Abstract
Background
Hepatic pedicle clamping (HPC) is frequently utilized during hepatectomy to reduce intraoperative bleeding and diminish the need for intraoperative blood transfusion (IBT). The long-term prognostic implications of HPC following hepatectomy for hepatocellular carcinoma (HCC) remain under debate. This study aims to elucidate the association between HPC and oncologic outcomes after HCC resection, stratified by whether IBT was administered.
Patients and Methods
Prospectively collected data on patients with HCC who underwent curative resection from a multicenter database was studied. Patients were stratified into two cohorts on the basis of whether IBT was administered. The impact of HPC on long-term overall survival (OS) and recurrence-free survival (RFS) between the two cohorts was assessed by univariable and multivariable Cox regression analyses.
Results
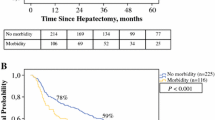
Of 3362 patients, 535 received IBT. In the IBT cohort, using or not using HPC showed no significant difference in OS and RFS outcomes (5-year OS and RFS rates 27.9% vs. 24.6% and 13.8% vs. 12.0%, P = 0.810 and 0.530). However, in the non-IBT cohort of 2827 patients, the HPC subgroup demonstrated significantly decreased OS (5-year 45.9% vs. 56.5%, P < 0.001) and RFS (5-year 24.7% vs. 33.3%, P < 0.001) when compared with the subgroup without HPC. Multivariable Cox regression analysis identified HPC as an independent risk factor of OS and RFS [hazard ratios (HR) 1.16 and 1.12, P = 0.024 and 0.044, respectively] among patients who did not receive IBT.
Conclusions
The impact of HPC on the oncological outcomes following hepatectomy for patients with HCC differed significantly whether IBT was administered, and HPC adversely impacted on long-term survival for patients without receiving IBT during hepatectomy.



Similar content being viewed by others
References
Vogel A, Meyer T, Sapisochin G, Salem R, Saborowski A. Hepatocellular carcinoma. Lancet. 2022;400:1345–62.
Chen H, Jia W. Progress in hepatectomy for hepatocellular carcinoma and peri-operation management. Genes Dis. 2020;7:320–7.
Gunasekaran G, Bekki Y, Lourdusamy V, Schwartz M. Surgical treatments of hepatobiliary cancers. Hepatology. 2021;73(Suppl 1):128–36.
Katz SC, Shia J, Liau KH, Gonen M, Ruo L, Jarnagin WR, et al. Operative blood loss independently predicts recurrence and survival after resection of hepatocellular carcinoma. Ann Surg. 2009;249:617–23.
Rana A, Petrowsky H, Hong JC, Agopian VG, Kaldas FM, Farmer D, et al. Blood transfusion requirement during liver transplantation is an important risk factor for mortality. J Am Coll Surg. 2013;216:902–7.
Yang T, Liu K, Liu CF, Zhong Q, Zhang J, Yu JJ, et al. Impact of postoperative infective complications on long-term survival after liver resection for hepatocellular carcinoma. Br J Surg. 2019;106:1228–36.
Pringle JHV. Notes on the arrest of hepatic hemorrhage due to trauma. Ann Surg. 1908;48:541–9.
Simillis C, Li T, Vaughan J, Becker LA, Davidson BR, Gurusamy KS. A cochrane systematic review and network meta-analysis comparing treatment strategies aiming to decrease blood loss during liver resection. Int J Surg. 2015;23:128–36.
Chen GX, Qi CY, Hu WJ, Wang XH, Hua YP, Kuang M, et al. Perioperative blood transfusion has distinct postsurgical oncologic impact on patients with different stage of hepatocellular carcinoma. BMC Cancer. 2020;20:487.
Tai YH, Wu HL, Mandell MS, Tsou MY, Chang KY. The association of allogeneic blood transfusion and the recurrence of hepatic cancer after surgical resection. Anaesthesia. 2020;75:464–71.
Cata JP, Wang H, Gottumukkala V, Reuben J, Sessler DI. Inflammatory response, immunosuppression, and cancer recurrence after perioperative blood transfusions. Br J Anaesth. 2013;110:690–701.
Vamvakas EC, Blajchman MA. Transfusion-related immunomodulation (TRIM): an update. Blood Rev. 2007;21:327–48.
Farid SG, White A, Khan N, Toogood GJ, Prasad KR, Lodge JP. Clinical outcomes of left hepatic trisectionectomy for hepatobiliary malignancy. Br J Surg. 2016;103:249–56.
Khajeh E, Shafiei S, Al-Saegh SA, Ramouz A, Hammad A, Ghamarnejad O, et al. Meta-analysis of the effect of the pringle maneuver on long-term oncological outcomes following liver resection. Sci Rep. 2021;11:3279.
Lin N, Li J, Ke Q, Xin F, Zeng Y, Wang L, et al. Does the intermittent Pringle maneuver affect the recurrence following surgical resection for hepatocellular carcinoma? A systematic review. PLoS One. 2020;15:e0229870.
Wei X, Zheng W, Yang Z, Liu H, Tang T, Li X, et al. Effect of the intermittent Pringle maneuver on liver damage after hepatectomy: a retrospective cohort study. World J Surg Oncol. 2019;17:142.
Famularo S, Giani A, Di Sandro S, Sandini M, Giacomoni A, Pinotti E, et al. Does the Pringle maneuver affect survival and recurrence following surgical resection for hepatocellular carcinoma? A western series of 441 patients. J Surg Oncol. 2018;117:198–206.
van der Bilt JD, Kranenburg O, Nijkamp MW, Smakman N, Veenendaal LM, Te Velde EA, et al. Ischemia/reperfusion accelerates the outgrowth of hepatic micrometastases in a highly standardized murine model. Hepatology. 2005;42:165–75.
van der Bilt JD, Kranenburg O, Borren A, van Hillegersberg R, Borel Rinkes IH. Ageing and hepatic steatosis exacerbate ischemia/reperfusion-accelerated outgrowth of colorectal micrometastases. Ann Surg Oncol. 2008;15:1392–8.
Agrawal S, Belghiti J. Oncologic resection for malignant tumors of the liver. Ann Surg. 2011;253:656–65.
Brown ZJ, Tsilimigras DI, Ruff SM, Mohseni A, Kamel IR, Cloyd JM, et al. Management of hepatocellular carcinoma: a review. JAMA Surg. 2023;158:410–20.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–9.
Zhou J, Sun H, Wang Z, Cong W, Wang J, Zeng M, et al. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (2019 Edition). Liver Cancer. 2020;9:682–720.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Bland JM, Altman DG. The logrank test. BMJ. 2004;328:1073.
Gill RD. Multistate life-tables and regression models. Math Popul Stud. 1992;3:259–76.
Xia F, Lau WY, Xu Y, Wu L, Qian C, Bie P. Does hepatic ischemia-reperfusion injury induced by hepatic pedicle clamping affect survival after partial hepatectomy for hepatocellular carcinoma. World J Surg. 2013;37:192–201.
Wassmer CH, Moeckli B, Berney T, Toso C, Orci LA. Shorter survival after liver pedicle clamping in patients undergoing liver resection for hepatocellular carcinoma revealed by a systematic review and meta-analysis. Cancers (Basel). 2021;13:637.
Hao S, Chen S, Yang X, Wan C. Adverse impact of intermittent portal clamping on long-term postoperative outcomes in hepatocellular carcinoma. Ann R Coll Surg Engl. 2017;99:22–7.
Wang CC, Iyer SG, Low JK, Lin CY, Wang SH, Lu SN, et al. Perioperative factors affecting long-term outcomes of 473 consecutive patients undergoing hepatectomy for hepatocellular carcinoma. Ann Surg Oncol. 2009;16:1832–42.
Tung-Ping Poon R, Fan ST, Wong J. Risk factors, prevention, and management of postoperative recurrence after resection of hepatocellular carcinoma. Ann Surg. 2000;232:10–24.
Yang F, Zhang Y, Ren H, Wang J, Shang L, Liu Y, et al. Ischemia reperfusion injury promotes recurrence of hepatocellular carcinoma in fatty liver via ALOX12-12HETE-GPR31 signaling axis. J Exp Clin Cancer Res. 2019;38:489.
Chen H, Lu D, Yang X, Hu Z, He C, Li H, et al. One shoot, two birds: alleviating inflammation caused by ischemia/reperfusion injury to reduce the recurrence of hepatocellular carcinoma. Front Immunol. 2022;13:879552.
Kamel YA, Sasa NAG, Helal SM, Attallah HA, Yassen KA. Monitoring the effects of automated gas control of sevoflurane versus target-guided propofol infusion on hemodynamics of liver patients during liver resection. A randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2023;39:74–83.
Giustiniano E, Nisi F, Rocchi L, Zito PC, Ruggieri N, Cimino MM, et al. Perioperative management of complex hepatectomy for colorectal liver metastases: the alliance between the surgeon and the anesthetist. Cancers (Basel). 2021;13:2203.
Page AJ, Kooby DA. Perioperative management of hepatic resection. J Gastrointest Oncol. 2012;3:19–27.
Melendez JA, Arslan V, Fischer ME, Wuest D, Jarnagin WR, Fong Y, et al. Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg. 1998;187:620–5.
Jones RM, Moulton CE, Hardy KJ. Central venous pressure and its effect on blood loss during liver resection. Br J Surg. 1998;85:1058–60.
Chen H, Merchant NB, Didolkar MS. Hepatic resection using intermittent vascular inflow occlusion and low central venous pressure anesthesia improves morbidity and mortality. J Gastrointest Surg. 2000;4:162–7.
Liang L, Li C, Wang MD, Wang H, Zhou YH, Zeng YY, et al. Development and validation of a novel online calculator for estimating survival benefit of adjuvant transcatheter arterial chemoembolization in patients undergoing surgery for hepatocellular carcinoma. J Hematol Oncol. 2021;14:165.
Liang L, Li C, Diao YK, Jia HD, Xing H, Pawlik TM, et al. Survival benefits from adjuvant transcatheter arterial chemoembolization in patients undergoing liver resection for hepatocellular carcinoma: a systematic review and meta-analysis. Therap Adv Gastroenterol. 2020;13:1756284820977693.
Yang T, Lu JH, Zhai J, Lin C, Yang GS, Zhao RH, et al. High viral load is associated with poor overall and recurrence-free survival of hepatitis B virus-related hepatocellular carcinoma after curative resection: a prospective cohort study. Eur J Surg Oncol. 2012;38:683–91.
Zhu H, Xing H, Yu B, Yan WT, Zhang CW, Guan MC, et al. Long-term survival and recurrence after curative resection for hepatocellular carcinoma in patients with chronic hepatitis C virus infection: a multicenter observational study from China. HPB (Oxford). 2020;22:1793–802.
Yu JJ, Shen F, Chen TH, Liang L, Han J, Xing H, et al. Multicentre study of the prognostic impact of preoperative bodyweight on long-term prognosis of hepatocellular carcinoma. Br J Surg. 2019;106:276–85.
Chiu CC, Lee KT, Wang JJ, Sun DP, Lee HH, Huang CC, et al. Preoperative health-related quality of life predicts minimal clinically important difference and survival after surgical resection of hepatocellular carcinoma. J Clin Med. 2019;8:576.
Acknowledgement
The authors thank all the surgeons and patients who participated in the study.
Funding
This study was supported by the National Natural Science Foundation of China (No. 62275050), the Major Research Projects for Young and Middle-aged Talent of Fujian Provincial Health Commission (no. 2021ZQNZD013), the Key Clinical Specialty Discipline Construction Program of Fuzhou, Fujian (Grant Number: 201912002), Fujian Provincial Clinical Research Center for Hepatobiliary and Pancreatic Tumors (Grant Number: 2020Y2013), the Scientific Foundation of Fuzhou Municipal Health Commission (Grant Number: 2021-S-wp1), Dawn Project Foundation of Shanghai (No. 21SG36), Shanghai Health and Hygiene Discipline Leader Project (Grant Number: 2022XD001), and Shanghai Outstanding Academic Leader Program (Grant Number: 23XD1424900). Role of the funder/sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Shi-Chuan Tang, Jia-Hao Xu, Yi-Fan Yang, Jia-Ning Shi, and Kong-Ying Lin contributed equally to this work. Drs Zeng and Yang had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization: Shi-Chuan Tang, Feng Shen, Yong-Yi Zeng, and Tian Yang. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: Shi-Chuan Tang, Jia-Hao Xu, Yi-Fan Yang, Wan Yee Lau, Yong-Yi Zeng, and Tian Yang. Critical revision of the manuscript for important intellectual content: Shi-Chuan Tang, Wei-Min Gu, Ya-Hao Zhou, Hong-Zhi Liu, Ying-Jian Liang, Wan Yee Lau, and Tian Yang. Statistical analysis: Shi-Chuan Tang, Jia-Hao Xu, Jia-Ning Shi, Kong-Ying Lin, Jie Kong, Xian-Ming Wang, Zhong-Qi Fan, Hong-Zhi Liu, and Tian Yang. Obtained funding: Yong-Yi Zeng and Tian Yang. Administrative, technical, or material support: Xian-Ming Wang, Wei-Min Gu, Ya-Hao Zhou, Ying-Jian Liang, Feng Shen, Yong-Yi Zeng, and Tian Yang. Study supervision: Wan Yee Lau, Feng Shen, Yong-Yi Zeng, and Tian Yang. Final approval of manuscript: all authors.
Corresponding authors
Ethics declarations
Disclosures
None reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tang, SC., Xu, JH., Yang, YF. et al. Impact of Hepatic Pedicle Clamping on Long-Term Survival Following Hepatectomy for Hepatocellular Carcinoma: Stratified Analysis Based on Intraoperative Blood Transfusion Status. Ann Surg Oncol 31, 1812–1822 (2024). https://doi.org/10.1245/s10434-023-14642-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14642-6