Abstract
Purpose
We conducted a patterns-of-care survey on chemoradiation for locoregionally confined anal cancer in Austria to evaluate areas of disagreement and to identify possible targets for further standardization.
Methods
An anonymous questionnaire comprising 38 questions was sent to all Austrian radiation oncology departments. Results were analyzed descriptively and compared to two international guidelines.
Results
The response rate was 93%. Work-up generally includes DRE, endoscopy, and cross-sectional imaging of chest/abdomen and pelvis. PET-CT is used by 38%. Screening for HIV and biopsies of suspicious lymph nodes are infrequently used. All centers perform IMRT, mainly with daily IGRT. Median doses to the primary are 54.7 Gy (T1–2) and 59.4 Gy (T3–4). Suspicious nodes receive a boost (median dose 54 Gy), while elective nodal areas are mainly treated with 45–50.4 Gy. Target delineation of elective nodal areas seems generally uniform, although disagreement exists regarding inclusion of the common iliac nodes. No agreement was found for OAR-delineation and dose constraints. Concurrent chemotherapy is mitomycin and 5‑FU/capecitabine. Supportive care beyond skin care is infrequently offered. Intensive follow-up is performed for at least 5 years. Treatment of T1N0 shows considerable disagreement.
Conclusion
We found a high rate of agreement between the centers and concordance with major guidelines. PET-CT, routine HIV testing, and biopsies of suspicious LN seem underrepresented. The largest controversy regarding target volumes concerns inclusion of the common iliac nodes. Prescribed doses are generally in line with the recommendations or higher. OAR delineation, dose constraints, supportive care, and treatment of early anal cancer represent areas for further standardization.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Background
Definitive chemoradiation (CRT) is the standard of care for curative-intent treatment of locoregionally confined anal cancer (AC). While the general indication is widely accepted, international consensus for issues like staging procedures; radiation technique, dose, and fractionation; target volume definition; supportive care; patient counseling; and treatment of early lesions is heterogeneous. Since not all pending questions will be addressed in prospective trials, evidence of lower levels must be taken into account. Surveys generally offer an easy possibility to analyze patterns of care; however, their value is often limited by low response rates. In this regard, regions with a limited number of centers treating the majority of patients may offer some advantages. In Austria, access to radiation therapy is limited to 14 institutions, which can be addressed easily via the Östereichische Gesellschaft für Radio-Onkologie (ÖGRO; Austrian Society of Radiation Oncology [RO]). We therefore conducted a survey regarding CRT of locoregionally confined AC to compare actual patterns of care in Austria with the recommendations of major international guidelines. The following text represents a summary of the main issues, while the full text including detailed results and discussion is available as electronic supplementary material.
Methods
All 14 Austrian RO institutions were invited to take part in the survey on the regular treatment of squamous cell, locoregionally confined, non-metastatic AC. It included 38 questions with either a predefined choice of answers or space for written description of the center’s approach (supplementary material). Because of the known controversies in treating early-stage AC, we included a clinical example and asked for the center’s opinion regarding the optimal approach for T1N0 lesions (supplementary material), while all other questions were restricted to T2-4N0-1M0 stages. The survey was made available online to allow anonymous participation. Numerical variables were analyzed descriptively. Results were compared to the current versions of international, multinationally used multidisciplinary guidelines from the US [1] and Europe [2]. A comparison with other national guidelines (e.g., German, French, or British guidelines) was intentionally not performed.
Results
Response rate/general information
Response rate was 93% (13/14 centers). Most institutions (69%) operate 1–3 linear accelerators, only one center is equipped with > 6. The median number of patients treated with curative-intent (chemo)radiation per year and institution was 14 (7–35). Written standard operating procedures are available in 46%, while no center reported clinical trials currently recruiting patients.
Work-up
Procedures routinely used for diagnostic work-up are listed in Table 1. Clinical examination is performed in all centers, although only 85% explicitly reported digital rectal examination (DRE). All perform some form of endoscopy with histological confirmation and pelvic MRI for locoregional staging. Endorectal ultrasound (39%), ultrasound of inguinal lymph nodes (LN) (23%), or biopsies of suspicious inguinal LN (15%) are infrequently used. To rule out distant metastases, all centers perform some form of chest and abdominal imaging; however, PET-CT is routinely used in only a minority (38%). Routine HIV testing is done in only two centers (15%) and does not change the general treatment principles. Routine HPV testing of the pathological specimen of the primary tumor is performed in 54%, although altering the treatment regime in only one center. Female patients generally receive a specific gynecological clinical examination in 62% and only in case of suspected vaginal involvement in a further 15%. Male patients wishing to preserve fertility or female patients with childbearing potential are routinely counselled with regard to fertility protection or cryopreservation in 77%. Multidisciplinary discussion of the case prior to treatment is routinely done in 85%.
Simulation/treatment planning
Treatment planning CT is done in prone position in one institution, while the remaining centers (92%) prefer supine position. Oral or intravenous contrast agents are used in 8 and 31%, respectively. Patients are required to have a full bladder in all institutions (100%) and eight centers (62%) also advise an empty rectum. The lower edge of the primary tumor (PT) or the anal verge is specifically marked with radio-opaque material in 77%, while only 23% of the centers mark the vagina in female patients. Four institutions (31%) indicated the use of bolus material in case of a prolapsed primary.
Target volume definition/prescription dose
In node-negative cases, all centers include the bilateral inguinal and internal iliac nodes into the CTV, most centers (85–92%) also include the external iliac, mesorectal, presacral, and obturator nodes, but only a minority (46%) include the common iliac nodes (Table 2). Indicated total doses were 30.6–54 Gy in conventional fractionation (single dose 1.65–2.0 Gy), with the majority of centers (n = 7) using total doses of 45–50.4 Gy for all elective nodal regions using 1.8 Gy per fraction.
In cN+ cases, all centers include the bilateral inguinal, internal iliac, external iliac, mesorectal, and obturator LN into the CTV. All but one (92%) would also include the presacral and 62% the common iliac nodes (Table 3). Indicated total doses were 30.6–60 Gy in conventional fractionation (single doses 1.65–2.0 Gy), although the median total doses were slightly higher for all elective nodal regions compared to the cN0 patients. Again, the majority of centers (n = 8) indicated total doses of 45–50.4 Gy for all elective nodal regions in 1.8-Gy single doses.
Most centers (77%) increase the total dose (boost) in suspicious nodes up to a median dose of 54 Gy (range 50–60 Gy), mainly independent of LN size. All institutions used conventional or slightly accelerated fractionation for boosting the LN or LN area (single doses 1.8–2.2 Gy).
Dose escalation in the PT region is generally performed by 92% (n = 12), either as sequential (54%) or simultaneous integrated (15%) external beam photon boost, as electron boost (15%), or via brachytherapy (15%). For small tumors (cT1–2), only 85% generally prescribe a boost, while all prescribe a boost for larger primaries (cT3–4). Ten centers (77%) explicitly indicated increased total doses in cT3–4 compared to cT1–2 tumors. For cT1–2 primaries, a median total dose of 54.7 Gy (50.4–59.4 Gy, single doses 1.8–2.2 Gy) was prescribed, while larger tumors (cT3–4) receive a median total dose of 59.4 Gy (55–64.4 Gy, single doses 1.8–2.3 Gy).
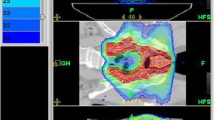
Treatment procedure
All centers use volumetric intensity-modulated RT. Participants were asked to provide information on generally outlined organs at risk (OAR) and whether they use specific dose constraints or just try to keep the dose reasonably low during the planning process (see Table 4). The given dose constraints varied widely even for a single organ at risk (data not shown).
Some form of image-guided RT (IGRT) is performed by all centers. Most departments indicated daily imaging (69%), which is done via cone-beam CT (CBCT) in five or portal imaging in four institutions. The latter is accompanied by CBCT once a week in three institutions. Four centers use daily CBCT in the first 3–5 days and schedule the following IGRT strategy according to the results.
Systemic chemotherapy
All institutions indicated the use of doublet regimens concurrent to RT including mitomycin (100%) and 5‑fluorouracil as continuous infusion (46%) or its prodrug capecitabine (54%). Eleven institutions made specific dose recommendations listed in Table 5. Systemic therapy is administered in the radiation oncology department in the majority of centers (62%).
Supportive treatment
The treatment procedure is performed on an outpatient basis in the majority of centers (69%), while 31% indicated to constantly treat patients on their ward. Specific supportive treatments beyond skin care are offered as nutritional advice in 38%, psycho-oncological support in 23%, and prevention of vaginal stenosis in 54% of the centers.
Follow-up
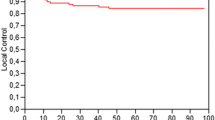
All institutions offer regular follow-up visits, including specific visits in the RO department in 10 centers (77%). Follow-up is offered regularly for 5 years in 77% and for 8–10 years in 15%. Visits are usually scheduled every 3 months for the first year, every 3–6 months for the second year, and every 6–12 months thereafter. Included examinations are listed in Table 6. In case of incomplete clinical remission, 54% of the centers perform biopsies at 3 months and 46% of the centers at 6 months.
Discussion
With a response rate of 93%, our survey represents a complete and valid image of the practice in Austria, clearly outmatching values reached in other countries. For example, a similar German survey recently reported only a 28% response rate [3]. We evaluated areas of agreement and disagreement between the centers and compared the general approach with the recommendations of major international guidelines, namely NCCN [1] and ESMO-ESSO-ESTRO (ESMO) [2] in their latest version.
Work-up
There is considerable agreement on most work-up and staging issues between the centers and with regard to current guidelines [1, 2]. Areas of disagreement mainly include specific additional staging procedures. For example, 54% of the centers indicated the use of a complete colonoscopy, although not recommended according to either guideline [1, 2]. The same is true for endorectal ultrasound (39%), which is not routinely required according to NCCN [1]. In contrast, PET-CT is used for staging in only a minority (38%), although recommended (if available) by NCCN [1] and ESMO [2] for possible advantages in staging accuracy and target volume delineation [4,5,6]. Only 15% of the Austrian centers indicated routine HIV testing, which is even lower than the 27% rate reported in the recent German survey [3]. This might be due to the fact that according to Austrian regulations, HIV testing requires a special informed consent form. Only 54% of the centers indicated routine HPV testing of biopsies, although evidence for HPV positivity as a positive predictive marker for outcome is growing [7, 8]. This might be because only one center indicated altering the treatment concept based on HPV status or because current guidelines [1, 2] do not recommend routine HPV testing nor guidance of treatment decisions by HPV status to date. Good accordance with major guidelines was also found regarding the recommendations for gynecological examinations and counseling for potential infertility. Interestingly, only 15% of the centers perform biopsies in case of suspicious inguinal LN, although recommended by both guidelines [1, 2], while inguinal ultrasound is used by 23%, although not recommended in either one. This practice might be explained by the absence of clear evidence regarding improved staging accuracy with biopsies, or by the fact that most centers indicated using dose escalation in suspicious LN.
Simulation/treatment planning/treatment procedure
Detailed recommendations specifically dealing with treatment planning are given to some extent in the guidelines. Supine treatment position is preferred by both [1, 2], while prone position is advocated only based on individual decisions. The latter is also true for the use of bolus material. Intravenous and/or oral contrast-enhanced CT for treatment planning and marking of the lower tumor edge is recommended only by NCCN [1]. Austrian centers are mainly in line with these recommendations. However, only a minority indicated the use of intravenous and/or oral contrast-enhanced planning CT (38%). Because of superior dose distributions and reduced toxicity [9,10,11,12,13,14,15,16,17], both guidelines [1, 2] clearly recommend intensity-modulated techniques, which has been adopted by all Austrian centers. Similarly, daily kV image guidance is advocated by NCCN [1], which is also preferred by the majority of Austrian centers.
Target volume definition/dose prescription
While NCCN [1] provides specific dose ranges for different disease stages and detailed recommendations regarding the target volume, ESMO [2] includes only very general advice regarding this issue. Therefore, guideline adherence is discussed mainly with regard to NCCN [1].
Regarding total dose to the PT, NCCN [1] recommends a boost beyond the doses prescribed for elective nodal areas of 5.4–14.4 Gy depending on T‑stage, resulting in total doses of 50.4–59.4 Gy (shrinking-field) or 50.4–54 Gy (SIB techniques). This recommendation has been adopted by nearly all Austrian centers, although most prefer sequential boosting. Most centers further indicated prescribing higher total doses in locally advanced primaries (median total 54.7 Gy for T1–2 and 59.4 Gy for T3–4 tumors). While these doses are still in line with the current guideline recommendations [1, 2], an even more personalized approach with further dose de-escalation in early stages and further dose escalation in advanced stages is currently being evaluated in several prospective trials (e.g., by the PLATO platform, ISRCTN88455282, or the DECREASE trial, NCT04166318).
Moreover, the vast majority (85%) indicated use of a boost to enlarged LN (median dose 54 Gy, range 50–60 Gy), mainly restricted to the LN itself rather than the affected region. While the preferred technique of boosting only the involved node is in line with the NCCN [1], the median reported boost dose is equivalent to the dose recommended only for nodes > 3 cm [1]. Interestingly, only one center indicated different doses depending on LN size, although recommended by NCCN [1].
We asked detailed questions regarding the covered elective nodal areas for cN0 and cN1 situations. Generally, high concordance rates between the centers exist regarding both scenarios. Most centers (85%) regularly include the bilateral inguinal, iliac external, iliac internal, mesorectal, presacral, and obturator nodes with an even slightly increased concordance rate for node-positive patients (92%). This pattern does exactly match the NCCN recommendations [1]. The only matter of debate seems to be the common iliac node area. While in cN0 patients, 46% indicated the inclusion of this area, this rate increased even further to 62% in cN1 patients. This finding seems somewhat surprising, as neither NCCN [1] nor ESMO [2] recommends the inclusion of this area in either situation, although increasing evidence suggests that its inclusion might be justified in high-risk situations [18,19,20].
Prescription doses to elective nodal volumes distinctly differ between major trials [10, 13, 14, 21], although all prescribed 30.6–45 Gy. Consequently, NCCN [1] generally recommends this dose range, while ESMO [2] just recommends including “any sites of likely nodal involvement” with no specific dose recommendation. All centers indicated doses to elective nodal regions within the recommended dose ranges or above. The reported median doses are higher for cN+ cases (compared to cN0), suggesting the assumption of controlling a larger amount of subclinical disease with slightly increased doses in cN+ patients. The median reported doses are above the recommended range, especially for cN+ patients (50–50.4 Gy) and to a lesser extent for cN0 patients, although this has not been evaluated or proven by randomized trials.
Regarding dose constraints for OAR, only NCCN [1] but not ESMO [2] provides specific recommendations. The answers given by the Austrian centers showed a large diversity of generally considered OARs and large variations in accepted doses. Contouring OARs and using specific dose constraints for AC might be a field of further improvement.
Systemic chemotherapy
Very strong agreement among Austrian centers and accordance with guidelines exists regarding the chemotherapy regimens for simultaneous CRT. All institutions indicated the use of a doublet including mitomycin (MMC) and 5‑FU or capecitabine, which both showed benefits in two large trials [13, 21, 22]. Capecitabine is preferred over infusional 5‑FU by a slight majority, which may either reflect its easier application or be because retrospective data suggests lower hematological toxicity compared to infusional 5‑FU in patients receiving IMRT [23].
Supportive care
Most centers perform CRT mainly on an outpatient basis, although 31% indicated regularly treating their patients on their wards. This may reflect the assumption of a need for intensified care for treatment side effects or the sometimes large travel distances due to the “centralized” structure of radiation oncology care in Austria as well as the country’s geography.
Clear recommendations regarding supportive care for specific side effects are rarely given by major guidelines, although NCCN provides detailed general recommendations in a specific guideline (NCCN principles of survivorship [24]). To cover this complex subject, we asked two questions referring to generally recommended issues [2, 24] and one to a specific late toxicity. Interestingly, only a minority of centers regularly offers nutritional advice (38%) or psycho-oncological support (23%), although both issues affect the majority of surviving patients after pelvic RT [25, 26]. In contrast, 54% advise female patients to use vaginal dilatators to prevent stenosis, which represents a high level of awareness compared to other reports on sexual dysfunction after pelvic RT [26].
Follow-up
Recommendations regarding follow-up investigations after chemoradiation for AC distinguish between response evaluation and follow-up in case of complete remission. The main issue in response evaluation is the timepoint at which to consider histological confirmation of clinically persistent disease for potential salvage surgery. Austrian centers are divided roughly equally between a 3-month and a 6-month interval, although both guidelines [1, 2] clearly favor the latter timepoint based on the data from ACT II [27].
Regarding follow-up after complete remission, major guidelines favor DRE [1, 2] supported by inguinal node palpation [1, 2] and anoscopy [1] every 3–6 months for 5 years [1], while cross-sectional imaging is recommended at larger intervals and/or only in advanced disease [1]. Accordingly, all Austrian institutions offer regular follow-up using the recommended methods at 3‑month intervals for the first 1–2 years, which are increased to 6–12 months over time. However, those visits usually include cross-sectional imaging (mainly pelvic MRI and chest/abdominal CT) at equal intervals.
Conclusion
In summary, we found high rates of agreement between the centers and concordance with the recommendations of international guidelines, at least covering the main issues of work-up, treatment, and follow-up for CRT of AC. Only PET-CT, routine HIV testing, and biopsy of suspicious LN seem to be less frequently used than recommended. While high agreement and concordance to guidelines are found in general with regard to modern radiation techniques and elective nodal target volumes, large controversy exists regarding inclusion of the common iliac nodes. Prescription doses vary to some extent, but are generally in line with the recommendations, although sometimes at or above the recommended upper dose range. In contrast, no agreement on delineation of OARs or dose constraints exists, which raises a possible need for standardization. The same is true for supportive care during/after CRT, which is underrepresented in major guidelines although this is assumed to be an integral part of the treatment [28]. Follow-up is performed even more intensively than recommended. Considerable disagreement regarding treatment of early AC exists, indicating a need for further research.
Abbreviations
- 5‑FU:
-
5 Fluorouracil
- AC:
-
Anal cancer
- CBCT:
-
Cone-beam computed tomography
- CRT:
-
Chemoradiation
- CT:
-
Computed tomography
- CTV:
-
Clinical target volume
- DRE:
-
Digital rectal examination
- ESMO:
-
European society for medical oncology
- GTV:
-
Gross tumor volume
- HIV:
-
Human immunodeficiency virus
- IGRT:
-
Image-guided radiation therapy
- IMRT:
-
Intensity modulated radiation therapy
- LN:
-
Lymph node
- MMC:
-
Mitomycin C
- MRI:
-
Magnetic resonance imaging
- NCCN:
-
National comprehensive cancer network
- OAR:
-
Organs at risk
- ÖGRO:
-
Östereichische Gesellschaft für Radio-Onkologie
- ÖGRO-GIT:
-
Östereichische Gesellschaft für Radio-Onkologie – Gastrointestinealer Tumoren
- PET-CT:
-
Positron-emission tomography computed tomography
- PT:
-
Primary tumor
- PTV:
-
Planning target volume
- RO:
-
Radiation oncology
- RT:
-
Radiation treatment/radiotherapy
- SIB:
-
Simultaneous integrated Boost
- SOP:
-
Standard operating procedures
- TNM:
-
Tumor Node Metastases
- VMAT:
-
Volumetric intensity-modulated radiation therapy
References
NCCN (2020) NCCN clinical practice guidelines in oncology anal carcinoma, version 2.2020. www.nccn.org. Accessed 20 Dec 2020
Glynne-Jones R, Nilsson PJ, Aschele C et al (2014) Anal cancer: ESMO-ESSO-ESTRO clinical practice guidelines for diagnosis, treatment and follow up. Radiother Oncol 111:330–339
Martin D, von der Grün J, Rödel C, Fokas E (2020) Management of anal cancer patients—a pattern of care analysis in german-speaking countries. Radiat Oncol 15:22
Mahmud A, Poon R, Jonker D (2017) PET imaging in anal cancer: a systematic review and meta-analysis. Br J Radiol 90:20170370
Jones M, Hruby G, Solomon M et al (2015) The role of FDG-PET in the initial staging and response assessment of anal cancer: a systematic review and meta-analysis. Ann Surg Oncol 22:3574–3581
Albertsson P, Alverbratt C, Liljegren A et al (2018) Positron emission tomography and computed tomography (PET/CT) imaging for radiation therapy planning in anal cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol 126:6–12
Urbute A, Rasmussen CL, Belmonte F et al (2020) Prognostic significance of HPV DNA and p16INK4a in anal cancer: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev 29:703–710
Rödel F, Wieland U, Fraunholz I et al (2015) Human papillomavirus DNA and p16INK4a expression predict for local control in patients with anal squamous cell carcinoma treated with chemoradiotherapy. Int J Cancer 136:278–288
Northover J, Glynne-Jones R, Sebag-Montefiore D et al (2010) Chemoradiation for the treatment of epidermoid anal cancer: 13-year follow-up of the first randomized UKCCR anal cancer trial (ACT I). Br J Cancer 102:1123–1128
Kachnic L, Winter K, Myerson RJ et al (2013) RTOG 0529: a phase II evaluation of dose-painted intensity modulated radiation therapy in combination with 5‑fluorouracil and mitomycin‑C for the reduction of acute morbidity in carcinoma of the anal canal. Int J Radiat Oncol Biol Phys 86:27–33
Flam M, John M, Pajak TF et al (1996) Role of mitomycin in combination with fluorouracil and radiotherapy, and of salvage chemoradiation in the definitive nonsurgical treatment of epidermoid carcinoma of the anal canal: results of a phase III randomized intergroup study. J Clin Oncol 14:2527–2539
Ajani JA, Winter KA, Gunderson LL et al (2008) Fluorouracil, mitomycin, and radiotherapy vs fluorouracil, cisplatin, and radiotherapy for carcinoma of the anal canal: a randomized controlled trial. JAMA 299:1914–1921
James RD, Glynne-Jones R, Meadows H et al (2013) Mitomycin or cisplatin chemoradiation with or without maintenance chemotherapy for treatment of squamous-cell carcinoma of the anus (ACT II): a randomized, phase 3, open-label, 2x2 factorial trial. Lancet Oncol 14:516–524
Pfeiffert D, Tournier-Rangeard L, Gerard JP et al (2012) Induction chemotherapy and dose intensification of the radiation boost in locally advanced anal canal carcinoma: final analysis of the randomized UNICANCER ACCORD 03 trial. J Clin Oncol 30:1941–1948
Chen YJ, Liu A, Tsai P et al (2005) Organ sparing by conformal avoidance intensity-modulated radiation therapy for anal cancer: dosimetric evaluation of coverage of pelvis and inguinal/femoral nodes. Int J Radiat Oncol Biol Phys 63:274–281
Chuong MD, Freilich JM, Hoffe SE et al (2013) Intensity-modulated radiation therapy vs. 3D conformal radiation therapy for squamous cell carcinoma of the anal canal. Gastrointest Cancer Res 6:39–45
Sauter M, Lombriser N, Bütikofer S et al (2020) Improved treatment outcome and lower skin toxicity with intensity-modulated radiotherapy vs. 3D conventional radiotherapy in anal cancer. Strahlenther Onkol 196:356–367
Wright JL, Patil SM, Temple LK et al (2010) Squamous cell carcinoma of the anal canal: patterns and predictors of failure and implications for intensity-modulated radiation treatment planning. Int J Radiat Oncol Biol Phys 78:1064–1072
Nilsson MP, Nilsson ED, Johnsson A et al (2020) Patterns of recurrence in anal cancer: a detailed analysis. Radiat Oncol 15:125
Dapper H, Schiller K, Münch S et al (2019) Have we achieved adequate recommendations for target volume definitions in anal cancer? A PET imaging based patterns of failure analysis in the context of established contouring guidelines. BMC Cancer 19:742
Gunderson LL, Winter KA, Ajani JA et al (2012) Long-term update of US GI Intergroup RTOG 98-11 phase III trial for anal carcinoma: survival, relapse, and colostomy failure with concurrent chemoradiation involving fluorouracil/mitomycin versus fluororuracil/cisplatin. J Clin Oncol 30:4344–4351
Martin D, Rödel C, Fokas E (2019) Chemoradiotherapy for anal cancer: Are we as good as we think? Strahlenther Onkol 195:369–373
Goodman KA, Julie D, Cercek A et al (2017) Capecitabine with mitomycin reduces acute hematologic toxicity and treatment delays in patients undergoing definitive chemoradiation using intensity modulated radiation therapy for anal cancer. Int J Radiat Oncol Biol Phys 98:1087–1095
NCCN (2020) NCCN clinical practice guidelines in oncology survivorship, version 2.2020. www.nccn.org. Accessed 20 Dec 2020
Sunesen KG, Norgaardt M, Lundby L et al (2015) Long-term anorectal, urinary and sexual dysfunction causing distress after radiotherapy for anal cancer: a danish multicentre cross-sectional questionnaire study. Colorectal Dis 17:O230–O239
White ID, Allan H, Faithfull S (2011) Assessment of treatment-induced female sexual morbidity in oncology: Is this a part of routine medical follow-up after radical pelvic radiotherapy? Br J Cancer 105:903–910
Glynne-Jones R, Sebag-Montenfiori D, Meadows HM et al (2017) Best time to assess complete clinical response after chemoradiotherapy in squamous cell carcinoma of the anus (ACT II): a post-hoc analysis of randomized controlled phase III trial. Lancet Oncol 18:347–356
Martin D, Rödel C, Fokas E (2020) Einfluss der Behandlungscompliance auf den Erfolg der Radiochemotherapie des Analkarzinoms. Strahlenther Onkol 196:952–953
Acknowledgements
We thank Mag. K. Leberbauer for her assistance in setting up the online version of the questionnaire.
Funding
Open access funding provided by Paracelsus Medical University.
Author information
Authors and Affiliations
Contributions
Gerum S. designed the questionnaire, analyzed the data, and drafted the manuscript. Iglseder W. assisted in designing the questionnaire and data acquisition. Schmid R., Peterka K., Knocke-Abulesz T.H., Harl P., Schwaiger S., Reiter I., Salinger J., Venhoda C., Kurzweil G., Poetscher M., Jaeger R., and Celedin B. answered the questionnaire on behalf of their centers, assisted in data analysis, and critically reviewed the manuscript. Roeder F. participated in design of the questionnaire, data analysis, manuscript draft, and critically revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
F. Roeder received travel grants and speaker honoraria from Lilly Germany and Intraop Medical. S. Gerum, W. Iglseder, R. Schmid, K. Peterka, T.H. Knocke-Abulesz, P. Harl, S. Schwaiger, I. Reiter, J. Salinger,C. Venhoda, G. Kurzweil, M. Poetscher, R. Jaeger, B. Celedin, and P. Clemens declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gerum, S., Iglseder, W., Schmid, R. et al. Practice of radiation therapy for anal cancer in Austria—a survey on behalf of the Austrian radiation oncology society gastrointestinal tumor group (ÖGRO-GIT). Strahlenther Onkol 197, 953–961 (2021). https://doi.org/10.1007/s00066-021-01842-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-021-01842-w