Abstract
Chronic obstructive pulmonary disease (COPD) primarily affects the lungs; however, cardiovascular conditions are among the most common extrapulmonary comorbidities. Besides shared risk factors such as cigarette smoking, pathophysiological connections between the lung and the heart have been identified as mediators of reduced cardiac output. Recent research has focused on hyperinflation of the lung as a pulmonary cause for heart dysfunction. Hyperinflation is a typical lung abnormality seen in COPD; it is characterized by increased residual volume, intrathoracic gas volume, and total lung capacity while vital capacity is decreased. The degree of hyperinflation with airway obstruction is inversely related to left ventricular filling, stroke volume, and cardiac output. The underlying mechanisms are assumed to be compression of the pulmonary veins and thus reduced preload of the left heart as well as decreased pulmonary microvascular blood flow due to compression of the pulmonary vasculature. Treatment with a dual bronchodilator antagonizes this detrimental lung–heart unbalance effectively: Pulmonary blood flow, left ventricular end-diastolic volume, and stroke volume increase in COPD patients without cardiac abnormalities. Similar effects, yet less pronounced, were reported with single bronchodilator therapy. Future work needs to investigate whether these promising findings can be reproduced in COPD patients with cardiovascular diseases.
Zusammenfassung
Die chronisch obstruktive Lungenkrankheit (COPD) betrifft in erster Linie die Atemwege, kardiovaskuläre Erkrankungen zählen jedoch zu den häufigsten Komorbiditäten. Neben gemeinsamen Risikofaktoren wie dem Rauchen tragen zusätzlich pathophysiologische Wechselwirkungen zwischen Lunge und Herz zu einer verringerten kardialen Auswurfleistung bei. Die aktuelle Forschung konzentriert sich v. a. auf die Lungenüberblähung als Ursache für eine reduzierte Herzleistung bei Patienten mit COPD. Die Überblähung ist eine für die COPD typische pulmonale Funktionsabweichung, die durch ein erhöhtes Residualvolumen, intrathorakales Gasvolumen und eine vergrößerte totale Lungenkapazität bei erniedrigter Vitalkapazität charakterisiert ist. Das Verhältnis zwischen dem Grad der Überblähung und linksventrikulärem enddiastolischem Volumen, Schlagvolumen und Auswurfleistung ist umgekehrt proportional. Dem zugrunde liegen vermutlich erstens eine Kompression der Pulmonalvenen, die zu einer verringerten linksventrikulären Vorlast führt, und zweitens eine Kompression des pulmonalen Kapillarbetts, die einen verminderten pulmonalen mikrovaskulären Blutfluss zur Folge hat. Die Behandlung mit einem dualen Bronchodilatator korrigiert dieses Ungleichgewicht zwischen Lunge und Herz in eine günstige Richtung: Pulmonaler Blutfluss, linksventrikuläres enddiastolisches Volumen und Schlagvolumen erhöhen sich bei überblähten COPD-Patienten ohne kardiale Vorerkrankungen. Ähnliche Effekte, jedoch schwächer ausgeprägt, lassen sich mit einer einfachen bronchienerweiternden Therapie erreichen. Eine zukünftige Forschungsaufgabe liegt darin zu untersuchen, ob sich ähnlich positive Ergebnisse bei COPD-Patienten mit kardiovaskulären Erkrankungen erzielen lassen.


Similar content being viewed by others
References
Adeloye D, Chua S, Lee C et al (2015) Global and regional estimates of COPD prevalence: Systematic review and meta-analysis. J Glob Health 5(2):020415. https://doi.org/10.7189/jogh.05-020415
World Health Organization (2018) Global health estimates 2016: deaths by cause, age, sex, by country and by region. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Sin DD, Anthonisen NR, Soriano JB et al (2006) Mortality in COPD: role of comorbidities. Eur Respir J 28(6):1245–1257. https://doi.org/10.1183/09031936.00133805
André S, Conde B, Fragoso E et al (2018) COPD and cardiovascular disease. Pulmonology. https://doi.org/10.1016/j.pulmoe.2018.09.006
The Global Initiative for Chronic Obstructive Lung Disease (2019) Global initiative for chronic obstructive lung disease 2019 report. https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf
Andreas S, Anker SD, Scanlon PD et al (2005) Neurohumoral activation as a link to systemic manifestations of chronic lung disease. Chest 128(5):3618–3624. https://doi.org/10.1378/chest.128.5.3618
Andreas S, Haarmann H, Klarner S et al (2014) Increased sympathetic nerve activity in COPD is associated with morbidity and mortality. Am J Physiol 192(2):235–241. https://doi.org/10.1007/s00408-013-9544-7
Heindl S, Lehnert M, Criee CP et al (2001) Marked sympathetic activation in patients with chronic respiratory failure. Am J Respir Crit Care Med 164(4):597–601. https://doi.org/10.1164/ajrccm.164.4.2007085
Raupach T, Bahr F, Herrmann P et al (2008) Slow breathing reduces sympathoexcitation in COPD. Eur Respir J 32(2):387–392. https://doi.org/10.1183/09031936.00109607
Forfia PR, Vaidya A, Wiegers SE (2013) Pulmonary heart disease: the heart-lung interaction and its impact on patient phenotypes. Pulm Circ 3(1):5–19. https://doi.org/10.4103/2045-8932.109910
Smith BM, Kawut SM, Bluemke DA et al (2013) Pulmonary hyperinflation and left ventricular mass. Circulation 127(14):1503–1511e6. https://doi.org/10.1161/CIRCULATIONAHA.113.001653
Heistad DD, Abboud FM (1980) Dickinson W. Richards Lecture: Circulatory adjustments to hypoxia. Circulation 61(3):463–470
Coats AJ, Adamopoulos S, Radaelli A et al (1992) Controlled trial of physical training in chronic heart failure. Exercise performance, hemodynamics, ventilation, and autonomic function. Circulation 85(6):2119–2131
Grassi G, Seravalle G, Quarti-Trevano F et al (2009) Sympathetic activation in congestive heart failure: evidence, consequences and therapeutic implications. Curr Vasc Pharmacol 7(2):137–145
Haarmann H, Folle J, Nguyen XP et al (2016) Sympathetic activation is associated with exercise limitation in COPD. COPD 13(5):589–594. https://doi.org/10.3109/15412555.2015.1136272
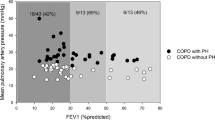
Watz H, Waschki B, Meyer T et al (2010) Decreasing cardiac chamber sizes and associated heart dysfunction in COPD: role of hyperinflation. Chest 138(1):32–38. https://doi.org/10.1378/chest.09-2810
Barr RG, Bluemke DA, Ahmed FS et al (2010) Percent emphysema, airflow obstruction, and impaired left ventricular filling. N Engl J Med 362(3):217–227. https://doi.org/10.1056/NEJMoa0808836
Alter P, Watz H, Kahnert K et al (2018) Airway obstruction and lung hyperinflation in COPD are linked to an impaired left ventricular diastolic filling. Respir Med 137:14–22. https://doi.org/10.1016/j.rmed.2018.02.011
Smith BM, Prince MR, Hoffman EA et al (2013) Impaired left ventricular filling in COPD and emphysema: is it the heart or the lungs? The Multi-Ethnic Study of Atherosclerosis COPD Study. Chest 144(4):1143–1151. https://doi.org/10.1378/chest.13-0183
Kohli P, Neilan TG, Natarajan P et al (2014) Hyperinflation: a potential effect modifier of cardiovascular performance in individuals with chronic obstructive pulmonary disease and heart disease. Am J Respir Crit Care Med 189:A1125
Aaron CP, Hoffman EA, Lima JAC et al (2017) Pulmonary vascular volume, impaired left ventricular filling and dyspnea: The MESA Lung Study. PLoS ONE 12(4):e176180. https://doi.org/10.1371/journal.pone.0176180
Cazzola M, Mantero A, Santus P et al (2007) Doppler echocardiographic assessment of the effects of inhaled long-acting beta2-agonists on pulmonary artery pressure in COPD patients. Pulm Pharmacol Ther 20(3):258–264. https://doi.org/10.1016/j.pupt.2006.02.002
Beeh KM, Singh D, Di Scala L et al (2012) Once-daily NVA237 improves exercise tolerance from the first dose in patients with COPD: the GLOW3 trial. Int J Chron Obstruct Pulmon Dis 7:503–513. https://doi.org/10.2147/COPD.S32451
Santus P, Radovanovic D, Di Marco S et al (2015) Effect of indacaterol on lung deflation improves cardiac performance in hyperinflated COPD patients: an interventional, randomized, double-blind clinical trial. Int J Chron Obstruct Pulmon Dis 10:1917–1923. https://doi.org/10.2147/COPD.S91684
Stone IS, Barnes NC, James W‑Y et al (2016) Lung deflation and cardiovascular structure and function in chronic obstructive pulmonary disease. A randomized controlled trial. Am J Respir Crit Care Med 193(7):717–726. https://doi.org/10.1164/rccm.201508-1647OC
Beeh K‑M, Derom E, Echave-Sustaeta J et al (2016) The lung function profile of once-daily tiotropium and olodaterol via Respimat® is superior to that of twice-daily salmeterol and fluticasone propionate via Accuhaler® (ENERGITO® study). Int J Chron Obstruct Pulmon Dis 11:193–205. https://doi.org/10.2147/COPD.S95055
Hohlfeld JM, Vogel-Claussen J, Biller H et al (2018) Effect of lung deflation with indacaterol plus glycopyrronium on ventricular filling in patients with hyperinflation and COPD (CLAIM): a double-blind, randomised, crossover, placebo-controlled, single-centre trial. Lancet Respir Med 6(5):368–378. https://doi.org/10.1016/S2213-2600(18)30054-7
Vogel-Claussen J, Schonfeld C‑O, Kaireit TF et al (2019) Effect of Indacaterol/Glycopyrronium on pulmonary perfusion and ventilation in Hyperinflated COPD patients (CLAIM): a double-blind, Randomised, crossover trial. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.201805-0995OC
Vogelmeier CF, Bateman ED, Pallante J et al (2013) Efficacy and safety of once-daily QVA149 compared with twice-daily salmeterol-fluticasone in patients with chronic obstructive pulmonary disease (ILLUMINATE): a randomised, double-blind, parallel group study. Lancet Respir Med 1(1):51–60. https://doi.org/10.1016/S2213-2600(12)70052-8
Bateman ED, Ferguson GT, Barnes N et al (2013) Dual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE study. Eur Respir J 42(6):1484–1494. https://doi.org/10.1183/09031936.00200212
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Bauersachs’s, T. Welte’s and J.M. Hohlfeld’s institutions received grant support for conducting clinical studies on the impact of dual bronchodilation in COPD patients by Novartis Pharma GmbH. Moreover, they received personal honoraria for advisory boards and lectures from Novartis Pharma GmbH. N. Struß declares that she has no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Struß, N., Bauersachs, J., Welte, T. et al. Left heart function in COPD. Herz 44, 477–482 (2019). https://doi.org/10.1007/s00059-019-4816-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-019-4816-5
Keywords
- Pulmonary disease, chronic obstructive
- Hyperinflation
- Bronchodilator effect
- Left ventricular function
- Cardiovascular disease