Abstract
Background
The impact of postoperative complications (POCs) on long-term outcomes following hepatocellular carcinoma (HCC) resection remains to be ascertained.
Methods
All consecutive HCC resected at a single center were analyzed. Patients with POCs, classified according to Clavien classification, were compared to those without in terms of demographics, pathology, management, overall survival (OS), and disease-free survival (DFS). Independent prognostic factors of POCs were identified using multivariable regression models.
Results
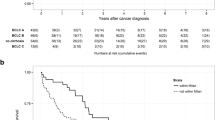
Among 341 patients, overall POCs rate was 34% (n = 116) and grade III–IV POCs rate was 14.4% (n = 49). POCs were an independent negative factor for OS [hazard ratio (HR) 1.40, 95% confidence interval (CI) 1.12–2.26, p = 0.009] with BCLC stage, the need for combined procedure, intraoperative transfusion, and the METAVIR score of the underlying parenchyma. Similarly, occurrence of POCs was associated independently with DFS (HR 1.59, 95% CI 1.18–2.15, p = 0.002), together with the presence of portal hypertension, BCLC stage, the need for combined procedure, intraoperative transfusion, and the presence of satellite nodules. After stratification, the negative impact of morbidity on OS and DFS reached statistical significance in the BCLC stage A subset only (p = 0.026, and p < 0.001, respectively). Open resection, intraoperative transfusion, and the existence of underlying liver injury were independent predictors of POCs.
Conclusions
POCs should be considered as a long-term prognostic factor. Careful patient selection requiring underlying liver assessment and appropriate strategy, such as mini-invasive surgery and restricted transfusion policy, might be promoted to prevent POCs.


Similar content being viewed by others
References
Llovet JM, Ducreux M, Lencioni R, et al. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56(4):908–43.
Bruix J, Sherman M. American association for the study of liver diseases. management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–2.
Torzilli G, Belghiti J, Kokudo N, et al. A snapshot of the effective indications and results of surgery for hepatocellular carcinoma in tertiary referral centers: is it adherent to the EASL/AASLD recommendations? An observational study of the HCC East-West study group. Ann Surg. 2013;257(5):929–37.
Yin L, Li H, Li AJ, et al. Partial hepatectomy versus transcatheter arterial chemoembolization for resectable multiple hepatocellular carcinoma beyond Milan Criteria: a RCT. J Hepatol. 2014;61(1):82–8.
Fan ST, Poon RT, Yeung C, et al. Outcome after partial hepatectomy for hepatocellular cancer within the Milan criteria. Br J Surg. 2011;98(9):1292–300.
Mazzaferro V, Romito R, Schiavo M, et al. Prevention of hepatocellular carcinoma recurrence with alpha-interferon after liver resection in HCV cirrhosis. Hepatology. 2006;44:1543–54.
Ishizawa T, Hasegawa K, Aoki T, et al. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology. 2008;134:1908–16.
Makuuchi M, Sano K. The surgical approach to HCC: our progress and results in Japan. Liver Transpl. 2004;10:S46–S52.
-Llovet JM, Schwartz M, Mazzaferro V. Resection and liver transplantation for hepatocellular carcinoma. Semin Liver Dis. 2005;25:181–200.
Shim JH, Jun MJ, Han S, et al. Prognostic nomograms for prediction of recurrence and survival after curative liver resection for hepatocellular carcinoma. Ann Surg. 2015;261(5):939–46.
Kusano T, Sasaki A, Kai S, et al. Predictors and prognostic significance of operative complications in patients with hepatocellular carcinoma who underwent hepatic resection. Eur J Surg Oncol. 2009;35(11):1179–85.
Eappen S, Lane BH, Rosenberg B, et al. Relationship between occurrence of surgical complications and hospital finances. JAMA. 2013;309(15):1599–606.
De Melo GM, Ribeiro KC, Kowalski LP, Deheinzelin D. Risk factors for postoperative complications in oral cancer and their prognostic implications. Arch Otolaryngol Head Neck Surg. 2001;127(7):828–33.
Mirnezami A, Mirnezami R, Chandrakumaran K, et al. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg. 2011;253(5):890–9.
Andalib A, Ramana-Kumar AV, Bartlett G, et al. Influence of postoperative infectious complications on long-term survival of lung cancer patients: a population-based cohort study. J Thorac Oncol. 2013;8(5):554–61.
Ito H, Are C, Gonen M, et al. Effect of postoperative morbidity on long-term survival after hepatic resection for metastatic colorectal cancer. Ann Surg. 2008;247(6):994–1002.
Farid SG, Aldouri A, Morris-Stiff G, et al. Correlation between postoperative infective complications and long-term outcomes after hepatic resection for colorectal liver metastasis. Ann Surg. 2010;251(1):91–100.
Laurent C, Sa Cunha A, Couderc P, et al. Influence of postoperative morbidity on long-term survival following liver resection for colorectal metastases. Br J Surg. 2003;90(9):1131–6.
Mavros MN, de Jong M, Dogeas E, et al. Impact of complications on long-term survival after resection of colorectal liver metastases. Br J Surg. 2013;100(5):711–8.
Spolverato G, Yakoob MY, Kim Y, et al. Impact of complications on long-term survival after resection of intrahepatic cholangiocarcinoma. Cancer. 2015;121(16):2730–9.
Chok KS, Ng KK, Poon RT, et al. Impact of postoperative complications on long-term outcome of curative resection for hepatocellular carcinoma. Br J Surg. 2009;96(1):81–7.
Ruan DY, Lin ZX, Li Y, et al. Poor oncologic outcomes of hepatocellular carcinoma patients with intra-abdominal infection after hepatectomy. World J Gastroenterol. 2015;21(18):5598–606.
Mizuguchi T, Kawamoto M, Meguro M, et al. Prognosis and predictors of surgical complications in hepatocellular carcinoma patients with or without cirrhosis after hepatectomy. World J Surg. 2013;37(6):1379–87.
Okamura Y, Takeda S, Fujii T, et al. Prognostic significance of postoperative complications after hepatectomy for hepatocellular carcinoma. J Surg Oncol. 2011;104(7):814–21.
Bruix J, Sherman M, Llovet JM, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. J Hepatol. 2001;35:421–30.
Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–36.
Mayo SC, Shore AD, Nathan H, et al. Refining the definition of perioperative mortality following hepatectomy using death within 90 days as the standard criterion. HPB. 2011;13(7):473–82.
The METAVIR Group. Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. Hepatology. 1994;20(1):15–20.
Azoulay D, Castaing D, Krissat J, et al. Percutaneous portal vein embolization increases the feasibility and safety of major liver resection for hepatocellular carcinoma in injured liver. Ann Surg. 2000;232:665–72.
Kluger MD, Salceda JA, Laurent A, et al. Liver resection for hepatocellular carcinoma in 313 Western patients: tumor biology and underlying liver rather than tumor size drive prognosis. J Hepatol. 2015;62:1131–40.
Santambrogio R, Kluger MD, Costa M, et al. Hepatic resection for hepatocellular carcinoma in patients with Child-Pugh’s A cirrhosis: is clinical evidence of portal hypertension a contraindication? HPB. 2013;15(1):78–84.
Couinaud C. Le foie: études anatomiques et chirurgicales. Masson, Paris, 1957.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149(5):713–24.
Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149(5):680–8.
Rahbari NN, Garden OJ, Padbury R, et al. Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB. 2011;13(8):528–35.
Dindo D, Demartines N, Clavien PA. Classification of Surgical Complications: A New Proposal with Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann Surg. 2004;240(2):205–13.
Benchimol EI, Langan S, Guttmann A, RECORD Steering Committee. Call to RECORD: the need for complete reporting of research using routinely collected health data. J Clin Epidemiol. 2013;66(7):703–5.
Cauchy F, Fuks D, Nomi T, et al. Risk factors and consequences of conversion in laparoscopic major liver resection. Br J Surg. 2015;102(7):785–95.
Han HS, Shehta A, Ahn S, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma: case-matched study with propensity score matching. J Hepatol. 2015;63(3):643–50.
Sposito C, Battiston C, Facciorusso A, et al. Propensity score analysis of outcomes following laparoscopic or open liver resection for hepatocellular carcinoma. Br J Surg. 2016;103(7):871–80.
Han DH, Choi SH, Park EJ, et al. Surgical outcomes after laparoscopic or robotic liver resection in hepatocellular carcinoma: a propensity-score matched analysis with conventional open liver resection. Int J Med Robot 2015 Nov 4. Epub ahead of print.
Komatsu S, Brustia R, Goumard C, et al. Laparoscopic versus open major hepatectomy for hepatocellular carcinoma: a matched pair analysis. Surg Endosc. 2016;30(5):1965–74.
Cucchetti A, Ercolani G, Vivarelli M, et al. Impact of model for end-stage liver disease (MELD) score on prognosis after hepatectomy for hepatocellular carcinoma on cirrhosis. Liver Transpl. 2006;12:966–71.
Worhunsky DJ, Dua MM, Tran TB, et al. Laparoscopic hepatectomy in cirrhotics: safe if you adjust technique. Surg Endosc. 2016;1–8.
Kawaguchi Y, Nomi T, Fuks D, et al. Hemorrhage control for laparoscopic hepatectomy: technical details and predictive factors for intraoperative blood loss. Surg Endosc. 2016;30(6):2543–51.
Shehta A, Han HS, Yoon YS, et al. Laparoscopic liver resection for hepatocellular carcinoma in cirrhotic patients: 10-year single-center experience. Surg Endosc. 2016;30(2):638–48.
Buettner S, Gani F, Amini N, et al. The relative effect of hospital and surgeon volume on failure to rescue among patients undergoing liver resection for cancer. Surgery. 2015;159(4):1004–12.
Lim C, DeJong CH, Farges O; e-HPBchir Study Group from the Association de Chirurgie Hépato-Biliaire et de Transplantation (ACHBT) (Association of Hepatobiliary and Transplant Surgery). Improving the quality of liver resection: a systematic review and critical analysis of the available prognostic models. HPB. 2015;17(3):209–21.
Yamashita Y, Yoshida Y, Kurihara T, et al. Surgical results for recurrent hepatocellular carcinoma after curative hepatectomy: repeat hepatectomy versus salvage living donor liver transplantation. Liver Transpl. 2015;21(7):961–8.
Mise Y, Hasegawa K, Shindoh J, et al. The feasibility of third or more repeat hepatectomy for recurrent hepatocellular carcinoma. Ann Surg. 2015;262(2):347–57.
Scatton O, Zalinski S, Terris B, et al. Hepatocellular carcinoma developed on compensated cirrhosis: Resection as a selection tool for liver transplantation. Liver Transpl. 2008;14:779–88.
Bhangui P, Allard MA, Vibert E, et al. Salvage versus primary liver transplantation for early hepatocellular carcinoma: do both strategies yield similar outcomes? Ann Surg. 2015;264(1):155–163.
Tribillon E, Barbier L, Goumard C, et al. When should we propose liver transplant after resection of hepatocellular carcinoma? A comparison of salvage and de Principe strategies. J Gastrointest Surg. 2016;20(1):66–76.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Bioemtrika. 1983;70(1):41–55.
Author information
Authors and Affiliations
Corresponding author
Additional information
Alexandre Doussot and Chetana Lim have contributed equally to this work and are co-first author.
Rights and permissions
About this article
Cite this article
Doussot, A., Lim, C., Lahat, E. et al. Complications after Hepatectomy for Hepatocellular Carcinoma Independently Shorten Survival: A Western, Single-Center Audit. Ann Surg Oncol 24, 1569–1578 (2017). https://doi.org/10.1245/s10434-016-5746-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5746-6