Abstract
RO7297089, an anti-B-cell maturation antigen (BCMA)/CD16A bispecific tetravalent antibody, is being developed as a multiple myeloma (MM) therapeutic. This study characterized nonclinical pharmacokinetics (PK), pharmacodynamics (PD), soluble BCMA (sBCMA), and soluble CD16 (sCD16) changes following administration of RO7297089 to support clinical trials. Unbound and total RO7297089 concentrations were measured in cynomolgus monkeys. RO7297089 exhibited a bi-phasic systemic concentration-time profile, similar to a typical human immunoglobulin 1 antibody. Target engagement by RO7297089 led to a robust increase (~100-fold) in total systemic sBCMA levels and relatively mild increase (~2-fold) in total sCD16 levels. To describe the relationship of nonclinical PK/PD data, we developed a target-mediated drug disposition (TMDD) model that includes the systemic target engagement of membrane BCMA (mBCMA), sBCMA, membrane CD16 (mCD16), and sCD16. We then used this model to simulate the PK/PD relationship of RO7297089 in MM patients by translating relevant PK parameters and target levels, based on the literature and newly generated data such as baseline sCD16A levels. Our model suggested that the impact of TMDD on RO7297089 exposure may be more significant in MM patients due to significantly higher expression levels of both mBCMA and sBCMA compared to healthy cynomolgus monkeys. Based on model simulations, we propose more frequent dosing of RO7297089 compared to regular monthly frequency in the clinic at the beginning of treatment to ensure sustained target engagement. This study demonstrates a translational research strategy for collecting relevant nonclinical data, establishing a TMDD model, and using simulations from this model to inform clinical dose regimens.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) is caused by the accumulation of malignant plasma cells in bone marrow triggering damage to the kidneys, bones, immune system, and other organs. The American Cancer Society estimated 32,110 new MM cases and 12,960 MM-related deaths in the USA in 2019 alone (1). Although many therapeutics have been developed for MM in recent years, these only slow disease progression resulting in relapsed or refractory MM with an overall survival less than a year (2, 3). Thus, there is a significant unmet need for novel therapeutics that treat MM.
B-cell maturation antigen (BCMA), a membrane receptor required for plasma cell survival, is a promising therapeutic target for MM. Membrane BCMA (mBCMA) is almost exclusively expressed on plasmablasts and differentiated plasma cells and is overexpressed in MM patients (4). The level of soluble BCMA (sBCMA), the shed extracellular fraction of mBCMA, is also associated with MM disease progression (5, 6). Studies have reported sBCMA as a biomarker to monitor clinical status and therapeutic response of relapsed/refractory MM patients on active treatment (5, 6). Several cancer therapeutics targeting BCMA are in clinical development and had positive clinical trials results, including an approved anti-BCMA antibody-drug conjugate (7), an approved BCMA-specific chimeric antigen receptor (CAR) T-cells (8, 9), and an anti-BCMA CD3-bispecific T-cell engager (BITE) on clinical trial (4).
The bispecific, tetravalent antibody, RO7297089, which binds specifically to BCMA and CD16A (also known as FcγRIIIa), was generated for MM treatment (10) and tested in the phase 1 clinical trial in relapsed/refractory MM (RRMM, Study NCT04434469). CD16A is a transmembrane receptor expressed exclusively on natural killer (NK) cells and macrophages with high expression levels (11,12,13). Engagement of both BCMA on malignant plasma cells and CD16A on NK cells triggers NK cell-mediated killing of BCMA-expressing malignant plasma cells, a process known as antibody-dependent cellular cytotoxicity (ADCC) (10). Macrophage-mediated phagocytosis (i.e., antibody-dependent cellular phagocytosis, ADCP) of malignant plasma cells may also be a mechanism of action (MoA) as CD16A is found on macrophages (14). However, compared to other antibodies, RO7297089 does not bind to other FcγR including CD16B (10) because it is an effectorless antibody and its binding is specific to CD16A via two anti-CD16A single-chain variable fragments with ~100-fold stronger affinity than regular antibody Fc-CD16A interaction.
Our previous work demonstrated that RO7297089 bound to human and cynomolgus monkey BCMA and CD16 (the only gene present in non-human primates that is homologous to human CD16A with 91.3% sequence identify and specifically expressed in NK cells and macrophages (15)) with high affinity and specificity (10). RO7297089 showed robust potency against cell lines with varying BCMA expression levels in the presence of bone marrow mononuclear cells (BMMCs) and NK cells isolated from the same MM patients (10). Unlike T-cell engagers (16, 17), we observed minimal increases in TNFa and IFNg, but not other cytokines/chemokines, in the presence of the BCMA-expressing MM tumor cell line (10). RO7297089 was well tolerated following five weekly intravenous administrations to monkeys at 0, 15, and 50 mg/kg. There were no adverse events, including cytokine release syndrome, at up to 50 mg/kg, nor an apparent change in numbers of circulating plasma cells or activated NK cells following single or repeat treatment with RO7297089. Observed decreases in serum IgM levels and mRNA gene expression levels of plasma cell markers (BCMA and J chain) indicated RO7297089-related in vivo pharmacological activity at 15 and 50 mg/kg (10).
In this study, we present a translational research strategy to support the clinical development of RO7297089. We collected pharmacokinetics (PK) of RO7297089, total sBCMA level, and total soluble CD16 (sCD16) level in the above-described cynomolgus monkey studies to establish a target-mediated drug disposition (TMDD) model. We then used the TMDD model to predict the PK/pharmacodynamic (PD) relationship of RO7297089 in MM patients and to inform the dose regimen for the current phase 1 clinical trial (study NCT04434469).
Materials and Methods
Anti-BCMA/CD16A Bispecific Molecule (RO7297089)
The anti-BCMA/CD16A molecule was in-licensed from Affimed GmbH, and RO7297089 was generated by Genentech. It is comprised of a humanized anti-BCMA antibody with two identical light and heavy chains of human IgG1 isotype and two anti-CD16A single-chain variable fragments (scFv) that are genetically fused to the C-terminal end of the IgG heavy chain residue G446 (EU nomenclature) via a (G4S)6 linker sequence. Additional amino acid changes were made to impair binding to human Fc gamma-receptors and attenuate Fc-mediated effector function.
Animal Housing and Procedure
The single-dose cynomolgus monkey study was performed at the Covance Preclinical Services GmbH test facility (Germany) and the repeat-dose cynomolgus monkey study was performed at the Covance Laboratories (UK). Both sites were fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care. All study procedures complied with the Animal Welfare Act and were approved by the local Institutional Animal Care and Use Committee.
Single-Dose Cynomolgus Monkey Study
A total of eight healthy male cynomolgus monkeys (2.9–7.0 kg) and four healthy female cynomolgus monkeys (2.9–4.5 kg) were included in the study. All animals were between 2 and 3 years old. Two males and one female were randomly assigned to each treatment group and received a single 1-h intravenous (IV) infusion of vehicle solution, or 5, 15, or 45 mg/kg of RO7297089. Approximately 1 mL of blood was sampled from the vena femoralis of each individual animal at multiple time points post-drug administration (Supplementary Fig. 1A). Blood samples were processed to obtain serum and evenly aliquoted for measuring unbound RO7297089 and ADA. All animals were euthanized via sedation by intramuscular injection of ketamine hydrochloride, followed by an IV sodium pentobarbital overdose prior to exsanguination. All collected samples were stored at −70°C before assessment.
Repeat-Dose Cynomolgus Monkey Study
The repeat-dose study was conducted in healthy cynomolgus monkeys between 2 and 3 years old (2.5–3.1 kg). Two male and two female animals were randomly assigned to each treatment group and received weekly 2-h IV infusion of vehicle solution, or 15, or 50 mg/kg/injection of RO7297089 for five injections. Approximately 0.2–0.5 mL blood was sampled at previously specified time points (Supplementary Fig. 1B) to isolate serum for assessing total RO7297089 concentration and ADA. To measure total sBCMA and sCD16 concentration in systemic circulation, 1.0 mL blood was obtained from the femoral or cephalic vein of each animal at pre-dose and 3, 7, 14, 21, 28, and 30 days post-treatment initiation and split into two tubes to measure target levels. Blood was centrifuged to obtain plasma. In addition to total sBCMA and sCD16 levels, systemic IgM level and RNA expression of plasma cells markers (such as J-chain and BCMA) (18) were evaluated and presented previously (10). All animals were euthanized using the same method described above. All samples were stored at −60 to −80°C before assessment.
Assay Development
Unbound RO7297089 concentration was measured by an ELISA assay with CD16A-human Fc for capture, BCMA-rabbit Fc for detection, and a horseradish peroxidase (HRP) conjugated donkey anti-rabbit IgG as secondary detection. The lower limit of quantitation (LLOQ) of the assay was 0.39 nM in cynomolgus monkey sera.
Total RO7297089 concentration (including unbound RO7297089, sBCMA-RO7297089 complex, RO7297089-sCD16 complex, and sBCMA-RO7297089-sCD16 complex) was analyzed using a method entitled a hybrid immunoaffinity capture liquid chromatography with tandem mass spectrometry (LC-MS/MS) method for the quantitation of RO7297089 in cynomolgus monkey serum, which was validated at Pharmaceutical Product Development (PPD), LLC. The LLOQ for neat samples was 25.0 nM. The method and validation of the assay for the measurement of RO7207089 is similar to what is described previously (19).
Total sBCMA concentration (including unbound sBCMA, sBCMA-RO7297089 complex, and sBCMA-RO7297089-sCD16 complex) was assessed using a hybrid immunoaffinity capture LC-MS/MS assay. The assay uses biotinylated goat anti-BCMA polyclonal antibody (does not compete with RO7297089 for BCMA binding) for capture. Streptavidin magnetic beads were then used to enrich the immune-complex. Because BCMA is too large for practical direct quantitative analysis using LC-MS/MS technology, the analyte captured on the beads was subjected to proteolysis with trypsin, following standard protein denaturation, reduction, and alkylation processing steps. The characteristic peptide fragments produced by this procedure can then be quantified as surrogates of soluble BCMA concentrations by LC-MS/MS (i.e., multiple reaction monitoring or MRM). The LLOQ for neat samples was 5 nM.
Total soluble CD16 concentration (including unbound sCD16, RO7297089-sCD16 complex, and sBCMA-RO7297089-sCD16 complex) was assessed using an ELISA. Plasma samples diluted 1/10 in buffer containing 75 μg/mL of RO7297089 were incubated before being added to a 96-well streptavidin microplate containing biotinylated anti-CD16a rabbit monoclonal antibody (does not compete with RO7297089 for CD16 binding). Human BCMA-Fc conjugated to digoxigenin was then added for detection. Horseradish peroxidase (HRP)-conjugated mouse monoclonal anti-digoxin followed by KPL TMB microwell peroxidase substrate were added for color development. The reaction was stopped with 1.0 M phosphoric acid and the plate was read on a platereader at 450 nm. The data was analyzed with a 4 parameter fit and 1/Y weighting factor. The LLOQ for neat samples was 2.5 nM.
The detection of ADAs to RO7297089 was performed using a bridging ELISA that utilized biotin-conjugated RO7297089 and digoxigenin (DIG)-conjugated RO7297089 to capture ADAs and an HRP-conjugated mouse anti-DIG antibody for detection. Using a mouse anti-human IgG antibody as a surrogate positive control, the relative sensitivity was determined to be 48.2 ng/mL, and the assay was able to detect 1000 ng/mL of the surrogate positive control in the presence of up to 400 ug/mL of RO7297089.
Data Analyses and PK Parameter Calculation
All graphs were plotted using Prism (GraphPad Inc., CA). Nominal sample collection times and nominal dose solution concentrations were used in data analysis. All PK analyses were based on individual animal data. Data from both ADA-positive and -negative animals were included in the PK parameter calculation. The PK parameters from both single-dose and repeat-dose cynomolgus monkey studies were calculated using non-compartmental analyses with Phoenix® WinNonlin® version 6.4 (Certara USA, Inc., NJ). The following PK parameters were calculated for the single-dose cynomolgus monkey study: maximum observed concentration (Cmax); area under the serum concentration-time curve from the end of infusion to the last measurable time point (AUC0-last); area under the concentration-time curve from day 0 to infinity (AUC0-inf); percentage of the AUC0-inf area determined by extrapolation (AUCinf %Extra); systemic clearance (CL); volume of distribution at steady state (Vss). The following parameters were obtained for the repeat-dose study: maximum observed concentration after first drug administration (Cmax Day 0) and fourth drug administration (Cmax Day 21); area under the serum concentration-time curve in the first dosing interval (AUC0-7) and fourth dosing interval (AUC21-28); area under the serum concentration-time curve from the end of infusion to the last measurable time point (AUC0-last); and accumulation ratio (AR) calculated as AUC21-28 / AUC0-7.
TMDD Model Development
A TMDD model was established to characterize the unbound and total RO7297089, total sBCMA, and total sCD16 concentrations from each individual animal (20, 21). The model structure is presented in the figures and a detailed explanation of the model parameters is shown in the table. The equations that describe the model are shown below:
Systemic PK of RO7297089 was described using a two-compartment model (Eqs. 1 and 2). V1 and V2 are volumes of distribution from central and peripheral compartments, respectively. CLD and CL are the intercompartmental and systemic clearance. RO7297089 could bind to both membrane and soluble targets reversibly in the central compartment.
Target binding kinetics were described using the dissociation constant kD and binding constant kon. Baseline levels of mBCMA, sBCMA, mCD16, and sCD16 are represented as CmBCMA (0), CsBCMA (0), CmCD16 (0), and CsCD16 (0). The kinetics of membrane and soluble targets were described in the model by a first-order elimination and a zero-order synthesis (Eqs. 3–14). The elimination of mBCMA and mCD16 was described as a combination of both target-shedding and endogenous degradation/internalization (Eqs. 4 and 8). The degradation rate constants of mBCMA (kdeg mBCMA), sBCMA (kdeg sBCMA), mCD16 (kdeg mCD16), and sCD16 (kdeg sCD16) were described by 0.693/half-life (Eqs. 15–18). The synthesis rates of both soluble and membrane targets were assumed to be constant during the study since we did not observe significant change of plasma and NK cells during the nonclinical study. Since the shedding of mBCMA or mCD16 was regarded as the only source of sBCMA or sCD16, the shedding rate of mBCMA (kshed_B) or mCD16 (kshed_C) is the synthesis rate of sBCMA or sCD16 (Eqs. 21 and 22). The synthesis rate of mBCMA and mCD16 was expressed as Eqs. 20 and 22. The elimination rates of soluble complexes (i.e., mAb-sBCMA, mAb-sCD16, and mAb-sBCMA-sCD16) were described by the adjusted clearance of RO7297089 (i.e., \({k}_{Complex}\bullet \frac{CL}{V_1}\)). The elimination rates of membrane complex (i.e., mAb-mBCMA, mAb-mCD16, mAb-mBCMA-sCD16, mAb-sBCMA-mCD16, and mAb-mBCMA-mCD16) were mainly driven by the membrane target internalization rates. The model parameters were simultaneously estimated using the particle swarm global fitting algorithm and combined error model from MATLAB® (Version 2018b) SimBiology® (MathWorks, MA).
Human Translation with TMDD Model
Several parameters of the TMDD model were adjusted accordingly for human translation. The PK parameters (CLD, CL, V1, and V2) in humans were adjusted using an allometric scaling method described by Deng R, et al. (22). Baseline sBCMA levels in different MM patient populations have been reported by multiple groups and are significantly higher than the levels in healthy cynomolgus monkeys (23,24,25,26). Since RO7297089 is designed for the treatment of RRMM, we used the reported sBCMA level in RRMM patients (26), which was 41-fold higher than the observed sBCMA level in healthy cynomolgus monkeys. mBCMA level in RRMM patients is unknown and therefore needs to be estimated. Since shedding of mBCMA is the only source of sBCMA and it was found positively correlated with the cell surface mBCMA expression and number of malignant plasma cells (24), the model assumed that mBCMA was also 41-fold higher in MM patients compared to healthy cynomolgus monkeys (the same fold-increase with sBCMA level). To address the uncertainty around this assumption, an additional ±30% variation was applied to the mBCMA level estimate. Baseline sCD16A levels in RRMM patients were measured and reported in this manuscript. The mCD16A levels were estimated by the same approach as the estimate of mBCMA, assuming sCD16A and mCD16A have the same fold-change in MM patients compared to cynomolgus monkeys with a ±30% variation included.
Results
Unbound RO7297089 Concentrations Exhibit Nonlinear Systemic PK in a Single-Dose Cynomolgus Monkey Study
We first assessed serum unbound concentrations of RO7297089 in cynomolgus monkeys using an enzyme-linked immunosorbent assay (ELISA) over 14 days following single intravenous (IV) administration of RO7297089 at 5, 15, or 45 mg/kg (N = 3 animals/group) (Supplementary Fig. 1A). The three dose levels were selected based on the experience from other NK cell engagers such as AFM13 (anti-CD30/CD16A) to enable assess the PK, PD, and toxicity of RO7297089 within the large dose range.
As this ELISA used CD16A-human Fc for capture and BCMA-rabbit Fc for detection, RO7297089 was measured as unbound drug as long as it had at least one unbound CD16A arm to be captured and at least one unbound BCMA arm to be detected. RO7297089 exhibited an approximately bi-phasic serum concentration-time profile in cynomolgus monkeys, which is similar to the PK profile for a typical human immunoglobulin 1 (hIgG1) antibody (Fig. 1). The systemic exposure (AUC0-last) of RO7297089 was slightly greater than dose-proportional, and the systemic CL decreased as dose increased. In contrast, no significant change in the volume of distribution at steady state (Vss) was observed at different doses (Table I). Seven out of nine animals developed anti-drug antibodies (ADAs) by the end of the study (concentration-time profiles of ADA-positive animals are shown as dashed curves in Fig. 1). As all the animals in the two lower dose groups (i.e., 5 and 15 mg/kg) were ADA-positive, the nonlinear and rapid reduction of unbound drug concentration after day 7 post-drug administration could be due to these ADAs.
Serum concentration-time profiles of unbound RO7297089 for each individual cynomolgus monkey following single IV administration of 5, 15, or 45 mg/kg drug. Animals with or without ADA are represented as dash and solid curves, respectively. The concentrations of unbound RO7297089 on day 14 from the 5 mg/kg treatment group are not shown as they were below LLOQ
Total RO7297089 Concentrations Exhibit Linear Systemic PK in the Repeat-Dose Cynomolgus Monkey Study
In addition to the unbound RO7297089 concentrations, we measured total serum concentration of RO7297089 (including unbound RO7297089, sBCMA-RO7297089 complex, RO7297089-sCD16 complex, and sBCMA-RO7297089-sCD16 complex) following weekly IV administration at 15 and 50 mg/kg in a 4-week repeat-dose study in cynomolgus monkeys (Fig. 2, Supplementary Fig. 1B). The systemic exposure of total RO7297089, reflected by Cmax and AUC in the 1st and 4th dosing interval, exhibited an approximately dose-proportional increase in the tested dose range (Table II). Accumulation (comparing AUC between 1st and 4th dose intervals) of total RO7297089 was observed at 50 mg/kg, but was not apparent at 15 mg/kg. ADAs were observed in four out of six animals from both the 15 mg/kg and 50 mg/kg dose groups. Apparent loss of exposure was observed only in three ADA-positive animals (animals P0103, P0402, P0403) from the 15 mg/kg dose group but not in the other five ADA-positive animals. ADA does not have an impact on PK at 50 mg/kg, which could be due to high systemic drug concentrations saturating the ADA and overcoming the loss of exposure due to ADA. Sex has no significant impact on the PK of RO7297089 (Supplementary Table 1).
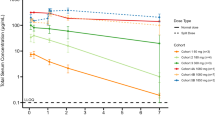
Increases in Plasma Total sBCMA and sCD16 Following Drug Administration Suggests Systemic Target Engagement of RO7297089
We next measured total sBCMA (including unbound sBCMA, sBCMA-RO7297089 complex, and sBCMA-RO7297089-sCD16 complex) and sCD16 (including unbound sCD16, RO7297089-sCD16 complex, and sBCMA-RO7297089-sCD16 complex) concentrations for the repeat-dose cynomolgus monkey study using liquid chromatography with tandem mass spectrometry (LC-MS/MS) and ELISA method respectively. We observed a robust 100 to 200-fold increase in total plasma sBCMA concentrations in all animals 3 days after first drug administration (Fig. 3A–C). In contrast, no increase in plasma sBCMA concentrations was observed in animals from the vehicle treatment group. We attributed sBCMA accumulation to RO7297089 binding and stabilization. Similar accumulation of systemic targets post-antibody treatment has been reported for other soluble targets with small molecular weight and short systemic half-life, such as VEGF (27, 28). Like VEGF, sBCMA has a much lower molecular weight than hIgG1 (5.3 vs. 150 kDa) (10). This explanation is further supported by total sBCMA concentrations in the three animals from 15 mg/kg group that did not maintain systemic exposures (i.e., animals P0103, P0402, and P0403). In these three animals, total sBCMA returned to baseline by day 28, whereas the animals without exposure loss maintained increased total sBCMA levels throughout the study. Similarly, an increase of total sCD16 was observed in plasma post-drug administration (Fig. 3A–F), although the extent of increase was smaller compared to sBCMA (2- vs. 100-fold from baseline).
Development of a TMDD Model for Characterizing PK and PD Data from Both Single- and Repeat-Dose Cynomolgus Monkey Studies
We developed a TMDD model to explain the PK and PD data from the two cynomolgus monkey studies reported above (Fig. 4). A two-compartment model with binding components to both soluble and membrane BCMA and CD16 was used to describe the PK of RO7297089 and sBCMA levels (see Material and Methods). We estimated all model parameters by simultaneously fitting the model to the observed unbound and total RO7297089 serum concentrations as well as the total sBCMA and sCD16 plasma levels from each individual animal (Table III). Data from both cynomolgus monkey studies were used for model fitting. However, we excluded the three ADA-positive animals in the repeat-dose study with apparent loss of systemic drug exposure (i.e., animals P0103, P0402, P0403). The model fits the observed total serum RO7297089, total plasma sBCMA, and total sCD16 concentrations well but did not accurately capture the rapid reduction of unbound RO7297089 concentration in the animals from 5 to 15 mg/kg treatment groups in the single-dose study after day 7 (Fig. 5). The rapid reduction of unbound RO7297089 after day 7 could be due to TMDD, which the model failed to capture, or due to the impact of ADA on the systemic exposure as all animals from the 5 and 15 mg/kg single-dose study groups were ADA-positive.
Schematic of the two-compartment TMDD model used to describe the systemic PK and PD of RO7297089. Systemic RO7297089 (AmAb central and V1) can distribute to peripheral tissues (AmAb peri, V2, CLD), undergo clearance (CL), and bind to soluble and membrane BCMA (kon_B, kD_B) or CD16 (kon_C, kD_C). Baseline levels of mBCMA, sBCMA, mCD16, and sCD16 are expressed as CmBCMA (0), CsBCMA (0), CmCD16 (0), and CsCD16 (0). The synthesis rate of mBCMA, sBCMA, mCD16, or sCD16 is expressed as ksyn mBCMA, ksyn sBCMA, ksyn mCD16, or ksyn mCD16. The degradation rate of free mBCMA, sBCMA, mCD16, or sCD16 is expressed as kdeg mBCMA, kdeg sBCMA, kdeg mCD16, or kdeg sCD16. Shedding of mBCMA (kshed_B) or mCD16 (kshed_C) is the only source of sBCMA or sCD16. The model assumes that internalization with mBCMA is the major cause of RO7297089-mBCMA complex elimination. The elimination rate of RO7297089-sBCMA may be slightly different from the elimination rate of RO7297089 alone. See Table III for a more detailed explanation and model estimates of the parameters
Assessment of model fitting through comparison of fitted vs. observed concentrations. Comparison of observed vs. predicted A–C unbound serum RO7297089 concentration (5, 15, and 45 mg/kg single dose), D–E total serum RO7297089 concentration, and total plasma sBCMA and sCD16 concentrations (15 and 50 mg/kg repeat dose) in cynomolgus monkeys. Observed concentration data are represented as open circles and predicted mean concentration data are represented as dashed curves. Data from three ADA-positive animals in 15 mg/kg group from the repeat-dose study (15 mg/kg) with apparent loss of drug exposure due to ADA were not used for fitting as all animals were ADA-positive
The comparison of observed value vs. model prediction and results of residual analysis also suggested no apparent bias in overall model fits except for the unbound RO7297089 concentrations (Supplementary Fig. 2). Most model parameters were estimated with good confidence, reflected by parameter estimate relative variability (CV%) below 30%, except for the half-life of sBCMA (\({t}_{\frac{1}{2}\ sBCMA}\), CV% = 45.3%), baseline level of mCD16 (C mCD16 (0), CV% = 77.1%), and half-life of mCD16 (\({t}_{\frac{1}{2}\ mCD16}\), CV% = 78.3%). All these parameters with relatively high CV% are related to target dynamics. This could be due to very limited data on target dynamics, especially membrane targets.
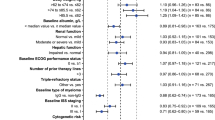
TMDD Model Suggests Frequent Dosing to Maintain Constant Target Engagement
In MM patients, CD16A and BCMA levels were expected to be different from healthy cynomolgus monkeys. While the sCD16A level in MM patients was slightly lower than in cynomolgus monkeys (Supplementary Table 2), both mBCMA and sBCMA were significantly higher (23,24,25,26). sBCMA can be a systemic sink that competes with the membrane target for drug binding. We used the TMDD model to explore the impact of soluble and membrane target levels on RO7297089 dose regimen in MM patients by translating the relevant PK parameters and target levels from cynomolgus monkeys to MM patients. The sBCMA levels in MM patients vary significantly between patient populations and studies (23,24,25). We selected median sBCMA levels in the target population (i.e., RRMM patients) from the study published by Rathi et al. (Supplementary Table 2), which was ~41-fold higher than the sBCMA level in healthy cynomolgus monkeys (26). mBCMA levels in MM patients remain unknown. However, mBCMA levels are expected to be higher in MM patients compared to healthy monkeys because sBCMA was positively correlated with the cell surface mBCMA expression and number of malignant plasma cells (24); thus, we assumed that mBCMA in MM patients was also 41-fold higher compared to the estimated level in healthy cynomolgus monkeys. Baseline levels of sCD16A in both healthy volunteers and RRMM patients were measured (Fig. 6). mCD16A levels were estimated using the same approach, assuming sCD16A and mCD16A have similar fold-changes in MM patients compared to cynomolgus monkeys. A ±30% variation was applied to the mBCMA and mCD16A level estimates. For the adjustment of PK parameters, an allometric scaling method reported by Deng et al. was used (assuming human body weight of 70 kg; for volume and clearance, the exponents of 1 and 0.85 were used, respectively) (22).
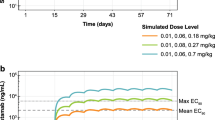
The TMDD model simulations suggest that while IV administration of 10 mg/kg RO7297089 every 3 weeks (q3w) can achieve > 80% mBCMA and mCD16A target engagement in healthy cynomolgus monkeys (Fig. 7A, B), a significantly higher dose of 30 mg/kg q3w IV administration of RO7297089 is required to achieve similar target engagement in MM patients (Fig. 7C, D). This is a result of unbound RO7297089 concentrations predicted from the simulations, which could not be maintained in the MM patients due to high sBCMA and mBCMA load (Supplementary Fig. 3). Increasing the dose frequency enabled sustained mBCMA and mCD16A target engagement throughout the 63 days with a lower dose of > 3 mg/kg (Fig. 7E, F). Besides engagement with membrane targets, the concentrations of RO7297089-mBCMA-mCD16A complex could be related to efficacy because engagement with both mBCMA and mCD16A is required for RO7297089 to achieve its tumor-killing effects (Supplementary Fig. 4). Consistent with the simulations on target engagement, the model simulation on RO7297089-mBCMA-mCD16A complex also recommended weekly dose frequency (Supplementary Fig. 4B, C). These simulations suggest that a higher dose frequency of RO7297089 compared to a typical q3w dosing regimen of antibody therapeutics may be necessary to achieve sufficient target engagement in MM patients at the beginning of treatment when BCMA levels are high.
Simulated mBCMA and mCD16A target engagement at different dose levels and dose frequencies in A–B healthy cynomolgus monkeys and C–F MM patients using the TMDD model. Fraction of bound mBCMA and mCD16A was simulated with a q3w dose frequency in cynomolgus monkeys and with both q3w and qw dose frequencies in MM patients. For the simulation in MM patients, a ±30% variation was added to the estimated mBCMA and mCD16A levels to address the uncertainties of membrane target levels in human
Discussion
In the present study, we report the nonclinical PK/PD for RO7297089, an anti-BCMA/CD16A bispecific antibody, in cynomolgus monkeys and describe a translational strategy to identify potential dosing regimens to maximize target engagement in MM patients. We collected nonclinical PK/PD and target engagement information from cynomolgus monkeys, the only relevant nonclinical, cross-reactive species (10). We assessed the systemic concentrations of unbound and total RO7297089 in two separate studies to generate a comprehensive profile of RO7297089 PK. We observed that exposure of unbound RO7297089 in a single-dose monkey study was slightly greater than dose-proportional. In contrast, the exposure of total RO7297089 was approximately dose-proportional in the repeat-dose monkey study. The nonlinearity of unbound RO7297089 concentration might be due to the engagement with membrane/soluble targets, but cannot be differentiated from potential impact of ADAs on the systemic exposure because all animals from the two low-dose groups in the single-dose study were ADA-positive. We explored the in vivo target engagement with BCMA and CD16 by measuring the total sBCMA and sCD16 levels.
The major challenge of using healthy cynomolgus monkeys for translational research of RO7297089 is the different expression levels of both membrane and soluble BCMA and CD16 compared to those in MM patients (4, 10, 17, 29). Therefore, we developed a TMDD model that used the PK-target engagement relationship in animal studies to bridge the gap between healthy cynomolgus monkeys and MM patients. The model takes into account the target engagement of both soluble and membrane targets. Similar TMDD models have been reported to describe the target engagement of a membrane target and its shed fraction. For example, the study by Li LZ, et al. established a minimal physiologically based pharmacokinetic (mini-PBPK) TMDD model to describe the clinical PK of trastuzumab and simulate its target engagement level (20). The developed TMDD model enabled evaluation of the effect of sBCMA levels on mBCMA occupancy to determine the dose range of RO7297089 in the clinical study. Our model captured not only the concentration-time profiles of RO7297089, total sBCMA, and total sCD16 but also estimated baseline levels of mBCMA and mCD16 and half-lives of both soluble and membrane BCMA and CD16. This allowed us to simulate the PK/PD relationship in MM patients.
We simulated the PK and target engagement of RO7297089 in patients by adjusting PK parameters, target binding affinity, and baseline values of soluble and membrane BCMA and CD16A in the model to a level reported in newly diagnosed untreated MM patients, the potential clinical study’s target population. It is unclear what factor determines efficacy so we explored different parameters including the saturation levels of membrane targets and the formation of RO7297089-mBCMA-mCD16A complexes. Although a q3w or monthly dose frequency has been widely applied for therapeutic antibodies, the model suggested that a high dose of 30 mg/kg was needed to achieve a sustained > 80% target engagement of mBCMA and mCD16A. This is because much stronger TMDD was predicted in MM patients when compared with the simulated PK in healthy cynomolgus monkeys at the same dose level and frequency. In contrast, an increasing dosing frequency enabled sustained target engagement by RO7297089 at a lower dose of > 3 mg/kg. These simulations suggest that at the beginning of therapy, a more frequent dose frequency may be needed to sustain engagement of both mBCMA and mCD16A.
Based on the MoA of RO7297089, an immunological synapse between NK cells/macrophage and malignant plasma cells is required for the molecule’s activity. Hypothetically, plasma levels of RO7297089-mBCMA-mCD16A complex may correlate better with efficacy than mBCMA and mCD16A target engagement. Therefore, we simulated the time profiles of RO7297089-mBCMA-mCD16A complex concentrations in plasma from MM patients with different dose levels and frequencies. Consistent with the simulations on the engagement of membrane targets, the model also suggested weekly dose frequency resulted in more sustained formation of RO7297089-mBCMA-mCD16A compared to a dose frequency of every 3 weeks. However, unlike membrane target engagement, which positively correlated with the dose level, model simulation suggested that high dose such as 30 mg/kg may limit the formation of complex since RO7297089 may bind to BCMA or CD16A separately when the concentration of RO7297089 was much higher than the target levels. Additional experiment data are needed to further validate this hypothesis.
The synthesis rates of sBCMA and mBCMA depend on the number of BCMA-expressing plasma cells. The model assumes a constant synthesis rate of both sBCMA and mBCMA as we did not observe a significant change of plasma cells in the cynomolgus monkeys during the short period of the study. However, in MM patients, the levels of both targets will decrease as malignant plasma cells are killed during active treatment. As a result, the impact of TMDD on the systemic exposure of RO7297089 may decrease during treatment, and the dose frequency of RO7297089 may need further adjustment. Our simulations suggest it is important to monitor malignant plasma cell number dynamics and total sBCMA concentration in MM patients to better characterize the PK and target engagement during future clinical studies so that the relationship between cell killing and synthesis of sBCMA can be included in the model.
Despite these challenges, this study presents a translational research strategy that combines nonclinical experimental data, published clinical information, and TMDD modeling to better understand the PK/PD relationship in nonclinical studies. This understanding allows us to overcome a variety of preclinical limitations in drug development for this difficult-to-characterize disease and to support the design of the phase 1 clinical study in MM patients, and the data of which has been published as the abstract/poster in the ASH meeting (30). Based on the simulation results, a more frequent dosing frequency was selected for the phase 1 trial on MM patients. Consistent with the model prediction, the RO7297089 exposures were rather low in patients at lower dose levels due to strong TMDD (30).
Conclusions
RO7297089, an anti-B-cell maturation antigen (BCMA)/CD16A bispecific tetravalent antibody for the treatment of MM, showed expected PK and robust target engagement in the systemic circulation from cynomolgus monkeys. The developed TMDD model was able to characterize the PK and target engagement data in cynomolgus monkeys, support the translation of PKPD relationship to MM patients, and design the dose regimen for the phase 1 clinical trial.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. Ca-Cancer J Clin. 2019;69(1):7–34. https://doi.org/10.3322/caac.21551.
Gandhi UH, Cornell RF, Lakshman A, Gahvari ZJ, McGehee E, Jagosky MH, et al. Outcomes of patients with multiple myeloma refractory to CD38-targeted monoclonal antibody therapy. Leukemia. 2019;33(9):2266–75. https://doi.org/10.1038/s41375-019-0435-7.
Usmani SZ, Weiss BM, Plesner T, Bahlis NJ, Belch A, Lonial S, et al. Clinical efficacy of daratumumab monotherapy in patients with heavily pretreated relapsed or refractory multiple myeloma. Blood. 2016;128(1):37–44. https://doi.org/10.1182/blood-2016-03-705210.
Cho SF, Anderson KC, Tai YT. Targeting B cell maturation antigen (BCMA) in multiple myeloma: potential uses of BCMA-based immunotherapy. Front Immunol. 2018;9:1821. https://doi.org/10.3389/fimmu.2018.01821.
Bujarski S, Udd K, Soof C, Chen HM, Spektor T, Safaie T, et al. Changes in serum B-cell maturation antigen levels rapidly predict progression free survival among multiple myeloma patients undergoing new treatment. Cl Lymph Myelom Leuk. 2019;19(10):E173–E4. https://doi.org/10.1016/j.clml.2019.09.290.
Udd K, Chen HM, Li MJ, Soof CM, Casas C, Etessami S, et al. Changes in serum B-cell maturation antigen levels are a more rapid indicator of therapeutic response or disease progression for patients with multiple myeloma. Blood. 2016;128(22). https://doi.org/10.1182/blood.V128.22.5654.5654.
Tai YT, Mayes PA, Acharya C, Zhong MY, Cea M, Cagnetta A, et al. Novel anti-B-cell maturation antigen antibody-drug conjugate (GSK2857916) selectively induces killing of multiple myeloma. Blood. 2014;123(20):3128–38. https://doi.org/10.1182/blood-2013-10-535088.
Raje N, Berdeja J, Lin Y, Siegel D, Jagannath S, Madduri D, et al. Anti-BCMA CAR T-cell therapy bb2121 in relapsed or refractory multiple myeloma. N Engl J Med. 2019;380(18):1726–37. https://doi.org/10.1056/NEJMoa1817226.
Fan F, Zhao WH, Liu J, He AL, Chen YX, Cao XM, et al. Durable remissions with BCMA-specific chimeric antigen receptor (CAR)-modified T cells in patients with refractory/relapsed multiple myeloma. J Clin Oncol. 2017;35(18). https://doi.org/10.1200/JCO.2017.35.18_suppl.LBA3001.
Kakiuchi-Kiyota S, Schutten MM, Adedeji AO, Cai H, Hendricks R, Liu L, et al. Preclinical pharmacology and safety of RO7297089, a novel anti-BCMA/CD16a bispecific antibody for the treatment of multiple myeloma. Cancer Res. 2020;80(16_Supplement):4556.
Pahl JHW, Koch J, Gotz JJ, Arnold A, Reusch U, Gantke T, et al. CD16A activation of NK cells promotes NK cell proliferation and memory-like cytotoxicity against cancer cells. Cancer Immunol Res. 2018;6(5):517–27. https://doi.org/10.1158/2326-6066.CIR-17-0550.
Reusch U, Burkhardt C, Fucek I, Le Gall F, Le Gall M, Hoffmann K, et al. A novel tetravalent bispecific TandAb (CD30/CD16A) efficiently recruits NK cells for the lysis of CD30+ tumor cells. mAbs. 2014;6(3):728-39. https://doi.org/10.4161/mabs.28591.
Rothe A, Sasse S, Topp MS, Eichenauer DA, Hummel H, Reiners KS, et al. A phase 1 study of the bispecific anti-CD30/CD16A antibody construct AFM13 in patients with relapsed or refractory Hodgkin lymphoma. Blood. 2015;125(26):4024–31. https://doi.org/10.1182/blood-2014-12-614636.
Li X, Ptacek TS, Brown EE, Edberg JC. Fcγ receptors: structure, function and role as genetic risk factors in SLE. Genes Immun. 2009;10(5):380–9. https://doi.org/10.1038/gene.2009.35.
Rogers KA, Scinicariello F, Attanasio R. IgG Fc receptor III homologues in nonhuman primate species: genetic characterization and ligand interactions. J Immunol. 2006;177(6):3848–56.
Hipp S, Tai YT, Blanset D, Deegen P, Wahl J, Thomas O, et al. A novel BCMA/CD3 bispecific T-cell engager for the treatment of multiple myeloma induces selective lysis in vitro and in vivo. Leukemia. 2017;31(8):1743–51. https://doi.org/10.1038/leu.2016.388.
Li J, Piskol R, Ybarra R, Chen YJ, Li J, Slaga D, et al. CD3 bispecific antibody–induced cytokine release is dispensable for cytotoxic T cell activity. Sci Transl Med. 2019;11(508):eaax8861.
Tarte K, Zhan FH, De Vos J, Klein B, Shaughnessy J. Gene expression profiling of plasma cells and plasmablasts: toward a better understanding of the late stages of B-cell differentiation. Blood. 2003;102(2):592–600. https://doi.org/10.1182/blood-2002-10-3161.
Kaur S, Liu L, Cortes DF, Shao J, Jenkins R, Mylott WR Jr, Xu K. Validation of a biotherapeutic immunoaffinity-LC–MS/MS assay in monkey serum:‘plug-and-play’across seven molecules. Bioanalysis. 2016;8(15):1565–77.
Li LZ, Gardner I, Rose R. Incorporating target shedding into a minimal PBPK-TMDD model for mAbs. J Pharmacokinet Phar. 2013;40:S90–S1.
Mager DE, Krzyzanski W. Quasi-equilibrium pharmacokinetic model for drugs exhibiting target-mediated drug disposition. Pharm Res. 2005;22(10):1589–96. https://doi.org/10.1007/s11095-005-6650-0.
Deng R, Iyer S, Theil FP, Mortensen DL, Fielder PJ, Prabhu S. Projecting human pharmacokinetics of therapeutic antibodies from nonclinical data: what have we learned? mAbs. 2011;3(1):61-6. https://doi.org/10.4161/mabs.3.1.13799.
Ghermezi M, Li MJ, Vardanyan S, Harutyunyan NM, Gottlieb J, Berenson A, et al. Serum B-cell maturation antigen: a novel biomarker to predict outcomes for multiple myeloma patients. Haematologica. 2017;102(4):785–95. https://doi.org/10.3324/haematol.2016.150896.
Lee L, Bounds D, Paterson J, Herledan G, Sully K, Seestaller-Wehr LM, et al. Evaluation of B cell maturation antigen as a target for antibody drug conjugate mediated cytotoxicity in multiple myeloma. Brit J Haematol. 2016;174(6):911–22. https://doi.org/10.1111/bjh.14145.
Sanchez E, Li MJ, Kitto A, Li J, Wang CS, Kirk DT, et al. Serum B-cell maturation antigen is elevated in multiple myeloma and correlates with disease status and survival. Brit J Haematol. 2012;158(6):727–38. https://doi.org/10.1111/j.1365-2141.2012.09241.x.
Rathi C, Collins J, Struemper H, Opalinska J, Jewell RC, Ferron-Brady G. Population pharmacokinetics of belantamab mafodotin, a BCMA-targeting agent in patients with relapsed/refractory multiple myeloma. CPT Pharmacometrics Syst Pharmacol. 2021;10(8):851–63. https://doi.org/10.1002/psp4.12660.
Eppler S, Combs D, Henry T, Lopez J, Ellis S, Yi J-H, et al. A target-mediated model to describe the pharmacokinetics and hemodynamic effects of recombinant human vascular endothelial growth factor in humans*. Clin Pharmacol Ther. 2002;72:20–32. https://doi.org/10.1067/mcp.2002.126179.
Sanchez E, Gillespie A, Tang G, Ferros M, Harutyunyan NM, Vardanyan S, et al. Soluble B-cell maturation antigen mediates tumor-induced immune deficiency in multiple myeloma. Clin Cancer Res. 2016;22(13):3383. https://doi.org/10.1158/1078-0432.CCR-15-2224.
Goldstein RL, Goyos A, Li CM, Deegen P, Bogner P, Sternjak A, et al. AMG 701 induces cytotoxicity of multiple myeloma cells and depletes plasma cells in cynomolgus monkeys. Blood Adv. 2020;4(17):4180–94. https://doi.org/10.1182/bloodadvances.2020002565.
Plesner T, et al. A phase I study of RO7297089, a B-cell maturation antigen (BCMA)-CD16a bispecific antibody in patients with relapsed/refractory multiple myeloma (RRMM). In: ASH 2021 Annual Meeting and Exposition. https://ash.confex.com/ash/2021/webprogram/Paper147418.html (2021). Accessed 6 May 2022.
Acknowledgements
We would like to thank Saroja Ramanujan and Xun Tao for helpful discussion on the TMDD model and Robert (Jinze) Li and Reginald Delarosa for their help on the cynomolgus monkey studies. We would also like to thank Anshin BioSolutions for editorial assistance.
Funding
This work was financially supported by Genentech Inc.
Author information
Authors and Affiliations
Contributions
Participated in research design: Cai, Kakiuchi-Kiyota, Adedeji, Hendricks, Zhong, Schutten, Kamath, and Ovacik. Sample analyses: Hendricks, Liu, and Chan. Data interpretation: Cai, Hendricks, Liu, and Ovacik. PKPD model: Cai and Ovacik.
Corresponding authors
Ethics declarations
Conflict of Interest
All the authors are current employees of Genentech Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 4063 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cai, H., Kakiuchi-Kiyota, S., Hendricks, R. et al. Nonclinical Pharmacokinetics, Pharmacodynamics, and Translational Model of RO7297089, A Novel Anti-BCMA/CD16A Bispecific Tetravalent Antibody for the Treatment of Multiple Myeloma. AAPS J 24, 100 (2022). https://doi.org/10.1208/s12248-022-00744-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-022-00744-8