Abstract
Objective
The aim of this study was to assess the effect of plasma homocysteine (Hcy) on left ventricular (LV) diastolic function in Chinese patients with essential hypertension.
Patients and methods
A total of 74 patients with hypertension were enrolled in the present study and were divided into two groups according to the plasma levels of Hcy: high levels of Hcy (Hhcy) group (n = 37) and control group (n = 37) with normal levels of homocysteine. The study participants consisted of 37 hypertensive patients with Hhcy and 37 hypertensive patients without Hhcy. Transthoracic Doppler echocardiography was performed to assess the LV diastolic function of the patients.
Results
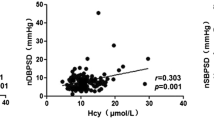
The plasma level of Hcy was directly related to LV diastolic echocardiographic parameters in patients with hypertension whereby the ratio E/e’ was higher (12.7 ± 2.64 vs. 8.98 ± 1.55, p < 0.01), e’/a’ was lower (0.59 ± 0.13 vs. 0.83 ± 0.20, p < 0.01), and the left atrial (LA) diameter was longer (43.4 ± 3.6 mm vs. 37.6 ± 5.0 mm, p < 0.01) in the Hhcy group than in the control group.
Conclusion
The LV diastolic function was significantly deteriorated in Chinese hypertensive patients with Hhcy and there were significant correlations between LV diastolic function indices and Hcy levels.
Zusammenfassung
Ziel
Ziel war es, die Auswirkungen des Homozysteins (Hcy) im Plasma auf die linksventrikuläre (LV) diastolische Funktion bei chinesischen Patienten mit essenzieller Hypertonie (HT) zu untersuchen.
Methoden
In die vorliegende Studie wurden 74 Patienten mit Hypertonie aufgenommen und je nach Plasmaspiegel für Hcy in 2 Gruppen unterteilt: eine Gruppe mit hohem Hcy-Spiegel (Hhcy; n = 37) und eine Kontrollgruppe mit normalem Hcy-Spiegel (n = 37). Die Studienteilnehmer bestanden aus 37 Hypertoniepatienten mit Hhcy und 37 Hypertoniepatienten ohne Hhcy. Zur Bestimmung der diastolischen LV-Funktion wurde bei den Patienten eine transthorakale Dopplerechokardiographie durchgeführt.
Ergebnisse
Der Hcy-Plasmaspiegel stand in direktem Zusammenhang mit diastolischen LV-Echokardiographieparametern bei Hypertoniepatienten. E/e‘ war höher (12,7 ± 2,64 vs. 8,98 ± 1,55; p < 0,01), e’/a‘ war niedriger (0,59 ± 0,13 vs. 0,83 ± 0,20; p < 0,01) und der linksatriale Durchmesser war in der Hhcy-Gruppe größer (43,4 ± 3,6 vs. 37,6 ± 5,0; p < 0,01) als in der Kontrollgruppe.
Schlussfolgerung
Die diastolische LV-Funktion war bei chinesischen Hypertoniepatienten mit Hhcy signifikant beeinträchtigt, dabei bestanden signifikante Korrelationen zwischen Indizes der diastolischen LV-Funktion und dem Hcy-Spiegel.

Similar content being viewed by others
References
Gandhi SK, Powers JC, Nomeir AM et al (2001) The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med 344:17–22
Vasan RS, Benjamin EJ (2001) Diastolic heart failure-no time to relax. N Engl J Med 344:56–59
Qu P, Ding Y, Xia D et al (2001) Variations in cardiac diastolic function in hypertensive patients with different left ventricular geometric patterns. Hypertens Res 24:601–604
Little WC, Ohno M, Kitzman DW et al (1995) Determination of left ventricular chamber stiffness from the time for deceleration of early left ventricular filling. Circulation 92:1933–1939
Wachtell K, Bella JN, Rokkedal J et al (2002) Change in diastolic left ventricular filling after one year of antihypertensive treatment. The Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) Study. Circulation 105:1071–1076
Takamura T, Onishi K, Sugimoto T et al (2008) Patients with a hypertensive response to exercise have impaired left ventricular diastolic function. Hypertens Res 31:257–263
Jiang Y, Xia X, Wang W et al (2012) Hyperhomocysteinemia and related genetic polymorphisms correlate with ulcerative colitis in Chinese Han population in Central China. Cell Biochem Biophys 62:203–210
Stanger O, Weger M (2003) Interactions of homocysteine, nitric oxide, folate and radicals in the progressively damaged endothelium. Clin Chem Lab Med 41:1444–1454
Toole JF, Malinow MR, Chambless LE et al (2004) Lowering homocysteine in patients with ischemic stroke to prevent recurrent stroke, myocardial infarction, and death: the Vitamin Intervention for Stroke Prevention (VISP) randomized trial. JAMA 291:565–575
Jakubowski H (2008) The pathophysiological hypothesis of homocysteine thiolactone-mediated vascular disease. J Physiol Pharmacol 59(Suppl 9):155–167
Dayal S, Lentz SR (2008) Murine models of hyperhomocysteinemia and their vascular phenotypes. Arterioscler Thromb Vasc Biol 28:1596–1605
Tyagi SC (1998) Homocysteine redox receptor and regulation of extracellular matrix components in vascular cells. Am J Physiol 274:C396–C405
Pezzini A, Del Zotto E, Padovani A (2007) Homocysteine and cerebral ischemia: pathogenic and therapeutical implications. Curr Med Chem 14:249–263
Nittynen L, Nurminen ML, Korpela R, Vapaatalo H (1999) Role of arginine, taurine and homocysteine in cardiovascular diseases. Ann Med 31:318–326
Rodrigo R, Passalacqua W, Araya J et al (2003) Homocysteine and essential hypertension. J Clin Pharmacol 43:1299–1306
Lip GY, Edmunds E, Martin SC et al (2001) A pilot study of homocyst(e)ine levels in essential hypertension: relationship to von Willebrand factor, an index of endothelial damage. Am J Hypertens 14:627–631
Sainani GS, Sainani R (2002) Homocysteine and its role in the pathogenesis of atherosclerotic vascular disease. J Assoc Physicians India 50(Suppl):16–23
Galderisi M (2005) Diastolic dysfunction and diastolic heart failure: diagnostic, prognostic and therapeutic aspects. Cardiovasc Ultrasound 3:9
Swedberg K, Cleland J, Dargie H et al (2005) Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): the Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur Heart J 26:1115–1140
Nieminen MS, Böhm M, Cowie MR et al (2005) Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute Heart Failure of the European Society of Cardiology. Eur Heart J 26:384–416
Maurer MS, Spevack D, Burkhoff D, Kronzon I (2004) Diastolic dysfunction: can it be diagnosed by Doppler echocardiography? J Am Coll Cardiol 44:1543–1549
Oh JK, Hatle L, Tajik AJ, Little WC (2006) Diastolic heart failure can be diagnosed by comprehensive two-dimensional and Doppler echocardiography. J Am Coll Cardiol 47:500–506
Gottdiener JS, Bednarz J, Devereux R et al (2004) American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr 17:1086–1119
Bess RL, Khan S, Rosman HS et al (2006) Technical aspects of diastology: why mitral inflow and tissue Doppler imaging are the preferred parameters? Echocardiography 23:332–339
Ishida Y, Meisner JS, Tsujioka K et al (1986) Left ventricular filling dynamics: influence of left ventricular relaxation and left atrial pressure. Circulation 74:187–196
Choong CY, Abascal VM, Thomas JD et al (1988) Combined influence of ventricular loading and relaxation on the transmitral flow velocity profile in dogs measured by Doppler echocardiography. Circulation 78:672–683
Thomas JD, Choong CY, Flachskampf FA, Weyman AE (1990) Analysis of the early transmitral Doppler velocity curve: effect of primary physiologic changes and compensatory preload adjustment. J Am Coll Cardiol 16:644–655
Sohn DW, Chai IH, Lee DJ et al (1997) Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol 30:474–480
Ommen SR, Nishimura RA, Appleton CP et al (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 102:1788–1794
Nagueh SF, Sun H, Kopelen HA et al (2001) Hemodynamic determinants of the mitral annulus diastolic velocities by tissue Doppler. J Am Coll Cardiol 37:278–285
Arques S (2003) Usefulness of combined Doppler indexes in predicting left ventricular filling pressures in patients with acute heart failure. Am J Cardiol 92:649–650
Gonzalez-Vilchez F, Ayuela J, Ares M et al (2002) Comparison of Doppler echocardiography, color M-mode Doppler, and Doppler tissue imaging for the estimation of pulmonary capillary wedge pressure. J Am Soc Echocardiogr 15:1245–1250
Rivas-Gotz C, Manolios M, Thohan V, Nagueh SF (2003) Impact of left ventricular ejection fraction on estimation of left ventricular filling pressures using tissue Doppler and flow propagation velocity. Am J Cardiol 91:780–784
Dokainish H, Zoghbi WA, Lakkis NM et al (2004) Optimal noninvasive assessment of left ventricular filling pressures: a comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation 109:2432–2439
Bruch C, Stypmann J, Grude M et al (2004) Tissue Doppler imaging in patients with moderate to severe aortic valve stenosis: clinical usefulness and diagnostic accuracy. Am Heart J 148:696–702
Bruch C, Grude M, Muller J et al (2005) Usefulness of tissue Doppler imaging for estimation of left ventricular filling pressures in patients with systolic and diastolic heart failure. Am J Cardiol 95:892–895
Hadano Y, Murata K, Liu J et al (2005) Can transthoracic Doppler echocardiography predict the discrepancy between left ventricular end-diastolic pressure and mean pulmonary capillary wedge pressure in patients with heart failure? Circ J 69:432–438
Paelinck BP, Roos A de, Bax JJ et al (2005) Feasibility of tissue magnetic resonance imaging: a pilot study in comparison with tissue Doppler imaging and invasive measurement. J Am Coll Cardiol 45:1109–1116
Arques S, Roux E, Luccioni R (2007) Current clinical applications of spectral tissue Doppler echocardiography (E/e’ ratio) as a noninvasive surrogate for left ventricular diastolic pressures in the diagnosis of heart failure with preserved left ventricular systolic function. Cardiovasc Ultrasound 5:16–28
Bursi F, Weston SA, Redfield MM et al (2006) Systolic and diastolic heart failure in the community. JAMA 296:2209–2216
Kim YJ, Sohn DW (2000) Mitral annulus velocity in the estimation of left ventricular filling pressure: prospective study in 200 patients. J Am Soc Echocardiogr 13:980–985
Kasner M, Westermann D, Steendijk P et al (2007) Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: a comparative Doppler-conductance catheterization study. Circulation 11:637–647
Nagueh SF, Appleton CP, Gillebert CT et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22:107–133
Welch GN, Upchurch G Jr, Loscalzo J (1997) Hyperhomocyst(e)inemia and atherothrombosis. Ann N Y Acad Sci 811:48–58
Andersson A, Lindgren A, Hultberg B (1995) Effect of thiol oxidation and thiol export from erythrocytes on determination of redox status of homocysteine and other thiols in plasma from healthy subjects and patients with cerebral infarction. Clin Chem 41:361–366
Starkebaum G, Harlan JM (1986) Endothelial cell injury due to copper-catalyzed hydrogen peroxide generation from homocysteine. J Clin Invest 77:1370–1376
Celermajer DS, Sorensen K, Ryalls M et al (1993) Impaired endothelial function occurs in the systemic arteries of children with homozygous homocystinuria but not in their heterozygous parents. J Am Coll Cardiol 22:854–858
Stamler JS, Osborne JA, Jaraki O et al (1993) Adverse vascular effects of homocysteine are modulated by endothelium-derived relaxing factor and related oxides of nitrogen. J Clin Invest 91:308–318
Reddy HK, Tjahja IE, Campbell SE et al (2004) Expression of matrix metalloproteinase activity in idiopathic dilated cardiomyopathy: a marker of cardiac dilatation. Mol Cell Biochem 264:183–191
Alter P, Rupp H, Rominger MB et al (2010) Association of hyperhomocysteinemia with left ventricular dilatation and mass in human heart. Clin Chem Lab Med 48:555–560
Au-Yeung KK, Woo CW, Sung FL et al (2004) Hyperhomocysteinemia activates nuclear factor-kappaB in endothelial cells via oxidative stress. Circ Res 94:28–36
Badiou S, Dupuy AM, Jaussent I et al (2012) Homocysteine as a determinant of left ventricular ejection fraction in patients with diabetes. Clin Chem Lab Med 50:1099–1106
Peer M, Boaz M, Zipora M, Shargorodsky M (2013) Determinants of left ventricular hypertrophy in hypertensive patients: identification of high-risk patients by metabolic, vascular, and inflammatory risk factors. Int J Angiol 22:223–228
Acknowledgments
We thank the technicians and staff at the Cardiology Department of Tongji Hospital for data collection and management. We also thank Professor Liu for his contribution to the statistical analysis.
Compliance with ethical guidelines
Conflict of interest. L. Ruhui, J. Jinfa, X. Jiahong, and M. Wenlin state that there are no conflicts of interest. All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruhui, L., Jinfa, J., Jiahong, X. et al. Influence of hyperhomocysteinemia on left ventricular diastolic function in Chinese patients with hypertension. Herz 40, 679–684 (2015). https://doi.org/10.1007/s00059-014-4098-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-014-4098-x
Keywords
- Prospective study
- Color Doppler echocardiography
- Doppler pulsed echocardiography
- Homocysteine
- Left ventricular diastolic function