Abstract
Purpose:
To investigate the lung tissue response measured with computed tomography (CT) after radiotherapy (RT) combined with metoclopramide.
Patients and Methods:
Patients with non-small cell lung cancer (tumor stage IIIA and IIIB), included in a multicenter, randomized phase III trial investigating the use of metoclopramide as a radiosensitizing agent, were examined with repetitive post-RT CT scans. The analysis comprised data up to 100 days after RT for a subgroup of 16 patients treated with a total dose of 60 Gy given in 1.82 Gy per fraction.
Results:
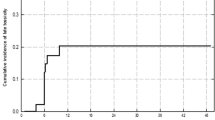
Large radiation doses to subvolumes were associated with denser lung tissue measured with CT (p < 0.001). Opposed to this finding, the volume of lung tissue irradiated with significant doses (V40Gy) was negatively correlated with the average increase in lung tissue density (p = 0.003). Patients randomized to metoclopramide injections also experienced less increase in lung tissue density (p = 0.01).
Conclusion:
There was an increase in the density of irradiated lung tissue with radiation dose and time after RT. Metoclopramide and significant radiation doses to larger lung volumes (V40Gy) seemed to protect against fibrosis development.
Zusammenfassung
Ziel:
Computertomographische (CT) Messung der Strahlenreaktion in Lungengewebe nach Strahlentherapie in Kombination mit Metoclopramid.
Patienten und Methodik:
Patienten mit nichtkleinzelligem Bronchialkarzinom (Tumorstadium IIIA und IIIB), die in eine randomisierte, multizentrische Phase-III-Studie zur Untersuchung des strahlensensitivierenden Effekts von Metoclopramid eingeschlossen waren, wurden mittels wiederholter posttherapeutischer CTs untersucht. Verlaufskontrolldaten bis 100 Tage nach Beendigung der Strahlentherapie einer Untergruppe von 16 Patienten, die mit einer Gesamtdosis von 60 Gy, appliziert in Tagesdosen von 1,82 Gy, behandelt wurden, standen für die Analyse zur Verfügung.
Ergebnisse:
Hohe Strahlendosen auf Teilvolumina resultierten in höherer CT-Dichte im bestrahlten Lungengewebe (p < 0,001). Im Gegensatz dazu korrelierte das mit signifikanter Dosis bestrahlte Lungenvolumen (V40Gy) negativ mit der Zunahme der CTDichte im bestrahlten Lungengewebe (p = 0,003). Bei Patienten, die in den Therapiarm mit Metoclopramid randomisiert wurden, war eine weniger ausgeprägte Zunahme der CT-Dichte im bestrahlten Lungengewebe zu verzeichnen (p = 0,01).
Schlussfolgerung:
Es fand sich ein Zusammenhang zwischen der Zunahme der gemessenen CT-Dichte im bestrahlten Lungengewebe, der applizierten Strahlendosis und der Zeit nach Bestrahlung. Metoclopramid und das mit signifikanter Dosis bestrahlte Lungenvolumen (V40Gy) scheinen einen protektiven Effekt auf die Entwicklung einer Lungenfibrose zu haben.
Similar content being viewed by others
References
Boersma LJ, Damen EM, de-Boer RW, et al. Dose-effect relations for local functional and structural changes of the lung after irradiation for malignant lymphoma. Radiother Oncol 1994;32:201–9.
Boersma LJ, Damen EM, de-Boer RW, et al. Estimation of overall pulmonary function after irradiation using dose-effect relations for local functional injury. Radiother Oncol 1995;36:15–23.
Bölling T, Könemann S, Ernst I, et al. Late effects of thoracic irradiation in children. Strahlenther Onkol 2008;184:289–95.
Bölling T, Schuck A, Paulussen M, et al. Whole lung irradiation in patients with exclusively pulmonary metastases of Ewing tumors. Toxicity analysis and treatment results of the EICESS-92 trial. Strahlenther Onkol 2008;184:193–7.
De Jaeger K, Seppenwoolde Y, Boersma LJ, et al. Pulmonary function following high-dose radiotherapy of non-small cell lung cancer. Int J Radiat Oncol Biol Phys 2003;55:1331–40.
Hua J, Olsson A, Sheng Y, Pero RW. Acidic and neutralized metoclopramide formulations sensitize ionising radiation-induced cytotoxicity in a human lung adenocarcinoma xenografted to scid mice. Anticancer Drugs 1995;6:451–5.
Joiner MC, van der Kogel AJ. The linear quadratic approach to fractionation and calculation of isoeffect relationships. In: Steel GG, ed. Basic clinical radiobiology, 2nd edn. London: Arnold, 1997:106–22.
Kjellen E, Pero RW, Brun E, et al. A phase I/II evaluation of metoclopramide as a radiosensitizer in patients with inoperable squamous cell carcinoma of the lung. Eur J Cancer 1995;31A:2196–202.
Libshitz HI. Radiation-induced pulmonary change: CT findings. J Comput Assist Tomogr 1984;8:15–9.
Libshitz HI. Radiation changes in the lung. Semin Roentgenol 1993;28:303–20.
Lybak S, Kjellen E, Nilsson P, et al. Normal tissue reactions in mice after combined treatment with metoclopramide and ionising radiation. Acta Oncol 1992;31:469–74.
Mirri MA, Arcangeli G, Benassi M, et al. Hypofractionated conformal radiotherapy (HCRT) for primary and metastatic lung cancers with small dimension. Strahlenther Onkol 2009;185:27–33.
Rosen II, Fischer T, Antolak JA, et al. Correlation between lung fibrosis and radiation therapy dose after concurrent radiation therapy and chemotherapy for limited small cell lung cancer. Radiology 2001;221:614–22.
Rotstein S, Lax I, Svane G. Influence of radiation therapy on the lung tissue in breast cancer patients: CT-assessed density changes and associated symptoms. Int J Radiat Oncol Biol Phys 1990;18:173–80.
Seppenwoolde Y, Muller SH, Theuws JC, et al. Radiation dose-effect relations and local recovery in perfusion for patients with non-small cell lung cancer. Int J Radiat Oncol Biol Phys 2000;47:681–90.
Skoczylas JZ, Bentzen SM, Overgaard M, Overgaard J. Time course of radiological lung density changes after postmastectomy radiotherapy. Acta Oncol 2000;39:181–7.
Stranzl H, Zurl B, Langsenlehner T, et al. Wide tangential fields including the internal mammary lymph nodes in patients with left-sided breast cancer. Strahlenther Onkol 2009;185:155–60.
Theuws JC, Kwa SL, Wagenaar AC, et al. Dose-effect relations for early local pulmonary injury after irradiation for malignant lymphoma and breast cancer. Radiother Oncol 1998;48:33–43.
Van Dyk J, Hill RP. Post-irradiation lung density changes measured by computerized tomography. Int J Radiat Oncol Biol Phys 1983;9:847–52.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dale, E., Hårsaker, V., Kristoffersen, D.T. et al. CT Density in Lung Cancer Patients After Radiotherapy Sensitized by Metoclopramide. Strahlenther Onkol 186, 163–168 (2010). https://doi.org/10.1007/s00066-010-2040-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-010-2040-6