Abstract
Background
Teclistamab, a B-cell maturation antigen × CD3 bispecific antibody, is approved in patients with relapsed/refractory multiple myeloma (RRMM) who have previously received an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 antibody.
Objective
We report the population pharmacokinetics of teclistamab administered intravenously and subcutaneously (SC) and exposure–response relationships from the phase I/II, first-in-human, open-label, multicenter MajesTEC-1 study.
Methods
Phase I of MajesTEC-1 consisted of dose escalation and expansion at the recommended phase II dose (RP2D; 1.5 mg/kg SC weekly, preceded by step-up doses of 0.06 and 0.3 mg/kg); phase II investigated the efficacy of teclistamab RP2D in patients with RRMM. Population pharmacokinetics and the impact of covariates on teclistamab systemic exposure were assessed using a 2-compartment model with first-order absorption for SC and parallel time-independent and time-dependent elimination pathways. Exposure–response analyses were conducted, including overall response rate (ORR), duration of response (DoR), progression-free survival (PFS), overall survival (OS), and the incidence of grade ≥ 3 anemia, neutropenia, lymphopenia, leukopenia, thrombocytopenia, and infection.
Results
In total, 4840 measurable serum concentration samples from 338 pharmacokinetics-evaluable patients who received teclistamab were analyzed. The typical population value of time-independent and time-dependent clearance were 0.449 L/day and 0.547 L/day, respectively. The time-dependent clearance decreased rapidly to < 10% after 8 weeks of teclistamab treatment. Patients who discontinue teclistamab after the 13th dose are expected to have a 50% reduction from Cmax in teclistamab concentration at a median (5th to 95th percentile) time of 15 days (7–33 days) after Tmax and a 97% reduction from Cmax in teclistamab concentration at a median time of 69 days (32–163 days) after Tmax. Body weight, multiple myeloma type (immunoglobulin G vs non–immunoglobulin G), and International Staging System (ISS) stage (II vs I and III vs I) were statistically significant covariates on teclistamab pharmacokinetics; however, these covariates had no clinically relevant effect on the efficacy of teclistamab at the RP2D. Across all doses, ORR approached a plateau at the concentration range associated with RP2D, and in patients who received the RP2D, a flat exposure–response curve was observed. No apparent relationship was observed between DoR, PFS, OS, and the incidence of grade ≥3 adverse events across the predicted exposure quartiles.
Conclusion
Body weight, myeloma type, and ISS stage impacted systemic teclistamab exposure without any clinically relevant effect on efficacy. The exposure–response analyses for ORR showed a positive trend with increasing teclistamab systemic exposure, with a plateau at the RP2D, and there was no apparent exposure–response trend for safety or other efficacy endpoints. These analyses support the RP2D of teclistamab in patients with RRMM.
Clinical Trial Registration
NCT03145181 (phase I, 09 May 2017); NCT04557098 (phase II, 21 September 2020).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The introduction of immunomodulatory agents (IMiDs), proteasome inhibitors (PIs), and anti-CD38 antibodies has led to improved survival outcomes for patients with multiple myeloma [1]. However, outcomes remain suboptimal for patients with relapsed/refractory disease [2, 3]; for these patients, the remission duration decreases with each subsequent treatment regimen administered [1].
B-cell maturation antigen (BCMA) represents a promising new treatment target. Few BCMA-targeting agents are currently approved for the treatment of heavily pretreated patients with relapsed/refractory multiple myeloma (RRMM) by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA); these include teclistamab and the chimeric antigen receptors T-cell (CAR-T) therapies idecabtagene vicleucel and ciltacabtagene autoleucel [4,5,6,7,8,9]. Patient access remains a challenge for CAR-T therapy, and strict inclusion criteria may prohibit some patients benefiting from promising overall response rates (ORR) of 67–83% [10,11,12]. Combined with the relatively modest ORR observed with the BCMA-targeting antibody drug conjugate belantamab mafodotin (31%) [13], which was recently withdrawn from the US market at the request of the FDA, there remains a significant unmet need for improved therapies for heavily pretreated patients with RRMM.
Teclistamab is the first BCMA × CD3 bispecific antibody approved for the treatment of triple-class–exposed RRMM. Teclistamab redirects CD3+ T cells to mediate T-cell activation and subsequent lysis of BCMA-expressing multiple myeloma cells [14]. MajesTEC-1 is a phase I/II trial designed to identify the recommended phase II dose (RP2D) of teclistamab in patients with RRMM who were relapsed, refractory, or intolerant to established therapies (ClinicalTrials.gov identifier: NCT03145181) [15]. The pivotal phase II portion of the trial (NCT04557098) assessed the efficacy and safety of weekly teclistamab at the RP2D of 1.5 mg/kg via subcutaneous (SC) injection, preceded by two step-up doses of 0.06 mg/kg and 0.3 mg/kg, in patients with RRMM who had progressed after at least three prior lines of therapy, including those who were triple-class exposed (i.e., exposed to a PI, an IMiD, and an anti-CD38 monoclonal antibody) [16]. In patients who received the RP2D of teclistamab across both phases of the trial, treatment resulted in a high rate of deep and durable response in patients with triple-class–exposed RRMM, and although adverse events (AEs) were common, they were mainly of low grade and reversible [15, 16]. Based on the results from the MajesTEC-1 trial, teclistamab was approved by the EMA as a monotherapy for the treatment of adult patients with RRMM who have received at least three prior therapies, including an IMiD, a PI, and an anti-CD38 antibody, and have demonstrated disease progression on the last line of therapy [6]. The FDA has also approved teclistamab for the treatment of patients with RRMM after receiving four lines of prior therapy, including a PI, an IMiD, and an anti-CD38 monoclonal antibody [9].
Here, we report the population pharmacokinetics (PK) of teclistamab administered intravenously (IV) and SC and the exposure–response relationships for efficacy and safety in patients with RRMM treated in the MajesTEC-1 trial.
2 Methods
2.1 Study Design
The population PK and exposure–response analyses included data from the phase I/II, first-in-human, open-label, multicenter MajesTEC-1 trial (ClinicalTrials.gov: NCT03145181 [phase I]; NCT04557098 [phase II]). The full study design has been described previously [15, 16]. Briefly, the MajesTEC-1 study enrolled patients aged ≥ 18 years with documented diagnosis of RRMM according to International Myeloma Working Group criteria [17]. In phase I, patients must have relapsed or been refractory or intolerant to established therapies [15]. In phase II, patients must have previously received at least three lines of therapy (including an IMiD, a PI, and an anti-CD38 antibody) and had progressive, measurable disease at screening, as well as an Eastern Cooperative Oncology Group (ECOG) performance status score of 0 or 1 [16].
The study consisted of 3 parts: phase I dose escalation (part 1), phase I dose expansion at the RP2D (part 2), and phase II dose expansion at the RP2D in patient cohorts with an unmet medical need (part 3). Phase I dose escalation consisted of teclistamab from 0.0003 mg/kg up to 0.0192 mg/kg every 2 weeks (Q2W) IV, from 0.0192 mg/kg up to 0.01/0.06/0.24 mg/kg then 0.72 mg/kg weekly (QW) IV, from 0.02 mg/kg then 0.08 mg/kg QW SC to 0.06/0.3/1.5 mg/kg then 6 mg/kg SC, and a flat dose of 2/6/30 mg followed by 150/300 mg QW/Q2W SC. Phase I dose expansion investigated teclistamab at 0.01/0.06/0.24 mg/kg then 0.72 mg/kg QW IV and the SC RP2D (SC 1.5 mg/kg QW, with the first treatment dose preceded by step-up doses of 0.06 mg/kg and 0.3 mg/kg). Phase II dose expansion investigated the RP2D in patients with RRMM who were triple-class exposed and had previously received three or more prior lines of therapy (cohort A) and in patients who had received three or more prior lines of therapy, including a PI, an IMiD, and an anti-CD38 antibody, as well as an anti-BCMA treatment with either a CAR-T or antibody drug conjugate therapy (cohort C). Patients received RP2D treatment until the occurrence of disease progression, unacceptable toxicity, withdrawal of consent, death, or the end of the study.
Serial PK sampling was conducted after the first full treatment dose in cycle 1 and cycle 3 in phase I of the trial, while sparse PK sampling was used for phase II dose expansion. Key elements regarding study doses and PK sampling are summarized in Suppl. Table 1 (see electronic supplementary material [ESM]).
2.2 Objectives and Analysis Populations
The aim of this analysis was to characterize the population PK of teclistamab (IV and SC) in patients with RRMM and to evaluate the effects of demographic characteristics, disease characteristics, prior treatment, and other intrinsic or extrinsic factors on teclistamab systemic exposure. Additional objectives were to explore the exposure–response relationship for selected efficacy endpoints, including ORR, duration of response (DoR), progression-free survival (PFS), and overall survival (OS), as well as to explore the exposure–response relationship for selected safety endpoints, including the incidence of grade ≥ 3 anemia, neutropenia, lymphopenia, leukopenia, thrombocytopenia, and infection in patients who received teclistamab SC. Response was assessed via independent review committee per International Myeloma Working Group criteria [17] and AEs relevant to this analysis were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 4.03.
The population PK analysis included patients from the phase I dose escalation and expansion and phase II dose expansion (cohorts A and C [triple-class exposed and prior BCMA-directed therapy]) portions of the MajesTEC-1 trial who received at least one dose of teclistamab and had at least one quantifiable teclistamab concentration. The PK data cutoff was December 1, 2021.
Patients who received teclistamab SC dosing in the phase I dose escalation and expansion and phase II dose expansion (cohort A) portions of the MajesTEC-1 trial were included in the exposure–response analysis for efficacy and safety. Patients treated with the RP2D were the focus of the exposure–response efficacy analysis. ORR, DoR, PFS, and OS were assessed in patients who received the RP2D in the phase I and II (cohort A) portions of the trial (N = 165). ORR was also assessed in patients who received phase I dosing in the SC cohorts in phase I of the trial (N = 92). Safety was assessed in patients who received SC dosing in phase I and II (cohort A) of the trial (N = 217), with a data cutoff of March 16, 2022.
2.3 Population PK Model Development
The population PK base model was selected following comparisons among several structural models, including 1- and 2-compartment linear models, 1- and 2-compartment models with parallel linear and Michaelis-Menten elimination pathways, a 2-compartment model with a parallel linear and Michaelis-Menten elimination pathway as well as with maximum capacity of the saturable clearance changes over time, and a 2-compartment model with time-dependent and time-independent clearance components.
Covariate relationships were identified using generalized additive modeling [18] on base model parameters, which were then tested using a stepwise covariate model. The statistical criteria were p < 0.05 for the forward inclusion step and p < 0.001 for the backward elimination step. The covariates assessed in the population PK analysis included demographic characteristics (body weight, age, sex, race, region, and ethnicity [Hispanic vs non-Hispanic; Asian vs non-Asian]), disease characteristics and biomarkers (baseline total T cells, baseline soluble BCMA [sBCMA] and sBCMA over time, baseline bone marrow percentage of plasma cells, baseline plasmacytoma, baseline type of myeloma, baseline lesion number, baseline lytic lesion[s], baseline ECOG status, baseline International Staging System [ISS] staging, baseline revised ISS staging, and cytogenetic risk), clinical characteristics (baseline creatinine clearance, baseline albumin, baseline alanine aminotransferase, baseline alkaline phosphatase, renal function, and hepatic function), prior treatment and refractory status (prior use of anti-CD38 antibodies, daratumumab, anti–programmed cell-death protein 1 [PD-1]/anti–programmed cell death-ligand 1 antibodies, anti-BCMA treatment, triple- and penta-refractory status, the number of prior lines of therapy [≤ 3 vs > 3]), and antibodies to teclistamab status. Body weight was included in the structural model as covariates on the clearance and volume of distribution parameters because body weight has been proven to be a significant covariate on clearance and volume for most IgG-based monoclonal antibodies [19,20,21].
Model selection was determined by graphical evaluation, assessment of statistically significant differences in the objective function value (OFV) between competing models (nominal p < 0.001, showing a change in OFV of < 10.83 with 1 degree of freedom under a chi-square distribution [22]), and the stability of the models based on model convergence and condition number. The performance of the final PK model was further evaluated using prediction-corrected visual predictive check (n = 1000 replicates) [23].
2.4 Exposure–Response Analysis
Individual exposure metrics were derived from the final population PK model using individual empirical Bayesian PK parameter estimates to support exposure–response analyses for efficacy and safety. Predicted average concentration of the first treatment dose (Cave,1stdose) and predicted trough concentration after the first four weekly treatment doses (Ctrough,4doses) were used to characterize the exposure–response relationship for efficacy. The exposure metrics for exposure–response safety analyses were predicted maximum concentration following the first treatment dose (Cmax,1stdose) and predicted maximum concentration following the first four weekly treatment doses (Cmax,4doses).
The relationship between systemic teclistamab exposure and ORR was evaluated by graphical exploration and logistic regression. An exploratory bivariate logistic regression analysis was conducted to assess any possible association between systemic teclistamab exposure and ORR. The influence of prognostic factors such as baseline disease characteristics and significant covariates for teclistamab PK, as identified in the population PK covariate analysis, on ORR were further explored using multivariate logistic regression. The time-to-event endpoints, OS, DoR, and PFS, were evaluated by the Kaplan–Meier method, stratified by tertiles of predicted PK exposure metrics. For patients who received RP2D and non-RP2D SC in the phase I portion of the trial, the exposure–response relationships for ORR were also explored. The exposure–response relationships for safety were explored according to exposure quartiles for selected AEs of interest, which were grade ≥3 anemia, neutropenia, lymphopenia, leukopenia, thrombocytopenia, and infection rate.
2.5 Software
The population PK analysis was performed using NONMEM (version 7.3.0, ICON Development Solutions LLC, Ellicott City, MD, USA) [24] within the environment of Perl-speaks-NONMEM (version 4.6.0). The first-order conditional estimation with interaction was employed for all model runs. Data management, exploratory analyses, diagnostic graphics, postprocessing of the data and NONMEM outputs, and the exposure–response analysis were performed using R software version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria) [25].
3 Results
3.1 Population PK Modeling Analysis Results
The final dataset for population PK included a total of 4840 measurable serum teclistamab concentrations from 338 PK-evaluable patients with RRMM. This included 83 patients (1976 PK observations) who received teclistamab IV administration and 255 (2864 PK observations) who received SC administration. Among the patients who received SC administration, 28 (604 PK observations) received doses <RP2D, 203 (1679 PK observations) received RP2D, 21 (502 PK observations) received doses >RP2D, and three (79 PK observations) received flat dosing.
The baseline disease characteristics and demographics for continuous and categorical covariates are shown in Table 1. Patients had a median age of 64 years and a median body weight of 74.3 kg, and the majority were white (83.4%), had normal or mild renal impairment (75.2%), and had normal hepatic function (88.2%). The number of patients with anti-teclistamab antibodies was low (two patients).
3.2 Base PK Model
The final base PK model was a 2-compartment model with first-order absorption and parallel time-independent and time-dependent elimination pathways (Suppl Fig. 1, see ESM) [26, 27], with interindividual variability (IIV) introduced for time-independent clearance, volume of distribution of the central compartment, clearance associated with time-dependent clearance, and first-order absorption rate constant. Inclusion of IIV on intercompartmental clearance, first-order rate constant for time-dependent clearance decrease over time, or F was attempted, but models were either not convergent or had significant increase in OFV. An additive model in the log-scale can adequately describe residual variability.
Compared with the 1-compartment models tested or 1-compartment model with parallel linear and Michaelis–Menten elimination pathways, the 2-compartment linear model greatly reduced OFV (> 700) and improved goodness-of-fit (p < 0.00001), indicating an improved model fit with the 2-compartment versus 1-compartment model. Both the 2-compartment model with parallel linear and Michaelis–Menten eliminations and the model with parallel time-independent and time-dependent clearances further reduced the OFV (p < 0.00001) compared with the simple 2-compartment linear model. However, the decrease in OFV was greater for the model with time-dependent clearance than for the Michaelis–Menten model. In addition, 2-compartment models with parallel linear and Michaelis–Menten elimination pathways with time-varying maximum velocity of the saturable clearance process were also attempted, but this model resulted in increased OFV and unstable parameters estimation. Therefore, the 2-compartment model with parallel time-independent and time-dependent clearance pathways was selected as the final population PK base model.
3.3 Covariate Model
The covariate effects included in the final model were the effect of body weight on time-independent clearance, volume of distribution of the central compartment and volume of distribution of the peripheral compartment, the effects of ISS staging on time-independent clearance, and the effect of type of myeloma (IgG vs non-IgG) on time-independent clearance and clearance associated with time-dependent clearance.
3.4 Final PK Model
The final population PK parameter estimates along with estimates of the included covariate effects are summarized in Table 2. All model parameters were estimated well with relative standard errors no greater than 30%, except for intercompartmental clearance. The IIV of shrinkages of the structural PK parameters were low to moderate; thus, estimates of individual PK parameters were considered consistent with disposition characteristics for a BCMA-targeting bispecific antibody.
The typical population value of time-independent clearance and clearance associated with time-dependent clearance were 0.449 L/day and 0.547 L/day, respectively; the first-order rate constant for clearance associated with time-dependent clearance decrease over time was 0.0292 day−1. The median time-dependent clearance of teclistamab was approximately 43% of the total clearance at initial treatment and decreased rapidly thereafter to <10% after week 8. The typical values of intercompartmental clearance, volume of distribution of the central compartment, and volume of distribution of the peripheral compartment were 0.039 L/day, 4.13 L, and 1.34 L, respectively. The typical value of first-order absorption rate constant was approximately 0.133 day−1, and the typical value of the subcutaneous bioavailability was 71.8%.
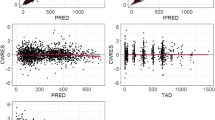
The evaluated performance of the final population PK model is shown in Suppl. Fig. 2 (see ESM). The final population PK model adequately captured the median serum concentration–time profile of teclistamab, as well as the associated variabilities. These results suggest that the final model described the observed data adequately.
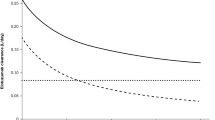
3.5 PK Simulations
The simulated concentration–time profiles following RP2D based on the final population PK model achieved 90% of steady-state exposure after 12 weekly treatment doses (Suppl. Fig. 3, see ESM). The mean accumulation ratio between the first and thirteenth weekly treatment dose of teclistamab 1.5 mg/kg was 4.2-fold for maximum concentration (Cmax), 4.1-fold for trough concentration (Ctrough), and 5.3-fold for area under the curve for the dosing interval. The median time to reach maximum concentration (Tmax) of teclistamab after the first and thirteenth treatment doses were 139 (range 19–168) and 72 (range 24–168) hours, respectively. Teclistamab clearance decreased over time, with a mean maximal reduction from baseline to the thirteenth treatment dose of 40.8% (coefficient of variation 56%). Patients who discontinue teclistamab after the thirteenth treatment dose are expected to have a 50% and 90% reduction from Cmax in teclistamab concentration at a median (5th to 95th percentile) time of 15 days (range 7–33) and 41 days (range 19–103), respectively, after Tmax, and a 97% reduction from Cmax in teclistamab concentration at a median time of 69 days (range 32–163) after Tmax.
The model-predicted individual average concentration of the first treatment dose (Cave,1stdose) was compared across different strata for covariates at the RP2D (Fig. 1). No clinically meaningful differences (< 20–25%) in the exposure to teclistamab were observed based on body weight for weight-based dosing. High-weight groups tended to have higher exposure, but the exposure range largely overlapped across body weight subgroups. The following disease status variables affected teclistamab exposure: multiple myeloma type (IgG vs non-IgG) and ISS stage (II vs I and III vs I). The simulated geometric mean Cave,1stdose was approximately 32% lower in patients with IgG multiple myeloma compared with those with non-IgG multiple myeloma, approximately 17% lower in patients with ISS stage II compared with those with ISS stage I, and approximately 29% lower in patients with ISS stage III compared with those with ISS stage I. Forest plots for predicted trough concentration after four weekly treatment doses (Ctrough,4doses) and predicted steady-state trough concentration were also generated (data not shown), and the results were similar to those from Cave,1stdose.
Forest plot of subgroup analyses of the predicted average concentration of the first treatment dose (Cave,1stdose) per the RP2D dose. Solid blue circle represents geometric mean ratio and error bar represents 95% CI. Dashed line represents reference value of 1. The associated values are shown on the right column. The dashed vertical lines refer to 0.8 and 1.25. Analyses assumed that all patients included in the population PK analysis data set received 1.5 mg/kg teclistamab SC administered weekly, with the first treatment dose preceded by step-up doses of 0.06 and 0.3 mg/kg. ECOG Eastern Cooperative Oncology Group, IgG immunoglobulin G, ISS International Staging System, PK pharmacokinetic, RP2D recommended phase II dose (1.5 mg/kg teclistamab SC administered weekly, with the first treatment dose preceded by step-up doses of 0.06 and 0.3 mg/kg), SC subcutaneous
3.6 Exposure–Response Efficacy
For 0.08–6 mg/kg SC doses in phase I, a positive exposure–response relationship was observed for ORR as responses at the concentration range associated with RP2D approached a plateau (Fig. 2), supporting the selection of the RP2D dose. Teclistamab exposure in responders (n = 61) and nonresponders (n = 31) overlapped when assessed by either Cave,1stdose or Ctrough,4doses.
Exposure–response relationship of the overall response in the phase I SC patients (phase I ORR; RP2D and non-RP2D) versus the predicted Cave,1stdose and Ctrough,4doses. Top panel: error bars are the 95% CI of ORR in the respective exposure tertile groups. Shaded areas of the logistic regression plots represent the 95% CI of the predicted ORR. Short vertical lines at the lower and upper part of the plotting area represent the exposure metrics in nonresponders and responders, respectively. Cave,1stdose average concentration during the first treatment dose, CI confidence interval, Ctrough,4doses trough concentration after the first four weekly treatment doses (i.e., predose concentration of the fifth weekly treatment dose), ORR overall response rate, RP2D recommended phase II dose (which is 1.5 mg/kg teclistamab SC administered weekly, with the first treatment dose preceded by step-up doses of 0.06 and 0.3 mg/kg), SC subcutaneous
The exposure–response relationship for ORR in patients who were administered teclistamab at the RP2D is shown in Fig. 3. A near flat exposure–response relationship was observed between ORR achieved at the RP2D and teclistamab exposure. Responders and nonresponders had a comparable and overlapping exposure range. The clinical subgroup analysis of ORR demonstrated that the clinical benefit of teclistamab was largely consistent in patients treated with the RP2D across subgroups (Fig. 4). Results from the logistic univariate regression analysis showed that the association between teclistamab exposure and the ORR achieved at the RP2D was not statistically significant for Cave,1stdose and Ctrough,4doses. Results from the multivariate regression analysis indicated that the factors that were significantly associated with the ORR were baseline sBCMA (per ng/mL) (OR 0.99; 95% CI 0.99–0.995; p < 0.001) and frequency of PD-1 expression on CD3+ T cells (OR 0.96; 95% CI 0.93–0.99; p = 0.0094).
Exposure–response relationship of the overall response in the patients who received the RP2D versus the predicted Cave,1stdose and Ctrough,4doses. Top panel: error bars are the 95% CI of ORR in the respective exposure tertile groups. Shaded areas of the logistic regression plots represent the 95% CI of the predicted ORR. Short vertical lines at the lower and upper part of the plotting area represent the exposure metrics in nonresponders and responders, respectively. Bottom panel: black dots are the individual exposure metrics predicted based on actual dosing and individual population PK model parameter estimates. Cave,1stdose average concentration during the first treatment dose, CI confidence interval, Ctrough,4doses trough concentration after the first 4 weekly treatment doses, ORR overall response rate, PK pharmacokinetic, RP2D recommended phase II dose (which is 1.5 mg/kg teclistamab SC administered weekly, with the first treatment dose preceded by step-up doses of 0.06 and 0.3 mg/kg), SC subcutaneous
Subgroup analysis of RP2D ORR based on baseline characteristics. Solid blue circle represents geometric mean ratio, and error bar represents 95% CI. The dashed vertical line shows the overall RP2D ORR of 62%. BCMA B-cell maturation antigen, CD cluster of differentiation, CI confidence interval, IgG immunoglobulin G, ISS International Staging System, ORR overall response rate, PD-1 programmed cell death protein 1, RP2D recommended phase II dose (which is 1.5 mg/kg teclistamab SC administered weekly, with the first treatment dose preceded by step-up doses of 0.06 and 0.3 mg/kg), SC subcutaneous
At the RP2D, no apparent relationship was observed between teclistamab exposure and DoR, PFS, and OS (Fig. 5). The p-value for OS versus tertile groups of Ctrough,4doses (p = 0.018) should be interpreted with caution given that the upper 95% CI of the median OS was not estimable due to data still maturing. Due to the overlapping Kaplan–Meier curves, no definitive exposure–response relationship in patients who received teclistamab SC across all dosing levels in phases I and II was found; these results were similar for DoR, PFS, and OS for patients who received teclistamab SC across all dosing levels (Suppl. Fig. 4, see ESM).
DoR, PFS, and OS stratified by predicted Cave,1stdose and Ctrough,4doses tertiles for RP2D. Numbers below the plots represent the number of patients at risk at each time point. Cave,1stdose average concentration during the first treatment dose, Ctrough,4doses trough concentration after the first four weekly treatment doses (i.e., predose concentration of the fifth weekly treatment dose), DoR duration of response, OS overall survival, PFS progression-free survival, RP2D recommended phase II dose (which is 1.5 mg/kg teclistamab SC administered weekly, with the first treatment dose preceded by step-up doses of 0.06 and 0.3 mg/kg), SC subcutaneous, T1 lowest exposure tertile group, T2 middle exposure tertile group, T3 highest exposure tertile group
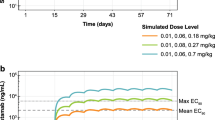
3.7 Exposure–Response Safety
In total, 217 patients received SC doses and were included for the exposure–safety analyses (28 patients received <RP2D, 160 received the RP2D, 21 received >RP2D, and three received flat dosing). No apparent relationship was observed in the incidence of grade ≥3 anemia, neutropenia, lymphopenia, leukopenia, thrombocytopenia, or infections across the predicted exposure quartiles (Fig. 6). However, a decreasing trend in the incidence of anemia was observed, with a highest rate observed in the lowest quartile group.
Comparison of AE occurrence rates by the predicted Cmax,1stdose and Cmax,4doses quartiles. Error bars are the 95% CI of AE occurrence rates in the respective exposure quartile groups. AE adverse event, CI confidence interval, Cmax,1stdose maximum concentration following the first treatment dose, Cmax,4doses maximum concentration following the first four weekly treatment doses, Gr grade, n number of patients
4 Discussion
In this report, we describe population PK and exposure–response analyses for teclistamab in patients with RRMM enrolled in the MajesTEC-1 study. Population PK and exposure–response analyses are commonly used to inform dose selection in drug development and support a product label. The results reported here were used to support the approval of teclistamab 1.5 mg/kg QW SC, with the first treatment dose preceded by step-up doses of 0.06 mg/kg and 0.3 mg/kg in patients with RRMM who have received prior treatment with an IMiD, a PI, and an anti-CD38 antibody [6, 9].
The observed teclistamab serum concentration–time data were adequately described by the 2-compartment model with first-order absorption and parallel time-independent and time-dependent elimination pathways. Combined population PK data, including half-life and exposure analyses, support the weekly dosing schedule for teclistamab at the RP2D of 1.5 mg/kg. The typical population values of time-independent clearance, clearance associated with time-dependent clearance, intercompartmental clearance, volume of distribution of the central compartment, and volume of distribution of the peripheral compartment in patients with a median weight of 74 kg were 0.449 L/day, 0.547 L/day, 0.039 L/day, 4.13 L, and 1.34 L, respectively. The rate constant for the clearance associated with time-dependent clearance decrease over time was 0.0292 day−1. The typical values of first-order absorption rate constant and SC bioavailability were 0.133 day−1 and 71.8%, respectively. Patients who discontinue teclistamab after the thirteenth treatment dose are expected to have a 50% reduction from Cmax in teclistamab concentration at a median (5th to 95th percentile) time of 15 days (7–33) after Tmax and a 97% reduction from Cmax in teclistamab concentration at a median time of 69 days (32–163) after Tmax. Of note, Cmax was approximately 4–5 times lower with SC dosing compared with IV dosing in this study [15]. Body weight, type of myeloma (IgG vs non-IgG), and ISS stage were statistically significant covariates on the teclistamab PK. ISS stage was a significant covariate on teclistamab PK while sBCMA was only a significant covariate in response analyses. This finding suggests that disease status may have a larger impact on teclistamab PK than target binding.
The immunogenicity analysis population in the MajesTEC-1 study comprised 321 patients who were anti-drug antibody (ADA)-evaluable with one or more post-dose ADA sample. Of the 321 patients, two (one receiving teclistamab IV and one receiving teclistamab SC) developed ADAs. These ADAs had a low titer of 20 and seemed to have no impact on safety. Both subject-level positive immune response and time-varying positive immune response were assessed in a sensitivity analysis using the final model, and there were no significant effects found on PK. In addition, the PK profile of patients with ADAs was within the range of observed PK profiles when compared with patients who did not develop ADAs. Based on available PK data, these ADAs did not seem to impact the PK of teclistamab.
Observed IgG concentrations are much higher in the IgG subtype compared with non-IgG subtypes of myeloma since the malignant cells of multiple myeloma patients can produce excessive amounts of monoclonal immunoglobulin, including IgG. The different IgG concentrations between IgG versus non-IgG subtypes could potentially contribute to the different catabolic rate observed for immunoglobulins (and teclistamab), belonging to the IgG category. Higher IgG concentrations are associated with higher elimination rate, where the excessive IgG saturates the neonatal Fc receptor (FcRn)-mediated recycling pathway of IgG and therefore leads to increased IgG (teclistamab) clearance and decreased exposures [28, 29]. This mechanistic explanation likely accounts for the difference in teclistamab concentrations between participants with non-IgG versus IgG subtypes of multiple myeloma. This aligns with findings reported for daratumumab [30,31,32].
Various base PK models, including quasi–steady-state target-mediated drug disposition (TMDD) models, were investigated to fit the teclistamab serum concentration–time data. Quasi–steady-state models improved the data fit for low teclistamab concentrations, which indicates the presence of TMDD (higher clearance at lower concentration) for teclistamab PK. However, while it addressed the bias in the low concentration values, the target concentration turnover may not be reliably estimated with only fitting the free drug concentration. The model also did not account for the contribution of target cell killing and effects of disease status on PK. Models relating time-dependent teclistamab clearance to time-varying sBCMA were also tested, as a rapid decrease in total sBCMA was observed in most responders within the first month of treatment in MajesTEC-1, and a greater reduction in sBCMA tended to occur in patients with deeper responses to teclistamab at the RP2D and in phase I dosing. Responders to teclistamab also showed a trend of sBCMA reduction over time. However, these models had significant increases in OFV. Soluble BCMA (baseline and time-variable) was not identified as an influencing covariate in a teclistamab population PK model. However, baseline sBCMA was identified as one of the prognostic factors that were significantly associated with ORR.
The model with time-dependent clearance was an approximation of TMDD equations [33], which includes a TMDD component, as well as a dynamic circular interaction between PK exposure and disease burden and ISS stage. The current model included PK effects on disease progression and a feedback loop from disease status to PK. The assumption for this approximation seems to hold given the antitumor activity of teclistamab, a BCMA × CD38 bispecific antibody. The mechanistic explanation for the decrease in monoclonal antibody clearance over the course of treatment may be associated with improvements in time-varying covariates related to disease severity and cancer-related cachexia, as shown with nivolumab [34, 35]. Inflammatory response related to cytokine release syndrome (CRS) is unlikely to affect teclistamab clearance since the cytokine release happened early in cycle 1 and was transient.
Step-up doses were used to mitigate the risk of severe CRS in the MajesTEC-1 study. The first step-up dose of 0.06 mg/kg was selected based on the observation of predominantly grade 1 CRS after this dose, with both grade 1 and 2 CRS observed at a dose of 0.08 mg/kg SC. CRS data across cohorts suggest that after the initial dose, subsequent step ups of up to six-fold are tolerable. The second step-up dose of 0.3 mg/kg was selected as a five-fold step up from 0.06 mg/kg, and the weekly dose of 1.5 mg/kg is a five-fold step up from this second dose. Although CRS was commonly reported in the study, these events were mainly low grade and clinically manageable [16]. Based on the results shown from this analysis, the RP2D of teclistamab, with the first dose preceded by step-up doses, is appropriate, with a near flat trend for ORR in patients who received the RP2D and no apparent relationship between exposure and the incidence of the assessed AEs.
Absolute lymphocyte count is unlikely to affect teclistamab clearance since the decline of lymphocytes happened early during step-up dosing and was transient. Ethnicity (Asian vs non-Asian) was assessed in a sensitivity analysis using the final PK model. The analysis did not find ethnicity to have a significant effect on teclistamab clearance.
Cave,1stdose, Ctrough,4doses, Cmax,1stdose and Cmax,4doses were used for exposure–response efficacy and safety analyses to maximize the number of patients included, avoiding potential bias caused by exclusion of nonresponders with early discontinuation, and to reduce the potential for confounding exposure–response relationships due to the time-varying clearance because of disease status improvement following treatment [36,37,38]. For phase I dosing of 0.08–6 mg/kg SC, a positive exposure–response relationship was observed for ORR, and the ORR approached a plateau at the concentration range associated with RP2D. Importantly, at the RP2D, responders and nonresponders had comparable and overlapping exposure ranges and DoR, PFS, and OS were not significantly correlated with teclistamab exposures. Taken together, these findings support the selection of teclistamab at 1.5 mg/kg SC administered weekly for the treatment of patients with RRMM.
The prognostic factors that were significantly associated with ORR in the multivariate analysis were baseline sBCMA and PD-1 expression, where patients with lower sBCMA or PD-1 expression tended to respond better than those with higher sBCMA or PD-1 expression. Other investigated factors did not significantly affect the ORR response, including body weight, type of multiple myeloma, and ISS stage. PD-1 is not a unique phenotypic marker for exhausted T cells and can also be expressed by activated T cells [39]. Therefore, additional characterization is needed to understand the phenotype of PD-1–expressing T cells at baseline. A rapid decrease in total sBCMA was observed in most responders within the first month of treatment, and a greater reduction in sBCMA tended to occur in patients with deeper responses to teclistamab at the RP2D and in phase I dosing [15, 16]. Responders to teclistamab also showed a trend of sBCMA reduction over time. It should be noted that sBCMA (baseline and time-variable) was not identified as an influencing covariate on teclistamab exposure in the population PK analysis. These results are consistent with recent findings from teclistamab and talquetamab monotherapy studies showing that sBCMA baseline level correlates with tumor burden and changes in sBCMA correlated with clinical activity in patients with RRMM [40, 41]. Patients with deep responses tended to have higher magnitudes of sBCMA reduction from baseline compared with patients with other responses or no response [40]. Moreover, it has been shown that high sBCMA levels are associated with disease characteristics, including baseline proportion of plasma cells in bone marrow, plasmacytoma, and ISS stage, suggesting that sBCMA could be a marker of disease burden. Change in sBCMA levels correlates well with drug response and disease progression, recommending it as a valuable marker for response in patients with multiple myeloma [40, 41].
No apparent exposure–response relationship was observed in the incidence of grade ≥ 3 anemia, neutropenia, lymphopenia, leukopenia, thrombocytopenia, and infections across the predicted exposure quartiles in patients who received teclistamab SC. The incidence of grade ≥ 3 anemia appeared to decrease with higher teclistamab exposure, which is likely due to confounding between ISS stage and exposure. Worse ISS stage tended to have higher incidences of grade ≥ 3 anemia and thrombocytopenia. However, worse ISS stage was associated with lower exposure in the population PK analysis. Another possible explanation was patients with treatment-emergent AEs tended to have dose interruptions or delays, which led to lower exposure in these patients. Overall, the exposure–response analyses on safety endpoints did not identify any safety concerns with the RP2D of teclistamab at 1.5 mg/kg SC QW.
The currently available data supports weight-based dosing for teclistamab. Body weight is a statistically significant covariate for teclistamab clearance and volume of distribution in the population PK model, that is, higher clearance and volume of distribution are associated with higher body weight. This aligns with the well-established impact of body weight on pharmacokinetics for monoclonal antibodies and bispecific antibodies as reported in previous studies [22, 30, 42]. Because teclistamab was administered using a weight-based dose in MajesTEC-1, no clinically meaningful differences (< 20–25%) in teclistamab exposure were observed in patients across different body weights. Further clinical efficacy subgroup analyses and ER analyses demonstrated that body weight had no clinically relevant effect on efficacy at the recommended dose regimen. Overall, the population PK and exposure–response analyses provided scientific support for body weight-based dosing for teclistamab in the current study.
In MajesTEC-1, patients who achieved and sustained a response were given the option to transition to a less frequent dosing schedule. Most patients who switched to less frequent dosing maintained deep responses. No new safety signals have emerged, and rates of new grade ≥ 3 infections decreased with time [43, 44]. This adjustment provided increased convenience and flexibility for patients, physicians, and caregivers.
The PK sample collection in MajesTEC-1 was intensive in phase I and sparse in phase II. Spare PK sampling was used to make PK assessments feasible and less burdensome for patients. Despite the PK sampling schedule, the teclistamab PK model characterized the exposure and change in clearance over time, corresponding well to the TMDD and disease burden. It should also be noted that PK metrics may be confounded by disease severity and treatment outcome; to mitigate against this, this study used both steady state and first dose exposure metrics for exposure–responses analyses, building confidence in these results.
5 Conclusion
Teclistamab population PK showed that body weight, myeloma type, and ISS stage may impact exposure; however, these factors did not have a clinically relevant effect on efficacy. sBCMA was not a significant covariate impacting teclistamab exposure. The exposure–response analyses for ORR showed a positive trend, with a plateau at the RP2D. There was no apparent exposure–response trend between teclistamab exposure and grade ≥3 hematologic and infection AEs. Overall, these analyses support the RP2D of teclistamab (1.5 mg/kg SC administered weekly, with the first treatment dose preceded by step-up doses of 0.06 mg/kg and 0.3 mg/kg) for the treatment of patients with RRMM.
References
Rajkumar SV. Multiple myeloma: 2020 update on diagnosis, risk-stratification and management. Am J Hematol. 2020;95(5):548–67.
Dimopoulos MA, Moreau P, Terpos E, et al. Multiple myeloma: EHA-ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Hemasphere. 2021;5(2):e528.
Mateos MV, Weisel K, De Stefano V, et al. LocoMMotion: a prospective, non-interventional, multinational study of real-life current standards of care in patients with relapsed and/or refractory multiple myeloma. Leukemia. 2022;36(5):1371–6.
EMA summary of product characteristics. Abecma (idecabtagene vicleucel). Vol. 2022.
EMA summary of product characteristics. CARVYKTI (ciltacabtagene autoleucel). Vol. 2022.
EMA summary of product characteristics. TECVAYLI (teclistamab). Vol. 2022.
US FDA. ABECMA® (idecabtagene vicleucel). Vol. 2022.
US FDA. CARVYKTI™ (ciltacabtagene autoleucel). Vol. 2022.
US FDA prescribing information. TECVAYLI™ (teclistamab). Vol. 2022.
Berdeja JG, Madduri D, Usmani SZ, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet. 2021;398(10297):314–24.
Munshi NC, Anderson LD Jr, Shah N, et al. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N Engl J Med. 2021;384(8):705–16.
Shah N, Chari A, Scott E, Mezzi K, Usmani SZ. B-cell maturation antigen (BCMA) in multiple myeloma: rationale for targeting and current therapeutic approaches. Leukemia. 2020;34(4):985–1005.
Lonial S, Lee HC, Badros A, et al. Belantamab mafodotin for relapsed or refractory multiple myeloma (DREAMM-2): a two-arm, randomised, open-label, phase 2 study. Lancet Oncol. 2020;21(2):207–21.
Pillarisetti K, Powers G, Luistro L, et al. Teclistamab is an active T cell-redirecting bispecific antibody against B-cell maturation antigen for multiple myeloma. Blood Adv. 2020;4(18):4538–49.
Usmani SZ, Garfall AL, van de Donk N, et al. Teclistamab, a B-cell maturation antigen × CD3 bispecific antibody, in patients with relapsed or refractory multiple myeloma (MajesTEC-1): a multicentre, open-label, single-arm, phase 1 study. Lancet. 2021;398(10301):665–74.
Moreau P, Garfall AL, van de Donk N, et al. Teclistamab in relapsed or refractory multiple myeloma. N Engl J Med. 2022;387(6):495–505.
Rajkumar SV, Harousseau JL, Durie B, et al. Consensus recommendations for the uniform reporting of clinical trials: report of the International Myeloma Workshop Consensus Panel 1. Blood. 2011;117(18):4691–5.
Mandema JW, Verotta D, Sheiner LB. Building population pharmacokinetic–pharmacodynamic models. I. Models for covariate effects. J Pharmacokinet Biopharm. 1992;20(5):511–28.
Chen Y, Xu Y. Pharmacokinetics of bispecific antibody. Curr Pharmacol Rep. 2017;3:126–37.
Keizer RJ, Huitema AD, Schellens JH, Beijnen JH. Clinical pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49(8):493–507.
Dirks NL, Meibohm B. Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49(10):633–59.
Xu Y, Hu C, Chen Y, et al. Population pharmacokinetics and exposure-response modeling analyses of ustekinumab in adults with moderately to severely active ulcerative colitis. J Clin Pharmacol. 2020;60(7):889–902.
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO. Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. Aaps J. 2011;13(2):143–51.
Beal SL, Boeckmann AJ, Bauer RJ. NONMEM 7.3.0 Users Guides. Vol. 2022. Ellicott City, MD: Icon Development Solutions; 1989-2015.
The R Project for Statistical Computing. Vol. 2022.
Gibiansky E, Gibiansky L, Carlile DJ, Jamois C, Buchheit V, Frey N. Population pharmacokinetics of obinutuzumab (GA101) in chronic lymphocytic leukemia (CLL) and non-Hodgkin’s lymphoma and exposure-response in CLL. CPT Pharmacometr Syst Pharmacol. 2014;3(10):e144.
Garrett M, Ruiz-Garcia A, Parivar K, Hee B, Boni J. Population pharmacokinetics of inotuzumab ozogamicin in relapsed/refractory acute lymphoblastic leukemia and non-Hodgkin lymphoma. J Pharmacokinet Pharmacodyn. 2019;46(3):211–22.
Jacobs JFM, Mould DR. The role of FcRn in the pharmacokinetics of biologics in patients with multiple myeloma. Clin Pharmacol Ther. 2017;102(6):903–4.
Pyzik M, Rath T, Lencer WI, Baker K, Blumberg RS. FcRn: the architect behind the immune and nonimmune functions of IgG and albumin. J Immunol. 2015;194(10):4595–603.
Yan X, Clemens PL, Puchalski T, et al. Target-mediated drug disposition of daratumumab following intravenous infusion in relapsed or refractory multiple myeloma after prior proteasome inhibitors and immunomodulatory drugs: a population pharmacokinetic analysis. Blood. 2015;126(23):4222.
Kim K, Phelps MA. Clinical pharmacokinetics and pharmacodynamics of daratumumab. Clin Pharmacokinet. 2023;62(6):789–806.
Xu XS, Schecter JM, Jansson R, Yan X. Response to “The role of FcRn in the pharmacokinetics of biologics in patients with multiple myeloma.” Clin Pharmacol Ther. 2017;102(6):905.
Gibiansky L, Gibiansky E. The relationship between target-mediated drug disposition (TMDD) and models with time-dependent clearance. Increasing drug development success: understanding drug-disease interactions through quantitative systems pharmacology. Vol. 2022: QuantPharm LLC; 2015.
Bajaj G, Wang X, Agrawal S, Gupta M, Roy A, Feng Y. Model-based population pharmacokinetic analysis of nivolumab in patients with solid tumors. CPT Pharmacometr Syst Pharmacol. 2017;6(1):58–66.
Zhang J, Sanghavi K, Shen J, et al. Population pharmacokinetics of nivolumab in combination with ipilimumab in patients with advanced malignancies. CPT Pharmacometr Syst Pharmacol. 2019;8(12):962–70.
Dai HI, Vugmeyster Y, Mangal N. Characterizing exposure-response relationship for therapeutic monoclonal antibodies in immuno-oncology and beyond: challenges, perspectives, and prospects. Clin Pharmacol Ther. 2020;108(6):1156–70.
Kawakatsu S, Bruno R, Kågedal M, et al. Confounding factors in exposure-response analyses and mitigation strategies for monoclonal antibodies in oncology. Br J Clin Pharmacol. 2021;87(6):2493–501.
Liu C, Yu J, Li H, et al. Association of time-varying clearance of nivolumab with disease dynamics and its implications on exposure response analysis. Clin Pharmacol Ther. 2017;101(5):657–66.
Pauken KE, Wherry EJ. Overcoming T cell exhaustion in infection and cancer. Trends Immunol. 2015;36(4):265–76.
Girgis S, Wang Lin SX, Pillarisetti K, et al. Teclistamab and talquetamab modulate levels of soluble B-cell maturation antigen in patients with relapsed and/or refractory multiple myeloma. J Clin Oncol. 2021;39(15_Suppl):8047–8047.
Girgis S, Wang Lin SX, Pillarisetti K, et al. Effects of teclistamab and talquetamab on soluble BCMA levels in patients with relapsed/refractory multiple myeloma. Blood Adv. 2023;7(4):644–8.
Chen Y, Miao X, Hsu CH, et al. Population pharmacokinetics and exposure-response modeling analyses of guselkumab in patients with psoriatic arthritis. Clin Transl Sci. 2022;15(3):749–60.
Usmani SZ, Karlin L, Benboubker L, et al. Durability of responses with biweekly dosing of teclistamab in patients with relapsed/refractory multiple myeloma achieving a clinical response in the MajesTEC-1 study. J Clin Oncol. 2023;41(16 suppl):8034.
van de Donk NWCJ, Moreau P, Garfall AL, et al. Long-term follow-up from MajesTEC-1 of teclistamab, a B-cell maturation antigen (BCMA) × CD3 bispecific antibody, in patients with relapsed/refractory multiple myeloma (RRMM). J Clin Oncol. 2023;41(16 suppl):8011.
Acknowledgements
The authors thank Sheri Skerget, PhD, and Deeksha Vishwamitra, PhD, of Janssen for their input on biomarkers. Medical writing support was provided by Craig Turner, MSc, of Eloquent Scientific Solutions, and was funded by Janssen Global Services, LLC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Janssen Research & Development, LLC.
Conflicts of Interest
Xin Miao, Liviawati S. Wu, Yuki Iwaki, Rachel Kobos, Tara Stephenson, Kristy Kemmerer, Clarissa M. Uhlar, Arnob Banerjee, Danielle Trancucci, Amit Apte, Raluca Verona, Lixia Pei, Rachit Desai, Kathleen Hickey, Yaming Su, Daniele Ouellet, Mahesh Samtani, and Yue Guo are employees of Janssen. Shun Xin Wang Lin is an employee of LinkiDose Medicine Co., Ltd. Yan Xu is an employee of Simcere Pharmaceuticals. Yang Chen is an employee of Daiichi Sankyo. Jenna D. Goldberg is an employee of Vividon and holds stock in Janssen. Alfred L. Garfall is a consultant for Janssen, GSK, and Amgen; has received research funding from Janssen, Novartis, Tmunity, and CRISPR Therapeutics; and is an independent data monitoring committee member for Janssen. Amrita Krishnan is a consultant for Adaptive, Janssen, Sanofi, BMS, Pfizer, and Regneron; is a current equity holder in BMS; has received research funding from Janssen; is a Speakers’ Bureau member for Takeda, GSK, and BMS; and is a member of the Board of Directors or advisory committee for Sutro. Saad Z. Usmani has served in a consulting or advisory role for Celgene, Amgen, Janssen, Takeda, GlaxoSmithKline, Karyopharm Therapeutics, AbbVie, Merck, Genentech, Gilead Sciences, and Bristol-Myers Squibb/Celgene; and has received research funding from Celgene, Array BioPharma, Janssen, Pharmacyclics, Sanofi, Bristol-Myers Squibb, Amgen, Seattle Genetics, Merck, Skyline Diagnostics, and GlaxoSmithKline. Honghui Zhou is an employee of Jazz Pharmaceuticals and owns stocks in Jazz Pharmaceuticals and Johnson & Johnson. Suzette Girgis is an employee of Jazz Pharmaceuticals and holds stocks in JNJ and BMS.
Availability of data and material
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. Although these data are not currently publicly available for sharing, requests for sharing can be sent to the Corresponding Author and will be evaluated on an individual basis.
Ethics Approval
Each study site’s local independent ethics committee or institutional review board approved the study protocol. The study was conducted in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice guidelines. All patients provided written informed consent.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Miao, X., Wu, L.S., Lin, S.X.W. et al. Population Pharmacokinetics and Exposure–Response with Teclistamab in Patients With Relapsed/Refractory Multiple Myeloma: Results From MajesTEC-1. Targ Oncol 18, 667–684 (2023). https://doi.org/10.1007/s11523-023-00989-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-023-00989-z