Abstract
Purpose
Preoperative malnutrition is a significant risk factor for post-esophagectomy morbidity. The Controlling Nutritional Status (CONUT) is an index used to assess nutritional status, and it has been suggested to predict post-esophagectomy morbidity. However, the difference in the predictive value of CONUT in estimating morbidities between open esophagectomy (OE) and minimally invasive esophagectomy (MIE) has not yet been elucidated.
Methods
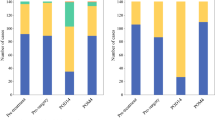
This study included patients who underwent a three-incision esophagectomy for esophageal cancer between April 2005 and August 2021. The patients were further divided into two groups according to their preoperative CONUT scores: normal and light malnutrition and moderate and severe malnutrition. Short-term outcomes between these groups were retrospectively compared in the OE and MIE groups.
Results
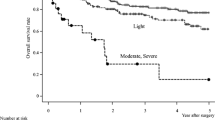
A total of 674 patients who underwent OE (296) and MIE (378) were analyzed. Moreover, 32 patients of the OE group and 16 of the MIE group were classified as having moderate and severe malnutrition, respectively. Moderate and severe malnutrition was significantly associated with a low body mass index, poor performance status, poor American Society of Anesthesiologists physical status, advanced cancer stage, and frequent preoperative treatment. These patients also experienced significantly more frequent morbidities of grade ≥ IIIb according to the Clavien–Dindo classification (CDc), respiratory, and cardiovascular morbidities after OE. Moreover, moderate and severe malnutrition in CONUT was an independent risk factor for morbidity of CDc ≥ IIIb (odds ratio [OR] vs. normal and light malnutrition = 3.38; 95% confidence interval [CI], 1.225–9.332; p = 0.019), respiratory (OR = 3.00; 95% CI, 1.161–7.736; p = 0.023), and cardiovascular morbidities (OR = 3.66; 95% CI, 1.068–12.55; p = 0.039) after OE. Meanwhile, moderate and severe malnutrition in CONUT did not increase the incidence of postoperative morbidities after MIE.
Conclusion
Preoperative malnutrition in CONUT reflects various disadvantageous clinical factors and could be a predictor of worse short-term outcomes after OE, but it has no value in MIE. The low invasiveness of MIE might reduce the effect of preoperative malnutrition on worse short-term outcomes.

Similar content being viewed by others
References
Marubashi S, Takahashi A, Kakeji Y, Hasegawa H, Ueno H, Eguchi S, Endo I, Goi T, Saiura A, Sasaki A, Takiguchi S, Takeuchi H, Tanaka C, Hashimoto M, Hiki N, Horiguchi A, Masaki T, Yoshida K, Gotoh M, Konno H, Yamamoto H, Miyata H, Seto Y, Kitagawa Y, National Clinical Database (2021) National Clinical Database Surgical outcomes in gastroenterological surgery in Japan: report of the National Clinical Database 2011–2019. Ann Gastroenterol Surg 5(5):639–658. https://doi.org/10.1002/ags3.12462
Yoshida N, Yamamoto H, Baba H, Miyata H, Watanabe M, Toh Y, Matsubara H, Kakeji Y, Seto Y (2020) Can minimally invasive esophagectomy replace open esophagectomy for esophageal cancer? Latest analysis of 24,233 esophagectomies from the Japanese National Clinical Database. Ann Surg 272(1):118–124
Yamane T, Yoshida N, Horinouchi T, Morinaga T, Eto K, Harada K, Ogawa K, Sawayama H, Iwatsuki M, Baba Y, Miyamoto Y, Baba H (2022) Minimally invasive esophagectomy may contribute to low incidence of postoperative surgical site infection in patients with poor glycemic control. Langenbecks Arch Surg 407(2):579–585. https://doi.org/10.1007/s00423-021-02306-6
Yoshida N, Horinouchi T, Toihata T, Harada K, Eto K, Sawayama H, Iwatsuki M, Nagai Y, Ishimoto T, Baba Y, Miyamoto Y, Baba H (2021) Clinical significance of pretreatment red blood cell distribution width as a predictive marker for postoperative morbidity after esophagectomy for esophageal cancer: a retrospective study. Ann Surg Oncol 1:1–8. https://doi.org/10.1245/s10434-021-10719-2
Nozoe T, Kimura Y, Ishida M, Saeki H, Korenaga D, Sugimachi K (2002) Correlation of pre-operative nutritional condition with post-operative complications in surgical treatment for oesophageal carcinoma. Eur J Surg Oncol 28(4):396–400. https://doi.org/10.1053/ejso.2002.1257
Filip B, Scarpa M, Cavallin F, Cagol M, Alfieri R, Saadeh L, Ancona E, Castoro C (2015) Postoperative outcome after oesophagectomy for cancer: nutritional status is the missing ring in the current prognostic scores. Eur J Surg Oncol 41(6):787–94. https://doi.org/10.1016/j.ejso.2015.02.014
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, González P, González B, Mancha A, Rodríguez F, Fernández G (2005) CONUT: a tool for controlling nutritional status First validation in a hospital population. Nutr Hosp 20(1):38–45
Yoshida N, Baba Y, Shigaki H, Harada K, Iwatsuki M, Kurashige J, Sakamoto Y, Miyamoto Y, Ishimoto T, Kosumi K, Tokunaga R, Imamura Y, Ida S, Hiyoshi Y, Watanabe M, Baba H (2016) Preoperative nutritional assessment by Controlling Nutritional Status (CONUT) is useful to estimate postoperative morbidity after esophagectomy for esophageal cancer. World J Surg 40(8):1910–7. https://doi.org/10.1007/s00268-016-3549-3
Brierley J, Gospodarowicz M, Wittekind C. The Union for International Cancer Control (UICC). TNM classification of malignant tumours. Eighth ed. Chichester: Wiley; 2017.
Kuwano H, Nishimura Y, Oyama T, Kato H, Kitagawa Y, Kusano M, Shimada H, Takiuchi H, Toh Y, Doki Y, Naomoto Y, Matsubara H, Miyazaki T, Muto M, Yanagisawa A (2015) Guidelines for diagnosis and treatment of carcinoma of the esophagus April 2012 edited by the Japan Esophageal Society. Esophagus 12:1–30. https://doi.org/10.1007/s10388-014-0465-1
Yoshida N, Nakamura K, Kuroda D, Baba Y, Miyamoto Y, Iwatsuki M, Hiyoshi Y, Ishimoto T, Imamura Y, Watanabe M, Baba H (2018) Preoperative smoking cessation is integral to the prevention of postoperative morbidities in minimally invasive esophagectomy. World J Surg 42:2902–2909. https://doi.org/10.1007/s00268-018-4572-3
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Mantziari S, Hübner M, Demartines N, Schäfer M (2014) Impact of preoperative risk factors on morbidity after esophagectomy: is there room for improvement? World J Surg 38(11):2882–90. https://doi.org/10.1007/s00268-014-2686-9
Cengiz O, Kocer B, Sürmeli S, Santicky MJ, Soran A (2006) Are pretreatment serum albumin and cholesterol levels prognostic tools in patients with colorectal carcinoma? Med Sci Monit 12(6):CR240-7
Yeun JY, Kaysen GA (1998) Factors influencing serum albumin in dialysis patients. Am J Kidney Dis 32:118–125. https://doi.org/10.1016/s0272-6386(98)70174-x
Wang Q, Lau WY, Zhang B, Zhang Z, Huang Z, Luo H, Chen X (2014) Preoperative total cholesterol predicts postoperative outcomes after partial hepatectomy in patients with chronic hepatitis B- or C-related hepatocellular carcinoma. Surgery 155(2):263–270. https://doi.org/10.1016/j.surg.2013.08.017
Oh TK, Kim HH, Park DJ, Ahn SH, Do SH, Hwang JW, Kim JH, Oh AY, Jeon YT, Song IA (2018) Association of preoperative serum total cholesterol level with postoperative pain outcomes after laparoscopic surgery for gastric cancer. Pain Pract 18(6):729–735. https://doi.org/10.1111/papr.12659
Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ (2005) Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 91(3):181–4. https://doi.org/10.1002/jso.20329
Delko T, Watson DI, Beck-Schimmer B, Immanuel A, Hussey DJ, Zingg U (2019) Cytokine response in the pleural fluid and blood in minimally invasive and open esophagectomy. World J Surg. 43(10):2631–2639. https://doi.org/10.1007/s00268-019-05069-w
Okamura A, Yamamoto H, Watanabe M, Miyata H, Kanaji S, Kamiya K, Kakeji Y, Doki Y, Kitagawa Y (2020) Association between preoperative HbA1c levels and complications after esophagectomy: analysis of 15801 esophagectomies from the National Clinical Database in Japan. Ann Surg. 17. https://doi.org/10.1097/SLA.0000000000004547
Mazaki T, Ishii Y, Murai I (2015) Immunoenhancing enteral and parenteral nutrition for gastrointestinal surgery: a multiple-treatments meta-analysis. Ann Surg. Apr 261(4):662–9. https://doi.org/10.1097/SLA.0000000000000935
Mudge LA, Watson DI, Smithers BM, Isenring EA, Smith L, Jamieson GG, Australian Immunonutrition Study Group (2018) Multicentre factorial randomized clinical trial of perioperative immunonutrition versus standard nutrition for patients undergoing surgical resection of oesophageal cancer. Br J Surg 105(10):1262–1272. https://doi.org/10.1002/bjs.10923
O Ahmed JC Bolger B O’Neill WB Robb 2020 Use of esophageal stents to relieve dysphagia during neoadjuvant therapy prior to esophageal resection a systematic review Dis Esophagus 33 1 https://doi.org/10.1093/dote/doz090
Yoshida N, Watanabe M, Baba Y, Iwagami S, Ishimoto T, Iwatsuki M, Sakamoto Y, Miyamoto Y, Ozaki N, Baba H (2014) Risk factors for pulmonary complications after esophagectomy for esophageal cancer. Surg Today 44(3):526–32. https://doi.org/10.1007/s00595-013-0577-6
Yoshida N, Baba Y, Hiyoshi Y, Shigaki H, Kurashige J, Sakamoto Y, Miyamoto Y, Iwatsuki M, Ishimoto T, Kosumi K, Sugihara H, Harada K, Tokunaga R, Izumi D, Watanabe M, Baba H (2016) Duration of smoking cessation and postoperative morbidity after esophagectomy for esophageal cancer: how long should patients stop smoking before surgery? World J Surg 40:142–147. https://doi.org/10.1007/s00268-015-3236-9
Valkenet K, Trappenburg JCA, Ruurda JP, Guinan EM, Reynolds JV, Nafteux P, Fontaine M, Rodrigo HE, van der Peet DL, Hania SW, Sosef MN, Willms J, Rosman C, Pieters H, Scheepers JJG, Faber T, Kouwenhoven EA, Tinselboer M, Räsänen J, Ryynänen H, Gosselink R, van Hillegersberg R, Backx FJG (2018) Multicentre randomized clinical trial of inspiratory muscle training versus usual care before surgery for oesophageal cancer. Br J Surg 5:502–511. https://doi.org/10.1002/bjs.10803
Yuda M, Yamashita K, Okamura A, Hayami M, Fukudome I, Toihata T, Imamura Y, Mine S, Ishizuka N, Watanabe M (2020) Influence of preoperative oropharyngeal microflora on the occurrence of postoperative pneumonia and survival in patients undergoing esophagectomy for esophageal cancer. Ann Surg 272(6):1035–1043. https://doi.org/10.1097/SLA.0000000000003287
Triantafyllou T, Olson MT, Theodorou D, Schizas D, Singhal S (2020) Enhanced recovery pathways vs standard care pathways in esophageal cancer surgery: systematic review and meta-analysis. Esophagus 17:100–112. https://doi.org/10.1007/s10388-020-00718-9
Watanabe M, Mine S, Nishida K, Yamada K, Shigaki H, Oya S, Matsumoto A, Kurogochi T, Okamura A, Imamura Y, Sano T (2016) Improvement in short-term outcomes after esophagectomy with a multidisciplinary perioperative care team. Esophagus 13:337–342. https://doi.org/10.1007/s10388-016-0539-3
Zheng C, Li XK, Zhang C, Zhou H, Ji SG, Zhong JH, Xu Y, Cong ZZ, Wang GM, Wu WJ, Shen Y (2021) Comparison of short-term clinical outcomes between robot-assisted minimally invasive esophagectomy: and video-assisted minimally invasive esophagectomy: a systematic review and meta-analysis. J Thorac Dis 13(2):708–719. https://doi.org/10.21037/jtd-20-2896
Barreto JC, Posner MC (2010) Transhiatal versus transthoracic esophagectomy for esophageal cancer. World J Gastroenterol 16(30):3804–10. https://doi.org/10.3748/wjg.v16.i30.3804
Rezaei R, Masuom SHF, Soroush N, Zehi V (2021) Comparison of transhiatal esophagectomy using a mediastinoscope with transhiatal esophagectomy by the classic method. Asian Cardiovasc Thorac Ann 1:33–37. https://doi.org/10.1177/0218492320963976
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
Tomo Horinouchi described and designed the article. Naoya Yoshida edited the article. Hideo Baba supervised the editing of the manuscript. Tomo Horinouchi, Naoya Yoshida, Kazuto Harada, Kojiro Eto, Masaaki Iwatsuki, and Yoshifumi Baba contributed to material preparation, data collection, and analysis. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statements
This study was conducted in accordance with the ethical standards of the Declaration of Helsinki 1975. The institutional ethics committee approved all the research procedures (Registration No. 1909) and waived the requirement for written informed consent owing to the retrospective nature of the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Horinouchi, T., Yoshida, N., Harada, K. et al. A retrospective study of preoperative malnutrition based on the Controlling Nutritional Status score as an associated marker for short-term outcomes after open and minimally invasive esophagectomy for esophageal cancer. Langenbecks Arch Surg 407, 3367–3375 (2022). https://doi.org/10.1007/s00423-022-02655-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02655-w