Abstract
To provide an in vitro estimation of the pressure drop across tracheal tubes (ΔPTT) in the face of given pulsatile frequencies and peak pressures (Pwork) delivered by a high-frequency percussive ventilator (HFPV) applied to a lung model. Tracheal tubes (TT) 6.5, 7.5 and 8.0 were connected to a test lung simulating the respiratory system resistive (R = 5, 20, 50 cmH2O/L/s) and elastic (C = 10, 20, and 50 mL/cmH2O) loads. The model was ventilated by HFPV with a pulse inspiratory peak pressure (work pressure Pwork) augmented in 5-cmH2O steps from 20 to 45 cmH2O, yielding 6 diverse airflows. The percussive frequency (f) was set to 300, 500 and 700 cycles/min, respectively. Pressure (Paw and Ptr) and flow (V’) measurements were performed for all 162 possible combinations of loads, frequencies, and work pressures for each TT size, thus yielding 486 determinations. For each respiratory cycle ΔPTT was calculated by subtracting each peak Ptr from its corresponding peak Paw. A non-linear model was constructed to assess the relationships between single parameters. Performance of the produced model was measured in terms of root mean square error (RMSE) and the coefficient of determination (r2). ΔPTT was predicted by Pwork (exponential Gaussian relationship), resistance (quadratic and linear terms), frequency (quadratic and linear terms) and tube diameter (linear term), but not by compliance. RMSE of the model on the testing dataset was 1.17 cmH2O, r2 was 0.79 and estimation error was lower than 1 cmH2O in 68% of cases. As a result, even without a flow value, the physician would be able to evaluate ΔPTT pressure. If the present results of our bench study could be clinically confirmed, the use of a nonconventional ventilatory strategy as HFPV, would be safer and easier.
Similar content being viewed by others
1 Introduction
During mechanical ventilation the pressure drop across the tracheal tube (ΔPTT) may dissipate an important amount of flow-dependent energy that could otherwise be used to inflate the patient [1,2,3]. Hence, peak pressure delivered by the ventilator does not correspond to the pressure actually present in the patient’s trachea. The latter is not commonly measured in a clinical setting because an extra pressure measuring device is required or a dedicated ventilator software that may estimate ΔPTT is needed. In this context, an exceedingly high ventilator-generated pressure may not indicate an elevated tracheal pressure (Ptr) because of the pressure drop owing to the tube connecting them. As a result, the estimation of ΔPTT may be very useful to the clinician, especially to avoid the development of barotrauma [4, 5] and to adequately apply the lung ventilatory protective strategy [6,7,8].
High-frequency percussive ventilation (HFPV) is characterized by a pulsatile flow delivery that determines the device’s working pressure (PWork) which is displayed on ventilator’s monitor [9]. Furthermore, the performance of the HFPV varies according to the physiological/physical feedback, i.e., resistive and elastic loads and corresponding time constants [10,11,12]. However, airflow (V’) value is not given [9,10,11,12], thus rendering impossible the estimation of ΔPTT by means of a flow-dependent model, e.g., Rohrer’s [13], taking into account the flow-dependency of tracheal tubes [3, 14]. To overcome this limitation a portable instrument has been proposed to measure flow during HFPV but it cannot estimate ΔPTT [15]. Recently, a model to calculate ΔPTT based on flow and Blasius’ constant has been described [16]. Even though it is very robust the flow measurement is mandatory, which may be difficult to perform in some clinical scenarios.
The aim of this study is to provide an in vitro estimation of ΔPTT, based on the ventilator set parameters (pulsatile frequencies, work pressure, displayed on ventilator’s monitor) and internal tube diameter, that could be clinically used in different mechanical loads.
2 Materials and methods
2.1 Experimental setup and measurements
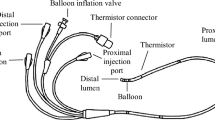
Figure 1 depicts the experimental setup used. A physical test lung (ACCU LUNG, Fluke Biomedical, Everett, WA, USA) was used to simulate the respiratory system loads, namely, resistive (R = 5, 20, 50 cmH2O/L/s) and elastic loads (C = 10, 20, and 50 mL/cmH2O). A high-frequency percussive ventilator (VDR-4, Percussionaire Corporation, Sandpoint, ID, USA) provided the ventilation. The inlet of a tracheal tube (TT, Rusch, Milan, Italy) with internal diameters (TTD) of 6.5, 7.5 and 8.0 mm was connected to the ventilator and pressure at this point (Paw) was measured by a differential pressure transducer (ASCX01DN, Honeywell, Morristown, NJ, USA) via a sideport. The distal end of the tracheal tube was indwelled into artificial trachea and the cuff was inflated to avoid leaks. The pressure distal to the TT (Ptr) was also measured by another pressure transducer (ASCX01DN, Honeywell, Morristown, NJ, USA). Flow (V’) was measured between the TT and the test lung by a pneumotachograph (Fleisch no. 2, Lausanne, Switzerland) connected to a differential pressure transducer (0.25 INCH-D-4V, All Sensors, Morgan Hill, CA, USA). The flow and pressure signals were fed into a 12-bit analog-to-digital converter (PCI-6023E, National Instrument, Austin, TX, USA), sampled at 2 kHz and low-passed filtered (second order Butterworth filter) at a cut-off frequency of 35 Hz. V’ signal was digitally integrated to generate volume [12, 15].
The VDR-4 ventilator delivered a pulse inspiratory/expiratory (i/e) duration ratio of 1:1, and inspiratory and expiratory duration (I/E) ratio of 1:1 [9, 10]. The work pressure was augmented in 5-cmH2O steps from 20 to 45 cmH2O, yielding 6 diverse airflows. The percussive frequency (f) was set to 300, 500 and 700 cycles/min, corresponding to 5, 8.33 and 11.67 Hz, respectively. Measurements were performed for all 162 possible combinations of loads, frequencies, and work pressures for each TT size, thus yielding 486 determinations. For each measurement setting two repeated measurements of a single respiratory cycle were performed in order to create two datasets: training and testing dataset. The training dataset was used to create the model while testing dataset was used to test model on new unseen data. For each respiratory cycle ΔPTT was calculated by subtracting each peak Ptr from its corresponding peak Paw (Fig. 2) : ΔPTT = Pawpeak − Ptrpeak. Concomitantly, peak flows (V’peak) were also measured.
From top to bottom: Pressures (Paw and Ptr, tube inlet and distal tube pressures, respectively), flow and pressure drop tracings during a single respiratory cycle. Circles indicate peak pressures during end-inspiratory plateau phase ΔPTT = Pawpeak − Ptrpeak; Pwork = 20 cmH2O, f = 300 cycles/min, R = 5 cmH2O/L/s, C = 20 mL/cmH2O, tube diameter 7.5 mm
2.2 Modeling and analysis
Preliminary analysis was conducted by using the training dataset and assessing the relationships between single parameters (i.e., pulsatile frequencies—f, work pressures—Pwork; respiratory system resistance—R and compliance—C; TT diameter—TTD) and ΔPTT. As a result of this preliminary analysis, a non-linear model was constructed and subsequently its parameters were identified by non-linear least squares method [17, 18]. In order to evaluate the model fitting, the estimated values were compared to measured ΔPTT by means of root mean square error (RMSE) and the coefficient of determination (r2). The predictive power of the model was also evaluated on the previously unseen testing dataset, calculating RMSE and r2. Signal processing and data analysis were conducted using scripts developed in MATLAB (Matlab, Mathworks Inc., Natick, MA, USA).
3 Results
The results of preliminary analysis showed that ΔPTT is predicted by Pwork (exponential Gaussian relationship), resistance (quadratic and linear terms), frequency (quadratic and linear terms) and tube inner diameter (linear term), but not by compliance. Thus the constructed model with identified parameters can be defined as:
where R, Pwork, f and TTD are expressed in cmH2O/L/s, cmH2O, Hz, and mm, respectively.
ΔPTT data calculated by the produced model were plotted against corresponding measured points in order to demonstrate the adequacy of the model to fit the experimental data on training dataset (Fig. 3). The results showed dispersion around identity line between measured and estimated data. The RMSE on training dataset was 1.18 cmH2O, r2 was 0.79 and estimation error was lower than 1 cmH2O in 69% of cases (points between dashed lines). In order to assess the performance of the model on previously unseen testing dataset, predictedΔPTT values were plotted versus those actually measured (Fig. 3). The estimation errors on testing dataset were very close to those obtained on training dataset (RMSE = 1.17 cmH2O; r2 = 0.79; 68% errors lower than 1 cmH2O) indicating good predictive power of the constructed model. The RMSE values were similar among tubes, slightly smaller for smaller size tubes (1.08, 1.14 and 1.29 cmH2O for 6.5, 7.5 and 8 mm tube, respectively).
4 Discussion
HFPV, a non-conventional high frequency ventilatory strategy, was recently reconsidered [19,20,21,22]. However, the lack of flow and volume measurement, as well as discordance in the reported tidal volumes between in-vitro HFPV studies [12, 23] induced skepticism and disaffection among the physicians [20]. A recent bench study [20] revisited conflicting results and interpretations from literature and reported tidal volumes similar to the ones reported in Lucangelo et al. [10, 12], not supporting the conclusions of Allan [23] that HFPV delivers injurious tidal volume under typical settings. In addition, another recent study showed that HFPV improves alveolar recruitment, gas exchanges and hemodynamics of patients with early non-focal ARDS without relevant hyperinflation and that pleural pressures are well below the HFPV work pressure, displayed on ventilator’s monitor [19]. For these reason the estimation of tracheal tube contribution to airway peak pressure is of paramount importance to avoid damage to the lung during mechanical ventilation [3], as well as to adequately apply the lung ventilatory protective strategy [6,7,8] and avoid under-treatment. Several models have been proposed to estimate pressure drop across the tracheal tube during artificial ventilation [3, 4, 13, 16]. However, all of them depend on flow measurement that is not present in high frequency percussive ventilators. Thus, a model that does not require flow measurement is clinically wanted. For this purpose, we developed a model able to predict ΔPTT considering only the parameters set and available on the HFPV ventilator associated with tracheal tube size and patient resistance.
Preliminary analysis disclosed the complex ΔPTT dependency on ventilatory and respiratory parameters, especially on Pwork and R. In particular, ΔPTT showed exponential Gaussian relationship whose amplitude depended on resistance value (quadratic and linear terms) (Fig. 4). Specific exponential dependency of ΔPTT on Pwork results from the complex flow delivery and feedback intrinsic to the HFPV ventilator. The set work pressure in VDR-4® is obtained by adjusting pulsatile flow rate that feeds the Phasitron®. Indeed, the latter employs a sliding flow regulator based on the Venturi logic that modulates flow delivery as function of inbound pulsatile flow and backpressure generated by output impedance [9,10,11,12, 24].
Relationship between peak pressure drop across the tracheal tube (ΔPTT) and peak airway work pressure (Pwork) and resistive load (R). All calculated 486 data points are presented. The grid surface describes the exponential Gaussian relationship and the quadratic model behavior expressed by the first term (0.0037 × R2 – 0.35 × R + 8.63) × e−(Pwork−26.21)/14.47 of model reported in Eq. 1. The points dispersion around the grid is the expression of frequency and tube diameter variation considered by the final part of Eq. 1 (– 0.026 × f 2 + 0.54 × f ) – 0.34 × TTD and the estimation error
To better describe the interplay between flow delivery, resistance load and Pwork we plotted peak flow against work pressures generated using the experimental lung model resistances (R = 5, 20, 50 cmH2O), as well as simulating R = 0 and ∞ cmH2O by open circuit and closed tube, respectively (Fig. 5). Depending on the load the measured peak flow varied with the working pressures measured by ventilator. When the system was open (no load, R = 0 cmH2O/L/s) there was no backpressure and flow increased linearly; the corresponding pressures represented Pwork measured by the ventilator. On the contrary, when the system was closed flow tends to zero; the corresponding pressure represented the high backward pressure produced by infinite resistance load. For the intermediate load values the pressure-flow relationships were curvilinear. The larger was the load the lower was the curve.
ΔPTT also depended on frequency, the relationship was curvilinear with a downward concavity and could be represented by (– 0.026 × f 2 + 0.54 × f ). In high frequency ventilation techniques without feedback, pressure drop increases with frequency [25, 26] because inertial effects increase total tube impedance. Additionally, the servo control mechanism of HFPV reduces flow delivery with increasing frequency due to the frequency dependent airway pressure increment.
ΔPTT presented an inverse linear relationship with tube diameter. Previous studies reported a non-linear relationship between flow and pressure across the TT [3, 25,26,27]. In our case the contribution of TT diameter was small enough to allow a linear approximation to its influence on ΔPTT. Our model did not depend on C to explain the mechanical properties of TT.
High frequency ventilation modalities can develop an intrinsic PEEP. Since the HFPV ventilatory circuit is open and that auto-PEEP during HFPV was previously observed only under extreme conditions (R = 200 cmH2O/L/s, C = 10 mL/cmH2O and R = 200 cmH2O/L/s, C = 20 mL/cmH2O) [10] not encountered in patients, the auto-PEEP was not considered in the present study.
The tubes sizes used in this study were chosen because they are the most frequently used in adolescent and adult patients. Lung simulator loads were chosen to represent normal subjects, obstructive and restrictive patients. In elevated patients resistive load, ΔPTT contributes a small fraction of the total pressure generated in the system and could be considered clinically, irrelevant during HFPV. On the other hand, ΔPTT should be clinically considered more important in patients presenting less severe resistive load.
Our study presents some limitation: range of loads, frequencies and tracheal tubes used.
5 Conclusion
This study propose an innovative approach to ΔPTT estimation without flow measurement during HFPV. If these results could be confirmed in a further clinical study, the use of a nonconventional ventilatory strategy as HFPV would be safer and easier. These clinical information could be used to adequately tailor HFPV in era of ventilatory protective ventilation.
References
Bersten AD, Rutten AJ, Vedig AE, Skowwronski GA. Additional work of breathing imposed by endotracheal tubes, breathing circuits, and intensive care ventilators. Crit Care Med. 1989;17:671–7.
Shapiro M, Wilson RK, Casar G, Bloom K, Teague RB. Work of breathing through different sized endotracheal tubes. Crit Care Med. 1980;14:1028–31.
Rocco PRM, Zin WA. Modelling the mechanical effects of tracheal tubes in normal subjects. Eur J Physiol. 1995;8:121–6.
Conti G, De Blasi RA, Lappa A, Ferretti A, Antonelli M, Bufi M, Gasparetto A. Evaluation of respiratory system resistance in mechanically ventilated patients: the role of the endotracheal tube. Intensive Care Med. 1994;20:421–4.
Gammon RB, Shin MS, Buchalter SE. Pulmonary barotrauma in mechanical ventilation. Patterns and risk factors. Chest. 1992;102:568–72.
Santschi M, Randolph AG, Rimensberger PC, Jouvet P. Mechanical ventilation strategies in children with acute lung injury: a survey on stated practice pattern. Pediatr Crit Care Med. 2013;14:e332–7.
Petrucci N, De Feo C. Lung protective ventilation strategy for the acute respiratory distress syndrome. Cochrane Database Syst Rev. 2013;2:CD003844.
Ajčević M, Lucangelo U, Accardo A. Tailoring of HFPV Treatment by Respiratory Parameters Measurement. In: Mindedal H, Persson M, editors 16th Nordic-Baltic Conference on Biomedical Engineering. IFMBE Proceedings, vol 48. Springer, Cham; 2015. pp 9–12. https://doi.org/10.1007/978-3-319-12967-9_3.
Lucangelo U, Fontanesi L, Antonaglia V, Pellis T, Berlot G, Liguori G, Bird FM, Gullo A. High frequency percussive ventilation (HFPV). Principles technique. Miner Anestesiol. 2003;69:841–51.
Lucangelo U, AntonagliaV, Zin WA, Berlot G, Fontanesi L, Peratoner A, Bird FM, Gullo A. Effects of mechanical load on flow, volume and pressure delivered by high-frequency percussive ventilation. Respir Physiol Neurobiol. 2004;142:81–91.
Lucangelo U, Accardo A, Bernardi A, Ferluga M, Borelli M, Antonaglia V, Riscica F, Zin WA. Gas distribution in a two-compartment model ventilated in high-frequency percussive and pressure-controlled modes. Intensive Care Med. 2010;36(12):2125–31.
Lucangelo U, Antonaglia V, Zin WA, Berlot G, Fontanesi L, Peratoner A, Bernabe` F, Gullo A. Mechanical loads modulate tidal volume and lung washout during high-frequency percussive ventilation. Respir Physiol Neurobiol. 2006;150:44–51.
Rohrer F. Der Stroemungswiderstand in den menschlichen Atemwegen und der Einfluss der unregelmaessigen Verzweigung des Bronchialsystems auf den Atmungsverlauf in verschiedenen Lungenbezirken. Pflug Arch Gesamte Physiol Menschen Tiere. 1915;162:225–59.
Behrakis PK, Higgs BD, Baydur A, Zin WA, Milic-Emili J. Respiratory mechanics during halothane anestesia and anesthesia-paralysis in humans. J Appl Physiol. 1983;55:1085–92.
Riscica F, Lucangelo U, Accardo A. Portable instrument for the volume measurement of high-frequency percussive ventilators—biomed 2010. Biomed Sci Instrum. 2010;46:93–8.
Ajčević M, Lucangelo U, Ferluga M, Zin WA, Accardo A. In vitro estimation of pressure drop across tracheal tubes during high-frequency percussive ventilation. Physiol Meas. 2014;35:177–88.
Coleman TF, Li Y. On the convergence of reflective Newton methods for large-scale nonlinear minimization subject to bounds. Math Program. 1994;67(2):189–224.
Coleman TF, Li Y. An interior, trust region approach for nonlinear minimization subject to bounds. SIAM J Optim. 1996;6:418–45.
Godet T, Jabaudon M, Blondonnet R, Tremblay A, Audard J, Rieu B, Pereira B, Garcier JM, Futier E, Constantin JM. High frequency percussive ventilation increases alveolar recruitment in early acute respiratory distress syndrome: an experimental, physiological and CT scan study. Crit Care. 2018;22(1):3. https://doi.org/10.1186/s13054-017-1924-6.
Dutta R, Xing T, Swanson C, Heltborg J, Murdoch GK. Comparison of flow and gas washout characteristics between pressure control and high frequency percussive ventilation using a test lung. Physiol Meas. 2018;39(3):035001. https://doi.org/10.1088/1361-6579/aaaaa2.
Wong I, Worku B, Weingarten JA, Ivanov A, Khusid F, Afzal A, Tranbaugh RF, Gulkarov I. High-frequency percussive ventilation in cardiac surgery patients failing mechanical conventional ventilation. Interact Cardiovasc Thorac Surg. 2017;25(6):937–41.
Miller AC, Ferrada PA, Kadri SS, Nataraj-Bhandari K, Vahedian-Azimi A, Quraishi SA. High-frequency ventilation modalities as salvage therapy for smoke inhalation–associated acute lung injury: a systematic review. J Intensive Care Med. 2018;33(6):335–45. https://doi.org/10.1177/0885066617714770.
Allan PF. High-frequency percussive ventilation: pneumotachograph validation and tidal volume analysis. Respir Care. 2010;55:734–40.
Fornasa E, Ajčević M, Accardo A. Characterization of the mechanical behavior of intrapulmonary percussive ventilation. Physiol Meas. 2013;34(12):1583. https://doi.org/10.1088/0967-3334/34/12/1583.
Shumann S, Krappitz M, Moeller K, Hentschel R, Braun G, Guttmann J. Pressure loss caused by pediatric endotracheal tubes during high frequency oscillation ventilation. Respir Physiol Neurobiol. 2008;162:132–7.
Smallwood CD, Bullock KJ, Gouldstone A. Pressure attenuation during high-frequency airway clearance therapy across different size endotracheal tubes: an in vitro study. J Crit Care. 2016;34:142–5.
Guttmann J, Eberhard L, Fabry B, Bertschmann W, Wolff G. Continuous calculation of intratracheal pressure in tracheally intubated patients. Anesthesiology. 1993;79:503–13.
Funding
The study was funded exclusively by University of Trieste research funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Because the measurements involved only the ICU ventilator and lung test model without affecting patents in anyway, no IRB approval was sought.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lucangelo, U., Ajčević, M., Lena, E. et al. On some factors determining the pressure drop across tracheal tubes during high-frequency percussive ventilation: a flow-independent model. J Clin Monit Comput 35, 885–890 (2021). https://doi.org/10.1007/s10877-020-00548-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00548-1