Abstract
Background
Women who undergo mastectomy for breast cancer may be prone to prolonged opioid use (POU). However, risk factors for long-term opioid use after mastectomy remain unclear. This study seeks to identify risk factors for POU after mastectomy.
Patients and Methods
A single-institution database was queried for women who underwent mastectomy for breast cancer between January 2016 and December 2017. Patients were stratified based on opioid use < 90 or ≥ 90 days after mastectomy or completion of their reconstruction. Clinicopathologic and operative parameters as well as preoperative and postoperative opioid usage were compared.
Results
Patients with opioid use ≥ 90 days after last procedure (POU) had a history of preoperative opioid use (29.3% vs 8.2%, p = 0.002), were more likely to have concomitant psychiatric illness (70% vs 35.6%, p < 0.001), and had received adjuvant chemotherapy (43.1% vs 24.7%, p = 0.03). Patients with POU also had greater daily opioid doses prescribed upon discharge (59.6 mg vs 44.6 mg, p < 0.001). On multivariable analysis, preoperative opioid use (OR 3.61, 95% CI 1.16–11.22, p = 0.03), daily oral morphine equivalents prescribed at discharge (OME-D) (OR 1.02, 95% CI 1.01–1.05, p = 0.003), and psychiatric illness (OR 4.48, 95% CI 1.85–10.89, p < 0.001) were independently associated with POU. Among opioid-naïve patients, 37% were found to have POU. Among these patients, OME at discharge (OR 1.02, 95% CI 1.003–1.04, p = 0.02) and psychiatric illness (OR 3.23, 95% CI 1.25–8.31, p = 0.02) independently predicted POU.
Conclusions
Preoperative opioid use, psychiatric illness, and daily OME at discharge independently predict POU after mastectomy.
Similar content being viewed by others
References
Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E. Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg. 2017;125(5):1733–40.
Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths–United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50–51):1378–82.
Uhrbrand P, Simoni AH, Olesen AE, Pedersen AB, Christiansen CF, Nikolajsen L. Opioid dependency as complication after surgery. Ugeskr Laeger. 2018;180(31):2–5.
Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504.
Lee JS, Hu HM, Edelman AL, et al. New persistent opioid use among patients with cancer after curative-intent surgery. J Clin Oncol. 2017;35(36):4042–49.
Lee JS, Howard RA, Klueh MP, et al. The impact of education and prescribing guidelines on opioid prescribing for breast and melanoma procedures. Ann Surg Oncol. 2019;26(1):17–24.
Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901–6.
Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286–93.
Keskey RC, LaJoie AS, Sutton BS, et al. Cost-effectiveness analysis of contralateral prophylactic mastectomy compared to unilateral mastectomy with routine surveillance for unilateral, sporadic breast cancer. Ann Surg Oncol. 2017;24(13):3903–10.
Yao K, Sisco M, Bedrosian I. Contralateral prophylactic mastectomy: current perspectives. Int J Womens Health. 2016;8:213–223.
Andreae MH, Andreae DA. Regional anaesthesia to prevent chronic pain after surgery: a Cochrane systematic review and meta-analysis. BJA. 2013;111(5):711–720.
Tripathy S, Rath S, Agrawal S, et al. Opioid-free anesthesia for breast cancer surgery: an observational study. J Anaesthesiol Clin Pharmacol. 2018;34(1):35–40.
Marcusa DP, Mann RA, Cron DC, et al. Prescription opioid use among opioid-naive women undergoing immediate breast reconstruction. Plast Reconstr Surg. 2017;140(6):1081–90.
Berglund DD, Rosas S, Kurowicki J, Horn B, Mijic D, Levy JC. Preoperative opioid use among patients undergoing shoulder arthroplasty predicts prolonged postoperative opioid use. J Am Acad Orthop Surg. 2019;27(15):E691–5.
Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naïve women. Am J Obstet Gynecol. 2016;215(3):353.e318–51.
Manchikanti L, Giordano J, Boswell MV, Fellows B, Manchukonda R, Pampati V. Psychological factors as predictors of opioid abuse and illicit drug use in chronic pain patients. J Opioid Manag. 2007;3(2):89–100.
Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A. Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ (Clin Res Ed). 2005;330(7493):702.
Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425–30.
Jung BF, Herrmann D, Griggs J, Oaklander AL, Dworkin RH. Neuropathic pain associated with non-surgical treatment of breast cancer. Pain. 2005;118(1–2):10–14.
Hill MV, McMahon ML, Stucke RS, Barth RJ, Jr. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265(4):709–14.
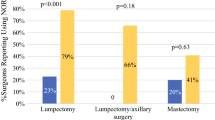
Lillemoe HA, Newhook TE, Vreeland TJ, et al. Educating surgical oncology providers on perioperative opioid use: results of a departmental survey on perceptions of opioid needs and prescribing habits. Ann Surg Oncol. 2019;26(7):2011–18.
Hill MV, Stucke RS, Billmeier SE, Kelly JL, Barth RJ, Jr. Guideline for discharge opioid prescriptions after inpatient general surgical procedures. J Am Coll Surg. 2018;226(6):996–1003.
Kennedy-Hendricks A, Gielen A, McDonald E, McGinty EE, Shields W, Barry CL. Medication sharing, storage, and disposal practices for opioid medications among US adultssharing, storage, and disposal practices for opioidsletters. JAMA Intern Med. 2016;176(7):1027–9.
Hasak JM, Roth Bettlach CL, Santosa KB, Larson EL, Stroud J, Mackinnon SE. Empowering post-surgical patients to improve opioid disposal: a before and after quality improvement study. J Am Coll Surg. 2018;226(3):235–40.
Hallway A, Vu J, Lee J, et al. Patient satisfaction and pain control using an opioid-sparing postoperative pathway. J Am Coll Surg. 2019;229(3):316–22.
Refai M, Andolfi M, Gentili P, Pelusi G, Manzotti F, Sabbatini A. Enhanced recovery after thoracic surgery: patient information and care-plans. J Thorac Dis. 2018;10(Suppl 4):S512–6.
Deng QF, Gu HY, Peng WY, et al. Impact of enhanced recovery after surgery on postoperative recovery after joint arthroplasty: results from a systematic review and meta-analysis. Postgrad Med J. 2018;94(1118):678–93.
Huang J, Cao C, Nelson G, Wilson RD. Review of enhanced recovery after surgery principles used for scheduled CD: perioperative process evaluation. J Obstet Gynaecol Can. 2018;41(12):1775–88.
Rojas KE, Manasseh DM, Flom PL, et al. A pilot study of a breast surgery enhanced recovery after surgery (ERAS) protocol to eliminate narcotic prescription at discharge. Breast Cancer Res Treat. 2018;171(3):621–26.
Richardson JD. Recovering from an operation. J Am Coll Surg. 2018;228(3):310–11.
Lee KJ, Min BW, Bae KC, Cho CH, Kwon DH. Efficacy of multimodal pain control protocol in the setting of total hip arthroplasty. Clin Orthop Surg. 2009;1(3):155–60.
Jin F, Chung F. Multimodal analgesia for postoperative pain control. J Clin Anesth. 2001;13(7):524–39.
Cho CH, Song KS, Min BW, et al. Multimodal approach to postoperative pain control in patients undergoing rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1744–8.
Horsley RD, Vogels ED, McField DAP, et al. Multimodal postoperative pain control is effective and reduces opioid use after laparoscopic roux-en-Y gastric bypass. Obes Surg. 2019;29(2):394–400.
Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol. 2014;69(2):153–66.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors have no disclosures pertaining to the work presented.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Woeste, M.R., Bhutiani, N., Geller, A.E. et al. Identifying Factors Predicting Prolonged Opioid Use After Mastectomy. Ann Surg Oncol 27, 993–1001 (2020). https://doi.org/10.1245/s10434-019-08171-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-08171-4