Abstract
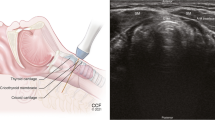
We compared intraoperative ultrasound (IOUS) to preoperative high-resolution real-time ultrasound in 25 consecutive patients undergoing reoperations for primary hyperparathyroidism. Intraoperative neck scanning was performed after the platysma muscle flaps were raised, and one or both sides of the neck were opened along the medial border of the sternocleidomastoid muscle. Preoperative localization studies were used to determine which side of the neck to explore. Pathologic parathyroid glands appeared sonolucent on both pre- and intraoperative ultrasound. Glands were always imaged in 2 planes.
Neither preoperative nor intraoperative scans were able to image normal parathyroid glands. Preoperative scans were correct for abnormal tissue in 9 patients, and intraoperative scans were correct in 19 patients (p=0.01).Size of a pathologic parathyroid gland was not a factor in the ability of IOUS to detect it, but location was. Intrathyroidal and inferior glands were detected reliably, but superior glands were missed (33%). If IOUS imaged the pathologic parathyroid tissue, the length of the surgical procedure was significantly reduced [5.9 hours versus 3.1 hours (p= 0.005)].IOUS did not appear to impact on ultimate outcome as 5 of 6 patients in whom IOUS failed to image the pathologic gland had successful surgery without complication.
Résumé
Les auteurs ont comparé les données de l'ultrasonographie préopératoire à celles de l'ultrasonographie opératoire chez 25 malades qui atteints d'hyperparathyroïdisme primitif ont du être réopérés après échec de la première intervention. L'ultrasonographie opératoire fut pratiquée après dissection des lambeaux de platysma musculaire et abord d'un ou des deux côtés du cou par incision cervicale tracée au niveau du bord axial du sternocléido-mastoidien. Avant l'intervention l'examen du cou avait été pratiqué pour déterminer le côté à explorer. Les parathyroïdes pathologiques se sont traduites par une image anormale au cours des 2 explorations. Les images furent obtenues en 2 plans. Elles firent défaut quand les parathyroïdes étaient normales. L'ultrasonographie préopératoire fut exacte chez 9 malades qui présentaient des parathyroïdes pathologiques et l'ultrasonographie opératoire fut exacte chez 19 opérés (p=0.01). L'habilité de la méthode pour déceler la lésion ne dépend pas de la taille de la parathyroïde pathologique mais de son siège. Les parathyroïdes intrathyroïdiennes et sous-thyroïdiennes anormales furent démasquées mais celles situées haut ne furent pas décelées dans 33% des cas. Lorsque l'échographie décela la lésion la durée de l'intervention fut notablement réduite (de 5.9 heures elle passa à 3.1 heures (p =0.005)) mais au total elle n'intervient pas sur la destinée de l'intervention puisque dans 5 des 6 cas où ses résultats avaient été négatifs la glande anormale fut découverte par le chirurgien et extirpée avec succès et sans complication.
Resumen
Hemos comparado la ultrasonografía de alta resolución de tiempo real intraoperatoria (USIO) con la preoperatoria en 25 pacientes sometidos a reoperación por hiperparatiroidismo primario. La ultrasonografía del cuello fue realizada después de levantar los colgajos del músculo cutáneo y una vez que uno o ambos lados del cuello fueron disecados a lo largo del borde interno del esternocleidomastoideo. Los estudios preoperatorios de localización fueron utilizados para determinar qué lado del cuello debería ser explorado. Las glándulas paratiroides anormales aparecieron sonolucientes tanto a la ultrasonografía precomo intraoperatoria. Las imágenes de las glándulas fueron siempre obtenidas en 2 pianos. No se logró visualizar glándulas paratiroides normales ni en el examen preni en el intraoperatorio. Los exámenes preoperatorios dieron resultados correctos para tejido paratiroideo anormal en 9 pacientes, y los intraoperatorios en 19 pacientes (p=0.01). El tamaño de la glándula paratiroidea anormal no fue un factor determinante de la capacidad de la USIO para su detección, pero sí lo fue la ubicación. Las glándulas paratiroideas en ubicación intratiroidea o inferior pudieron ser detectadas en forma confiable, pero las de ubicación superior se escaparon a la detección (33%). Cuando la USIO logró demostrar el tejido paratiroideo anormal, el procedimiento operatorio se acortó en forma significativa (5.9 horas versus 3.1 horas,p=0.005). La USIO no parece determinar el resultado final de operación, puesto que 5 de 6 pacientes en quienes la USIO falló en la demostración de glándulas anormales fueron operados sin complicación.
Similar content being viewed by others
References
Brennan, M.F.: Reoperation for suspected hyperparathyroidism. Clinical Surgery International, vol. 4. Surgery of the Thyroid and Parathyroid Glands. New York, Churchill-Livingston, 1983, pp. 168–176
Wang, C.A.: Parathyroid re-exploration. Ann. Surg.186:140, 1977
Billings, P.J., Milroy, E.J.D.: Reoperative parathyroid surgery. Br. J. Surg.70:542, 1983
Edis, A.J., Sheedy, P.F., Beahrs, O.H.: Results of reoperation for hyperparathyroidism, with evaluation of preoperative localization studies. Surgery84:384, 1978
Saxe, A.W., Brennan, M.F.: Reoperative parathyroid surgery for primary hyperparathyroidism caused by multiple gland disease: Total parathyroidectomy and autotransplantation with cryopreserved tissue. Surgery91:616, 1982
Brennan, M.F., Norton, J.A.: Reoperation for persistent and recurrent hyperparathyroidism. Ann. Surg.201:40, 1985
Patow, C.A., Norton, J.A., Brennan, M.F.: Vocal cord paralysis and reoperative parathyroidectomy, a prospective study. Surg. Forum35:553, 1984
Edis, A.J., Evans, T.C.: High-resolution, real-time ultrasonography in the preoperative location of parathyroid tumors, a pilot study. N. Engl. J. Med.301:532, 1979
Egdahl, R.H.: Preoperative parathyroid localization. N. Engl. J. Med.301:548, 1979
Clark, O.H., Stark, D.D., Gooding, G.A., Moss, A.A., Arnaud, S.B., Newton, T.H., Norman, D., Bank, W.O., Arnaud, C.D.: Localization procedures in patients requiring reoperation for hyperparathyroidism. World J. Surg.8:509, 1984
Krudy, A.G., Shawker, T.H., Doppman, J.L., Horvath, K., Schneider, P.D., Norton, J.A., Marx, S.J., Spiegel, A.M.: Ultrasonic parathyroid localization in previously operated patients. Clin. Radiol.35:113, 1984
Sigel, B., Duarte, B., Coelho, J.C.U., Nyhus, L.M., Baker, R.J., Machi, J.: Localization of insulinomas of the pancreas at operation by real-time ultrasound scanning. Surg. Gynecol. Obstet.156:145, 1983
Norton, J.A., Sigel, B., Baker, A.R., Ettinghausen, S.E., Shawker, T.H., Krudy, A.G., Doppman, J.L., Taylor, S.I., Gordon, P.: Localization of an occult insulinoma by intraoperative ultrasonography. Surgery97:381, 1985
Sigel, B., Kraft, A.R., Nyhus, L.M., Coelho, J.C.U., Gavin, M.P., Spigos, D.G.: Identification of a parathyroid adenoma by operative ultrasonography. Arch. Surg.116:234, 1981
Charboneau, J.W., Grant, C.S., James, E.M., Goellner, J.R., Hodgson, S.F.: High-resolution ultrasound-guided percutaneous needle biopsy and intraoperative ultrasonography of the cervical parathyroid adenoma in a patient with persistent hyperparathyroidism. Mayo Clin. Proc.58:497, 1983
Norton, J.A., Brennan, M.F., Saxe, A.W., Wesley, R.A., Doppman, J.L., Krudy, A.G., Marx, S.J., Santora, A.C., Hicks, M., Aurbach, G.D., Spiegel, A.M.: Intraoperative urinary cyclic adenosine monophosphate as a guide to successful reoperative parathyroidectomy. Ann. Surg.200:389, 1984
Sigel, B., Coelho, J.C.U., Nyhus, L.M., Velasco, J.M., Donahue, P.E., Wood, D.K., Spigos, D.G.: Detection of pancreatic tumors by ultrasound during surgery. Arch. Surg.117:1058, 1982
van Heerden, J.A., James, E.M., Karsell, T.R., Charboneau, J.W., Grant, C.S., Purnell, D.C.: Small-part ultrasonography and primary hyperparathyroidism. Ann. Surg.195:774, 1982
Wang, C.A.: The anatomic basis of parathyroid surgery. Ann. Surg.183:271, 1976
Wells, S.A., Jr., Leight, G.F., Ross, A.: Primary hyperparathyroidism. Curr. Probl. Surg.17:398, 1980
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Norton, J.A., Shawker, T.H., Jones, B.L. et al. Intraoperative ultrasound and reoperative parathyroid surgery: An initial evaluation. World J. Surg. 10, 631–638 (1986). https://doi.org/10.1007/BF01655542
Issue Date:
DOI: https://doi.org/10.1007/BF01655542