Abstract
Although hypertension is a clear risk factor for cardiovascular disease, how prehypertension and controlled hypertension influence left ventricular (LV) diastolic function and structure remain to be elucidated. Thus, this study was intended to investigate the link between LV diastolic dysfunction and structural changes in different categories of hypertension. A cohort of 52 111 Korean adults receiving echocardiograms was enrolled. The study population was stratified into five groups according to the following categories of hypertension and blood pressure (BP): normotensive (<120/80 mm Hg), prehypertensive (120–139/80–89 mm Hg), controlled hypertensive (<140/90 mm Hg), newly recognized hypertensive and uncontrolled hypertensive (⩾140/90 mm Hg). Multivariate logistic regression analyses were used to assess the odds ratios (ORs) for LV hypertrophy (LVH) and increased relative wall thickness (RWT), and the adjusted mean values of diastolic parameters were used to examine differences in LV diastolic function. We found a significant relationship between elevated BP and LVH. In addition, an association was observed with LV remodeling (increased RWT). The ORs of LV hypertrophy, remodeling and adjusted mean values of echocardiographic parameters showed dose–response relationships across the study groups, in the order (from lowest to highest) of normotensive, prehypertensive, controlled hypertension, newly recognized hypertension and uncontrolled hypertension. The full adjusted ORs of increased RWT were 1.65 (95% confidence interval (CI): 1.45–1.87) in prehypertension, 2.02 (95% CI: 1.74–2.34) in controlled hypertension, 2.85 (95% CI: 2.35–3.43) in newly recognized hypertension and 3.31 (95% CI: 2.68–4.07) in uncontrolled hypertension. The present study results suggest the importance of early detection and proper management of hypertension.
Similar content being viewed by others
Introduction
Hypertension is a well-known risk factor for cardiovascular (CV) and all-cause mortality.1, 2 Although the treatment of hypertension has been improving for decades, many hypertensive patients remain in an uncontrolled state.3 In the 1999 to 2000 National Health and Nutrition Examination Survey (NHANES), blood pressure (BP) was found to be adequately controlled in only 31% of hypertensive patients.4 In addition, it is thought that many adults are unaware that they have nonoptimal BP levels, such as prehypertension or high normal BP. Although prehypertension is not considered serious, its high prevalence rate may pose substantial health problems. Previous studies have also reported the clinical significance of prehypertension or ‘high normal BP’ as an independent predictor of future CV events and mortality.1, 2, 5 The NHANES 2005–2006 data indicate that ∼25% of the US adult population has prehypertension.6 Thus, given that more than half of adults have nonoptimal BP levels,1, 2, 3, 4, 6 the adverse influence of elevated BP on the CV system is an important clinical issue in public health. In particular, studies have suggested a clinical association among all categories of high BP, prior subclinical LV changes and adverse CV outcomes.7, 8, 9, 10, 11, 12, 13, 14, 15 In previous studies, prehypertension has been found to be an independent risk factor for unfavorable left ventricular (LV) functional and structural changes,7, 8, 9, 10, 11 and individuals with LV diastolic dysfunction, remodeling and hypertrophy have higher risks of CV and all-cause mortality.12, 13, 14, 15 Nonetheless, to date, only a few studies have investigated the association between all categories of BP and subclinical LV functional and structural changes in a general population. Thus, this study was conducted to evaluate the risk for subclinical LV diastolic dysfunction and geometric change across all categories of blood pressure, including controlled hypertension, in the general Korean population.
Methods
Study design and population
A cross-sectional study was conducted to investigate the clinical association between BP categories and subclinical LV changes. Relevant clinical and echocardiographic data were obtained from the Kangbuk Samsung Health Study. The Kangbuk study primarily consisted of Korean men and women undergoing a medical health check-up program at the Health Promotion Center of Kangbuk Samsung Hospital, Sungkyunkwan University, Seoul, Republic of Korea. Among patients in the original study, 55 214 men and women had received at least one echocardiogram, including tissue Doppler echocardiography, between January 2013 and December 2014.
Among the 55 214 participants, 3103 did not meet the final inclusion criteria. A total of 161 patients were excluded because of arrhythmias, such as atrial fibrillation, atrioventricular block or tachycardia. In addition, 58 patients were excluded because of systolic LV dysfunction (ejection fraction ⩽50%). In all, 1448 patients had a history of cancer; 1017 had a severe medical condition, such as asthma, chronic obstructive pulmonary disease or end-stage renal disease; 386 had a history of myocardial infarction or angina; and 33 were excluded for other reasons, such as missing BP data. The final number of eligible participants was 52 111 (Figure 1). Ethics approvals for the study protocol and data analysis were obtained from the institutional review board of Kangbuk Samsung Hospital. Informed consent was not required because only retrospective data without personal identifying information were used.
Clinical and laboratory measurements
Study data included medical history, physical examination, echocardiographic data, information from a self-administered questionnaire, anthropometric measurements and laboratory measurements. Examining physicians assessed the medical and drug prescription histories. All study participants were asked to respond to a health-related behavior questionnaire that included topics of alcohol consumption, smoking and exercise. The questions about alcohol intake included the weekly and daily frequency of alcohol consumption. The degree of physical activity was evaluated with the Korean-validated version of the International Physical Activity Questionnaire.16 The physical activity of participants was classified into three categories (inactive, minimally active and health-enhancing physically active).16, 17 Diabetes mellitus was defined on the basis of a fasting serum glucose level of at least 126 mg dl−1 or a serum hemoglobin A1c level of at least 6.5%, a prior diagnosis of diabetes or the current use of any blood glucose-lowering medications. The body mass index was calculated by dividing the weight (in kg) by the square of the height (in m2).
Blood samples were collected after >12 h of fasting and were drawn from the antecubital vein. The fasting serum glucose was measured using the hexokinase method. Total cholesterol and triglycerides were measured using enzymatic colorimetric tests. Low-density lipoprotein cholesterol was measured using a homogeneous enzymatic colorimetric test, and high-density lipoprotein cholesterol was measured using the selective inhibition method (Advia 1650 Autoanalyzer, Bayer Diagnostics, Leverkusen, Germany).
Fasting insulin concentrations were measured with an immunoradiometric assay (Biosource, Nivelles, Belgium), and hemoglobin A1c was measured using an immunoturbidimetric assay with a Cobra Integra 800 automatic analyzer (Roche Diagnostics, Basel, Switzerland). Insulin resistance was calculated on the basis of homeostasis model assessment-insulin resistance (HOMA-IR). High-sensitivity C-reactive protein was analyzed via particle-enhanced immunonephelometry with a BNII System (Dade Behring, Marburg, Germany).
BP measurements
Trained nurses measured sitting BP levels by using automatic BP equipment (53000-E2, Welch Allyn, Skaneateles Falls, NY, USA) three times after a 5 min rest. Each BP measurement occurred during an interval of at least 30 s. Final BP levels were obtained as the average of the second and third BP measurements. Hypertension was defined on the basis of a prior diagnosis of hypertension (including the current use of any antihypertensive medications) or a measured BP ⩾140/90 mm Hg at initial examination. Controlled hypertension and uncontrolled hypertension were categorized on the basis of measured BP level (uncontrolled hypertension ⩾140/90 mm Hg and controlled hypertension <140/90 mm Hg) for people with a prior diagnosis of hypertension. According to the Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of Hypertension (JNC 7), prehypertension was defined as systolic blood pressure (SBP) of 120–139 mm Hg or diastolic blood pressure (DBP) of 80–89 mm Hg.1 Normal BP was defined as an SBP of <120 mm Hg and a DBP of <80 mm Hg.
Echocardiographic data
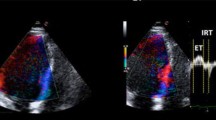
Two-dimensional transthoracic echocardiography with a 4 MHz, sector-type transducer probe was performed on each individual (Vivid 7 and E9, GE, Milwaukee, WI, USA). A trained registered sonographer conducted transthoracic echocardiography according to a standardized protocol. Images from standard parasternal long- and short-axis views were digitally stored and reviewed. Left ventricular end-diastolic diameter (LVEDD), left ventricular end-systolic diameter (LVESD), interventricular septum thickness (IVST) and posterior LV wall thickness (PWT) were routinely measured. The LV mass was calculated with the following formula: LV mass=0.8 × (1.04[(LVEDD+IVST+PWT)3−LVEDD)3])+0.6 g,18 and was indexed on the basis of body surface area). The LV end-systolic volume (LVESV) and LV end-diastolic volume were calculated with the following formula: 7.0/(2.4+LVESD) × LVESD3 and 7.0/(2.4+LVEDD) × LVEDD3. Relative wall thickness (RWT) was calculated with the formula: (2 × PWT)/LVEDD. Increased RWT was defined as RWT >0.42. LV hypertrophy (LVH) was defined as an LV mass index of ⩾115 in males or ⩾95 in females.19 LV geometry was categorized as normal, concentric remodeling, eccentric hypertrophy or concentric hypertrophy.18
Deceleration time was measured via pulsed-wave Doppler ultrasound using the apical four-chamber view. Peak velocities of the early (E) and late (A) phases of mitral inflow were also measured, and E/A ratios were calculated. LV myocardial velocities were evaluated with tissue Doppler imaging. The peak early diastolic (e′) and late diastolic (a′) velocities were measured at the level of the septal mitral valve annulus.19
Statistical analyses
All participants were divided on the basis of their BP values and histories of hypertension: normal, prehypertension, controlled hypertension (history of hypertension, SBP <140 mm Hg and DBP <90 mm Hg), newly recognized hypertension and controlled hypertension (history of hypertension, SBP ⩾140 mm Hg or DBP ⩾90 mm Hg). The data are presented as mean±s.d. within study groups for continuous variables and as proportions for categorical variables. The main clinical characteristics and echocardiographic parameters between five groups were compared using analysis of variance for continuous variables and χ2 tests for categorical variables.
The odds ratios (ORs) of increased RWT- and LVH-based BP categories were calculated using multivariate logistic regression analysis. After testing for multicollinearity, selected variables were enrolled into the adjusting covariates for multivariate logistic regression analysis. We used two models to evaluate the adjusted ORs of BP categories for increased RWT and LVH. Model 1 was adjusted for age and sex, and model 2 was adjusted for covariates related to obesity, dyslipidemia, diabetes, health-related behaviors and chronic inflammation (model 1+body mass index, high-density lipoprotein cholesterol, physical activity, smoking, average alcohol use, diabetes and high-sensitivity C-reactive protein).
The adjusted mean values of echocardiograph parameters, including septal e' velocity, E/e' ratio, E/A ratio LA diameter, LV mass, LVMI and RWT, were used to examine the differences in echocardiographic parameters across the BP categories. We also analyzed LV structural and functional changes in the nondiabetic group to assess the independent effect of prehypertension and hypertension. All statistical analyses were performed using R 3.2.1 (R Foundation for Statistical Computing, Vienna, Austria). The P-values of <0.05 were considered to be statistically significant.
Results
Clinical characteristics of the study population
A total of 52 111 participants were enrolled (36 973 men and 15 138 women). The mean age of the study population was 40.3±8.1 years. The proportion of participants with prehypertension was 17.8% (n=9283), 9.2% had controlled hypertension (n=4795), 3.5% had newly recognized hypertension (n=1818) and 2.7% had controlled hypertension (n=1129). The main demographic characteristics by study population are shown in Table 1. In general, compared with the normotensive group, the prehypertensive group and the three hypertension groups were more likely to have unfavorable clinical characteristics and metabolic parameters such as diabetes, increased body mass index and waist circumference. The proportion of participants using antihypertensive medication was 68.9% for those with controlled hypertension and 35.4% for those with uncontrolled hypertension.
General echocardiographic characteristics
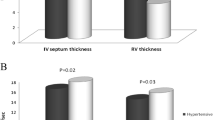
The echocardiographic parameters related to general LV function and structure are shown in Table 2. LV dimension parameters (IVST, PWT, LVEDD, LVESD), LV mass, LVMI (per body surface area or height2.7) and RWT showed a dose–response relationship order (from lowest to highest) of normotensive, prehypertensive, controlled hypertensive and uncontrolled hypertensive groups. Participants with prehypertension and hypertension had higher E/e' ratios and LA diameters and lower E/A ratios and septal e' velocities than did patients in the normotensive group. In general, participants with prehypertension and those in the two hypertensive groups had increased LV mass and impaired diastolic function than did patients in the normotensive group, and the effect was dose responsive. In addition, the participants with increased RWT and LVH also showed similar relationships among study groups. The proportion of LVH was 0.9% in the normotensive group, 1.6% in the prehypertensive group, 4.9% in controlled hypertensives, 3.4% in newly recognized hypertensives and 8.1% in controlled hypertensives. The proportions of increased RWT and LV geometry changes also showed similar relationships.
LV diastolic function and structure according to BP category
Multivariate logistic regression analysis of increased RWT and LVH according to BP and hypertension category is presented in Table 3. Unadjusted ORs showed a very clear dose–response relationship across the study groups. The statistically significant dose–response relationships across the study groups were consistently indicated in models 1 and 2. In model 2, the adjusted ORs of increased RWT were 1.65 (95% confidence interval (CI): 1.45–1.87) in the prehypertensive group, 2.02 (95% CI: 1.74–2.34) in controlled hypertensives, 2.85 (95% CI: 2.35–3.43) in newly recognized hypertensives and 3.31 (95% CI: 2.68–4.07) in uncontrolled hypertensives. The fully adjusted ORs of LVH were 2.10 (95% CI: 1.63–2.70) in the prehypertensive group, 3.02 (95% CI: 2.33–3.91) in controlled hypertensives, 5.03 (95% CI: 3.56–6.99) in newly recognized hypertensives and 10.94 (95% CI: 7.99–14.87) in uncontrolled hypertensives.
The adjusted mean values of echocardiographic parameters are shown in Table 4. The adjusted mean E/e' ratio, indicating increased LV filling pressure,20 was 7.56 (95% CI: 7.52–7.59) in normotensives, 7.89 (95% CI: 7.85–7.94) in prehypertensives, 8.14 (95% CI: 8.09–8.20) in controlled hypertensives, 8.28 (95% CI: 8.20–8.36) in newly recognized hypertensives and 8.54 (95% CI: 8.45–8.64) in uncontrolled hypertensives (model 2). These findings suggested that individuals with well-controlled hypertension had more favorable LV diastolic function than those with uncontrolled or untreated hypertension. Adjusted mean values of LA diameter, LV mass, LVMI and RWT also showed similar relationships across the BP and hypertensive categories in a dose–response manner. In general, prehypertensive and hypertensive groups had more impaired LV diastolic function and geometry changes than did the normotensive group. The participants with uncontrolled hypertension had the worst LV deterioration features among the study groups.
Supplementary Tables 1 and 2 show LV structural and functional changes in the nondiabetic subgroup of BP and hypertensive groups. The ORs of LV structure and adjusted mean values of LV parameters yielded similar findings even in the nondiabetic subgroup.
Discussion
Many studies have demonstrated that hypertension and prehypertension are significantly associated with LV diastolic dysfunction and structural changes. However, only a few studies have investigated LV functional and structural changes across all categories of hypertension in an Asian population. In addition, little is known about the influence of newly recognized, controlled and uncontrolled hypertension on LV functional and structural changes. Here, we had the unique opportunity to assess the risk of LV functional and structural changes across all categories of BP and hypertension in a general population.
In the present study, we obtained two major findings.
First, there were clear dose–response relationships between unfavorable LV structural changes and BP and hypertension categories in the order (from lowest to highest) of normotensive, prehypertensive, controlled hypertensive, newly recognized hypertensive and uncontrolled hypertensive groups. In particular, the controlled hypertensive group had slightly lower SBP and DBP values than did the normotensive group, and had higher ORs for LV structural change than did the prehypertensive group. This finding suggests that LV structural change begins in an early phase of hypertension and progresses to an irreversible state despite proper control of BP. In addition, newly recognized hypertension, compared with controlled hypertension, was more significantly associated with unfavorable LV structural changes, and uncontrolled hypertension had the most adverse influence on LV structure. Interestingly, the most common type of LV structural change across all BP and hypertension categories was concentric remodeling (increased RWT without LVH), thus suggesting an adverse influence of elevated BP on CV outcomes. Previous studies have shown that concentric remodeling is related to an increased risk of CV events.21–23 Furthermore, we revealed that the likelihood of increased RWT was significantly elevated in all categories of hypertension. Thus, our study findings can be extrapolated to suggest clinical significance of optimal BP and proper management of hypertension.
The second major finding was the effect of elevated BP on subclinical LV diastolic function. All categories of hypertension and prehypertension were more significantly associated with impaired LV diastolic function than was the normotensive state. In addition, echocardiographic parameters related to LV diastolic function showed a dose–response relationship in all BP and hypertensive groups, and this relationship was most prominent in the uncontrolled hypertensive group. These findings indicate that elevated BP, especially in individuals with uncontrolled hypertension, has the most harmful effects on the CV system. Furthermore, individuals with controlled hypertension showed more favorable LV diastolic function than did newly recognized or uncontrolled hypertensives. The present study results indicate the importance of early detection and appropriate management of hypertension.
Several previous studies have suggested possible predictors of subclinical LV deterioration, including carotid intima–media thickness, cardio-ankle vascular index and abdominal obesity.24, 25, 26 The present study confirmed that the subclinical range of BP is another possible predictor. The influences of elevated BP on LV function and structure have a consistent tendency revealing that adverse events of LV function and structure begin at a comparatively low BP level (⩾120/80 mm Hg). This finding is consistent with results from a previous meta-analysis revealing that the BP threshold associated with CV death could be lowered to 115/75 mm Hg.5 In the present study, the prehypertensive group, compared with the normal group, had more than twofold ORs of LVH and increased RWT, and the adjusted mean values also showed that participants with prehypertension had impaired LV diastolic function and adverse LV structural changes. These findings are also consistent with previous findings demonstrating an association between prehypertension and unfavorable LV outcomes.7, 8, 9, 10, 11 However, previous studies had some limitations, including the small sample size and limited age distribution. In addition, only a few studies have investigated the influence of elevated BP on subclinical LV changes in Asian groups. Because our study was based on large-scale echocardiographic data obtained from an apparently healthy general Asian population, the influence of elevated BP on LV function and structure might have been more evident.
Our study also showed a strong association among unrecognized uncontrolled hypertension and LV deterioration that may provide a mechanistic explanation for results from previous studies showing increased morbidity and mortality among people with untreated and uncontrolled hypertension.1, 2, 3, 4, 27, 28, 29 Nonetheless, a previous study has demonstrated that more than half of hypertensive patients, despite improvement in hypertension treatment over decades, remain uncontrolled.3 Our study participants also included substantial proportions of untreated and uncontrolled hypertension. Thus, considering the findings that significant unfavorable LV change begins in unrecognized hypertension and progresses in an uncontrolled hypertensive state, early detection of hypertension and education about antihypertensive medications should be warranted.
The major strength of our study was the large-scale epidemiologic study design, including echocardiographic data and detailed histories of hypertension. Nonetheless, we also recognize several weaknesses and limitations of the present study.
First, we conducted only single BP measurements because most of our study participants had annual or biannual health check-ups. Therefore, our data could not assess daily BP fluctuations. Second, we could not measure relevant echocardiographic parameters to assess LV diastolic function, such as lateral e' velocity, isovolumic relaxation time and LA volume. Third, this was a cross-sectional study. Despite our use of large-scale echocardiographic data, our study was unable to address the causal relationship between blood pressure groups and LV deterioration. Fourth, because our study participants had regular medical check-ups, the proportion of uncontrolled hypertension was slightly lower than that in previous studies. Thus, our study may not adequately reflect the nature of the general population with hypertension. Fifth, although the duration of the disease or treatment may be a key point in the LV remodeling, we could not consider this parameter in this study because there were too many data gaps regarding the duration of the disease or treatment.
In conclusion, our study showed an adverse influence of all types of hypertension on LV diastolic function and structure. LV diastolic dysfunction and remodeling began during prehypertension and peaked in the uncontrolled hypertensive state through controlled and newly recognized hypertension. In addition, participants with undiagnosed hypertension had more significant LV deterioration than did controlled hypertensives. These findings suggest the clinical importance of early detection and appropriate control of hypertension.
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ . Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206–1252.
Mancia G, Fagard R, Narkiewicz K, Redán J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F . 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens 2013; 31: 1925–1938.
Chobanian AV . The hypertension paradox—more uncontrolled disease despite improved therapy. N Engl J Med 2009; 361: 878–887.
Wang TJ, Vasan RS . Epidemiology of uncontrolled hypertension in the United States. Circulation 2005; 112: 1651–1662.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–1913.
Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O'Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y, American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009; 119: 480–486.
Markus MR, Stritzke J, Lieb W, Mayer B, Luchner A, Döring A, Keil U, Hense HW, Schunkert H . Implications of persistent prehypertension for ageing-related changes in left ventricular geometry and function: the MONICA/KORA Augsburg study. J Hypertens 2008; 26: 2040–2049.
Kim SH, Cho GY, Baik I, Lim SY, Choi CU, Lim HE, Kim EJ, Park CG, Park J, Kim J, Shin C . Early abnormalities of cardiovascular structure and function in middle-aged Korean adults with prehypertension: The Korean Genome Epidemiology study. Am J Hypertens 2011; 24: 218–224.
Urbina EM, Khoury PR, McCoy C, Daniels SR, Kimball TR, Dolan LM . Cardiac and vascular consequences of pre-hypertension in youth. J Clin Hypertens (Greenwich) 2011; 13: 332–342.
Drukteinis JS, Roman MJ, Fabsitz RR, Lee ET, Best LG, Russell M, Devereux RB . Cardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults: the Strong Heart Study. Circulation 2007; 115: 221–227.
Santos AB, Gupta DK, Bello NA, Gori M, Claggett B, Fuchs F, Shah AM, Coresh J, Sharrett AR, Cheng S, Solomon SD . Prehypertension is associated with abnormalities of cardiac structure and function in the Atherosclerosis Risk in Communities Study. Am J Hypertens 2016; 29: 568–574.
Kane GC, Karon BL, Mahoney DW, Redfield MM, Roger VL, Burnett JC Jr, Jacobsen SJ, Rodeheffer RJ . Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA 2011; 306: 856–863.
Bella JN, Palmieri V, Roman MJ, Liu JE, Welty TK, Lee ET, Fabsitz RR, Howard BV, Devereux RB . Mitral ratio of peak early to late diastolic filling velocity as a predictor of mortality in middle-aged and elderly adults: the Strong Heart Study. Circulation 2002; 105: 1928–1933.
Sundström J, Lind L, Arnlöv J, Zethelius B, Andrén B, Lithell HO . Echocardiographic and electrocardiographic diagnoses of left ventricular hypertrophy predict mortality independently of each other in a population of elderly men. Circulation 2001; 103: 2346–2351.
Brown DW, Giles WH, Croft JB . Left ventricular hypertrophy as a predictor of coronary heart disease mortality and the effect of hypertension. Am Heart J 2000; 140: 848–856.
Oh JY, Yang YJ, Kim BS, Kang JH . Validity and reliability of Korean version of International Physical Activity Questionnaire (IPAQ) short form. J Korean Acad Fam Med 2007; 28: 532–541.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P . International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S, Spencer KT, St John Sutton M, Stewart W, American Society of Echocardiography's Nomenclature and Standards Committee Task Force on Chamber Quantification American College of Cardiology Echocardiography Committee American Heart Association European Association of Echocardiography, European Society of Cardiology. Recommendations for chamber quantification. Eur J Echocardiogr 2006; 7: 79–108.
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A . Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 2009; 22: 107–133.
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ . Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 2000; 102: 1788–1794.
Pierdomenico SD, Di Nicola M, Pierdomenico AM, Lapenna D, Cuccurullo F . Cardiovascular risk in subjects with left ventricular concentric remodeling at baseline examination: a meta-analysis. Hum Hypertens 2011; 25: 585–591.
Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Battistelli M, Bartoccini C, Santucci A, Santucci C, Reboldi G, Porcellati C . Adverse prognostic significance of concentric remodeling of the left ventricle in hypertensive patients with normal left ventricular mass. J Am Coll Cardiol 1995; 25: 871–878.
Muiesan ML, Salvetti M, Monteduro C, Bonzi B, Paini A, Viola S, Poisa P, Rizzoni D, Castellano M, Agabiti-Rosei E . Left ventricular concentric geometry during treatment adversely affects cardiovascular prognosis in hypertensive patients. Hypertension 2004; 43: 731–738.
Yildirim A, Kosger P, Ozdemir G, Sahin FM, Ucar B, Kilic Z . Carotid intima-media thickness and elastic properties of aortas in normotensive children of hypertensive parents. Hypertens Res 2015; 38: 621–626.
Schillaci G, Battista F, Settimi L, Anastasio F, Pucci G . Cardio-ankle vascular index and subclinical heart disease. Hypertens Res 2015; 38: 68–73.
Krzesiński P, Stańczyk A, Piotrowicz K, Gielerak G, Uziębło-Zyczkowska B, Skrobowski A . Abdominal obesity and hypertension: a double burden to the heart. Hypertens Res 2016; 39: 349–355.
Centers for Disease Control and Prevention (CDC). Vital signs: awareness and treatment of uncontrolled hypertension among adults—United States, 2003-2010. MMWR Morb Mortal Wkly Rep 2012; 61: 703–709.
Gu Q, Burt VL, Paulose-Ram R, Yoon S, Gillum RF . High blood pressure and cardiovascular disease mortality risk among U.S. adults: the third National Health and Nutrition Examination Survey mortality follow-up study. Ann Epidemiol 2008; 18: 302–309.
Ezzati M, Oza S, Danaei G, Murray CJ . Trends and cardiovascular mortality effects of state-level blood pressure and uncontrolled hypertension in the United States. Circulation 2008; 117: 905–914.
Acknowledgements
This study was based on medical data collected and arranged by the Kangbuk Samsung Cohort Study (KSCS). Therefore, this study was supported by all staff working at KSCS and the Total Healthcare Center, Kangbuk Samsung Hospital. In addition, we especially appreciate Ms Jiin Ahn and Professor Yoosoo Chang of the Kangbuk Samsung Cohort team. We are also grateful to staff working in the gastroenterology division of the Kangbuk Samsung Total Healthcare Center (Hee Seon Kim, Na Rae Ha and Yun Young Lee). Their technological and statistical assistance largely contributed to our study.
Author contributions
SKP and JYJ coordinated the study, analyzed the data and wrote the manuscript as co-first authors. C-MO analyzed the data and edited the manuscript. JGK and J-MC contributed to writing the discussion and reviewing the manuscript. J-HL participated in reviewing the manuscript. J-HR is the guarantor of this work, and as such has full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Jung, J., Park, S., Oh, CM. et al. The influence of prehypertension, controlled and uncontrolled hypertension on left ventricular diastolic function and structure in the general Korean population. Hypertens Res 40, 606–612 (2017). https://doi.org/10.1038/hr.2016.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.191
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Prevalence of prehypertension and left ventricular hypertrophy
Hypertension Research (2017)