Abstract
Numerous mechanisms involved in promoting cancer cell survival under nutrient starvation have been described. Long noncoding RNAs (lncRNAs) have emerged as critical players in colorectal cancer (CRC) progression, but the role of lncRNAs in the progression of CRC under nutrient starvation has not been well clarified. Here, we identified a lncRNA, LINC01615, that was significantly upregulated in response to serum starvation. LINC01615 can contribute to the adaptation of CRC cells to serum-deprived conditions and enhance cell survival under similar conditions. LINC01615 activated the pentose phosphate pathway (PPP) under serum starvation, manifested as decreased ROS production and enhanced nucleotide and lipid synthesis. Glucose-6-phosphate dehydrogenase (G6PD) is a key rate-limiting enzyme of the PPP, and LINC01615 promoted G6PD expression by competitively binding with hnRNPA1 and facilitating G6PD pre-mRNA splicing. Moreover, we also found that serum starvation led to METTL3 degradation by inducing autophagy, which further increased the stability and level of LINC01615 in a m6A-dependent manner. LINC01615 knockdown combined with oxaliplatin achieved remarkable antitumor effects in PDO and PDX models. Collectively, our results demonstrated a novel adaptive survival mechanism permitting tumor cells to survive under limiting nutrient supplies and provided a potential therapeutic target for CRC.







Similar content being viewed by others
Availability of data and materials
The data generated in this study are available upon request from the corresponding author.
Abbreviations
- CRC:
-
Colorectal cancer
- PPP:
-
Pentose phosphate pathway
- G6PD:
-
G6P dehydrogenase
- lncRNAs:
-
Long noncoding RNAs
- ROS:
-
Reactive oxygen species
- 3-MA:
-
3-Methyladenine
- Baf-A1:
-
Bafilomycin
- shRNA:
-
Short hairpin RNA
- siRNA:
-
Short interfering RNA
- qRT–PCR:
-
Real-time quantitative reverse transcription PCR
- WB:
-
Western blot
- ChIRP-MS:
-
Chromatin isolation by RNA purification-mass spectrometry
- RIP:
-
RNA immunoprecipitation
- PDO:
-
Patient-derived organoid
- PDX:
-
Patient-derived xenograft
- GSEA:
-
Gene set enrichment analysis
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
- ceRNA:
-
Competing endogenous RNA
- Co-IP:
-
Co-immunoprecipitation
- IHC:
-
Immunohistochemistry
- 6-AN:
-
6-Aminonicotinamide
- NAC:
-
N-Acetyl-L-cysteine
- RGG:
-
Arg-Gly-Gly tripeptide repeats
- CCK-8:
-
Cell counting kit-8
- NMR:
-
Nuclear magnetic resonance
- FISH:
-
Fluorescence in situ hybridization
- meRIP:
-
Methylated RNA immunoprecipitation
- TEM:
-
Transmission electron microscopy
References
Cederholm T et al (2017) ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 36:49–64. https://doi.org/10.1016/j.clnu.2016.09.004
Payton M et al (2014) Antagonism of Ang-Tie2 and Dll4-Notch signaling has opposing effects on tumor endothelial cell proliferation, evidenced by a new flow cytometry method. Lab Invest 94:1296–1308. https://doi.org/10.1038/labinvest.2014.116
Izuishi K, Kato K, Ogura T, Kinoshita T, Esumi H (2000) Remarkable tolerance of tumor cells to nutrient deprivation: possible new biochemical target for cancer therapy. Cancer Res 60:6201–6207
Schmitt AM, Chang HY (2016) Long noncoding RNAs in cancer pathways. Cancer Cell 29:452–463. https://doi.org/10.1016/j.ccell.2016.03.010
Kino T, Hurt DE, Ichijo T, Nader N, Chrousos GP (2010) Noncoding RNA gas5 is a growth arrest- and starvation-associated repressor of the glucocorticoid receptor. Sci Signal 3:ra8. https://doi.org/10.1126/scisignal.2000568
Khan MR, Xiang S, Song Z, Wu M (2017) The p53-inducible long noncoding RNA TRINGS protects cancer cells from necrosis under glucose starvation. EMBO J 36:3483–3500. https://doi.org/10.15252/embj.201696239
Li TY et al (2016) ULK1/2 constitute a bifurcate node controlling glucose metabolic fluxes in addition to autophagy. Mol Cell 62:359–370. https://doi.org/10.1016/j.molcel.2016.04.009
Yang HC et al (2019) The redox role of G6PD in Cell growth, cell death, and cancer. Cells. https://doi.org/10.3390/cells8091055
Patra KC, Hay N (2014) The pentose phosphate pathway and cancer. Trends Biochem Sci 39:347–354. https://doi.org/10.1016/j.tibs.2014.06.005
Bernard M et al (2020) Autophagy drives fibroblast senescence through MTORC2 regulation. Autophagy 16:2004–2016. https://doi.org/10.1080/15548627.2020.1713640
Huang S et al (2021) Sirtuin 1 promotes autophagy and proliferation of endometrial cancer cells by reducing acetylation level of LC3. Cell Biol Int 45:1050–1059. https://doi.org/10.1002/cbin.11549
Mancuso A, Sharfstein ST, Tucker SN, Clark DS, Blanch HW (1994) Examination of primary metabolic pathways in a murine hybridoma with carbon-13 nuclear magnetic resonance spectroscopy. Biotechnol Bioeng 44:563–585. https://doi.org/10.1002/bit.260440504
Desideri E et al (2014) MAPK14/p38alpha-dependent modulation of glucose metabolism affects ROS levels and autophagy during starvation. Autophagy 10:1652–1665. https://doi.org/10.4161/auto.29456
Driehuis E, Kretzschmar K, Clevers H (2020) Establishment of patient-derived cancer organoids for drug-screening applications. Nat Protoc 15:3380–3409. https://doi.org/10.1038/s41596-020-0379-4
Arena S et al (2020) A subset of colorectal cancers with cross-sensitivity to olaparib and oxaliplatin. Clin Cancer Res 26:1372–1384. https://doi.org/10.1158/1078-0432.CCR-19-2409
Xiao L et al (2018) Long noncoding RNA uc173 promotes renewal of the intestinal mucosa by inducing degradation of MicroRNA 195. Gastroenterology 154:599–611. https://doi.org/10.1053/j.gastro.2017.10.009
Jiao Z et al (2020) Statin-induced GGPP depletion blocks macropinocytosis and starves cells with oncogenic defects. Proc Natl Acad Sci USA 117:4158–4168. https://doi.org/10.1073/pnas.1917938117
Zhang X et al (2019) Circular RNA circNRIP1 acts as a microRNA-149-5p sponge to promote gastric cancer progression via the AKT1/mTOR pathway. Mol Cancer 18:20. https://doi.org/10.1186/s12943-018-0935-5
Ju HQ et al (2017) Disrupting G6PD-mediated Redox homeostasis enhances chemosensitivity in colorectal cancer. Oncogene 36:6282–6292. https://doi.org/10.1038/onc.2017.227
Chang X et al (2019) Roles for VEGF-C/NRP-2 axis in regulating renal tubular epithelial cell survival and autophagy during serum deprivation. Cell Biochem Funct 37:290–300. https://doi.org/10.1002/cbf.3402
Stincone A et al (2015) The return of metabolism: biochemistry and physiology of the pentose phosphate pathway. Biol Rev Camb Philos Soc 90:927–963. https://doi.org/10.1111/brv.12140
Bensaad K, Cheung EC, Vousden KH (2009) Modulation of intracellular ROS levels by TIGAR controls autophagy. EMBO J 28:3015–3026. https://doi.org/10.1038/emboj.2009.242
Lu J et al (2018) Overexpression of ULK1 Represents a potential diagnostic marker for clear cell renal carcinoma and the antitumor effects of SBI-0206965. EBioMedicine 34:85–93. https://doi.org/10.1016/j.ebiom.2018.07.034
Xu S et al (2019) Ai-lncRNA EGOT enhancing autophagy sensitizes paclitaxel cytotoxicity via upregulation of ITPR1 expression by RNA-RNA and RNA-protein interactions in human cancer. Mol Cancer 18:89. https://doi.org/10.1186/s12943-019-1017-z
Lee YJ, Wang Q, Rio DC (2018) Coordinate regulation of alternative pre-mRNA splicing events by the human RNA chaperone proteins hnRNPA1 and DDX5. Genes Dev 32:1060–1074. https://doi.org/10.1101/gad.316034.118
Kashima T, Rao N, David CJ, Manley JL (2007) hnRNP A1 functions with specificity in repression of SMN2 exon 7 splicing. Hum Mol Genet 16:3149–3159. https://doi.org/10.1093/hmg/ddm276
Hong X et al (2014) PTEN antagonises Tcl1/hnRNPK-mediated G6PD pre-mRNA splicing which contributes to hepatocarcinogenesis. Gut 63:1635–1647. https://doi.org/10.1136/gutjnl-2013-305302
Zhou J et al (2018) N(6)-methyladenosine guides mRNA alternative translation during integrated stress response. Mol Cell 69:636-647.e637. https://doi.org/10.1016/j.molcel.2018.01.019
Wang Y, Le WD (2019) Autophagy and ubiquitin-proteasome system. Adv Exp Med Biol 1206:527–550. https://doi.org/10.1007/978-981-15-0602-4_25
He C (2022) Balancing nutrient and energy demand and supply via autophagy. Curr Biol 32:R684-r696. https://doi.org/10.1016/j.cub.2022.04.071
Chen W, Lian W, Yuan Y, Li M (2019) The synergistic effects of oxaliplatin and piperlongumine on colorectal cancer are mediated by oxidative stress. Cell Death Dis 10:600. https://doi.org/10.1038/s41419-019-1824-6
McQuade RM, Stojanovska V, Bornstein JC, Nurgali K (2017) Colorectal cancer chemotherapy: the evolution of treatment and new approaches. Curr Med Chem 24:1537–1557. https://doi.org/10.2174/0929867324666170111152436
Ahmad S (2010) Platinum-DNA interactions and subsequent cellular processes controlling sensitivity to anticancer platinum complexes. Chem Biodivers 7:543–566. https://doi.org/10.1002/cbdv.200800340
Zhao M et al (2021) Combining neratinib with CDK4/6, mTOR, and MEK inhibitors in models of HER2-positive cancer. Clin Cancer Res 27:1681–1694. https://doi.org/10.1158/1078-0432.CCR-20-3017
Chikashige Y et al (2020) Gcn2 eIF2α kinase mediates combinatorial translational regulation through nucleotide motifs and uORFs in target mRNAs. Nucleic Acids Res 48:8977–8992. https://doi.org/10.1093/nar/gkaa608
Yang X et al (2018) LncRNA PDIA3P interacts with c-Myc to regulate cell proliferation via induction of pentose phosphate pathway in multiple myeloma. Biochem Biophys Res Commun 498:207–213. https://doi.org/10.1016/j.bbrc.2018.02.211
Wang X, Chen K, Zhao Z (2020) LncRNA OR3A4 regulated the growth of osteosarcoma cells by modulating the miR-1207-5p/G6PD signaling. Onco Targets Ther 13:3117–3128. https://doi.org/10.2147/OTT.S234514
Li Q et al (2020) Rac1 activates non-oxidative pentose phosphate pathway to induce chemoresistance of breast cancer. Nat Commun 11:1456. https://doi.org/10.1038/s41467-020-15308-7
Chen S et al (2022) Enhanced pentose phosphate pathway activity promotes pancreatic ductal adenocarcinoma progression via activating YAP/MMP1 axis under chronic acidosis. Int J Biol Sci 18:2304–2316. https://doi.org/10.7150/ijbs.69526
Lin J et al (2022) The POU2F1-ALDOA axis promotes the proliferation and chemoresistance of colon cancer cells by enhancing glycolysis and the pentose phosphate pathway activity. Oncogene 41:1024–1039. https://doi.org/10.1038/s41388-021-02148-y
Ju HQ, Lin JF, Tian T, Xie D, Xu RH (2020) NADPH homeostasis in cancer: functions, mechanisms and therapeutic implications. Signal Transduct Target Ther 5:231. https://doi.org/10.1038/s41392-020-00326-0
Ge T et al (2020) The Role of the Pentose Phosphate Pathway in Diabetes and Cancer. Front Endocrinol 11:365. https://doi.org/10.3389/fendo.2020.00365
Dreher D, Junod AF (1996) Role of oxygen free radicals in cancer development. Eur J Cancer (Oxf, Engl 1990) 32A:30–38
Moloney JN, Cotter TG (2018) ROS signalling in the biology of cancer. Semin Cell Dev Biol 80:50–64. https://doi.org/10.1016/j.semcdb.2017.05.023
Szeszel-Fedorowicz W, Talukdar I, Griffith BN, Walsh CM, Salati LM (2006) An exonic splicing silencer is involved in the regulated splicing of glucose 6-phosphate dehydrogenase mRNA. J Biol Chem 281:34146–34158
Triantaphyllopoulos KA, Laliotis GP, Bizelis IA (2014) Energy balance-dependent regulation of ovine glucose 6-phosphate dehydrogenase protein isoform expression. Adipocyte 3:30–38. https://doi.org/10.4161/adip.26437
Roy R et al (2014) hnRNPA1 couples nuclear export and translation of specific mRNAs downstream of FGF-2/S6K2 signalling. Nucleic Acids Res 42:12483–12497. https://doi.org/10.1093/nar/gku953
Zhu W et al (2020) Heterogeneous nuclear ribonucleoprotein A1 exerts protective role in intracerebral hemorrhage-induced secondary brain injury in rats. Brain Res Bull 165:169–177. https://doi.org/10.1016/j.brainresbull.2020.09.023
Roy R, Huang Y, Seckl MJ, Pardo OE (2017) Emerging roles of hnRNPA1 in modulating malignant transformation. Wiley Interdiscip Rev RNA. https://doi.org/10.1002/wrna.1431
Sun G et al (2020) HnRNP A1 - mediated alternative splicing of CCDC50 contributes to cancer progression of clear cell renal cell carcinoma via ZNF395. J Exp Clin Cancer Res 39:116. https://doi.org/10.1186/s13046-020-01606-x
Lan Z et al (2020) The interaction between lncRNA SNHG6 and hnRNPA1 contributes to the growth of colorectal cancer by enhancing aerobic glycolysis through the regulation of alternative splicing of PKM. Front Oncol 10:363. https://doi.org/10.3389/fonc.2020.00363
Liu Y et al (2020) hnRNP A1 regulates alternative splicing of tau exon 10 by targeting 3’ splice sites. Cells. https://doi.org/10.3390/cells9040936
Chen XY, Zhang J, Zhu JS (2019) The role of m(6)A RNA methylation in human cancer. Mol Cancer 18:103. https://doi.org/10.1186/s12943-019-1033-z
Yang S et al (2019) m(6)A mRNA demethylase FTO regulates melanoma tumorigenicity and response to anti-PD-1 blockade. Nat Commun 10:2782. https://doi.org/10.1038/s41467-019-10669-0
Niu Y et al (2013) N6-methyl-adenosine (m6A) in RNA: an old modification with a novel epigenetic function. Genom Proteom Bioinform 11:8–17. https://doi.org/10.1016/j.gpb.2012.12.002
Zhou Z et al (2020) Mechanism of RNA modification N6-methyladenosine in human cancer. Mol Cancer. https://doi.org/10.1186/s12943-020-01216-3
Jiao L et al (2018) Regulation of glycolytic metabolism by autophagy in liver cancer involves selective autophagic degradation of HK2 (hexokinase 2). Autophagy 14:671–684. https://doi.org/10.1080/15548627.2017.1381804
Amaravadi R, Kimmelman AC, White E (2016) Recent insights into the function of autophagy in cancer. Genes Dev 30:1913–1930. https://doi.org/10.1101/gad.287524.116
Liu W et al (2015) HMGB1-mediated autophagy modulates sensitivity of colorectal cancer cells to oxaliplatin via MEK/ERK signaling pathway. Cancer Biol Ther 16:511–517. https://doi.org/10.1080/15384047.2015.1017691
Yin H et al (2020) Chiauranib selectively inhibits colorectal cancer with KRAS wild-type by modulation of ROS through activating the p53 signaling pathway. Am J Cancer Res 10:3666–3685
Acknowledgements
We thank all individuals who participated in this work.
Funding
This research was supported by grants from the National Natural Science Foundation of China (No.82072729, No.81602568, No.81773130), China Postdoctoral Science Foundation (No.2018M643009), the Natural Science Foundation of Jiangsu (BK20211606), the National Natural Science Foundation of Hunan Province (No. 2019JJ50906) and Xuzhou Key R&D Program (KC20064).
Author information
Authors and Affiliations
Contributions
YZ and LX conceived and designed the experiment, performed experiment, and wrote the manuscript. ZR, XL, JS, PZ, CZ, SG, NW, and XZ performed experiment, collected data and analyzed data. CX, ZL, MM, YZ, and YC interpreted data and constructed figures. CL conceptualized the study, designed the experiment, interpreted data and reviewed the manuscript. All authors read and approved the final version of the manuscript. YZ and CL have accessed and verified the data, and CL was responsible for the decision to submit the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest.
Ethical approval and consent to participate
This study was performed according to the ethical standards of Declaration of Helsinki and was approved by the ethics committee of the Xuzhou Medical University (XYFY2019-KL221-01). All animal experiments were approved by the Animal Care Committee of Xuzhou Medical University.
Consent for publication
We have obtained consents to publish this paper from all the participants of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
18_2022_4675_MOESM2_ESM.tif
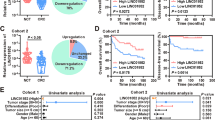
Supplementary file2 Supplementary Figure 1 (A) Venn diagram showing the numbers of overlapping lncRNAs between the differentially downregulated lncRNAs in HCT116 and DLD1 cells after serum-free medium treatment. (B) Kaplan–Meier analysis of the OS rate in CRC patients in the TCGA database with high or low expression of CTD-2147F2.1. (C) The non-coding nature of LINC01615 was predicted by coding-potential analysis (PhyloCSF). (D) The relative expression of LINC01615 in various types of tumor tissues and corresponding peritumor tissues based on data obtained from TCGA database. (E) The relative expression of LINC01615 in tumor tissue and corresponding peritumor tissue based on data obtained from the GEO database (GSE115856). (F) qRT-PCR showed the expression of LINC01615 in normal intestinal epithelial cell line FHC and CRC cell lines (DLD1, HT-29, SW620, SW480, LoVo and HT29). (G) qRT-PCR examined the expression of LINC01615 after knockdown in DLD1 and HCT116 cells. (H) qRT-PCR examined the expression of LINC01615 after overexpression in LoVo cells. (I) CCK-8 assay showed the effects of LINC01615 knockdown on proliferation in HCT116 cells without serum supplementation. (J) Colony formation assays were performed to examine the effects of LINC01615 knockdown on proliferation in HCT116 cells without serum supplementation. (K) Statistical analysis of colony formation numbers in (J). (L-M) CCK-8 assay showed the effect of LINC01615 knockdown on proliferation in DLD1 and HCT116 cells under normal conditions. (N-O) Images of flow cytometry analysis showing the effects of LINC01615 knockdown and LINC01615 overexpression on the apoptotic rate in DLD1, HCT116 and LoVo cells without serum supplementation. (P) Flow cytometry data presented as histograms showing the effects of LINC01615 knockdown on the apoptotic rate in HCT116 cells without serum supplementation. (Q) WB was used to examine the effects of LINC01615 knockdown on the expression of cleaved caspase 3, caspase 7, caspase 9 and BCL-2 in HCT116 cells without serum supplementation. GAPDH was used as a loading control. Data are shown as the mean ± S.E. * p<0.05, ** p<0.01. (TIF 6432 kb)
18_2022_4675_MOESM3_ESM.tif
Supplementary file3 Supplementary Figure 2 (A) HCT116 cells were transfected with LINC01615 shRNA or control shRNA. Then, the cells were cultured in medium containing [2-13C] glucose and without serum supplementation. Oxidative PPP flux was measured based on the rate of glucose consumption and the ratio of 13C incorporated into carbon 2 (indicating glycolysis) and carbon 3 (indicating PPP) of lactate by nuclear magnetic resonance (NMR) spectroscopy. (B) NADP+/NADPH ratios were measured in the cells from (A). (C) ROS levels were measured in the cells from (A). (D) Images of flow cytometry analysis showing the effects of LINC01615 knockdown and LINC01615 overexpression on the ROS level in DLD1 and LoVo cells without serum supplementation. (E) CCK-8 assay showed the effects of LINC01615 inhibition on proliferation in HCT116 cells treated with or without NAC under serum-free starvation conditions. (F) Images of flow cytometry analysis showing the effects of LINC01615 inhibition on the apoptotic rate in DLD1 and HCT116 cells treated with or without NAC under serum-free starvation conditions. (G) Flow cytometry data presented as histograms show the effects of LINC01615 inhibition on the apoptotic rate in HCT116 cells treated with or without NAC under serum-free starvation conditions. (H) WB was used to examine the effects of LINC01615 inhibition on cleaved caspase 3, caspase 7, caspase 9 and BCL-2 expression in HCT116 cells treated with or without NAC under serum-free starvation conditions. (I-J) CCK-8 assay showed the effects of LINC01615 inhibition on proliferation in DLD1 and HCT116 cells treated with or without R5P under serum-free starvation conditions. (K) Statistical analysis of EdU (+) cells in (Figure 3M). (L) EdU staining assay showed the effect of LINC01615 inhibition on nucleotide synthesis in HCT116 cells treated with or without R5P under serum-free starvation conditions. (M) Statistical analysis of EdU (+) cells in (L). (N-O) CCK-8 assay showed the effects of LINC01615 inhibition on proliferation in DLD1 and HCT116 cells treated with or without NADPH under serum-free starvation conditions. (P) Oil red O staining assay showed the effect of LINC01615 inhibition on lipid synthesis in HCT116 cells treated with or without NADPH under serum-free starvation conditions. Data are shown as the mean ± S.E. * p<0.05, ** p<0.01. (TIF 5630 kb)
18_2022_4675_MOESM4_ESM.tif
Supplementary file4 Supplementary Figure 3 (A) The top-scoring genes recurring in the PPP gene sets, including G6PD. (B) The statistical analysis of G6PD expression in 275 colon cancer tissues and 41 normal tissues; paired t-test. In the boxplots, the middle line depicts the median and the whiskers are the min to max range. (C) The correlation between LINC01615 and G6PD expression in 275 colon cancer tissues. (D) The expression of G6PD in normal tissues and CRC tissues was assessed by IHC. (E-F) Statistical analysis of EdU (+) cells in (Figure 4I-J). (G) Antibodies against hnRNPA1 were used for RIP, followed by LINC01615 qRT–PCR in DLD1 and LoVo cells. (H) Antibodies against hnRNPA1 were used for RIP, followed by LINC01615 qRT–PCR, in DLD1 cells with or without serum supplementation. (I) Antibodies against hnRNPA1 were used for RIP, followed by G6PD pre-mRNA qRT–PCR in DLD1 and LoVo cells. (J) Antibodies against hnRNPA1 were used for RIP, followed by G6PD pre-mRNA qRT–PCR in LoVo cells transfected with LINC01615 overexpression plasmid or control vector. (K-L) WB was used to examine the effects of hnRNPA1 knockdown and overexpression on the expression of hnRNPA1 in DLD1, HCT116 and LoVo cells. (M) Antibodies against Flag were used for RIP, followed by G6PD pre-mRNA qRT–PCR in DLD1 cells. (N) Colony formation assay was conducted to examine the effects of hnRNPA1 truncated plasmids with or without RRM2 domain on proliferation in DLD1 cells which overexpressing LINC01615 and without serum supplementation. (O) Statistical analysis of colony formation numbers in (N). (P) Images of flow cytometry analysis showing the effects of hnRNPA1 truncated plasmid with or without RRM2 domain on the apoptotic rate in DLD1 cells overexpressing LINC01615 under serum-free starvation conditions. (Q) Flow cytometry data presented as histograms showing the effects of hnRNPA1 truncated plasmid with or without RRM2 domain on the apoptotic rate in DLD1 cells overexpressing LINC01615 and without serum supplementation. Data are the means ± SD (n = 3 independent experiments), * p<0.05, ** p<0.01. (TIF 7126 kb)
18_2022_4675_MOESM5_ESM.tif
Supplementary file5 Supplementary Figure 4 (A) SRAMP (http://www.cuilab.cn/sramp/) prediction revealed several m6A sites distributed in LINC01615. (B) WB analysis of the expression of METTL3, METTL14 and FTO in DLD1 cells cultured with or without serum supplementation. (C-D) WB was used to examine the effects of METTL3 knockdown and overexpression on the expression of METTL3 in DLD1 and LoVo cells. (E) qRT–PCR analysis of the expression of LINC01615 in LoVo cells transfected with METTL3 overexpression plasmid or control vector. (F) qRT–PCR analysis of LINC01615 expression in LoVo cells cultured with or without serum supplementation and transfected with METTL3 overexpression plasmid or control vector. (G) The correlation between METTL3 and LINC01615 expression in colon tissues. (H) Statistical analysis of IHC staining scores in (Figure 6D). (I) meRIP-qPCR showing the m6A modification enrichment of LINC01615 in LoVo cells after METTL3 overexpression. (J) qRT–PCR analysis of the stability of LINC01615 in LoVo cells with or without METTL3 overexpression. Data are the means ± SD (n = 3 independent experiments), * p<0.05, ** p<0.01. (TIF 2502 kb)
18_2022_4675_MOESM6_ESM.tif
Supplementary file6 Supplementary Figure 5 (A) WB analysis of METTL3 protein stability in LoVo cells cultured with or without serum supplementation for different times. (B) Transmission electron microscopy images of autophagic vacuoles in DLD1 and LoVo cells under normal or serum-free starvation conditions. Arrows indicate autophagosomes; scale bar, 500 nm. (C) Representative confocal microscopy images of LC3B puncta distribution in LoVo cells under normal or serum-free starvation conditions and treated with or without Baf A1 (1000× magnification). (D-E) Statistical analysis of fluorescence puncta of autolysosome (free red) and autophagosome (yellow) in (Figure 6H) and (C). (F) WB analysis of ATG5, METTL3 and LC3B expression after ATG5 knockdown in DLD1 cells without serum supplementation. (G) The expression of LINC01615 after 3-MA, ATG5 knockdown and Baf A1 treatment in DLD1 cells without serum supplementation. (H) WB analysis of METTL3 and LC3B expression in LoVo cells treated with or without Baf-A1 under serum-free starvation conditions. (I) Co-IP analysis was performed with specific antibodies against HA and Flag in 293T cells under normal or serum-free starvation conditions after transfection of HA-METTL3 and Flag-LC3B plasmids. WB analysis of the interaction between METTL3 and LC3B. (J) Representative confocal microscopy images of METTL3, LC3B and LAMP1 distribution in DLD1 cells under serum-free starvation conditions (1000× magnification). Data are the means ± SD (n = 3 independent experiments), * p<0.05, ** p<0.01. (TIF 11211 kb)
18_2022_4675_MOESM7_ESM.tif
Supplementary file7 Supplementary Figure 6 (A) qRT-PCR was used to detect the expression of LINC01615 in two donor patients’ tumor tissues. (B) PDXs images of control group, sh-LINC01615 group, oxaliplatin group, and sh-LINC01615 combined with oxaliplatin group. (C) The expression levels of LINC01615 in PDX tumors of control group, sh-LINC01615 group, oxaliplatin group, and sh-LINC01615 combined with oxaliplatin group through qRT–PCR. (D) Statistical analysis of IHC staining scores in (Figure 7F). (E) WB analysis of LC3B and METTL3 expression in sh-Ctrl and sh-LINC01615 group treated with or without oxaliplatin. Data are the means ± SD (n = 3 independent experiments), * p<0.05, ** p<0.01. (TIF 3063 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Y., Xu, L., Ren, Z. et al. LINC01615 maintains cell survival in adaptation to nutrient starvation through the pentose phosphate pathway and modulates chemosensitivity in colorectal cancer. Cell. Mol. Life Sci. 80, 20 (2023). https://doi.org/10.1007/s00018-022-04675-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00018-022-04675-7