Abstract
Background
The association between body mass index (BMI) and short-term outcomes after esophagectomy remains controversial.
Methods
A meticulous search for articles describing the association between BMI and perioperative outcomes after esophagectomy was conducted using PubMed, EMBASE, and the Cochrane Library. The study classified BMI according to the World Health Organization definitions and Asian-specific BMI cutoff values. Normal weight was selected as the comparator, and the odds ratio (OR) was calculated as the primary effect.
Results
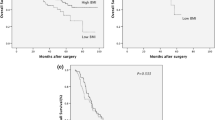
This meta-analysis included 13 studies with 5480 patients. Obese patients exhibited higher risks of overall complication (OR 1.37; P = 0.013), anastomotic leakage (OR 1.74; P = 0.001), and thromboembolic complications (OR 2.05; P = 0.039). Subgroup analysis indicated that obese patients from Western countries had a higher risk of wound infection (OR 2.22; P = 0.022), whereas obese Asians were more likely to experience pulmonary complications (OR 1.64; P = 0.002). Overweight patients displayed no significant differences in major complications relative to normal-weight patients, except for the increased risk of overall complications (OR 1.32; P = 0.030). Additionally, underweight patients showed increased incidence of pulmonary complications (OR 1.92; P = 0.020 and anastomotic leakage (OR 1.64; P = 0.034). Morbid obesity also was analyzed separately with limited data, and this group displayed a higher risk of wound infection (OR 1.62; P = 0.027) and thromboembolic complications (OR 2.65; P = 0.003). No significant differences in mortality were observed among patients in different BMI categories.
Conclusions
Obesity and underweight statuses were confirmed risk factors for several complications after esophagectomy, whereas overweight patients tended to experience greater benefit from surgery.





Similar content being viewed by others

References
Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3:524–48.
Jain S, Dhingra S. Pathology of esophageal cancer and Barrett’s esophagus. Ann Cardiothorac Surg. 2017;6:99–109.
Pasquali S, Yim G, Vohra RS, et al. Survival after neoadjuvant and adjuvant treatments compared to surgery alone for resectable esophageal carcinoma: a network meta-analysis. Ann Surg. 2017;265:481–91.
Low DE, Kuppusamy MK, Alderson D, et al. Benchmarking complications associated with esophagectomy. Ann Surg. 2019;269:291–8.
Lerut T, Moons J, Coosemans W, et al. Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence: role of systematic grading of complications using the modified Clavien classification. Ann Surg. 2009;250:798–807.
Baba Y, Yoshida N, Shigaki H, et al. Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: a retrospective single-institution study. Ann Surg. 2016;264:305–11.
Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005; 143:199–201.
Lagergren J, Bergström R, Nyrén O. Association between body mass and adenocarcinoma of the esophagus and gastric cardia. Ann Intern Med. 1999;130:883–90.
Kruhlikava I, Kirkegard J, Mortensen FV, Kjaer DW. Impact of body mass index on complications and survival after surgery for esophageal and gastro-esophageal-junction cancer. Scand J Surg. 2017;106:305–10.
Wightman SC, Posner MC, Patti MG, Ganai S, Watson S, Prachand V, Ferguson, MK. Extremes of body mass index and postoperative complications after esophagectomy. Dis Esophagus. 2017;30:1–6.
Scarpa M, Cagol M, Bettini S, et al. Overweight patients operated on for cancer of the esophagus survive longer than normal-weight patients. J Gastrointest Surg. 2013;17:218–27.
Melis M, Weber J, Shridhar R, Hoffe S, Almhanna K, Karl RC, Meredith KL. Body mass index and perioperative complications after oesophagectomy for adenocarcinoma: a systematic database review. BMJ Open. 2013;3:e001336.
Salem AI, Thau MR, Strom TJ, et al. Effect of body mass index on operative outcome after robotic-assisted Ivor-Lewis esophagectomy: retrospective analysis of 129 cases at a single high-volume tertiary care center. Dis Esophagus. 2016;30:1–7.
Shridhar R, Hayman T, Hoffe SE, et al. Body mass index and survival in esophageal adenocarcinoma treated with chemoradiotherapy followed by esophagectomy. J Gastrointest Surg. 2012;16:1296–302.
Blom RL, Lagarde SM, Klinkenbijl JH, Busch OR, van Berge Henegouwen MI. A high body mass index in esophageal cancer patients does not influence postoperative outcome or long-term survival. Ann Surg Oncol. 2012;19:766–71.
Watanabe M, Ishimoto T, Baba Y, Nagai Y, Yoshida N, Yamanaka T, Baba H. Prognostic impact of body mass index in patients with squamous cell carcinoma of the esophagus. Ann Surg Oncol. 2013;20:3984–91.
Miao L, Chen H, Xiang J, Zhang Y. A high body mass index in esophageal cancer patients is not associated with adverse outcomes following esophagectomy. J Cancer Res Clin Oncol. 2014;141:941–50.
Hasegawa T, Kubo N, Ohira M, et al. Impact of body mass index on surgical outcomes after esophagectomy for patients with esophageal squamous cell carcinoma. J Gastrointest Surg. 2015;19:226–33.
Wu N, Zhu Y, Kadel D, Pang L, Chen G, Chen Z. The prognostic influence of body mass index, resting energy expenditure, and fasting blood glucose on postoperative patients with esophageal cancer. BMC Gastroenterol. 2016;16:142.
Bhayani NH, Gupta A, Dunst CM, Kurian AA, Halpin VJ, Swanstrom LL. Does morbid obesity worsen outcomes after esophagectomy? Ann Thorac Surg. 2013;95:1756–61.
Scipione CN, Chang AC, Pickens A, Lau CL, Orringer MB. Transhiatal esophagectomy in the profoundly obese: implications and experience. Ann Thorac Surg. 2007;84:376–82 (discussion 383).
Kayani B, Okabayashi K, Ashrafian H, et al. Does obesity affect outcomes in patients undergoing esophagectomy for cancer? A meta-analysis. World J Surg. 2012;36:1785–95.
Mengardo V, Pucetti F, Mc Cormack O, Chaudry A, Allum WH. The impact of obesity on esophagectomy: a meta-analysis. Dis Esophagus. 2018. https://doi.org/10.1093/dote/dox149.
World Health Organization. BMI classification. Retrieved 1 May 2018 at http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.
Zhang SS, Yang H, Luo KJ, et al. The impact of body mass index on complication and survival in resected oesophageal cancer: a clinical-based cohort and meta-analysis. Br J Cancer. 2013;109:2894–903.
Park SK, Ryoo JH, Oh CM, et al. Effect of overweight and obesity (defined by Asian-specific cutoff criteria) on left ventricular diastolic function and structure in a general Korean population. Circ J. 2016;80:2489–95.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, Tierney JF. Preferred reporting items for systematic review and meta-analyses of individual participant data: the PRISMA-IPD statement. JAMA. 2015;313:1657–65.
Wells GA, Shea B, O’Connell D, Peterson J, Weich V, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Retrieved 1 May 2018 at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
STARSurg Collaborative. Multicentre prospective cohort study of body mass index and postoperative complications following gastrointestinal surgery. Br J Surg. 2016;103:1157–72.
31. Zogg CK, Mungo B, Lidor AO, Stem M, Rios Diaz AJ, Haider AH, Molena D. Influence of body mass index on outcomes after major resection for cancer. Surgery. 2015;158:472–85.
Ata A, Valerian BT, Lee EC, Bestle SL, Elmendorf SL, Stain SC. The effect of diabetes mellitus on surgical-site infections after colorectal and noncolorectalgeneral surgical operations. Am Surg. 2010;76:697–702.
Okamura A, Watanabe M, Imamura Y, Kamiya S, Yamashita K, Kurogochi T, Mine S. Preoperative glycosylated hemoglobin levels predict anastomotic leak after esophagectomy with cervical esophagogastric anastomosis. World J Surg. 2017;41:200–7.
Mullen JT, Moorman DW, Davenport DL. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg Oncol. 2009;250:166–72.
American Gastroenterological Association. American Gastroenterological Association medical position statement on the management of Barrett’s esophagus. Gastroenterology. 2011;140:1084–91.
Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA. 2003;290:66–72.
Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol. 2013;19:5598–606.
Cheung KP, Taylor KR, Jameson JM. Immunomodulation at epithelial sites by obesity and metabolic disease. Immunol Res. 2012;52:182–99.
Rondina MT, Wheeler M, Rodgers GM, Draper L, Pendleton RC. Weight-based dosing of enoxaparin for VTE prophylaxis in morbidly obese, medically-Ill patients. Thromb Res. 2010;125:220–3.
Thomas DC, Arnold BN, Hoag JR, et al. Timing and risk factors associated with venous thromboembolism after lung cancer resection. Ann Thorac Surg. 2018;105:1469–75.
Kilic A, Schuchert MJ, Pennathur A, Yaeger K, Prasanna V, Luketich JD, Gilbert S. Impact of obesity on perioperative outcomes of minimally invasive esophagectomy. Ann Thorac Surg. 2009;87:412–5.
Yoshida N, Watanabe M, Baba Y, et al. Risk factors for pulmonary complications after esophagectomy for esophageal cancer. Surg Today. 2014;44:526–32.
Bluman LG, Mosca L, Newman N, Simon DG. Preoperative smoking habits and postoperative pulmonary complications. Chest. 1998;113:883–9.
Van Daele E, Van de Putte D, Ceelen W, Van Nieuwenhove Y, Pattyn P. Risk factors and consequences of anastomotic leakage after Ivor Lewis oesophagectomydagger. Interact Cardiovasc Thorac Surg. 2016;22:32–7.
Baucom RB, Poulose BK, Herline AJ, Muldoon RL, Cone MM, Geiger TM. Smoking as dominant risk factor for anastomotic leak after left colon resection. Am J Surg. 2015;210:1–5.
Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay, and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22:235–9.
Cederholm T, Bosaeus I, Barazzoni R, et al. Diagnostic criteria for malnutrition: an ESPEN consensus statement. Clin Nutr. 2015;34:335–40.
Thomas MN, Kufeldt J, Kisser U, et al. Effects of malnutrition on complication rates, length of hospital stay, and revenue in elective surgical patients in the G-DRG-system. Nutrition. 2016;32:249–54.
Sun L, Quan XQ, Yu S. An epidemiological survey of cachexia in advanced cancer patients and analysis on its diagnostic and treatment status. Nutr Cancer. 2015;67:1056–62.
Muscaritoli M, Anker SD, Argiles J, et al. Consensus definition of sarcopenia, cachexia, and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr. 2010;29:154–9.
Mesquita AF, Silva ECD, Eickemberg M, Roriz AKC, Barreto-Medeiros JM, Ramos LB. Factors associated with sarcopenia in institutionalized elderly. Nutr Hosp. 2017;34:345–51.
Harada K, Ida S, Baba Y, et al. Prognostic and clinical impact of sarcopenia in esophageal squamous cell carcinoma. Dis Esophagus. 2016;29:627–33.
Ida S, Watanabe M, Yoshida N, et al. Sarcopenia is a predictor of postoperative respiratory complications in patients with esophageal cancer. Ann Surg Oncol. 2015;22:4432–7.
An X, Zhao Y, Zhang Y, Yang Q, Wang Y, Cheng W, Yang Z. Risk assessment of morbidly obese parturient in cesarean section delivery: a prospective, cohort, single-center study. Medicine Baltimore. 2017;96:e8265.
De Jong A, Verzilli D, Geniez M, Chanques G, Nocca D, Jaber S. Why is the morbidly obese patient at high risk of anesthetic complications. Presse Med. 2018;47:453–63.
Carson JT, Shah SG, Ortega G, Thamyongkit S, Hasenboehler EA, Shafiq B. Complications of pelvic and acetabular fractures in 1331 morbidly obese patients (BMI ≥ 40): a retrospective observational study from the National Trauma Data Bank. Patient Saf Surg. 2018;12:26.
Hopkins TJ, Raghunathan K, Barbeito A, et al. Associations between ASA physical status and postoperative mortality at 48 h: a contemporary dataset analysis compared to a historical cohort. Perioper Med London. 2016;5:29.
Ondeck NT, Bohl DD, Bovonratwet P, et al. Predicting adverse outcomes after total hip arthroplasty: a comparison of demographics, the American Society of Anesthesiologists class, the Modified Charlson Comorbidity Index, and the Modified Frailty Index. J Am Acad Orthop Surg. 2018;26:735-43.
Schlottmann F, Strassle PD, Patti MG. Transhiatal vs transthoracic esophagectomy: a NSQIP analysis of postoperative outcomes and risk factors for morbidity. J Gastrointest Surg. 2017;21:1757–63.
Fuentes E, Ahmad R, Hong TS, et al. The impact of neoadjuvant therapy for gastroesophageal adenocarcinoma on postoperative morbidity and mortality. J Surg Oncol. 2016;113:560–4.
Sunpaweravong S, Ruangsin S, Laohawiriyakamol S, Mahattanobon S, Geater A. Prediction of major postoperative complications and survival for locally advanced esophageal carcinoma patients. Asian J Surg. 2012;35:104–9.
Raymond DP, Seder CW, Wright CD, et al. Predictors of major morbidity or mortality after resection for esophageal cancer: a Society of Thoracic Surgeons General Thoracic Surgery database risk adjustment model. Ann Thorac Surg. 2016;102:207–14.
Mayanagi S, Tsubosa Y, Omae K, et al. Negative impact of skeletal muscle wasting after neoadjuvant chemotherapy followed by surgery on survival for patients with thoracic esophageal cancer. Ann Surg Oncol. 2017;24:3741–7.
Thomson IG, Wallen MP, Hall A, et al. Neoadjuvant therapy reduces cardiopulmunary function in patients undegoing oesophagectomy. Int J Surg. 2018;53:86–92.
Sathornviriyapong S, Matsuda A, Miyashita M, et al. Impact of neoadjuvant chemoradiation on short-term outcomes for esophageal squamous cell carcinoma patients: a meta-analysis. Ann Surg Oncol. 2016;23:3632–40.
van Hagen P, Hulshof MC, van Lanschot JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366:2074–84.
Mungo B, Molena D, Stem M, et al. Does neoadjuvant therapy for esophageal cancer increase postoperative morbidity or mortality? Dis Esophagus. 2015;28:644–51.
Degisors S, Pasquer A, Renaud F, et al. Are thoracotomy and/or intrathoracic anastomosis still predictors of postoperative mortality after esophageal cancer surgery? A nationwide study. Ann Surg. 2017;266:854–62.
Hurewitz AN, Khan SU, Groth ML, Patrick PA, Brand DA. Dosing of unfractionated heparin in obese patients with venous thromboembolism. J Gen Intern Med. 2011;26:487–91.
Gockel I, Niebisch S, Ahlbrand CJ, et al. Risk and complication management in esophageal cancer surgery: a review of the literature. Thorac Cardiovasc Surg. 2016;64:596–605.
Pavia R, Barresi P, Piermanni V, Mondello B, Urgesi R. Role of artificial nutrition in patients undergoing surgery for esophageal cancer. Rays. 2006;31:25–9.
Acknowledgment
We thank M. K. Ferguson (Department of Surgery, The University of Chicago Medicine, Chicago, Illinois, USA) for providing advice and sharing data, and we also thank all the authors of the studies included in our article. The study was founded by the Project of Science and Technology of Henan Province (Grant No. 152102310160) and Spatiotemporal Data Analysis of Cancer Burden in China (Grant No. 2018-I2M-3-003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, P., Li, Y., Sun, H. et al. Predictive Value of Body Mass Index for Short-Term Outcomes of Patients with Esophageal Cancer After Esophagectomy: A Meta-analysis. Ann Surg Oncol 26, 2090–2103 (2019). https://doi.org/10.1245/s10434-019-07331-w
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07331-w