Abstract
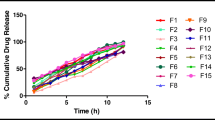
Nifedipine is a BCS Class II drug used for treatment of hypertension and preterm labor. Large inter-patient variability in nifedipine absorption results in variable exposure among different patients. We conducted in vitro dissolution studies to compare nifedipine dissolution from immediate release (IR) capsules with different volumes of dissolution media. Results from dissolution studies were used to design a crossover study in healthy volunteers to evaluate the effect of coadministered water volume with nifedipine 10 mg IR capsules on nifedipine pharmacokinetics, especially absorption (C max, t max, and AUC0-6). Dissolution studies demonstrated that larger gastric fluid volumes result in enhanced nifedipine dissolution from 10 mg IR cosolvent capsules (73 vs. 17% in 200 and 100 mL simulated gastric fluid, respectively, at 30 min). The pharmacokinetic crossover study in healthy volunteers (N = 6) did not show a significant effect of the water volume administered with the capsule (50 vs. 250 mL) on C max, t max, or AUC0-6 of orally administered nifedipine IR capsules (10 mg). However, administration of large water volumes resulted in lower variability in nifedipine C max (47 vs. 70% for 250 and 50 mL, respectively). Administration of large water volumes with nifedipine 10 mg IR cosolvent capsules may reduce inter-individual variability in plasma exposure. Evaluation of similar effects in other BCS Class II drugs is recommended.




Similar content being viewed by others
References
Wu C-Y, Benet LZ. Predicting drug disposition via application of BCS: transport/absorption/ elimination interplay and development of a biopharmaceutics drug disposition classification system. Pharm Res. 2005;22(1):11–23.
Guazzi M, Olivari MT, Polese A, Fiorentini C, Magrini F, Moruzzi P. Nifedipine, a new antihypertensive with rapid action. Clin Pharmacol Ther. 1977;22(5 Pt 1):528–32.
Fox NS, Gelber SE, Kalish RB, Chasen ST. Contemporary practice patterns and beliefs regarding tocolysis among u.s. Maternal-fetal medicine specialists. Obstet Gynecol. 2008;112(1):42–7.
ACOG. Practice Bulletin No. 159: Management of Preterm Labor. Obstet Gynecol. 2016;127(1):e29–38.
Vogel JP, Oladapo OT, Manu A, Gulmezoglu AM, Bahl R. New WHO recommendations to improve the outcomes of preterm birth. Lancet Glob Health. 2015;3(10):e589–90.
Nassar AH, Aoun J, Usta IM. Calcium channel blockers for the management of preterm birth: a review. Am J Perinatol. 2011;28(1):57–66.
Haas DM, Caldwell DM, Kirkpatrick P, McIntosh JJ, Welton NJ. Tocolytic therapy for preterm delivery: systematic review and network meta-analysis. BMJ. 2012;345:e6226.
King JF, Flenady VJ, Papatsonis DN, Dekker GA, Carbonne B. Calcium channel blockers for inhibiting preterm labour. Cochrane Database Syst Rev. 2002;2:CD002255.
Patki KC, Von Moltke LL, Greenblatt DJ. In vitro metabolism of midazolam, triazolam, nifedipine, and testosterone by human liver microsomes and recombinant cytochromes p450: role of cyp3a4 and cyp3a5. Drug Metab Dispos. 2003;31(7):938–44.
Kleinbloesem CH, van Harten J, Wilson JP, Danhof M, van Brummelen P, Breimer DD. Nifedipine: kinetics and hemodynamic effects in patients with liver cirrhosis after intravenous and oral administration. Clin Pharmacol Ther. 1986;40(1):21–8.
Raemsch KD, Sommer J. Pharmacokinetics and metabolism of nifedipine. Hypertension. 1983;5(4 Pt 2):II18–24.
Toal CB. Formulation dependent pharmacokinetics—does the dosage form matter for nifedipine? J Cardiovasc Pharmacol. 2004;44(1):82–6.
Haas DM, Quinney SK, Clay JM, Renbarger JL, Hebert MF, Clark S, et al. Nifedipine pharmacokinetics are influenced by CYP3A5 genotype when used as a preterm labor tocolytic. Am J Perinatol. 2013;30(4):275–81.
Thelen K, Jantratid E, Dressman JB, Lippert J, Willmann S. Analysis of nifedipine absorption from soft gelatin capsules using PBPK modeling and biorelevant dissolution testing. J Pharm Sci. 2010;99(6):2899–904.
Jantratid E, Janssen N, Reppas C, Dressman JB. Dissolution media simulating conditions in the proximal human gastrointestinal tract: an update. Pharm Res. 2008;25(7):1663–76.
Vertzoni M, Dressman J, Butler J, Hempenstall J, Reppas C. Simulation of fasting gastric conditions and its importance for the in vivo dissolution of lipophilic compounds. Eur J Pharm Biopharm. 2005;60(3):413–7.
Vertzoni M, Pastelli E, Psachoulias D, Kalantzi L, Reppas C. Estimation of intragastric solubility of drugs: in what medium? Pharm Res. 2007;24(5):909–17.
Klein S, Shah VP. A standardized mini paddle apparatus as an alternative to the standard paddle. AAPS PharmSciTech. 2008;9(4):1179–84.
Haas DM, Quinney SK, Clay JM, Renbarger JL, Hebert MF, Clark S, et al. Nifedipine pharmacokinetics are influenced by CYP3A5 genotype when used as a preterm labor tocolytic. Am J Perinatol. 2012;8:8.
Zhang Y, Huo M, Zhou J, Xie S. PKSolver: an add-in program for pharmacokinetic and pharmacodynamic data analysis in Microsoft Excel. Comput Methods Programs Biomed. 2010;99(3):306–14.
Yu KS, Cho JY, Shon JH, Bae KS, Yi SY, Lim HS, et al. Ethnic differences and relationships in the oral pharmacokinetics of nifedipine and erythromycin. Clin Pharmacol Ther. 2001;70(3):228–36.
ACOG. ACOG practice bulletin no. 127: management of preterm labor. Obstet Gynecol. 2012;119(6):1308–17.
Schiller C, Frohlich CP, Giessmann T, Siegmund W, Monnikes H, Hosten N, et al. Intestinal fluid volumes and transit of dosage forms as assessed by magnetic resonance imaging. Aliment Pharmacol Ther. 2005;22(10):971–9.
Barton JR, Prevost RR, Wilson DA, Whybrew WD, Sibai BM. Nifedipine pharmacokinetics and pharmacodynamics during the immediate postpartum period in patients with preeclampsia. Am J Obstet Gynecol. 1991;165(4 Pt 1):951–4.
Welling PG, Huang H, Hewitt PF, Lyons LL. Bioavailability of erythromycin stearate: influence of food and fluid volume. J Pharm Sci. 1978;67(6):764–6.
Bustrack JA, Katz JD, Hull JH, Foster JR, Hammond JE, Christenson RH. Bioavailability of digoxin capsules and tablets: effect of coadministered fluid volume. J Pharm Sci. 1984;73(10):1397–400.
Beveridge T, Nüesch E, Ohnhaus EE. Absolute bioavailability of digoxin tablets. Arzneimittelforschung. 1978;28(4):701–3.
Mather LE, Austin KL, Philpot CR, McDonald PJ. Absorption and bioavailability of oral erythromycin. Br J Clin Pharmacol. 1981;12(2):131–40.
Acknowledgments
This study was supported, in part, by the Indiana Clinical and Translational Sciences Institute funded, in part by Grant # UL1TR001108 from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award. SKQ is supported by 1K23HD071134 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
We thank Indiana Clinical Research Center nursing staff for their efforts in coordinating the conduct of the clinical study, Janelle Owens for her efforts with chromatographic analysis of nifedipine dissolution samples, and the Clinical Pharmacology Analytical Core Laboratory at Indiana University for analysis of clinical samples.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Nader, A.M., Quinney, S.K., Fadda, H.M. et al. Effect of Gastric Fluid Volume on the In Vitro Dissolution and In Vivo Absorption of BCS Class II Drugs: a Case Study with Nifedipine. AAPS J 18, 981–988 (2016). https://doi.org/10.1208/s12248-016-9918-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-016-9918-x