Purpose:
To evaluate the impact of wide-tangent fields including the internal mammary chain during deep inspiration breath-hold (DIBH) radiotherapy in patients with left-sided breast cancer on cardiac exposure.
Patients and Methods:
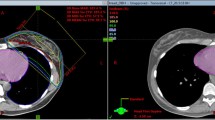
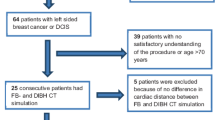
Eleven patients with left-sided breast cancer were irradiated postoperatively and underwent CT scans during free breathing and DIBH. For scientific interest only, treatment plans were calculated consisting of wide tangents including the ipsilateral mammary lymph nodes using both, the free breathing and respiratory-controlled CT scan. The resulting dose-volume histograms were compared for irradiated volumes and doses to organs at risk.
Results:
The mean patient age was 51 years (range: 37–65 years). Radiotherapy using wide tangents with DIBH as compared to free breathing led to a significantly lower cardiac exposure. Mean irradiated heart volumes (≥ 20 Gy) were 14 cm3 (range: 0–51.3 cm3) versus 35 cm3 (range: 2.1–78.7 cm3; p = 0.01). For eight patients, DIBH reduced irradiated relative lung volume, while in three patients, the lung volume slightly increased.
Conclusion:
Radiation exposure of organs at risk can significantly be reduced for breast cancer patients using the DIBH technique. If radiotherapy of the internal mammary lymph nodes is considered necessary, DIBH may be the preferable technique.
Ziel:
Untersuchung des Stellenwerts einer atemgesteuerten (DIBH) Strahlenbehandlung bei Verwendung flacher tangentialer Felder und Einschluss der Lymphknoten entlang der A. mammaria interna bei Patientinnen mit linksseitigem Mammakarzinom im Hinblick auf die Herzbelastung.
Patienten und Methodik:
Bei elf Patientinnen mit linksseitigem Mammakarzinom wurde postoperativ eine lokale Strahlenbehandlung durchgeführt. Für diese CT-Studie wurden unter Bedingungen der Normalatmung und in tiefer Inspiration (Abbildung 1) ein Planungs-CT durchgeführt und jeweils ein optimierter Bestrahlungsplan mit zwei flachen tangentialen Bestrahlungsfeldern unter Berücksichtigung der ipsilateralen Lymphknoten entlang der A. mammaria interna erstellt. Die Dosis-Volumen-Histogramme für die Risikoorgane wurden zwischen beiden Atmungstechniken verglichen.
Ergebnisse:
Der Mittelwert des Alters lag bei 51 Jahren (Range: 37–65 Jahre). Die Bestrahlung mit flachen Tangenten und DIBH erbrachte im Vergleich zur Normalatmung eine signifikant geringere Herzbelastung. Die mittlere Herzbelastung (≥ 20 Gy) ergab 14 cm3 (Range: 0–51,3 cm3) im Vergleich zu 35 cm3 (Range: 2,1–78,7 cm3; p = 0,01; Tabelle 1). Bei acht Patientinnen reduzierte die atemgetriggerte Bestrahlung auch das bestrahlte Lungenvolumen (%), wobei es bei drei Patientinnen geringfügig anstieg (Tabelle 2).
Schlussfolgerung:
Die atemgetriggerte Bestrahlung in tiefer Inspiration reduziert signifikant die Strahlenbelastung an Risikoorganen. Bei Indikation des Einschlusses der Lymphknoten entlang der A. mammaria interna kann die Bestrahlung in DIBH von Vorteil sein.
Similar content being viewed by others
References
Budach W. Cardiac risks in multimodal breast cancer treatment. Strahlenther Onkol 2007;183:Special Issue 2:9–10.
Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomized trials. Lancet 2005;366:2087–106.
Dorr H, Herrmann T. Second tumors after oncologic treatment. Strahlenther Onkol 2008;184:67–72.
Fowble B, Hanlon A, Freedmann G, et al. Internal mammary node irradiation neither decreases distant metastases nor improves survival in stage I and II in breast cancer. Int J Radiat Oncol Biol Phys 2000;47:883–94.
Freedmann GM, Fowble B, Nicolaou N, et al. Should internal mammary lymph nodes in breast cancer be a target for the radiation oncologist? Int J Radiat Oncol Biol Phys 2000;46:805–14.
Grabenbauer GG. Internal mammary nodes in invasive breast carcinoma – to treat or not to treat? Strahlenther Onkol 2004;180:690–4.
Hare GB, Proulx GM, Lamonica DM, et al. Internal mammary lymph nodes (IMN) coverage by standard tangent fields in patients showing IMN drainage on lymphoscintigraphy. Therapeutic implications. Am J Clin Oncol 2004;27:274–8.
Hurkmanns CW, Borger JH, Bos LJ, et al. Cardiac and lung complication probabilities after breast cancer irradiation. Radiother Oncol 2000;55:145–51.
Overgaard M, Hansen PS, Overgaard J, et al. Postoperative radiotherapy in high-risk pre-menopausal women with breast cancer who receive adjuvant chemotherapy. N Engl Med 1997;337:949–55.
Overgaard M, Jensen MB, Overgaard J, et al. Postoperative radiotherapy in high-risk postmenopausal breast cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomized trial. Lancet 1999;353:1641–8.
Poortmans P, Kouloulias V, van Tienhoven G, et al., on behalf of the EORTC Radiation Oncology and Breast Cancer Groups. Quality assurance in the EORTC randomized trial 22922/10925 investigating the role of irradiation of the internal mammary and medial supraclavicular lymph node chain works. Strahlenther Onkol 2006;182:576–82.
Ragaz J, Olivotto IA, Spinelli JJ, et al. Locoregional radiotherapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial. J Natl Cancer Inst 2005;97:116–26.
Recht A, Gray R, Davidson NE, et al. Local-regional failure ten years following mastectomy and adjuvant chemotherapy with or without tamoxifen without radiation. Experience of the Eastern Cooperative Oncology Group. J Clin Oncol 1999;17:1689–700.
Recht A, Pierce SM, Abner A, et al. Regional nodal failure after conservative surgery and radiotherapy for early stage breast carcinoma. J Clin Oncol 1991;9:988–96.
Roth J, Martinez AE. Bestimmung von Organdosen und effektiven Dosen in der Radioonkologie. Strahlenther Onkol 2007;183:392–7.
Sarp S, Fioretta G, Verkooijen HM, et al. Tumor location of the lower-inner quadrant is associated with an impaired survival for women with early-stage breast cancer. Ann Surg Oncol 2007;14:1031–9.
Sauer R, fur die Expertenrunde der DEGRO. Leitlinie: Radiotherapie des Mammakarzinoms. Strahlenther Onkol 2006;182:Suppl I:1–28.
Sautter-Bihl ML, Budach W, Dunst J, et al. DEGRO practical guidelines for radiotherapy of breast cancer I. Breast-conserving therapy. Strahlenther Onkol 2007;183:661–6.
Sautter-Bihl ML, Hultenschmidt B, Melcher U, et al. Radiotherapy of internal mammary lymph nodes in breast cancer. Principle considerations on the basis of dosimetric data. Strahlenther Onkol 2002;178:18–24.
Souchon R, Budach W, Dunst J, et al. Auf eine Radiotherapie nach brusterhaltender Operation eines duktalen Carcinoma in situ (DCIS) darf nicht verzichtet werden. Update der DEGRO-Leitlinie zur Radiotherapie des Mammakarzinoms 2005. Strahlenther Onkol 2006;182:429–30.
Stranzl H, Peintinger F, Ofner P, et al. Regional nodal recurrence in the management of breast cancer patients with 1–3 positive axillary lymph nodes: outcome of patients following tangential irradiation without a separate nodal field. Strahlenther Onkol 2004;180:623–8.
Taylor CW, Nisbet A, McGale P, et al. Cardiac exposures in breast cancer radiotherapy: 1950s–1990s. Int J Radiat Oncol Biol Phys 2007;69:1484–95.
Van de Steene J, Soete G, Storme G. Adjuvant radiotherapy for breast cancer significantly improves overall survival: the missing link. Radiother Oncol 2000;55:263–72.
Yao MS, Kurland BF, Smith AH, et al. Internal mammary nodal chain drainage is a prognostiv indicator in axillary node-positive breast cancer. Ann Surg Oncol 2007;14:2985–93.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stranzl, H., Zurl, B., Langsenlehner, T. et al. Wide Tangential Fields Including the Internal Mammary Lymph Nodes in Patients with Left-Sided Breast Cancer. Strahlenther Onkol 185, 155–160 (2009). https://doi.org/10.1007/s00066-009-1939-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-009-1939-2
Key Words:
- Left-sided breast carcinoma
- Deep inspiration breath-hold technique
- Internal mammary chain
- Organs at risk
- Wide tangents