Abstract
Background
Postoperative prescriptions have contributed to the opioid epidemic. In response, a large, integrated health care delivery system implemented initiatives to reduce outpatient opioid prescriptions. We evaluated the impact of these interventions on opioid-prescribing practices after breast surgery.
Methods
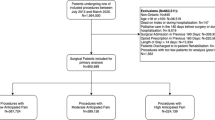
We examined postoperative prescribing practices before and after the 2016–2018 intervention period. Primary endpoints were the use of non-opioid regimens (NORs) and morphine milligram equivalents (MMEs) prescribed for postoperative pain management, while secondary endpoints were emergency department (ED) visits and readmissions within 7 days of surgery.
Results
In a survey of breast surgeons, 23% reported using NORs in 2017 versus 79% in 2019 (p < 0.001). Comparing 1917 breast operations from 2016 with 2166 operations from 2019, NORs increased from 9% in 2016 to 39% in 2019 (p < 0.001). Average discharge MMEs per operation decreased from 190 in 2016 to 106 in 2019 (p < 0.001). NOR failure (defined as an additional opioid prescription within 2 weeks of surgery) was < 1%. Significantly fewer postoperative ED visits occurred in the NOR group (1.9% NOR vs. 3.4% opioid regimen [OR]; p < 0.001). The 7-day readmission rates for NOR and OR patients were similar (0.49% NOR vs. 0.32% OR; p = 0.45).
Conclusion
Between 2016 and 2019, breast surgeons in a large, integrated health care delivery system adopted NORs for nearly 40% of breast operations, and prescribed significantly fewer MMEs, with no increases in ED visits or readmissions for NOR patients. This suggests that initiatives to decrease opioid prescribing were successful and that a NOR for pain management after breast surgery is feasible.




Similar content being viewed by others
References
Wilson N, Kariisa M, Seth P, Smith H, Davis NL. Drug and opioid-involved overdose deaths. MMWR Morbidity and mortality weekly report 2020;69(11): 290–297. https://doi.org/10.15585/mmwr.mm6911a4
Clark DJ, Schumacher MA. America’s opioid epidemic: supply and demand considerations. Anesth Analg. 2017;125(5):1667-1674. https://doi.org/10.1213/ane.0000000000002388
Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long term analgesic use after low risk surgery. Arch Intern Med. 2012;172(5):425-430. https://doi.org/10.1001/archinternmed.2011.1827
Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286-93. https://doi.org/10.1001/jamainternmed.2016.3298
Barth RJ, Waljee JF (2020) Classification of opioid dependence, abuse, or overdose in opioid-naive patients as a “Never Event”. JAMA Surg, https://doi.org/10.1001/jamasurg.2020.0432
Overton HN, Hanna MN, Bruhn WE, Hutfless S, Bicket MC, Makary MA. Opioids After Surgery Workgroup. Opioid-prescribing guidelines for common surgical procedures: an expert panel consensus. J Am Coll Surg, 2018;227(4):411-418. https://doi.org/10.1016/j.jamcollsurg.2018.07.659
Chou R, Gordon DB, Leon-Casasola OAD, et al. Management of postoperative pain: a clinical practice guideline from the American pain society, the American society of regional anesthesia and pain medicine, and the American society of anesthesiologists committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016;17(2):131-57. https://doi.org/10.1016/j.jpain.2015.12.008
Rao R, Jackson RS, Rosen B, et al. Pain control in breast surgery: survey of current practice and recommendations for optimizing management—American society of breast surgeons opioid/pain control workgroup. Ann Surg Oncol. 2020;27(4):985-990. https://doi.org/10.1245/s10434-020-08197-z
Gordon NP. Similarity of the adult Kaiser Permanente membership in Northern California to the insured and general population in northern California: statistics from the 2011 California health interview survey. [Internet] Oakland, CA: Kaiser Permanente Division of Research; 2015. Jun 19, [cited 2015 Nov 11]. Available from: https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/chis_non_kp_2011.pdf
Liu VX, Rosas E, Hwang J, et al. Enhanced recovery after surgery program implementation in 2 surgical populations in an integrated health care delivery system. JAMA Surg. 2017;152(7):e171032. https://doi.org/10.1001/jamasurg.2017.1032
Liu VX, Eaton A, Lee DC, et al. Postoperative opioid use before and after enhanced recovery after surgery program implementation. Ann Surg. 2019; 270(6):e69-e71. https://doi.org/10.1097/sla.0000000000003409
Rothenberg KA, Huyser MR, Edquilang JK, et al. Experience with a nonopioid protocol in ambulatory breast surgery: opioids are rarely necessary and use is surgeon-dependent. Perm J. 2019;23:18-127. https://doi.org/10.7812/tpp/18-127
Rojas KE, Manasseh DM, Flom PL, et al. A pilot study of a breast surgery enhanced recovery after surgery (ERAS) protocol to eliminate narcotic prescription at discharge. Breast Cancer Res Treat. 2018;171(3):621-626. https://doi.org/10.1007/s10549-018-4859-y
Hartford LB, Van Koughnett JAM, Murphy PB, et al. The standardization of outpatient procedure (STOP) narcotics: a prospective health systems intervention to reduce opioid use in ambulatory breast surgery. Ann Surg Oncol. 2019; 26(10):3295-3304. https://doi.org/10.1245/s10434-019-07539-w.
Gee KM, Jones RE, Nevarez N, Mcclain LE, Wools G, Beres AL. No pain is gain: a prospective evaluation of strict non-opioid pain control after pediatric appendectomy. J Pediatr Surg. 2020;55(6):1043–1047. https://doi.org/10.1016/j.jpedsurg.2020.02.051
Weinheimer K, Michelotti B, Silver J, Taylor K, Payatakes A. A prospective, randomized, double-blinded controlled trial comparing ibuprofen and acetaminophen versus hydrocodone and acetaminophen for soft tissue hand procedures. J Hand Surg Am. 2019;44(5):387-393. https://doi.org/10.1016/j.jhsa.2018.10.014
Sim V, Hawkins S, Gave AA, et al. How low can you go: achieving postoperative outpatient pain control without opioids. J Trauma Acute Care Surg. 2019;87(1):100-103. https://doi.org/10.1097/ta.0000000000002295
Carrier CS, Garvey KD, Brook EM, Matzkin EG. Patient satisfaction with nonopioid pain management following knee arthroscopic partial meniscectomy and/or chondroplasty. Orthopedics. 2018;41(4):209-214. https://doi.org/10.3928/01477447-20180613-02
Papoian V, Handy KG, Villano AM, et al. Randomized control trial of opioid- versus nonopioid-based analgesia after thyroidectomy. Surgery. 2020;167(6):957–961. https://doi.org/10.1016/j.surg.2020.01.011
Kennedy GT, Hill CM, Huang Y, et al. Enhanced recovery after surgery (ERAS) protocol reduces perioperative narcotic requirement and length of stay in patients undergoing mastectomy with implant-based reconstruction. Am J Surg. 2020;220(1):147–152. https://doi.org/10.1016/j.amjsurg.2019.10.007.07
Rendon JL, Hodson T, Skoracki RJ, Humeidan M, Chao AH. Enhanced recovery after surgery protocols decrease outpatient opioid use in patients undergoing abdominally based microsurgical breast reconstruction. Plast Reconstr Surg. 2020; 145(3):645-651. https://doi.org/10.1097/prs.0000000000006546
Morrow M, Jagsi R, McLeod MC, Shumway D, Katz SJ. Surgeon attitudes toward the omission of axillary dissection in early breast cancer. JAMA Oncol. 2018; 4(11): 1511-1516. https://doi.org/10.1001/jamaoncol.2018.1908
Vuong B, Graff-Baker AN, Yanagisawa M, et al. Implementation of a post-mastectomy home recovery program in a large, integrated health care delivery system. Ann Surg Oncol. 2019;26(10):3178-3184. https://doi.org/10.1245/s10434-019-07551-0
Sada A, Thiels CA, Britain MK, Dudakovic A, et al. Optimizing discharge opioid prescribing practices after mastectomy with immediate reconstruction. Mayo Clin Proc Innov Qual Outcomes. 2019;3(2):183-188. https://doi.org/10.1016/j.mayocpiqo.2019.03.001
Fan B, Valente SA, Shilad S, et al. Reducing narcotic prescriptions in breast surgery: a prospective analysis. Ann Surg Oncol. 2019;26(10):3109-3114. https://doi.org/10.1245/s10434-019-07542-1
Hart AM, Broecker JS, Kao L, Losken A. Opioid use following outpatient breast surgery: are physicians part of the problem? Plast Reconstr Surg. 2018;142(3):611-620. https://doi.org/10.1097/prs.0000000000004636
Acknowledgment
The authors thank the Kaiser Permanente Enhanced Recovery™ team for editorial input.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
Avani R. Patel, Brooke Vuong, Gillian E. Kuehner, Patience Odele, Garner Low, Alison Savitz, Veronica Shim, Margaret Mentakis, Elizabeth Linehan, and Sharon B. Chang have no disclosures to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Appendix 1: Kaiser Permanente Enhanced Recovery™ Perioperative Multimodal Analgesia Regimens
Appendix 1: Kaiser Permanente Enhanced Recovery™ Perioperative Multimodal Analgesia Regimens
-
Provide as many modalities as appropriate from the list below, except where contraindicated.
-
Outpatients: encourage the use of ≥ 2 modalities. For patients not anticipated to need ANY opioid analgesics in PACU, encourage the use of at least 1 modality.
Component | Regimen |
|---|---|
Acetaminophen | 1 gm IV/PO perioperatively, then Q6H ATC |
Gabapentin | 300-600 mg PO preoperatively |
NSAIDs | Ketorolac 15-30 mg IV perioperatively, then Q6H x 24 h |
Ibuprofen 400-600 mg PO Q6H ATC | |
Celecoxib 100-400 mg PO preoperatively | |
Peripheral nerve blocks | |
Ketamine | Per anesthesia provider |
Dexmedetomidine |
Rights and permissions
About this article
Cite this article
Patel, A.R., Vuong, B., Kuehner, G.E. et al. Adoption of Opioid-Sparing and Non-Opioid Regimens After Breast Surgery in a Large, Integrated Health Care Delivery System. Ann Surg Oncol 27, 4835–4843 (2020). https://doi.org/10.1245/s10434-020-08897-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08897-6