Abstract
Background
Studies have shown a variety of nutritional indices to be prognostic predictors for esophageal cancer patients. However, which nutritional index should be used and when it should be measured during the perioperative period remain unclear. This study attempted to clarify the details surrounding predictive nutritional evaluation by assessing the longitudinal data of serologic indices in perioperative esophageal cancer patients.
Methods
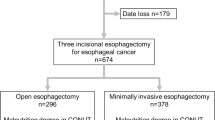
The study included 141 esophageal cancer patients who underwent neoadjuvant chemotherapy after radical esophagectomy at Tohoku University Hospital from April 2008 to December 2017. The nutritional status was retrospectively assessed during the perioperative period, and the prognostic factors related to survival were analyzed.
Results
Use of the controlling nutritional status (CONUT) score showed that malnutrition occurred only from 14 days after surgery in most cases. Use of the prognostic nutritional index (PNI) showed that the ratio of malnutrition increased gradually from presurgery to 14 days after surgery. The timing of malnutrition that affected survival was 14 days after surgery with the CONUT score and presurgery and 4 months after surgery with the PNI. A multivariable analysis of independent prognostic factors predicting survival identified malnutrition 14 days after surgery with the CONUT score and a low PNI before surgery, invasion depth of the primary lesion, and node metastasis.
Conclusions
Malnutrition occurring during the perioperative state of esophageal cancer was shown to be a survival prognostic factor. Development of an optimal nutritional intervention is recommended for esophageal cancer patients to prevent malnutrition both before and after surgery.



Similar content being viewed by others
References
Arends J, Baracos V, Bertz H, et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr. 2017;36:1187–96.
Ando N, Kato H, Igaki H, et al. A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol. 2012;19:68–74.
Gebski V, Burmeister B, Smithers BM, Foo K, Zalcberg J, Simes J. Australasian Gastro-Intestinal Trials Group. Survival benefits from neoadjuvant chemoradiotherapy or chemotherapy in oesophageal carcinoma: a meta-analysis. Lancet Oncol. 2007;8:226–34.
Nagaraja V, Cox MR, Eslick GD. Safety and efficacy of esophageal stents preceding or during neoadjuvant chemotherapy for esophageal cancer: a systematic review and meta-analysis. J Gastrointest Oncol. 2014;5:119–26.
Weimann A, Braga M, Carli F, et al. ESPEN guideline: clinical nutrition in surgery. Clin Nutr. 2017;36:623–50.
Capra S, Ferguson M, Ried K. Cancer: impact of nutrition intervention outcome: nutrition issues for patients. Nutrition. 2001;17:769–72.
Lanuti M, DeDelva P, Morse CR, et al. Management of delayed gastric emptying after esophagectomy with endoscopic balloon dilatation of the pylorus. Ann Thorac Surg. 2011;91:1019–24.
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, et al. CONUT: a tool for controlling nutritional status: first validation in a hospital population. Nutr Hosp. 2005;20:38–45.
Onodera T, Goseki N, Kosakim G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Zasshi. 1984;85:1001–5.
Yoshida N, Baba Y, Shigaki H, et al. Preoperative nutritional assessment by controlling nutritional status (CONUT) is useful to estimate postoperative morbidity after esophagectomy for esophageal cancer. World J Surg. 2016;40:1910–7.
Yoshida N, Harada K, Baba Y, et al. Preoperative controlling nutritional status (CONUT) is useful to estimate the prognosis after esophagectomy for esophageal cancer. Langenbecks Arch Surg. 2017;402:333–41.
Nakatani M, Migita K, Matsumoto S, et al. Prognostic significance of the prognostic nutritional index in esophageal cancer patients undergoing neoadjuvant chemotherapy. Dis Esophagus. 2017;30:1–7.
Matsumoto H, Okamoto Y, Kawai A, et al. Prognosis prediction for postoperative esophageal cancer patients using Onodera’s Prognostic Nutritional Index. Nutr Cancer. 2017;69:849–54.
Okadome K, Baba Y, Yagi T, et al. Prognostic nutritional index, tumor-infiltrating lymphocytes, and prognosis in patients with esophageal cancer. Ann Surg. 2018. https://doi.org/10.1097/SLA.0000000000002985.
NCCN guidelines: esophageal and esophagogastric junction cancers. Retrieved 23 Jan 2019 at http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#site.
Brierley JD, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. 8th ed. Wiley, Oxford; 2017.
Ichikawa H, Miyata G, Miyazaki S, et al. Esophagectomy using a thoracoscopic approach with an open laparotomic or hand-assisted laparoscopic abdominal stage for esophageal cancer: analysis of survival and prognostic factors in 315 patients. Ann Surg. 2013;257:873–85.
Teshima J, Miyata G, Kamei T, et al. Comparison of short-term outcomes between prone and lateral decubitus positions for thoracoscopic esophagectomy. Surg Endosc. 2015;29:2756–62.
Japan Esophageal Society. Japanese Classification of Esophageal Cancer, 11th edition: parts II and III. Esophagus. 2017;14:37–65.
National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE), version 4.0. U.S. Department of Health and Human Services, National Institutes of Health, Bethesda, MD, 2010. Retrieved 23 Jan 2019 at https://cabig-kc.nci.nih.gov/Vocab/KC/index.php/CTCAE.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Chen P, Han L, Wang C, et al. Preoperative serum lipids as prognostic predictors in esophageal squamous cell carcinoma patients with esophagectomy. Oncotarget. 2017;8:41605–19.
Lee H, Jeong CW, Kwak C, et al. Preoperative cholesterol level is associated with worse pathological outcomes and postoperative survival in localized renal cell carcinoma patients: a propensity score-matched study. Clin Genitourin Cancer. 2017;15:e935–41.
Lee SH, Lee JY, Hong TH, Kim BO, Lee YJ, Lee JG. Severe persistent hypocholesterolemia after emergency gastrointestinal surgery predicts in-hospital mortality in critically ill patients with diffuse peritonitis. PLoS ONE. 2018;13:e0200187.
Baba Y, Yoshida N, Shigaki H, et al. Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: a retrospective single-institution study. Ann Surg. 2016;264:305–11.
Goense L, Meziani J, Ruurda JP, van Hillegersberg R. Impact of postoperative complications on outcomes after oesophagectomy for cancer. Br J Surg. 2019;106:111–9.
Kanekiyo S, Takeda S, Iida M, et al. Efficacy of perioperative immunonutrition in esophageal cancer patients undergoing esophagectomy. Nutrition. 2019;59:96–102.
Wu N, Chen G, Hu H, Pang L, Chen Z. Low pretherapeutic serum albumin as a risk factor for poor outcome in esophageal squamous cell carcinomas. Nutr Cancer. 2015;67:481–5.
Tan Z, Zhang M, Han Q, et al. A novel blood tool of cancer prognosis in esophageal squamous cell carcinoma: the fibrinogen/albumin ratio. J Cancer. 2017;8:1025–9.
Yamana I, Takeno S, Shimaoka H, et al. Geriatric Nutritional Risk Index as a prognostic factor in patients with esophageal squamous cell carcinoma: retrospective cohort study. Int J Surg. 2018;56:44–8.
Mitzman B, Schipper PH, Edwards MA, Kim S, Ferguson MK. Complications after esophagectomy are associated with extremes of body mass index. Ann Thorac Surg. 2018;106:973–80.
Wightman SC, Posner MC, Patti MG, et al. Extremes of body mass index and postoperative complications after esophagectomy. Dis Esophagus. 2017;30:1–6.
Ida S, Watanabe M, Karashima R, et al. Changes in body composition secondary to neoadjuvant chemotherapy for advanced esophageal cancer are related to the occurrence of postoperative complications after esophagectomy. Ann Surg Oncol. 2014;21:3675–9.
Reisinger KW, Bosmans JW, Uittenbogaart M, et al. Loss of skeletal muscle mass during neoadjuvant chemoradiotherapy predicts postoperative mortality in esophageal cancer surgery. Ann Surg Oncol. 2015;22:4445–52.
Ida S, Watanabe M, Yoshida N, et al. Sarcopenia is a predictor of postoperative respiratory complications in patients with esophageal cancer. Ann Surg Oncol. 2015;22:4432–7.
Paireder M, Asari R, Kristo I, et al. Impact of sarcopenia on outcome in patients with esophageal resection following neoadjuvant chemotherapy for esophageal cancer. Eur J Surg Oncol. 2017;43:478–84.
Miyata H, Yano M, Yasuda T, et al. Randomized study of clinical effect of enteral nutrition support during neoadjuvant chemotherapy on chemotherapy-related toxicity in patients with esophageal cancer. Clin Nutr. 2012;31:330–6.
Taniguchi H, Sasaki T, Fujita H, et al. Effects of goal-directed fluid therapy on enhanced postoperative recovery: an interventional comparative observational study with a historical control group on oesophagectomy combined with ERAS program. Clin Nutr ESPEN. 2018;23:184–93.
Acknowledgment
This study did not receive any specific grant from any funding agencies in the public, commercial, or not-for-profit sectors. No preregistration was conducted for the study reported in this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
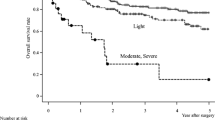
Supplementary Fig.
1. Survival curves according to the nutrition score-based malnutrition groups derived using the Kaplan–Meier method. a The overall survival (OS) according to the prognostic nutritional index (PNI) pre-surgery (P = 0.066). b The OS according to the PNI four months after surgery (P = 0.069). (TIFF 15250 kb)
Rights and permissions
About this article
Cite this article
Hikage, M., Taniyama, Y., Sakurai, T. et al. The Influence of the Perioperative Nutritional Status on the Survival Outcomes for Esophageal Cancer Patients with Neoadjuvant Chemotherapy. Ann Surg Oncol 26, 4744–4753 (2019). https://doi.org/10.1245/s10434-019-07742-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07742-9