Abstract
Background
Patients with overweight reportedly have more comorbidities, including diabetes mellitus and cardiovascular disease, and longer operating times as well as more blood loss during surgery compared with those with normal weight. However, the impact of overweight on the short-term outcome after transthoracic esophagectomy for patients with esophageal squamous cell carcinoma (ESCC) remains unclear. We hypothesized that overweight has a negative impact on short-term surgical outcomes after esophagectomy for patients with ESCC.
Methods
A total of 304 patients who underwent transthoracic esophagectomy for ESCC were included in this study. Body mass index (BMI) was classified into three categories, <18.49, 18.50–24.99, and >25.00 (kg/m2), defined as low, normal, and high BMI, respectively, according to the World Health Organization criteria. We investigated the association of BMI status with patient demographics and surgical outcomes after esophagectomy for patients with ESCC. In addition, overall survival and relapse-free survival stratified by BMI were compared.
Results
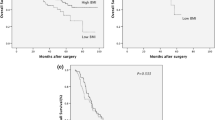
Fifty-nine (19.4 %) and 41 (13.4 %) patients were classified to low BMI and high BMI, respectively. The high-BMI group had significantly higher comorbidity rates of diabetes mellitus (p < 0.01) and anastomotic leakage (p = 0.011) than the normal-BMI group. There were no significant association between high BMI and another various complications except for an anastomotic leakage, severe complications defined by Clavien–Dindo classification and in-hospital mortality. In multivariate analysis, high BMI was a significant risk factor for anastomotic leakage (p = 0.030, hazard ratio; 3.423, 95%CI; 1.128–10.38). On the other hand, no significant association was observed between low BMI and short surgical outcomes. There were no significant differences in overall and relapse-free survival among the three BMI groups in univariate and multivariate analysis (p = 0.128 and p = 0.584, respectively).
Conclusion
The surgical treatment should not be denied for patients with ESCC due to overweight and underweight. However, intraoperative prevention and postoperative careful monitoring for anastomotic leakage might be required after esophagectomy for overweight patients with ESCC.

Similar content being viewed by others
References
Adams JP, Murphy PG. Obesity in anaesthesia and intensive care. Br J Anaesth 2000; 85 (1):91–108.
Ashrafian H, Athanasiou T, le Roux CW. Heart remodelling and obesity: the complexities and variation of cardiac geometry. Heart 2011; 97 (3):171–2.
Dindo D, Muller MK, Weber M, Clavien PA. Obesity in general elective surgery. Lancet 2003; 361 (9374):2032–5.
Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology 2007; 132 (6):2087–2102
Mathur AK, Ghaferi AA, Osborne NH, Pawlik TM, Campbell DA, Englesbe MJ, et al. Body mass index and adverse perioperative outcomes following hepatic resection. J Gastrointest Surg 2010; 14 (8):1285–91
Nobuoka D, Gotohda N, Kato Y, Takahashi S, Konishi M, Kinoshita T, et al. Influence of excess body weight on the surgical outcomes of total gastrectomy. Surg Today 2011; 41 (7):928–34.
Yasunaga H, Horiguchi H, Matsuda S, Fushimi K, Hashimoto H, Ayanian JZ. Body mass index and outcomes following gastrointestinal cancer surgery in Japan. Br J Surg 2013; 100 (10):1335–43.
Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kinura W, et al. A Risk Model for Esophagectomy Using Data of 5354 Patients Included in a Japanese Nationwide Web-Based Database. Ann Surg 2014 in press (DOI: 10.1097/SLA.0000000000000644)
Ye T, Sun Y, Zhang Y, et al. Three-field or two-field resection for thoracic esophageal cancer: a meta-analysis. Ann Thorac Surg 2013; 96:1933–1941
Kubo N, Ohira M, Yamashita Y, Sakurai K, Toyokawa T, Tanaka H, et al. The impact of combined thoracoscopic and laparoscopic surgery on pulmonary complications after radical esophagectomy in patients with resectable esophageal cancer. Anticancer Res 2014; 34 (5):2399–2404
Kubo N, Ohira M, Yamashita, Sakurai K, Lee T, Toyokawa T, et al. Thoracoscopic esophagectomy in the prone position versus in the lateral position for patients with esophageal cancer: a comparison of short-term surgical results. Surg Laparosc Endosc Percutan Tech 2014; 24 (2):158–63
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894:i-xii, 1–253
Onodera T, Goseki N, Kosaki G. [Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients]. Nihon Geka Gakkai Zasshi 1984; 85:1001–1005
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240 (2):205–13
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 1992; 20 (6):864–74.
Sobin LH, Compton CC. TNM seventh edition: what’s new, what’s changed: communication from the International Union Against Cancer and the American Joint Committee on Cancer. Cancer 2010; 116:5336–5339
Yoshiike N, Seino F, Tajima S, Arai Y, Kawano M, Furuhata T, et al. Twenty-year changes in the prevalence of overweight in Japanese adults: the National Nutrition Survey 1976–95. Obes Rev 2002 (3); 3:183–90.
Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med 2005; 143 (3):199–211.
Kubo A, Corley DA. Body mass index and adenocarcinomas of the esophagus or gastric cardia: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev 2006; 15 (5):872–8.
Zhang SS, Yang H, Luo KJ, Luo KJ, Huang QY, Chen JY, et al. The impact of body mass index on complication and survival in resected oesophageal cancer: a clinical-based cohort and meta-analysis. Br J Cancer 2013; 109 (11):2894–903.
Watanabe M, Ishimoto T, Baba Y, Nagai Y, Yoshida N, Yamanaka T, et al. Prognostic impact of body mass index in patients with squamous cell carcinoma of the esophagus. Ann Surg Oncol 2013; 20 (12):3984–91.
Blom RL, Lagarde SM, Klinkenbijl JH, Busch OR, van Berge Henegouwen MI. A high body mass index in esophageal cancer patients does not influence postoperative outcome or long-term survival. Ann Surg Oncol 2012; 19 (3):766–71.
Kayani B, Okabayashi K, Ashrafian H, Harling L, Rao C, Darzi A, et al. Does obesity affect outcomes in patients undergoing esophagectomy for cancer? A meta-analysis. World J Surg 2012; 36 (8):1785–95.
Kassis ES, Kosinski AS, Ross P, Jr., Koppes KE, Donahue JM, Daniel VC. Predictors of anastomotic leak after esophagectomy: an analysis of the society of thoracic surgeons general thoracic database. Ann Thorac Surg 2013; 96 (6):1919–26.
Tang H, Xue L, Hong J, Tao X, Xu Z, Wu B. A method for early diagnosis and treatment of intrathoracic esophageal anastomotic leakage: prophylactic placement of a drainage tube adjacent to the anastomosis. J Gastrointest Surg 2012; 16 (4):722–7.
Dai JG, Zhang ZY, Min JX, Huang XB, Wang JS. Wrapping of the omental pedicle flap around esophagogastric anastomosis after esophagectomy for esophageal cancer. Surgery 2011; 149 (3):404–10.
Lantos JE, Levine MS, Rubesin SE, Lau CT, Torigian DA. Comparison between esophagography and chest computed tomography for evaluation of leaks after esophagectomy and gastric pull-through. J Thorac Imaging 2013; 28 (2):121–8.
Strauss C, Mal F, Perniceni T, Bouzar N, Lenoir S, Gayet B, et al. Computed tomography versus water-soluble contrast swallow in the detection of intrathoracic anastomotic leak complicating esophagogastrectomy (Ivor Lewis): a prospective study in 97 patients. Ann Surg 2010; 251 (4):647–51.
Schaible A, Sauer P, Hartwig W, Hackert T, Hinz U, Radeleff B, et al. Radiologic versus endoscopic evaluation of the conduit after esophageal resection: a prospective, blinded, intraindividually controlled diagnostic study. Surg Endosc 2014; 28 (7):2078–85.
Scipione CN, Chang AC, Pickens A, Lau CL, Orringer MB. Transhiatal esophagectomy in the profoundly obese: implications and experience. Ann Thorac Surg 2007; 84 (2):376–82.
Scarpa M, Cagol M, Bettini S, Alfieri R, Carraro A, Cavallin F, et al. Overweight patients operated on for cancer of the esophagus survive longer than normal-weight patients. J Gastrointest Surg 2013; 17 (2):218–27.
Grotenhuis BA, Wijnhoven BP, Hotte GJ, van der Stok EP, Tilanus HW, van Lanschot JJ. Prognostic value of body mass index on short-term and long-term outcome after resection of esophageal cancer. World J Surg 2010; 34 (11):2621–7.
Yoon HH, Lewis MA, Shi Q, Khan M, Cassivi SD, Diasio RB, et al. Prognostic impact of body mass index stratified by smoking status in patients with esophageal adenocarcinoma. J Clin Oncol 2011; 29 (34):4561–7
van Kruijsdijk RC, van der Wall E, Visseren FL. Obesity and cancer: the role of dysfunctional adipose tissue. Cancer Epidemiol Biomarkers Prev 2009; 18 (10):2569–78.
Conflict of Interest
The authors have no financial or other interests with regard to the submitted manuscript that may be construed as a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hasegawa, T., Kubo, N., Ohira, M. et al. Impact of Body Mass Index on Surgical Outcomes after Esophagectomy for Patients with Esophageal Squamous Cell Carcinoma. J Gastrointest Surg 19, 226–233 (2015). https://doi.org/10.1007/s11605-014-2686-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2686-y