by a favorable safety profile, regardless of whether TT was interrupted during and around SRT [96]. A consensus recommendation from the ESTRO-EORTC OligoCare Consortium published in 2023 focused on extracranial stereotactic body radiotherapy (SBRT) and systemic therapy. Consensus was reached that trastuzumab and pertuzumab can be administered on the same day as SBRT without a treatment break or dose reduction, whereas no such consensus was reached for T‑DM1. For T‑DM1, CDK4/6 inhibitors, HER2 inhibitors, and PARP inhibitors, there was consensus that SBRT can be performed without dose reduction; however, there was no consensus regarding interruption of systemic therapy during SBRT. These recommendations should not be uncritically applied to SRS/SRT for BCBM, since pathomechanisms of toxicity may differ [94]. Due to the lack of reliable data, the decision on whether systemic therapy needs to be interrupted during radiotherapy should be made individually on a case-by-case basis within an interdisciplinary board.
2) Can local therapy be postponed when systemic therapy with relevant intracranial response rates is given?
Local interventions such as resection and radiation are the standard of care for BCBM, but systemic therapies are increasingly effective in the treatment of brain metastases. In patients with HER2+ BCBM, relevant intracranial response rates have been reported for antibody–drug conjugates like T‑DM1 and T‑DXd as well as kinase inhibitor-containing regimens such as tucatinib/capecitabine/trastuzumab, neratinib/capecitabine, and lapatinib/capecitabine [97, 98]. The intracranial response rates in some of the randomized studies are reported to be > 60% in treatment-naïve HER2+ BCBM. The randomized controlled HER2CLIMB trial demonstrated an improvement in overall survival in the predefined subgroup of 291 patients with BCBM with the addition of tucatinib to trastuzumab/capecitabine. In this trial, 174 patients were considered to have active brain metastases; however, only 66 of these patients had previously untreated BCBM (Table 6).
Hence, when interpreting these data, it is crucial to consider the inclusion criteria of the underlying trials. While most trials enrolled patients with small asymptomatic brain metastases not requiring immediate local therapy, only a minority allowed for active brain metastases that were either untreated or progressed after prior local therapy. Furthermore, high intracranial response rates must be interpreted in the context of progression-free and overall survival as well as toxicity. Trials comparing systemic therapy only vs. systemic therapy with SRS/SRT are missing so far in HER2+ BCBM. Data regarding the treatment of HER2− (luminal or TNBC) BCBM are even more sparse. For the CDK4/6 inhibitor abemaciclib, an intracranial response (defined as complete or partial response) was observed in 5.2% of patients, median intracranial PFS was 4.9 months [108]. According to a small phase II trial, brain metastases in primary tumors with a PD-L1 of ≥ 1% showed in 29.7% a response to pembrolizumab [109].
It should be noted that local control rates of SRS with up to > 90% after 2 years, are higher than the response rates in any of the existing trials on systemic therapy for BCBM. Nevertheless, intracranial control is an issue with SRS/SRT, as 30–40% of patients experience distant intracranial progression within 1 year. Furthermore, it needs to be considered, as mentioned earlier, that the receptors in brain metastases differ from the primary tumor in more than 40% of patients. Given the high risk of complications in case of progressive brain metastases and the low rate of toxicity of SRS/SRT, local therapy is generally recommended in limited BCBM regardless of molecular subtype and systemic therapy. If SRS/SRT is technically infeasible, in patients with multiple (≥ 5) asymptomatic HER2+ BCBM (e.g., due to prior irradiation), systemic therapy combined with early reassessment of response (after 8–12 weeks) and reevaluation of radiotherapy can be considered after interdisciplinary discussion to defer or avoid WBRT. Similarly, in case of asymptomatic disseminated brain metastases, systemic therapy combined with early reassessment can be considered after interdisciplinary discussion. However, in case of systemic therapy only, patients need to be informed about the risk of progressive intracranial disease with subsequent complications and should be actively involved in the decision.
Recommendations
-
The biological subtype and breast cancer-specific GPAs should be considered for evaluation of prognosis in patients with BCBM.
-
Limited brain metastases (n = ≤ 4):
-
Local therapy including SRS/SRT is generally recommended irrespective of molecular subtype and systemic therapy.
-
In case of limited intact BCBM (n = ≤ 4), SRS/SRT should be used.
-
After resection with a limited number of remaining BCBM (n = ≤ 4), SRS/SRT to the resection cavity should be used as postoperative treatment with additional SRS/SRT of the intact BCBM.
-
-
Multiple brain metastases:
-
SRS should be considered in case of n = 5–10 intact BCBM (cumulative volume < 15 ml); alternatively, WBRT can be applied.
-
After resection of BCBM and limited further BCBM (n = 5–10 and < 15 ml), SRS/SRT to the resection cavity and remaining intact BCBM is a possible option. Alternatively, WBRT can be applied.
-
In disseminated brain metastases (n = > 10), WBRT is generally recommended.
-
After interdisciplinary discussion, in cases of asymptomatic disseminated brain metastases (n = > 10) or in multiple BCBM if SRS/SRT is not feasible, WBRT can be postponed with early reassessment and reevaluation of local treatment options (8–12 weeks) if HER2-targeted systemic therapy with significant response rates in the CNS (tucatinib/trastuzumab/capecitabine, trastuzumab deruxtecan) is being used.
-
-
Leptomeningeal carcinomatosis:
-
In symptomatic leptomeningeal carcinomatosis, local radiotherapy (WBRT/involved-field SRS/SRT or local spinal irradiation) should be administered to symptomatic lesions in addition to systemic therapy.
-
In case of patients with disseminated leptomeningeal carcinomatosis in good clinical condition and with limited, stable extra-CNS disease, CSI may be considered.
-
-
Technique:
-
The decision on the optimal fractionation regimen is dependent on the size and location of the metastases/resection cavity.
-
In case of WBRT, hippocampal avoidance should be considered, especially for patients with a good prognosis according to GPA score.
-
Administration of memantine or donepezil may be considered with WBRT (off-label use in Germany).
-
-
Concurrent systemic therapy:
-
There is a general lack of data regarding the combination of systemic therapy and SRS/SRT for brain metastases.
-
Each case should be discussed individually in an interdisciplinary setting based on the type of systemic therapy, size and location of the metastases, as well as planned dose and fractionation.
-
Particular caution should be taken when administering SRS/SRT concurrently (≤ 7 days before or ≤ 21 days after) with antibody drug–conjugates.
-
Conclusion
Due to the increasing effectiveness of systemic therapy in improving long-term survival in metastatic breast cancer, achieving local control in the CNS has become a crucial treatment goal. SRS and fractionated SRT have demonstrated excellent control rates and low toxicity rates for cases with a limited number of brain metastases, regardless of molecular subtype and systemic therapy, and should therefore be recommended. For patients with leptomeningeal carcinomatosis, local radiation can significantly improve symptoms. In cases with favorable prognostic factors, CSI may also be performed to improve oncological outcomes.
References
DeSantis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A (2015) International Variation in Female Breast Cancer Incidence and Mortality Rates. Cancer Epidemiol Biomarkers Prev 24(10):1495–1506
Sperduto PW, Mesko S, Li J, Cagney D, Aizer A, Lin NU, Nesbit E, Kruser TJ, Chan J, Braunstein S, Lee J, Kirkpatrick JP, Breen W, Brown PD, Shi D, Shih HA, Soliman H, Sahgal A, Shanley R, Sperduto W, Lou E, Everett A, Boggs DH, Masucci L, Roberge D, Remick J, Plichta K, Buatti JM, Jain S, Gaspar LE, Wu CC, Wang TJC, Bryant J, Chuong M, Yu J, Chiang V, Nakano T, Aoyama H, Mehta MP (2020) Beyond an Updated Graded Prognostic Assessment (Breast GPA): A Prognostic Index and Trends in Treatment and Survival in Breast Cancer Brain Metastases From 1985 to Today. Int J Radiat Oncol Biol Phys 107(2):334–343
Sperduto PW, Mesko S, Li J, Cagney D, Aizer A, Lin NU, Nesbit E, Kruser TJ, Chan J, Braunstein S, Lee J, Kirkpatrick JP, Breen W, Brown PD, Shi D, Shih HA, Soliman H, Sahgal A, Shanley R, Sperduto WA, Lou E, Everett A, Boggs DH, Masucci L, Roberge D, Remick J, Plichta K, Buatti JM, Jain S, Gaspar LE, Wu CC, Wang TJC, Bryant J, Chuong M, An Y, Chiang V, Nakano T, Aoyama H, Mehta MP (2020) Survival in Patients With Brain Metastases: Summary Report on the Updated Diagnosis-Specific Graded Prognostic Assessment and Definition of the Eligibility Quotient. J Clin Oncol 38(32):3773–3784
Palmer, J. D., B. G. Klamer, K. V. Ballman, P. D. Brown, J. H. Cerhan, S. K. Anderson, X. W. Carrero, A. C. Whitton, J. Greenspoon, I. F. Parney, N. N. I. Laack, J. B. Ashman, J. P. Bahary, C. G. Hadjipanayis, J. J. Urbanic, F. G. Barker, 2nd, E. Farace, D. Khuntia, C. Giannini, J. C. Buckner, E. Galanis and D. Roberge (2022). “Association of Long-term Outcomes With Stereotactic Radiosurgery vs Whole-Brain Radiotherapy for Resected Brain Metastasis: A Secondary Analysis of The N107C/CEC.3 (Alliance for Clinical Trials in Oncology/Canadian Cancer Trials Group) Randomized Clinical Trial.” JAMA Oncol 8(12): 1809–1815.
Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE (2004) Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 22(14):2865–2872
Darlix A, Louvel G, Fraisse J, Jacot W, Brain E, Debled M, Mouret-Reynier MA, Goncalves A, Dalenc F, Delaloge S, Campone M, Augereau P, Ferrero JM, Levy C, Fumet JD, Lecouillard I, Cottu P, Petit T, Uwer L, Jouannaud C, Leheurteur M, Dieras V, Robain M, Chevrot M, Pasquier D, Bachelot T (2019) Impact of breast cancer molecular subtypes on the incidence, kinetics and prognosis of central nervous system metastases in a large multicentre real-life cohort. Br J Cancer 121(12):991–1000
Kuksis M, Gao Y, Tran W, Hoey C, Kiss A, Komorowski AS, Dhaliwal AJ, Sahgal A, Das S, Chan KK, Jerzak KJ (2021) The incidence of brain metastases among patients with metastatic breast cancer: a systematic review and meta-analysis. Neuro Oncol 23(6):894–904
Martin, A. M., D. N. Cagney, P. J. Catalano, L. E. Warren, J. R. Bellon, R. S. Punglia, E. B. Claus, E. Q. Lee, P. Y. Wen, D. A. Haas-Kogan, B. M. Alexander, N. U. Lin and A. A. Aizer (2017). “Brain Metastases in Newly Diagnosed Breast Cancer: A Population-Based Study.” JAMA Oncol 3(8): 1069–1077.
Bailleux C, Eberst L, Bachelot T (2021) Treatment strategies for breast cancer brain metastases. Br J Cancer 124(1):142–155
Mills MN, Figura NB, Arrington JA, Yu HM, Etame AB, Vogelbaum MA, Soliman H, Czerniecki BJ, Forsyth PA, Han HS, Ahmed KA (2020) Management of brain metastases in breast cancer: a review of current practices and emerging treatments. Breast Cancer Res Treat 180(2):279–300
Rostami R, Mittal S, Rostami P, Tavassoli F, Jabbari B (2016) Brain metastasis in breast cancer: a comprehensive literature review. J Neurooncol 127(3):407–414
Aoyama, H., H. Shirato, M. Tago, K. Nakagawa, T. Toyoda, K. Hatano, M. Kenjyo, N. Oya, S. Hirota, H. Shioura, E. Kunieda, T. Inomata, K. Hayakawa, N. Katoh and G. Kobashi (2006). “Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial.” JAMA 295(21): 2483–2491.
Churilla, T. M., I. H. Chowdhury, E. Handorf, L. Collette, S. Collette, Y. Dong, B. M. Alexander, M. Kocher, R. Soffietti, E. B. Claus and S. E. Weiss (2019). “Comparison of Local Control of Brain Metastases With Stereotactic Radiosurgery vs Surgical Resection: A Secondary Analysis of a Randomized Clinical Trial.” JAMA Oncol 5(2): 243–247.
Kim JS, Kim K, Jung W, Shin KH, Im SA, Kim HJ, Kim YB, Chang JS, Kim JH, Choi DH, Park YH, Kim DY, Kim TH, Choi BO, Lee SW, Kim S, Kwon J, Kang KM, Chung WK, Kim KS, Yoon WS, Cha J, Oh YK, Kim IA (2021) New brain metastases after whole-brain radiotherapy of initial brain metastases in breast cancer patients: the significance of molecular subtypes (KROG 16–12). Breast Cancer Res Treat 186(2):453–462
Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, Luo X, Sneed PK, Chao ST, Weil RJ, Suh J, Bhatt A, Jensen AW, Brown PD, Shih HA, Kirkpatrick J, Gaspar LE, Fiveash JB, Chiang V, Knisely JP, Sperduto CM, Lin N, Mehta M (2012) Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol 30(4):419–425
Hwang KT, Kim J, Jung J, Chang JH, Chai YJ, Oh SW, Oh S, Kim YA, Park SB, Hwang KR (2019) Impact of Breast Cancer Subtypes on Prognosis of Women with Operable Invasive Breast Cancer: A Population-based Study Using SEER Database. Clin Cancer Res 25(6):1970–1979
Cagney DN, Lamba N, Montoya S, Li P, Besse L, Martin AM, Brigell RH, Catalano PJ, Brown PD, Leone JP, Tanguturi SK, Haas-Kogan DA, Alexander BM, Lin NU, Aizer AA (2019) Breast cancer subtype and intracranial recurrence patterns after brain-directed radiation for brain metastases. Breast Cancer Res Treat 176(1):171–179
Chong JU, Ahn SG, Lee HM, Park JT, Lee SA, Park S, Jeong J, Kim SI (2015) Local control of brain metastasis: treatment outcome of focal brain treatments in relation to subtypes. J Breast Cancer 18(1):29–35
Cacho-Diaz B, Garcia-Botello DR, Wegman-Ostrosky T, Reyes-Soto G, Ortiz-Sanchez E, Herrera-Montalvo LA (2020) Tumor microenvironment differences between primary tumor and brain metastases. J Transl Med 18(1):1
Kim JS, Kim K, Jung W, Shin KH, Im S-A, Kim H-J, Kim YB, Chang JS, Choi DH, Park YH, Kim DY, Kim TH, Choi BO, Lee S-W, Kim S, Kwon J, Kang KM, Chung W-K, Kim KS, Nam JH, Yoon WS, Kim JH, Cha J, Oh YK, Kim IA (2020) Survival outcomes of breast cancer patients with brain metastases: A multicenter retrospective study in Korea (KROG 16–12). Breast 49:41–47. ISSN 0960-9776, https://doi.org/10.1016/j.breast.2019.10.007
Tse VM, Ph D (2022) https://emedicine.medscape.com/article/1157902-overview#a8
Redmond KJ, Gui C, Benedict S, Milano MT, Grimm J, Vargo JA, Soltys SG, Yorke E, Jackson A, El Naqa I, Marks LB, Xue J, Heron DE, Kleinberg LR (2021) Tumor Control Probability of Radiosurgery and Fractionated Stereotactic Radiosurgery for Brain Metastases. Int J Radiat Oncol Biol Phys 110(1):53–67
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363(9422):1665–1672
Kocher M, Soffietti R, Abacioglu U, Villà S, Fauchon F, Baumert BG, Fariselli L, Tzuk-Shina T, Kortmann RD, Carrie C, Hassel MB, Kouri M, Valeinis E, van den Berge D, Collette S, Collette L, Mueller RP (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol 29(2):134–141
Brown, P. D., K. Jaeckle, K. V. Ballman, E. Farace, J. H. Cerhan, S. K. Anderson, X. W. Carrero, F. G. Barker, R. Deming, S. H. Burri, C. Ménard, C. Chung, V. W. Stieber, B. E. Pollock, E. Galanis, J. C. Buckner and A. L. Asher (2016). “Effect of Radiosurgery Alone vs Radiosurgery With Whole Brain Radiation Therapy on Cognitive Function in Patients With 1 to 3 Brain Metastases: A Randomized Clinical Trial.” JAMA 316(4): 401–409.
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10(11):1037–1044
Wijetunga A, Jayamanne D, Cook R, Parkinson J, Little N, Curtis J, Brown C, Back M (2020) Hypofractionated adjuvant surgical cavity radiotherapy following resection of limited brain metastasis. Clin Neurosci A 82:155–161. ISSN 0967-5868, https://doi.org/10.1016/j.jocn.2020.10.041
Kayama, T., S. Sato, K. Sakurada, J. Mizusawa, R. Nishikawa, Y. Narita, M. Sumi, Y. Miyakita, T. Kumabe, Y. Sonoda, Y. Arakawa, S. Miyamoto, T. Beppu, K. Sugiyama, H. Nakamura, M. Nagane, Y. Nakasu, N. Hashimoto, M. Terasaki, A. Matsumura, E. Ishikawa, T. Wakabayashi, Y. Iwadate, S. Ohue, H. Kobayashi, M. Kinoshita, K. Asano, A. Mukasa, K. Tanaka, A. Asai, T. Abe, Y. Muragaki, K. Iwasaki, T. Aoki, T. Watanabe, H. Sasaki, S. Izumoto, M. Mizoguchi, T. Matsuo, H. Takeshima, M. Hayashi, H. Jokura, T. Mizowaki, E. Shimizu, H. Shirato, M. Tago, H. Katayama, H. Fukuda, S. Shibui and J. C. O. Group (2018). “Effects of Surgery With Salvage Stereotactic Radiosurgery Versus Surgery With Whole-Brain Radiation Therapy in Patients With One to Four Brain Metastases (JCOG0504): A Phase III, Noninferiority, Randomized Controlled Trial.” J Clin Oncol: JCO2018786186.
Mahajan A, Ahmed S, McAleer MF, Weinberg JS, Li J, Brown P, Settle S, Prabhu SS, Lang FF, Levine N, McGovern S, Sulman E, McCutcheon IE, Azeem S, Cahill D, Tatsui C, Heimberger AB, Ferguson S, Ghia A, Demonte F, Raza S, Guha-Thakurta N, Yang J, Sawaya R, Hess KR, Rao G (2017) Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol 18(8):1040–1048. https://doi.org/10.1016/S1470-2045(17)30414-X. Epub 2017 Jul 4. Erratum in: Lancet Oncol 2017 Aug, 18(8):e433. Erratum in: Lancet Oncol 2017 Sep, 18(9):e510. PMID: 28687375; PMCID: PMC5560102
Brown PD, Ballman KV, Cerhan JH, Anderson SK, Carrero XW, Whitton AC, Greenspoon J, Parney IF, Laack NNI, Ashman JB, Bahary JP, Hadjipanayis CG, Urbanic JJ, Barker FG, Farace E, Khuntia D, Giannini C, Buckner JC, Galanis E, Roberge D (2017) Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC·3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 18(8):1049–1060
Eitz KA, Lo SS, Soliman H, Sahgal A, Theriault A, Pinkham MB, Foote MC, Song AJ, Shi W, Redmond KJ, Gui C, Kumar AMS, Machtay M, Meyer B, Combs SE (2020) Multi-institutional Analysis of Prognostic Factors and Outcomes After Hypofractionated Stereotactic Radiotherapy to the Resection Cavity in Patients With Brain Metastases. JAMA Oncol 6(12):1901–1909. https://doi.org/10.1001/jamaoncol.2020.4630. Erratum in: JAMA Oncol 2020 Dec 1, 6(12):1985. Erratum in: JAMA Oncol 2023 Dec 28, PMID: 33057566, PMCID: PMC7563677
Chang, W. S., H. Y. Kim, J. W. Chang, Y. G. Park and J. H. Chang (2010). “Analysis of radiosurgical results in patients with brain metastases according to the number of brain lesions: is stereotactic radiosurgery effective for multiple brain metastases?” J Neurosurg 113 Suppl: 73–78.
Yamamoto M, Serizawa T, Shuto T, Akabane A, Higuchi Y, Kawagishi J, Yamanaka K, Sato Y, Jokura H, Yomo S, Nagano O, Kenai H, Moriki A, Suzuki S, Kida Y, Iwai Y, Hayashi M, Onishi H, Gondo M, Sato M, Akimitsu T, Kubo K, Kikuchi Y, Shibasaki T, Goto T, Takanashi M, Mori Y, Takakura K, Saeki N, Kunieda E, Aoyama H, Momoshima S, Tsuchiya K (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15(4):387–395
Wilson TG, Robinson T, MacFarlane C, Spencer T, Herbert C, Wade L, Reed H, Braybrooke JP (2020) Treating Brain Metastases from Breast Cancer: Outcomes after Stereotactic Radiosurgery. Clin Oncol (r Coll Radiol) 32(6):390–396
El Shafie RA, Celik A, Weber D, Schmitt D, Lang K, König L, Bernhardt D, Höne S, Forster T, von Nettelbladt B, Adeberg S, Debus J, Rieken S (2020) A matched-pair analysis comparing stereotactic radiosurgery with whole-brain radiotherapy for patients with multiple brain metastases. J Neurooncol 147(3):607–618. https://doi.org/10.1007/s11060-020-03447-2. Epub 2020 Apr 1. PMID: 32239433
Hartgerink D, Bruynzeel A, Eekers D, Swinnen A, Hurkmans C, Wiggenraad R, Swaak-Kragten A, Dieleman E, van der Toorn PP, Oei B, van Veelen L, Verhoeff J, Lagerwaard F, de Ruysscher D, Lambin P, Zindler J (2021) A Dutch phase III randomized multicenter trial: whole brain radiotherapy versus stereotactic radiotherapy for 4–10 brain metastases. Neurooncol Adv 3(1):vdab21
J. Li, E. B. L., Y. Wang, N. Guha-Thakurta, M. F. McAleer, S. H. Settle Jr, D. N. Yeboa, A. J. Ghia, S. L. McGovern, C. Chung, K. D. Woodhouse, T. M. Briere, C. M. Sullaway, D. D. Liu, G. Rao, E. L. Chang, A. Mahajan, E. P. Sulman, P. D. Brown, and J. S. Wefel (2020). “Stereotactic radiosurgery versus whole-brain radiation therapy for patients with 4–15 brain metastases: A phase III randomized controlled trial.”
Kim JS, Kim K, Jung W, Shin KH, Im SA, Kim HJ, Kim YB, Chang JS, Kim JH, Choi DH, Park YH, Kim DY, Kim TH, Choi BO, Lee SW, Kim S, Kwon J, Kang KM, Chung WK, Kim KS, Yoon WS, Kim JH, Cha J, Oh YK, Kim IA (2023) Comparison of initial and sequential salvage brain-directed treatment in patients with 1–4 vs. 5–10 brain metastases from breast cancer (KROG 16–12). Breast Cancer Res Treat 200(1):37–45
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322(8):494–500. https://doi.org/10.1056/NEJM199002223220802. PMID: 2405271
Vecht CJ, Haaxma-Reiche H, Noordijk EM, Padberg GW, Voormolen JH, Hoekstra FH, Tans JT, Lambooij N, Metsaars JA, Wattendorff AR et al (1993) Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol 33(6):583–590. https://doi.org/10.1002/ana.410330605. PMID: 8498838
Mintz AH, Kestle J, Rathbone MP, Gaspar L, Hugenholtz H, Fisher B, Duncan G, Skingley P, Foster G, Levine M (1996) A randomized trial to assess the efficacy of surgery in addition to radiotherapy in patients with a single cerebral metastasis. Cancer 78(7):1470–1476. https://doi.org/10.1002/(sici)1097-0142(19961001)78:71470::aid-cncr143.0.co;2-x. PMID: 8839553
Soffietti R, Abacioglu U, Baumert B, Combs SE, Kinhult S, Kros JM, Marosi C, Metellus P, Radbruch A, Villa Freixa SS, Brada M, Carapella CM, Preusser M, Le Rhun E, Rudà R, Tonn JC, Weber DC, Weller M (2017) Diagnosis and treatment of brain metastases from solid tumors: guidelines from the European Association of Neuro-Oncology (EANO). Neuro Oncol 19(2):162–174
Sperduto PW, Shanley R, Luo X, Andrews D, Werner-Wasik M, Valicenti R, Bahary JP, Souhami L, Won M, Mehta M (2014) Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1–3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int J Radiat Oncol Biol Phys 90(3):526–531
Patchell RA, Tibbs PA, Regine WF, Dempsey RJ, Mohiuddin M, Kryscio RJ, Markesbery WR, Foon KA, Young B (1998) Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA 280(17):1485–1489. https://doi.org/10.1001/jama.280.17.1485. PMID: 9809728
Specht HM, Combs SE (2016) Stereotactic radiosurgery of brain metastases. J Neurosurg Sci 60(3):357–366
Tsao M, Xu W, Sahgal A (2012) A meta-analysis evaluating stereotactic radiosurgery, whole-brain radiotherapy, or both for patients presenting with a limited number of brain metastases. Cancer 118(9):2486–2493
O’Sullivan CC, Davarpanah NN, Abraham J, Bates SE (2017) Current challenges in the management of breast cancer brain metastases. Semin Oncol 44(2):85–100
Lin X, DeAngelis LM (2015) Treatment of Brain Metastases. J Clin Oncol 33(30):3475–3484
Pinkham MB, Sanghera P, Wall GK, Dawson BD, Whitfield GA (2015) Neurocognitive Effects Following Cranial Irradiation for Brain Metastases. Clin Oncol (r Coll Radiol) 27(11):630–639
Li, J., E. B. Ludmir, Y. Wang, N. Guha-Thakurta, M. F. McAleer, S. H. S. Jr., D. N. Yeboa, A. J. Ghia, S. L. McGovern, C. Chung, K. D. Woodhouse, T. M. Briere, C. M. Sullaway, D. D. Liu, G. Rao, E. L. Chang, A. Mahajan, E. P. Sulman, P. D. Brown and J. S. Wefel (NOVEMBER 01, 2020). “Stereotactic Radiosurgery versus Whole-brain Radiation Therapy for Patients with 4–15 Brain Metastases: A Phase III Randomized Controlled Trial.” VOLUME 108(ISSUE 3): S21–S22.
Hartgerink D, Swinnen A, Roberge D, Nichol A, Zygmanski P, Yin FF, Deblois F, Hurkmans C, Ong CL, Bruynzeel A, Aizer A, Fiveash J, Kirckpatrick J, Guckenberger M, Andratschke N, de Ruysscher D, Popple R, Zindler J (2019) LINAC based stereotactic radiosurgery for multiple brain metastases: guidance for clinical implementation. Acta Oncol 58(9):1275–1282
Yamamoto M, Serizawa T, Higuchi Y, Sato Y, Kawagishi J, Yamanaka K, Shuto T, Akabane A, Jokura H, Yomo S, Nagano O, Aoyama H (2017) A Multi-institutional Prospective Observational Study of Stereotactic Radiosurgery for Patients With Multiple Brain Metastases (JLGK0901 Study Update): Irradiation-related Complications and Long-term Maintenance of Mini-Mental State Examination Scores. Int J Radiat Oncol Biol Phys 99(1):31–40
Balermpas, P., S. Stera, J. Müller von der Grün, B. Loutfi-Krauss, M. T. Forster, M. Wagner, C. Keller, C. Rödel, V. Seifert, O. Blanck and R. Wolff (2018). “Repeated in-field radiosurgery for locally recurrent brain metastases: Feasibility, results and survival in a heavily treated patient cohort.” PLoS One 13(6): e0198692.
McKay WH, McTyre ER, Okoukoni C, Alphonse-Sullivan NK, Ruiz J, Munley MT, Qasem S, Lo HW, Xing F, Laxton AW, Tatter SB, Watabe K, Chan MD (2017) Repeat stereotactic radiosurgery as salvage therapy for locally recurrent brain metastases previously treated with radiosurgery. J Neurosurg 127(1):148–156
Franzoi MA, Hortobagyi GN (2019) Leptomeningeal carcinomatosis in patients with breast cancer. Crit Rev Oncol Hematol 135:85–94
Dudani S, Mazzarello S, Hilton J, Hutton B, Vandermeer L, Fernandes R, Ibrahim MF, Smith S, Majeed H, Al-Baimani K, Caudrelier JM, Shorr R, Clemons M (2016) Optimal Management of Leptomeningeal Carcinomatosis in Breast Cancer Patients—A Systematic Review. Clin Breast Cancer 16(6):456–470
Gauthier H, Guilhaume MN, Bidard FC, Pierga JY, Girre V, Cottu PH, Laurence V, Livartowski A, Mignot L, Diéras V (2010) Survival of breast cancer patients with meningeal carcinomatosis. Ann Oncol 21(11):2183–2187
Scott BJ, Kesari S (2013) Leptomeningeal metastases in breast cancer. Am J Cancer Res 3(2):117–126
Boogerd W, van den Bent MJ, Koehler PJ, Heimans JJ, van der Sande JJ, Aaronson NK, Hart AA, Benraadt J, Vecht CJ (2004) The relevance of intraventricular chemotherapy for leptomeningeal metastasis in breast cancer: a randomised study. Eur J Cancer 40(18):2726–2733
Meattini I, Livi L, Saieva C, Franceschini D, Marrazzo L, Greto D, Scotti V, Scoccianti S, Paiar F, Bordi L, Nori J, Sanchez L, Orzalesi L, Bianchi S, Biti G (2012) Prognostic factors and clinical features in patients with leptominengeal metastases from breast cancer: a single center experience. J Chemother 24(5):279–284
Atalar B, Modlin LA, Choi CY, Adler JR, Gibbs IC, Chang SD, Harsh GR, Li G, Nagpal S, Hanlon A, Soltys SG (2013) Risk of leptomeningeal disease in patients treated with stereotactic radiosurgery targeting the postoperative resection cavity for brain metastases. Int J Radiat Oncol Biol Phys 87(4):713–718
Kirkpatrick JP (2020) Classifying Leptomeningeal Disease: An Essential Element in Managing Advanced Metastatic Disease in the Central Nervous System. Int J Radiat Oncol Biol Phys 106(3):587–588
Lehrer EJ, Kowalchuk RO, Ruiz-Garcia H, Merrell KW, Brown PD, Palmer JD, Burri SH, Sheehan JP, Quninoes-Hinojosa A, Trifiletti DM (2022) Preoperative stereotactic radiosurgery in the management of brain metastases and gliomas. Front Surg 9:972727
Le Rhun, E., M. Weller, M. van den Bent, D. Brandsma, J. Furtner, R. Ruda, D. Schadendorf, J. Seoane, J. C. Tonn, P. Wesseling, W. Wick, G. Minniti, S. Peters, G. Curigliano, M. Preusser, E. G. Committee and E. G. C. E. a. clinicalguidelines@esmo.org (2023). “Leptomeningeal metastasis from solid tumours: EANO-ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up.” ESMO Open 8(5): 101624.
Le Rhun E, Rudà R, Devos P, Hoang-Xuan K, Brandsma D, Segura PP, Soffietti R, Weller M (2017) Diagnosis and treatment patterns for patients with leptomeningeal metastasis from solid tumors across Europe. J Neurooncol 133(2):419–427
Lee YC, Hsieh CC, Chuang JP, Li CY (2017) The necessity of intrathecal chemotherapy for the treatment of breast cancer patients with leptomeningeal metastasis: A systematic review and pooled analysis. Curr Probl Cancer 41(5):355–370
Glantz MJ, Jaeckle KA, Chamberlain MC, Phuphanich S, Recht L, Swinnen LJ, Maria B, LaFollette S, Schumann GB, Cole BF, Howell SB (1999) A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res 5(11):3394–3402
Grossman SA, Finkelstein DM, Ruckdeschel JC, Trump DL, Moynihan T, Ettinger DS (1993) Randomized prospective comparison of intraventricular methotrexate and thiotepa in patients with previously untreated neoplastic meningitis. Eastern Cooperative Oncology Group. J Clin Oncol 11(3):561–569
Hitchins RN, Bell DR, Woods RL, Levi JA (1987) A prospective randomized trial of single-agent versus combination chemotherapy in meningeal carcinomatosis. J Clin Oncol 5(10):1655–1662
Niwińska A, Rudnicka H, Murawska M (2015) Breast cancer leptomeningeal metastasis: the results of combined treatment and the comparison of methotrexate and liposomal cytarabine as intra-cerebrospinal fluid chemotherapy. Clin Breast Cancer 15(1):66–72
Kumthekar PU, Avram MJ, Lassman AB, Lin NU, Lee E, Grimm SA, Schwartz M, Burdett KLB, Lukas RV, Dixit K, Perron I, Zhang H, Gradishar WJ, Pentsova EI, Jeyapalan S, Groves MD, Melisko M, Raizer JJ (2023) A phase I/II study of intrathecal trastuzumab in human epidermal growth factor receptor 2-positive (HER2-positive) cancer with leptomeningeal metastases: Safety, efficacy, and cerebrospinal fluid pharmacokinetics. Neuro Oncol 25(3):557–565
Oberkampf F, Gutierrez M, Trabelsi Grati O, Rhun EL, Tredan O, Turbiez I, Kadi A, Dubot C, Taillibert S, Vacher S, Bonneau C (2023) Phase II study of intrathecal administration of trastuzumab in patients with HER2-positive breast cancer with leptomeningeal metastasis. Neuro Oncol 25(2):365–374
Rudnicka H, Niwińska A, Murawska M (2007) Breast cancer leptomeningeal metastasis—the role of multimodality treatment. J Neurooncol 84(1):57–62
Wolf A, Donahue B, Silverman JS, Chachoua A, Lee JK, Kondziolka D (2017) Stereotactic radiosurgery for focal leptomeningeal disease in patients with brain metastases. J Neurooncol 134(1):139–143
Yang JT, Wijetunga NA, Pentsova E, Wolden S, Young RJ, Correa D, Zhang Z, Zheng J, Steckler A, Bucwinska W, Bernstein A, Betof AW, Yu H, Kris MG, Seidman AD, Wilcox JA, Malani R, Lin A, DeAngelis LM, Lee NY, Powell SN, Boire A (2022) Randomized Phase II Trial of Proton Craniospinal Irradiation Versus Photon Involved-Field Radiotherapy for Patients With Solid Tumor Leptomeningeal Metastasis. J Clin Oncol 40(33):3858–3867
Gondi V, Bauman G, Bradfield L, Burri SH, Cabrera AR, Cunningham DA, Eaton BR, Hattangadi-Gluth JA, Kim MM, Kotecha R, Kraemer L, Li J, Nagpal S, Rusthoven CG, Suh JH, Tome WA, Wang TJC, Zimmer AS, Ziu M, Brown PD (2022) Radiation Therapy for Brain Metastases: An ASTRO Clinical Practice Guideline. Pract Radiat Oncol 12(4):265–282
Le Rhun, E., M. Guckenberger, M. Smits, R. Dummer, T. Bachelot, F. Sahm, N. Galldiks, E. de Azambuja, A. S. Berghoff, P. Metellus, S. Peters, Y. K. Hong, F. Winkler, D. Schadendorf, M. van den Bent, J. Seoane, R. Stahel, G. Minniti, P. Wesseling, M. Weller, M. Preusser, E. E. Board and E. G. C. E. a. clinicalguidelines@esmo.org (2021). “EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours.” Ann Oncol 32(11): 1332–1347.
Brown, P. D., V. Gondi, S. Pugh, W. A. Tome, J. S. Wefel, T. S. Armstrong, J. A. Bovi, C. Robinson, A. Konski, D. Khuntia, D. Grosshans, T. L. S. Benzinger, D. Bruner, M. R. Gilbert, D. Roberge, V. Kundapur, K. Devisetty, S. Shah, K. Usuki, B. M. Anderson, B. Stea, H. Yoon, J. Li, N. N. Laack, T. J. Kruser, S. J. Chmura, W. Shi, S. Deshmukh, M. P. Mehta, L. A. Kachnic and N. R. G. O. for (2020). “Hippocampal Avoidance During Whole-Brain Radiotherapy Plus Memantine for Patients With Brain Metastases: Phase III Trial NRG Oncology CC001.” J Clin Oncol 38(10): 1019–1029.
Belderbos JSA, De Ruysscher DKM, De Jaeger K, Koppe F, Lambrecht MLF, Lievens YN, Dieleman EMT, Jaspers JPM, Van Meerbeeck JP, Ubbels F, Kwint MH, Kuenen MA, Deprez S, De Ruiter MB, Boogerd W, Sikorska K, Van Tinteren H, Schagen SB (2021) Phase 3 Randomized Trial of Prophylactic Cranial Irradiation With or Without Hippocampus Avoidance in SCLC (NCT01780675). J Thorac Oncol 16(5):840–849
Gondi V, Pugh SL, Tome WA, Caine C, Corn B, Kanner A, Rowley H, Kundapur V, DeNittis A, Greenspoon JN, Konski AA, Bauman GS, Shah S, Shi W, Wendland M, Kachnic L, Mehta MP (2014) Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol 32(34):3810–3816
Rodríguez de Dios N, Couñago F, Murcia-Mejía M, Rico-Oses M, Calvo-Crespo P, Samper P, Vallejo C, Luna J, Trueba I, Sotoca A, Cigarral C, Farré N, Manero RM, Durán X, Gispert JD, Sánchez-Benavides G, Rognoni T, Torrente M, Capellades J, Jiménez M, Cabada T, Blanco M, Alonso A, Martínez-San JM, Escribano J, González B, López-Guerra JL (2021) Randomized Phase III Trial of Prophylactic Cranial Irradiation With or Without Hippocampal Avoidance for Small-Cell Lung Cancer (PREMER): A GICOR-GOECP-SEOR Study. J Clin Oncol 39(28):3118–3127
Yang WC, Chen YF, Yang CC, Wu PF, Chan HM, Chen JL, Chen GY, Cheng JC, Kuo SH, Hsu FM (2021) Hippocampal avoidance whole-brain radiotherapy without memantine in preserving neurocognitive function for brain metastases: a phase II blinded randomized trial. Neuro Oncol 23(3):478–486
Rapp SR, Case LD, Peiffer A, Naughton MM, Chan MD, Stieber VW, Moore DF Jr., Falchuk SC, Piephoff JV, Edenfield WJ, Giguere JK, Loghin ME, Shaw EG (2015) Donepezil for Irradiated Brain Tumor Survivors: A Phase III Randomized Placebo-Controlled Clinical Trial. J Clin Oncol 33(15):1653–1659
Brown PD, Pugh S, Laack NN, Wefel JS, Khuntia D, Meyers C, Choucair A, Fox S, Suh JH, Roberge D, Kavadi V, Bentzen SM, Mehta MP, Watkins-Bruner D, (2013) Radiation Therapy Oncology Group (RTOG). Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol 15(10):1429–1437. https://doi.org/10.1093/neuonc/not114. Epub 2013 Aug 16. PMID: 23956241; PMCID: PMC3779047
Brown PD, Gondi V, Pugh S, Tome WA, Wefel JS, Armstrong TS, Bovi JA, Robinson C, Konski A, Khuntia D, Grosshans D, Benzinger TLS, Bruner D, Gilbert MR, Roberge D, Kundapur V, Devisetty K, Shah S, Usuki K, Anderson BM, Stea B, Yoon H, Li J, Laack NN, Kruser TJ, Chmura SJ, Shi W, Deshmukh S, Mehta MP, Kachnic LA (2020) for NRG Oncology. Hippocampal Avoidance During Whole-Brain Radiotherapy Plus Memantine for Patients With Brain Metastases: Phase III Trial NRG Oncology CC001. J Clin Oncol 38(10):1019–1029. https://doi.org/10.1200/JCO.19.02767. Epub 2020 Feb 14. PMID: 32058845; PMCID: PMC7106984
Yang WC, Chen YF, Yang CC, Wu PF, Chan HM, Chen JL, Chen GY, Cheng JC, Kuo SH, Hsu FM (2021) Hippocampal avoidance whole-brain radiotherapy without memantine in preserving neurocognitive function for brain metastases: a phase II blinded randomized trial. Neuro Oncol 23(3):478–486. https://doi.org/10.1093/neuonc/noaa193. Erratum in: Neuro Oncol. 2021 Dec 1; 23(12):2125. PMID: 32789503; PMCID: PMC7992885
Bernhardt, D., L. Konig, A. Grosu, B. Wiestler, S. Rieken, W. Wick, J. Gempt, S. M. Krieg, F. Schmidt-Graf, F. Sahm, B. Meyer, B. J. Krause, C. Petersen, R. Fietkau, M. Thomas, F. Giordano, A. Wittig-Sauerwein, J. Debus, G. Tabatabai, P. Hau, J. Steinbach, S. E. Combs and O. Expert Panel of the German Society of Radiation (2022). “DEGRO practical guideline for central nervous system radiation necrosis part 1: classification and a multistep approach for diagnosis.” Strahlenther Onkol 198(10): 873–883.
AGO, B. C. (2023). “Recommendations 2023. Diagnosis and Treatment of Patients with Primary and Metastatic Breast Cancer.” Retrieved 08.08.2023, 2023, from https://www.ago-online.de/leitlinien-empfehlungen/leitlinien-empfehlungen/kommission-mamma.
Lebow E, Pike L, Seidman A, Moss N, Beal K, Yu Y (2023) Symptomatic Necrosis With Antibody-Drug Conjugates and Concurrent Stereotactic Radiotherapy for Brain Metastases. JAMA Oncol
Yao Y, Emily L (2023) “Author Reply—Symptomatic Necrosis With Antibody-Drug Conjugates and Concurrent Stereotactic Radiotherapy for. Brain (Metastases” JAMA Oncol)
Figura NB, Potluri TK, Mohammadi H, Oliver DE, Arrington JA, Robinson TJ, Etame AB, Tran ND, Liu JK, Soliman H, Forsyth PA, Sahebjam S, Yu HM, Han HS, Ahmed KA (2019) CDK 4/6 inhibitors and stereotactic radiation in the management of hormone receptor positive breast cancer brain metastases. J Neurooncol 144(3):583–589
Barcellini A, Loap P, Murata K, Villa R, Kirova Y, Okonogi N, Orlandi E (2021) PARP Inhibitors in Combination with Radiotherapy: To Do or Not to Do? Cancers (basel) 13(21)
Suwinski R (2021) Combination of immunotherapy and radiotherapy in the treatment of brain metastases from non-small cell lung cancer. J Thorac Dis 13(5):3315–3322
Kroeze SGC, Pavic M, Stellamans K, Lievens Y, Becherini C, Scorsetti M, Alongi F, Ricardi U, Jereczek-Fossa BA, Westhoff P, But-Hadzic J, Widder J, Geets X, Bral S, Lambrecht M, Billiet C, Sirak I, Ramella S, Battista IG, Benavente S, Zapatero A, Romero F, Zilli T, Khanfir K, Hemmatazad H, de Bari B, Klass DN, Adnan S, Peulen H, Salinas Ramos J, Strijbos M, Popat S, Ost P, Guckenberger M (2023) Metastases-directed stereotactic body radiotherapy in combination with targeted therapy or immunotherapy: systematic review and consensus recommendations by the EORTC-ESTRO OligoCare consortium. Lancet Oncol 24(3):e121–e132
Meattini I, Livi L, Lorito N, Becherini C, Bacci M, Visani L, Fozza A, Belgioia L, Loi M, Mangoni M, Lambertini M, Morandi A (2022) Integrating radiation therapy with targeted treatments for breast cancer: From bench to bedside. Cancer Treat Rev 108:102417
Kroeze SG, Fritz C, Hoyer M, Lo SS, Ricardi U, Sahgal A, Stahel R, Stupp R, Guckenberger M (2017) Toxicity of concurrent stereotactic radiotherapy and targeted therapy or immunotherapy: A systematic review. Cancer Treat Rev 53:25–37
Krop IE, Lin NU, Blackwell K, Guardino E, Huober J, Lu M, Miles D, Samant M, Welslau M, Diéras V (2015) Trastuzumab emtansine (T-DM1) versus lapatinib plus capecitabine in patients with HER2-positive metastatic breast cancer and central nervous system metastases: a retrospective, exploratory analysis in EMILIA. Ann Oncol 26(1):113–119
Lin NU, Borges V, Anders C, Murthy RK, Paplomata E, Hamilton E, Hurvitz S, Loi S, Okines A, Abramson V, Bedard PL, Oliveira M, Mueller V, Zelnak A, DiGiovanna MP, Bachelot T, Chien AJ, O’Regan R, Wardley A, Conlin A, Cameron D, Carey L, Curigliano G, Gelmon K, Loibl S, Mayor J, McGoldrick S, An X, Winer EP (2020) Intracranial Efficacy and Survival With Tucatinib Plus Trastuzumab and Capecitabine for Previously Treated HER2-Positive Breast Cancer With Brain Metastases in the HER2CLIMB Trial. J Clin Oncol 38(23):2610–2619
Lin, N. U., R. K. Murthy, V. Abramson, C. Anders, T. Bachelot, P. L. Bedard, V. Borges, D. Cameron, L. A. Carey, A. J. Chien, G. Curigliano, M. P. DiGiovanna, K. Gelmon, G. Hortobagyi, S. A. Hurvitz, I. Krop, S. Loi, S. Loibl, V. Mueller, M. Oliveira, E. Paplomata, M. Pegram, D. Slamon, A. Zelnak, J. Ramos, W. Feng and E. Winer (2023). “Tucatinib vs Placebo, Both in Combination With Trastuzumab and Capecitabine, for Previously Treated ERBB2 (HER2)-Positive Metastatic Breast Cancer in Patients With Brain Metastases: Updated Exploratory Analysis of the HER2CLIMB Randomized Clinical Trial.” JAMA Oncol 9(2): 197–205.
Hurvitz SA, Hegg R, Chung WP, Im SA, Jacot W, Ganju V, Chiu JWY, Xu B, Hamilton E, Madhusudan S, Iwata H, Altintas S, Henning JW, Curigliano G, Perez-Garcia JM, Kim SB, Petry V, Huang CS, Li W, Frenel JS, Antolin S, Yeo W, Bianchini G, Loi S, Tsurutani J, Egorov A, Liu Y, Cathcart J, Ashfaque S, Cortés J (2023) Trastuzumab deruxtecan versus trastuzumab emtansine in patients with HER2-positive metastatic breast cancer: updated results from DESTINY-Breast03, a randomised, open-label, phase 3 trial. Lancet 401(10371):105–117
Bartsch R, Berghoff AS, Furtner J, Marhold M, Bergen ES, Roider-Schur S, Starzer AM, Forstner H, Rottenmanner B, Dieckmann K, Bago-Horvath Z, Haslacher H, Widhalm G, Ilhan-Mutlu A, Minichsdorfer C, Fuereder T, Szekeres T, Oehler L, Gruenberger B, Singer CF, Weltermann A, Puhr R, Preusser M (2022) Trastuzumab deruxtecan in HER2-positive breast cancer with brain metastases: a single-arm, phase 2 trial. Nat Med 28(9):1840–1847
Montemurro, F., S. Delaloge, C. H. Barrios, R. Wuerstlein, A. Anton, E. Brain, T. Hatschek, C. M. Kelly, C. Peña-Murillo, M. Yilmaz, M. Donica and P. Ellis (2020). “Trastuzumab emtansine (T-DM1) in patients with HER2-positive metastatic breast cancer and brain metastases: exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trial.” Ann Oncol 31(10): 1350–1358.
Bachelot T, Romieu G, Campone M, Diéras V, Cropet C, Dalenc F, Jimenez M, Le Rhun E, Pierga JY, Gonçalves A, Leheurteur M, Domont J, Gutierrez M, Curé H, Ferrero JM, Labbe-Devilliers C (2013) Lapatinib plus capecitabine in patients with previously untreated brain metastases from HER2-positive metastatic breast cancer (LANDSCAPE): a single-group phase 2 study. Lancet Oncol 14(1):64–71
Saura C, Oliveira M, Feng YH, Dai MS, Chen SW, Hurvitz SA, Kim SB, Moy B, Delaloge S, Gradishar W, Masuda N, Palacova M, Trudeau ME, Mattson J, Yap YS, Hou MF, De Laurentiis M, Yeh YM, Chang HT, Yau T, Wildiers H, Haley B, Fagnani D, Lu YS, Crown J, Lin J, Takahashi M, Takano T, Yamaguchi M, Fujii T, Yao B, Bebchuk J, Keyvanjah K, Bryce R, Brufsky A, Investigators N (2020) Neratinib Plus Capecitabine Versus Lapatinib Plus Capecitabine in HER2-Positive Metastatic Breast Cancer Previously Treated With ≥2 HER2-Directed Regimens: Phase III NALA Trial. J Clin Oncol 38(27):3138–3149
Freedman RA, Gelman RS, Wefel JS, Melisko ME, Hess KR, Connolly RM, Van Poznak CH, Niravath PA, Puhalla SL, Ibrahim N, Blackwell KL, Moy B, Herold C, Liu MC, Lowe A, Agar NY, Ryabin N, Farooq S, Lawler E, Rimawi MF, Krop IE, Wolff AC, Winer EP, Lin NU (2016) Translational Breast Cancer Research Consortium (TBCRC) 022: A Phase II Trial of Neratinib for Patients With Human Epidermal Growth Factor Receptor 2‑Positive Breast Cancer and Brain Metastases. J Clin Oncol 34(9):945–952
Lin NU, Pegram M, Sahebjam S, Ibrahim N, Fung A, Cheng A, Nicholas A, Kirschbrown W, Kumthekar P (2021) Pertuzumab Plus High-Dose Trastuzumab in Patients With Progressive Brain Metastases and HER2-Positive Metastatic Breast Cancer: Primary Analysis of a Phase II Study. J Clin Oncol 39(24):2667–2675
Awada, A., R. Colomer, K. Inoue, I. Bondarenko, R. A. Badwe, G. Demetriou, S. C. Lee, A. O. Mehta, S. B. Kim, T. Bachelot, C. Goswami, S. Deo, R. Bose, A. Wong, F. Xu, B. Yao, R. Bryce and L. A. Carey (2016). “Neratinib Plus Paclitaxel vs Trastuzumab Plus Paclitaxel in Previously Untreated Metastatic ERBB2-Positive Breast Cancer: The NEfERT‑T Randomized Clinical Trial.” JAMA Oncol 2(12): 1557–1564.
Tolaney SM, Sahebjam S, Le Rhun E, Bachelot T, Kabos P, Awada A, Yardley D, Chan A, Conte P, Dieras V, Lin NU, Bear M, Chapman SC, Yang Z, Chen Y, Anders CK (2020) A Phase II Study of Abemaciclib in Patients with Brain Metastases Secondary to Hormone Receptor-Positive Breast Cancer. Clin Cancer Res 26(20):5310–5319
Goldberg SB, Schalper KA, Gettinger SN, Mahajan A, Herbst RS, Chiang AC, Lilenbaum R, Wilson FH, Omay SB, Yu JB, Jilaveanu L, Tran T, Pavlik K, Rowen E, Gerrish H, Komlo A, Gupta R, Wyatt H, Ribeiro M, Kluger Y, Zhou G, Wei W, Chiang VL, Kluger HM (2020) Pembrolizumab for management of patients with NSCLC and brain metastases: long-term results and biomarker analysis from a non-randomised, open-label, phase 2 trial. Lancet Oncol 21(5):655–663
Sperduto PW, Mesko S, Li J, Cagney D, Aizer A, Lin NU, Nesbit E, Kruser TJ, Chan J, Braunstein S, Lee J, Kirkpatrick JP, Breen W, Brown PD, Shi D, Shih HA, Soliman H, Sahgal A, Shanley R, Sperduto W, Lou E, Everett A, Boggs DH, Masucci L, Roberge D, Remick J, Plichta K, Buatti JM, Jain S, Gaspar LE, Wu CC, Wang TJC, Bryant J, Chuong M, Yu J, Chiang V, Nakano T, Aoyama H, Mehta MP (2020) Estrogen/progesterone receptor and HER2 discordance between primary tumor and brain metastases in breast cancer and its effect on treatment and survival. Neuro Oncol 22(9):1359–1367
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
K.J. Borm has received honoraria from Accuray. D. Krug has received honoraria from Merck Sharp & Dome, med update, onkowissen, best practice onkologie, ESO, ESMO, Gilead, Astra Zeneca, and Pfizer as well as research funding from Merck KGaA. S.T. Behzadi, J. Hörner-Rieber, R. Baumann, S. Corradini, M.N. Duma, J. Dunst, G. Fastner, P. Feyer, R. Fietkau, W. Haase, W. Harms, T. Hehr, C. Matuschek, M.D. Piroth, L.C. Schmeel, R. Souchon, V. Strnad, W. Budach and S.E. Combs declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Kai J. Borm, Sophie T. Behzadi, Wilfried Budach, Stephanie E. Combs
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Borm, K.J., Behzadi, S.T., Hörner-Rieber, J. et al. DEGRO guideline for personalized radiotherapy of brain metastases and leptomeningeal carcinomatosis in patients with breast cancer. Strahlenther Onkol 200, 259–275 (2024). https://doi.org/10.1007/s00066-024-02202-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-024-02202-0