Abstract
Background
Musculoskeletal disorders are common problems that affect the elderly. They severely restrict mobility and dexterity, resulting in early retirement from work, lower levels of well-being, and reduced ability to participate in society. With the increase in life expectancy, the older populations are dreaming of active, painless, and independent lives in the face of functional limitations that are the result of various comorbidities with age progression.
Main text
The aim of the study is to highlight aging changes in the musculoskeletal system, risk factors that may have a negative impact on musculoskeletal, as well as strategies to optimize musculoskeletal health in the elderly. A narrative review was conducted through a series of literature searches in the database MEDLINE/PubMed focusing on musculoskeletal health. The search terms used were “muscle building,” “bone building,” “osteoporosis,” “osteopenia,” “sarcopenia,” “osteosarcopenia,” “fractures,” “falls,” “functional ability,” “nutrition,” “diet,” “obesity,” “comorbidity,” and “medication.” Data extraction was carried out by the investigators using a standardized data collection form with subsequent discussion among the authors. Peer-reviewed observational controlled and non-controlled studies (case–control and cohort studies) were selected. The data collected in the selected articles were all related to musculoskeletal health.
Conclusion
Many of the changes in the musculoskeletal system result more from disuse than from simple aging. Less than 10% of the Egyptian population participate in regular exercise, and the most sedentary group is older than 50 years of age. Long-term regular exercises may reduce the loss of bone and muscle mass and prevent age-associated increases in body fat.
Similar content being viewed by others
Background
Throughout the people’s life course, healthy bones, joints, and muscles are the best components of the human body capable of keeping the person’s functional abilities at their optimum level. Over the past decade, there has been a significant change in the perception of aging at the scientific and social levels [1]. People increasingly started to look forward to living active, pain-free, and independent lives in their older years. For some people, this may involve continuing to work, whereas for the majority, this entails enjoying an active retirement, without feeling afraid of pain and falls. Consequently, there has been an adjustment to the retirement concept and a change in the traditional description of retirement as “more sitting and less moving.” Living longer has several benefits to both the economy and society which incorporates a wide range of financial, social, and cultural aspects. This is based on the skills, knowledge, and experience of the older adults which can reflect positively on their own psychology and benefit the broader population. Therefore, there is a high chance to employ this raised longevity as a resource.
Healthy aging was identified by the World Health Organization (WHO) in their update on the Decade of Healthy Ageing (2020–2030) as “the process of developing and maintaining the functional ability that enables wellbeing in older age” [2]. This concept is open for each person anywhere in the world. “Being free of disease or infirmity is not a requirement for healthy aging, as many older adults have one or more health conditions that, when well controlled, have little influence on their wellbeing” [3]. This coincided with the calls for transforming the impression about musculoskeletal conditions and how they are managed. In the meantime, it paved the way for the new concept of early diagnosis and management to replace the policy of treating older adults when they are at their most severe stages. Therefore, prevention, early detection, and management can enable people to live in good health and remain independent and connected to one’s community.
Though musculoskeletal conditions can affect people across the life course, their incidence gets higher among older adults [4]. There are multiple risk factors that can intensify people’s susceptibility to musculoskeletal disorders. These include getting obese or overweight, physical inactivity, nutritional deficiency particularly in vitamin D or calcium, smoking, comorbidities, medications, and genetic predisposition. Fractures, which are often a consequence of a fall, are one of the major musculoskeletal problems reported in the older population. Unfortunately, there is a low level of awareness of the link between healthy lifestyles and musculoskeletal health. This represents a gap in the people education as well as the management strategies adopted by health care professionals. There is also a real need to challenge the misconceptions that nothing can be done about getting older. This review aims to highlight the value of prioritizing musculoskeletal health and approaches to build bones as well as muscles particularly in older adults.
Main text
Method: search strategy
A narrative review was conducted through a series of literature searches in the database MEDLINE/PubMed for English language articles focusing on musculoskeletal health. The search strategy included a combination of medical subject headings and keywords. The search terms used were “muscle building,” “bone building,” “osteoporosis,” “osteopenia,” “sarcopenia”, “osteosarcopenia,” “fractures,” “falls,” “functional ability,” “nutrition,” “diet,” “obesity,” “comorbidity,” and “medication.” Sources published within the last 7 years were given preference. The investigators extracted data using a standardized data collection form, followed by a discussion among the authors. The studies were peer-reviewed observational controlled and non-controlled (case–control and cohort studies). All of the studies were conducted at a referral center, hospital, or in the community. The information gathered in the selected articles was all about musculoskeletal health. Case reports and articles that did not assess people’s muscle and bone health were excluded.
National data available to paint a picture of aging in Egypt
The Egyptian population is growingly aging. The percent of older people “defined as 60 years of age and more” was 6.1% of the total population according to the Egyptian census in 1996. It was postulated that the expected percentage of older people may reach 7.2% in 2006, 8.9% in 2016, and expected to reach 10.9% in 2026. According to the latest WHO data published in 2020 [2], life expectancy in Egypt is 69.6 years in males and 74.1 years in females with a total life expectancy of 71.8 years which gives Egypt a World Life Expectancy ranking of 112 [5], whereas, according to official data from the Central Agency for Public Mobilisation and Statistics (CAPMAS), Egypt’s life expectancy increased from 73.9 years in 2019 to 74.3 years in 2021 (73.4 years for males and 75.9 years for females) [6]. Egypt has approximately 141,000 hospital beds, 93,000 of which (66%) are affiliated with the Ministry of Health and Population. Of these, the total number of beds for older adults is 3856 (4.1%). Health services are distributed all over the country. In each governorate (province), there are three levels of health care, primary, secondary, and tertiary, but the geriatric specialty is presented mostly in Cairo and a few large cities [7]. A pilot project [8] is currently being implemented by the Egyptian Academy of Bone Health in collaboration with the Egyptian Food Bank and Hayat Karima in four governorates to renovate and build geriatric bone health care centers. It includes the provision of medical treatment, dietary supply rich in calcium and vitamin D, appropriate therapeutic exercises, and patients’ education. The main objective of this project is the primary prevention of fragility fractures and early detection of geriatric musculoskeletal problems together with the development of an effective rehabilitation policy.
Targeted population
Though, for statistical purposes, “older person” is defined in Egypt as an individual aged 60 and over, considering the incidence of hip fractures in Egypt, which was found to be sharply increased starting from the age of 50 [9], to ensure positive outcomes, this article targets the Egyptian population in both the pre-elderly age group (50–60 years old) as well as older adults (60 years old and over).
Aging changes in the bones, muscles, and joints
As people get old, musculoskeletal tissues exhibit increased bone fragility, loss of cartilage resilience, decreased soft tissue elasticity, loss of muscular strength, and fat redistribution, all of which reduce the tissues’ ability to perform their normal functions [10]. The loss of mobility and physical independence caused by subsequent fractures can be especially devastating in this population, not only physically and psychologically but also in terms of higher mortality rates [11].
Bones
The aging process causes bone structure and function to deteriorate, predisposing to osteoporosis and fragility fractures. At the bone surface, age-related bone loss is caused by two opposing processes: subperiosteal apposition, which occurs on the outside of the bone, and endosteal bone resorption, which occurs on the inside of the bone. The overall effects of this imbalance are cortical thinning, increased cortical porosity, trabecular thinning, and loss of trabecular connectivity, all of which reduce bone quality and bone strength [12].
Muscles
Bone and muscle tissues influence each other, which was recently described as bone-muscle crosstalk. They are also known to secrete osteokines, myokines, and cytokines into the circulation that influence the biological and pathological activities in local and distant organs and cells, giving rise to the term “osteosarcopenia.” Muscle mass, strength, and physical function decline with age, as do bones [13]. This has been linked to deterioration in muscle composition, with myosteatosis occurring independently of body weight changes. Furthermore, several mitochondrial processes in the skeletal muscle are impaired, including mitochondrial synthesis and breakdown, as well as mitochondrial bioenergetics. Muscle weakness and wasting have been linked to impaired mitochondrial function. Reduced mitochondrial bioenergetic capacity in the muscle was found to be the main factor distinguishing the presence of sarcopenia in older adults in a genome-wide transcriptional profiling study [14, 15]. Muscle weakness has been identified as an independent risk factor for high mortality in older adults [16,17,18].
Joints
In concordance with the changes in the bones and muscles with age, joint motion becomes more restricted and flexibility decreases. This has been attributed to changes in tendons and ligaments. Furthermore, as the cushioning cartilage begins to break down from a lifetime of use, the joints become inflamed and arthritic [19].
Risk factors of age-related musculoskeletal dysfunction
Aging, in addition to different combinations of intrinsic and extrinsic risk factors, accelerates the decline in bone and muscle mass making those people more susceptible to musculoskeletal disorders. These include getting obese or overweight, physical inactivity, nutritional deficiency particularly in vitamin D or calcium, smoking, comorbidities, medications, and genetic predisposition [20, 21]. This section will discuss the most common and important risk factors.
Obesity and musculoskeletal health
Obesity is a common condition known for its negative impact on the person’s health with increased morbidity and mortality. The very first link between obesity and bone was the common belief that an individual with obesity has stronger bones [22]. Despite this common misconception, studies have revealed a surprising bidirectional relationship between excess fat and bone. Obesity increases the risk of osteoporosis [23] and bone fractures [24], despite the fact that extra weight builds bone and extra fat padding protects the bone during a fall. This emphasizes the existence of osteosarcopenic obesity, a condition that links obesity and osteoporosis to muscle weakness [25]. Although excessive weight pressure may strengthen the bone [26], it appears that obesity causes poor bone quality. Several mechanisms have been proposed to explain the negative effects of obesity on both health and fitness, including the low-grade inflammatory state associated with obesity [27, 28], replacement of osteoblasts by fat cells in bone marrow [29,30,31], and fat mass and obesity (FTO-associated gene mutation associated with obesity and poor bone health) [32, 33].
Body fat increases with age, and weight is mostly gained as fat rather than lean mass [34]. This age-related decrease in lean muscle mass is caused by lower resting metabolic rates [35], low physical activity [36], decreased mitochondrial volume [37, 38], and decreased oxidative capacity. Sarcopenia exacerbates the negative effects of obesity in older people, resulting in sarcopenic obesity. Sarcopenic obesity is a clinical and functional condition marked by the coexistence of obesity (excess fat mass) and sarcopenia [39]. On the other hand, obesity can cause independent muscle mass and function loss due to the negative impact of adipose tissue-dependent metabolic derangements such as oxidative stress, inflammation, and insulin resistance, all of which have a negative impact on muscle mass [40]. As a result, obesity and sarcopenia may complement one another, resulting in a vicious cycle of fat gain and muscle loss due to decreased mobility, dependency, and disability [41]. Adipokines, such as leptin, resistin, adiponectin, and TNFα which are released from adipose tissues, were found to modulate bone turnover and bone mineral density (BMD) as well as skeletal muscle catabolism in aging [13].
Physical inactivity and musculoskeletal health
Low physical activity is a major risk factor for osteoporosis because it reduces the mechanical stimulation of osteoblasts. Although the mechanism underlying exercise’s effects on bone remodeling is not fully understood, some hypotheses seem more likely. Mechanical loadings, such as compression, strain, and fluid shear, are important stimuli for osteoblast differentiation and mineralization, as well as for maintaining proper bone mass and density [42]. Another effect is the vascular effect, which occurs when an increase in muscle activity causes a positive variation in bone blood flow, thereby improving local metabolism [43]. Exercise also regulates hormones in the body such as estrogen, parathyroid hormone, and glucocorticoids, which may be another important mechanism in bone metabolism and remodeling [44]. In particular, exercises that focus on antigravity loading have the most significant benefits. Also, the bone response to exercise is greater when more mechanical stress is exerted. Additionally, it appears that aerobic exercise is particularly effective in the enzymatic activation of the osteoblasts [45].
Low levels of physical activity in the elderly result in decreased mechanical loading of the muscles, which leads to reductions in skeletal muscle size and strength, exacerbating the normal declines associated with sarcopenia [46]. Indeed, a variety of factors, including insufficient energy intake and protein malnutrition, can influence the progression of sarcopenic muscle loss, with physical inactivity hastening the process. Sarcopenic decline raises the risk of subsequent hospitalization or disuse, which leads to further muscle loss [47]. Long periods of bed rest (35 or 90 days) were reported to cause a significant decrease in lower limb muscle force and power-generating capacity, supporting the quality changes at the contractile elements of muscle fibers [48].
Malnutrition and musculoskeletal health
Malnutrition in the elderly is frequently underdiagnosed and undertreated [49, 50]. According to a systematic review, the amount of food consumed by the elderly is 20% lower than that of young adults [51]. Malnutrition in the elderly can be caused by a variety of factors, some of which are complex and multifaceted. Poor appetite, poor dentition [52], loss of taste and smell, difficulty accessing and preparing food, and cognitive impairment [53] are among them. Micronutrient and macronutrient deficiencies appear to be strongly linked to the pathogenesis of bone loss in the elderly, as well as frailty. In a cross-sectional study of postmenopausal women, nutrients were found to be directly related to bone density in the total body, spine, and hip [54].
A growing body of evidence suggests that nutritional status may be a modifiable risk factor for muscle deterioration and the acceleration of sarcopenia. Malnutrition parameters were found to be related to both relative and absolute muscle mass in geriatric outpatients [55]. Physiological changes also play a role, as older patients may develop anabolic resistance, necessitating a higher protein intake [56, 57]. Furthermore, the skeletal muscle is prone to muscle protein dissociation in catabolic states, which frequently occur during malnutrition or acute illness [58, 59].
Bone minerals and musculoskeletal health
Calcium is an important structural element of the bone tissue. In conjunction with phosphate, it forms the mineral component of the bone, which is laid down within the collagen scaffold built by osteoblasts.
Calcium deficiency is common in the elderly population for a variety of reasons, including low calcium intake over time, medication interactions that may reduce dietary calcium absorption, and the underlying chronic disease osteoporosis, which alters bone formation and strength [60, 61].
The human skin produces vitamin D as a result of exposure to ultraviolet light. It needs to be hydroxylated at two sites before it becomes biologically active. Given that this is a crucial component of the regulation of circulating calcium levels, the activation of vitamin D is subject to precise homeostatic regulation. By enhancing calcium absorption in the upper small bowel and encouraging osteoclastic bone resorption, activated vitamin D helps to maintain serum calcium levels. Additionally, activated vitamin D promotes phosphate absorption in the gut.
As we get older, there is a reduction in the skin’s concentration of 7-dehydrocholesterol (the basic raw material for the synthesis of vitamin D) [62]. Specifically, for each decade past the age of 40, there is approximately a 10 to 15% decrease in the level of 7-dehydrocholesterol. Furthermore, there is limited exposure to sunlight due to the short time of outdoor activities. Furthermore, after the age of 70, there is a 35% decrease in intestinal calcium absorption [63]. This reduction is even greater in women due to decreased fractional calcium absorption and estrogen changes after menopause, which results in increased urinary calcium losses [64]. Other causes of age-related vitamin D deficiency include inadequate vitamin D and calcium intake. With age, polypharmacy and comorbidity must also be considered, with a particular emphasis on renal and liver insufficiency.
Contradictory results were found regarding the association between calcium and sarcopenia [65,66,67,68]. This might be because the study populations’ calcium intakes varied. Intake was higher in studies [67, 68] that did not discover an association than in studies [65, 66] that did discover an association between calcium and sarcopenia. According to recent research, muscle weakness in the elderly may be closely related to altered calcium homeostasis and decreased calcium absorption [69, 70].
Vitamin D is an important nutritional element that was linked to muscle health. One research has demonstrated that vitamin D deficiency is associated with increased oxidative stress and impaired mitochondrial function in skeletal muscles [71]. Additionally, a link between low vitamin D status and sarcopenia was also evident [72].
Low protein intake and musculoskeletal health
Protein intake is lower in older males (87 g/day) and females (69 g/day) than in their younger counterparts (97 g/day and 73 g/day, respectively), which raises concerns about inadequate protein intake in older adults [73]. This has been attributed to multimorbidity, tooth loss, changes in deglutition, appetite loss, and loss of functional independence [74]. Furthermore, increased disease-related tissue catabolism and inflammation can offset protein requirements [75].
Inadequate protein intake is detrimental to both bone mass acquisition during childhood and adolescence and bone mass preservation as we age. Poor nutritional status, particularly in terms of protein, is common in the elderly, and it appears to be worse in patients with hip fractures than in the general population [76]. In a prospective cohort study, elderly men and women who consumed less total and animal protein had higher rates of hip and spine bone loss than those who consumed more protein [77]. There is also evidence that increasing protein intake improves BMD in elderly men and women receiving calcium and vitamin D supplements, implying that these nutrients work synergistically to improve skeletal health [78].
Older adults may develop anabolic resistance, a reduced muscle protein synthesis rate response to protein intake [79]. Furthermore, prolonged disuse of the muscles and increased sedentary behavior could contribute to muscle atrophy among older adults [80]. If dietary intakes of protein remain below the recommended intake with greater protein needs during aging, over time, these could manifest as physical functional limitations [81].
Smoking, alcohol, and musculoskeletal health
According to a majority of the published studies, smoking had adverse effects on BMD across age categories and sex. Male smokers were found to have significantly lower BMD than nonsmokers [82, 83]. Additionally, cross-sectional study findings demonstrated that postmenopausal women who smoked had significantly lower BMD than postmenopausal women who did not smoke. An increased risk of falls was also reported in smokers regardless of the BMD T-score [84, 85]. Moreover, smoking was reported to increase the risk of fractures in the elderly population [86, 87]. Compared to bones, few studies investigated the effect of tobacco smoking on the skeletal muscles. Muscle wasting and reduction in muscle mass were evident in smokers and were explained by stimulation of protein breakdown, impaired muscle protein synthesis, and oxidative fiber atrophy [88,89,90].
In a large data analysis of women and men, higher levels of alcohol intake (more than 2 standard units of alcohol daily) were found to produce a significant increase in the risk of hip and other osteoporotic fractures [91]. Excessive alcohol consumption is known to have a direct negative impact on bone-forming cells and the hormones that regulate calcium metabolism. Furthermore, chronic, heavy alcohol consumption is linked to decreased food intake (including low calcium, vitamin D, and protein intakes) and overall poor nutritional status, which has a negative impact on skeletal health. Excessive alcohol consumption also increases the risk of falling and, as a result, the possibility of fracture.
Falls risks in elderly
Falls are one of the most common and serious issues that contribute to disability, particularly among the elderly. Every year, more than 30% of people over the age of 65 fall. The falls are recurring in roughly half of the cases. This percentage rises to around 40% in people over the age of 85 [92]. Falls are the most common type of accident in people 65 and older, and they are the leading cause of hospitalization for injury in this age group. Fall-related injuries are associated with an increased risk of death. The associated use of ambulance services, social services, and hospital care incurs significant financial costs [93].
There are many risk factors that contribute to the vulnerability of falling in this age group. Person-specific (or intrinsic) and environmental (or extrinsic) fall risk factors are frequently distinguished. Personal factors include a person’s age, functional abilities, chronic diseases such as diabetes and spondylodegenerative disorders, polypharmacy, visual problems, and gait disturbances. Poor-fitting footwear, slippery floors or loose rugs, tripping hazards, a lack of stair railings or grab bars, unstable furniture, and poor lighting are examples of environmental risk factors [94].
Counteracting the negative effects of aging on the musculoskeletal system
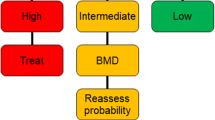
There is substantial inter-individual variability in the aging process, so biological age can differ considerably from chronological age [95]. Therefore, it is advisable to tailor an individualized management program that meets the requirements, abilities, and risk factors of the specific person. Figure 1 shows a scheme for optimizing musculoskeletal health in the elderly. This will be discussed in more detail in this section.
Algorithm to optimize musculoskeletal health in the elderly population proposed by the Egyptian Academy of Bone Health & Metabolic Bone Diseases
FRAX Fracture Risk Assessment Tool, FRAS Fall Risk Assessment Score, SARS-F Sarcopenia Screening Questionnaire, *VF screening questionnaire Vertebral Fracture Screening Questionnaire (Table 1)
Patient education
The complexities and heterogeneities of the aging process have made defining and measuring aging difficult; therefore, patient education relies primarily on the individual patient’s challenges and how to tackle them. Table 2 shows recommendations for how to guide the person to attain stronger bones, joints, and muscles.
Exercises for healthier bone and muscles
Like medications, exercises should be prescribed as regards the type of exercise, strength, frequency, and duration. The choice and type of exercise should be based on shared decision-making with the patient and tailored to the patient’s own condition.
Stretching exercises
These exercises aim to stretch the muscle fibers and their tendons to help improve the range of joint motion. They are an essential warm-up component of every exercise program as they decrease the incidence of muscle and tendon injury during exercise (Table 3).
Strengthening exercises
These are the exercises performed against resistance aiming to increase muscle power and/or bulk. A noticeable increase in muscle strength and endurance was observed when elderly individuals participate in a resistance training program of appropriate duration and intensity [96].
Resistance can be provided by the use of elastic bands or free weights such as dumbbells. Strength-training exercises should be done 2–3 times per week. Depending on how long the older adult rests between sets or exercises, the program should last 20 to 30 min. You might suggest that older adults listen to music while doing the workout.
Each exercise should be performed 8 to 15 times. If the elderly person cannot lift the weight eight times, it is too heavy and he or she should choose a lighter weight. If an older person can complete 15 repetitions of each exercise, he or she should use a heavier weight. After 8 to 15 repetitions, instruct the older adult to rest for 1 to 2 min before repeating the exercise for another 8 to 15 repetitions. A set is defined as 8 to 15 repetitions. Each strengthening exercise should be performed 1–2 times by the elderly person.
Dietary considerations are important in stimulating muscle hypertrophy with exercise. A recent meta-analysis found that protein supplementation can boost muscle mass and strength gains from strength training in both young and old volunteers [97].
Balance exercises
These exercises improve the balance of elderly persons and prevent falls with their sequels. It is either static or dynamic balance exercises. Static balance exercises are done while the patient is standing still, while dynamic balance exercises are done while the patient is changing his position.
The eyes and inner ears aid the nervous and musculoskeletal systems in maintaining balance and preventing falls. Many times, one exercise can help with both strength and balance, especially when the lower limb muscles are strengthened.
Most balance exercises can be done almost anywhere, at any time, and as frequently as older adults want, as long as they have something sturdy nearby to hold or exercising in a room corner with a sturdy chair in front if they become unsteady. Begin by incorporating balance training into daily activities, such as standing on one foot while doing dishes or brushing your teeth. Balance exercises should be done in supportive shoes or bare feet.
The older adult can begin with five balance-specific exercises performed twice per week for 10 to 15 s each.
Endurance exercises
Endurance exercises involve the contraction of the big muscles and increase the heat and respiratory rates with an intensity that allows an individual to sustain the activity for prolonged periods of time without undue fatigue. They include walking, swimming, biking, dancing, and stair-climbing. These 4 types of exercises were recommended and incorporated in several studies [98,99,100].
The hallmark of this type of exercise training is an enhanced metabolic capacity. However, endurance training is not typically associated with changes in muscle size or force-generating capacity.
It is worth mentioning that although walking primarily works the major muscles of the legs, older adults should also swing their arms. This will help to loosen their shoulders and make the walk more enjoyable and effective.
Both resistance and endurance exercises appear to benefit mitochondrial health and function by reducing oxidative damage, improving oxidative coupling ability, and increasing mitochondrial and mitochondrial protein genesis [101].
Tai Chi training
“Tai Chi” is a traditional Chinese exercise that has been practiced for over a thousand years in China. This is a mind–body sport that helps the body stay healthy. It also includes movement in quiescence or action, which is appropriate for the elderly as exercise. By strengthening the muscles and training the body to maintain balance in a variety of positions, Tai Chi can reduce the fear of falling.
Growing evidence suggests that “Tai Chi” improves physical function and the quality of life for the elderly. This improved body balance, flexibility, and muscle strength, as well as boosted elderly confidence [102]. More than 500 studies and 120 systematic reviews on Tai Chi have been published. The strongest evidence of benefit is for preventing falls in community-dwelling older adults, osteoarthritis, Parkinson disease, chronic obstructive pulmonary disease rehabilitation, cognitive capacity improvement, and balance and aerobic capacity improvement [103].
Tai Chi is a low-impact, slow-motion exercise in which a person moves while breathing deeply and naturally, focusing one’s attention on bodily sensations, similar to some types of meditation. Although there are various schools of tai chi, key features such as mindfulness, structural alignment, and flexibility are shared by all [104]. Tai Chi forms are constantly evolving, including shortened protocols for the elderly.
Exercise contraindications in elderly
Only a few untreatable or serious medical conditions may prevent an elderly person from engaging in moderate to vigorous exercise (Table 4). Certain types of exercise may need to be avoided temporarily during treatment for illnesses such as cancer, hernias, cataracts, retinal bleeding, or joint injuries. It is important to note that having cardiovascular disease, diabetes, stroke, osteoporosis, depression, dementia, chronic pulmonary disease, chronic renal failure, peripheral vascular disease, or arthritis (all of which can exist in the same person) is not a reason to avoid exercise. Most of these conditions will benefit from exercise, which may not be possible with medication alone [105].
Patient monitoring: developing a toolkit for the assessment and monitoring of musculoskeletal aging
Monitoring of all the musculoskeletal tissue age-related changes is vital for the long-term management program of older adults. This can be achieved through the development of a toolkit able to provide an integrated evaluation of musculoskeletal aging. This toolkit is intended to be a standard-practice instrument for quantifying and characterizing musculoskeletal tissues during “normal aging.” Fig. 2 shows a suggested toolkit for the assessment and monitoring of musculoskeletal aging. This toolkit should be valid, quantifiable, reproducible, and applicable on a large scale.
Suggested toolkit for the assessment and monitoring of musculoskeletal aging
*OPQolQ Osteoporosis Quality of Life Questionnaire (Table 5). FRAX 10-year fracture probability assessment, FRAS Falls Risk Assessment Score, SARC-F Sarcopenia Screening Questionnaire, MRI Magnetic resonance imaging, CT Computed tomography
National strategies to promote musculoskeletal health: One Musculoskeletal Health program
A better understanding of healthy musculoskeletal aging and the risk factors associated with premature aging will allow for the development of new and better-targeted therapies for common musculoskeletal disorders. The One Health program is “an approach to designing and implementing programs, policies, legislation, and research in which multiple sectors communicate and work together to achieve better public health outcomes” (https://www.who.int/europe/initiatives/one-health). One Musculoskeletal Healthprogram is a good example of how efforts can be collated at a national level to optimize bone and muscle health particularly in older adults.
The Ministry of Health and Population began developing health programs for older people within its structure in 2001. The Ministry of Social Affairs has its fund to provide a monthly allowance (pension) to the low-income families. The elderly clubs (daycare centers in which older adults can practice different activities under the supervision of the organizing committees and the Ministry of Social Affairs) and social training programs (program for older adults in Egypt to prepare them for the changes to occur after retirement) are provided by the Ministry of Social Affairs.
The Egyptian Academy of Bone Health and Metabolic Bone Diseases has also participated in the national musculoskeletal health optimization program. Primary prevention of osteoporotic fractures through opportunistic risk-based screening in older adults in care homes has been launched by the Egyptian Academy [8]. Primary prevention is the first level of defense and is all about preventing the fragility fracture from actually occurring. In the same vein, the academy has launched its national Fracture Liaison Service (FLS) which represents the best secondary fracture prevention model of care for managing osteoporosis following fragility fractures and falls. Fourteen centers recognized the International Osteoporosis Foundation (IOF) are functioning in Egypt covering 70% of the population. The Academy has published its clinical standards for Fracture Liaison Services [106] which has proved to be effective in both individual morbidity and mortality as well as cost [107]. Economic evaluation of osteoporosis liaison service for secondary fracture prevention in osteoporotic older adults with previous hip fracture in Egypt was reported to be cost-effective [108]. Patient and health care professional education, social media, and community activities help to increase awareness among the Egyptian population health care providers facilitating the early identification of those at high risk of fracture.
The academy had also developed the first integrated program for post-fracture care in Egypt which involved assessment of fracture probability, fall risk, sarcopenia, and quality of life alongside with prescription of the proper anti-osteoporotic medications and rehabilitation program with scheduled monitoring of the patient to ensure the medication adherence, any medication side effects, physical activity, and imminent fractures if any [109].
Conclusion
Many changes in the musculoskeletal system are the result of disuse rather than simple aging. Less than 10% of the Egyptian population engages in regular exercise, with the most sedentary group being those over the age of 60. Long-term, regular exercise may help to prevent bone and muscle mass loss as well as age-related increases in body fat. Exercise also helps the body maintain its ability to deliver and use oxygen efficiently, as well as improve its response time. It is not necessary for an exercise program to be strenuous in order for it to be considered effective. The 30 min of moderate activity can be divided into shorter increments. Even moderate physical activity can lower an individual’s risk of developing high blood pressure, heart disease, diabetes, and some forms of cancer.
Availability of data and materials
The data sets used are available from the corresponding author upon reasonable request.
Abbreviations
- BMD:
-
Bone mineral density
- CAPMAS:
-
Central Agency for Public Mobilization and Statistics
- CT:
-
Computed tomography
- FLS:
-
Fracture Liaison Service
- FRAS:
-
Fall Risk Assessment Score
- FRAX:
-
Fracture Risk Assessment Tool
- FTO:
-
Fat mass and obesity-associated gene
- IOF:
-
International Osteoporosis Foundation
- MRI:
-
Magnetic resonance imaging
- OPQolQ:
-
Osteoporosis Quality of Life Questionnaire
- VF:
-
Vertebral fracture
- WHO:
-
World Health Organization
References
Weiss D, Zhang X (2020) Multiple sources of aging attitudes: perceptions of age groups and generations from adolescence to old age across China, Germany, and the United States. J Cross Cult Psychol 51(6):407–423
Decade of healthy ageing 2020–2030. WHO. https://www.who.int/docs/default-source/documents/decade-of-health-ageing/decade-healthy-ageing-update-march-2019.pdf?sfvrsn=5a6d0e5c_2#:~:text=Healthy%20Ageing%20is%20the%20process,enables%20wellbeing%20in%20older%20age. [Accessed on 13 Apr 2023]
Healthy ageing and functional ability. WHO. https://www.who.int/news-room/questions-and-answers/item/healthy-ageing-and-functional-ability [Accessed on 13 April 2023].
Andrew M Briggs, Marita J Cross, Damian G Hoy, Lídia Sànchez-Riera, Fiona M Blyth, Anthony D Woolf, et al. Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 World Health Organization World Report on Ageing and Health. Gerontologist. 2016;56 Suppl 2:S243–55. https://doi.org/10.1093/geront/gnw002.
WORLDHEALTHRANKINGS.https://www.worldlifeexpectancy.com/egypt-life-expectancy.
Present and justify a problem and solution requirements. https://sites.google.com/a/stemegypt.edu.eg/2015-1-70/Present-and-Justify-a-Problem-and-Solution-Requirements.
El Miedany Y, Gadallah NA, Toth M (2022) Optimizing osteoporosis management: targeting to treat—an initiative by the Egyptian Academy of Bone Health. Egypt Rheumatol Rehabil 49:61. https://doi.org/10.1186/s43166-022-00161-x
El Miedany Y, El Gaafary M, Gadallah N, Mahran S, Fathi N, Abu Zaid MH et al (2023) Osteoporosis treatment gap in patients at risk of fracture in Egypt: a multi-center, cross-sectional observational study. Arch Osteoporos 18(1):58
Freemont AJ, Hoyland JA (2007) Morphology, mechanisms and pathology of musculoskeletal ageing. J Pathol 211:252–259
Cheong HW, Peh WC, Guglielmi G (2008) Imaging of diseases of the axial and peripheral skeleton. Radiol Clin North Am 46(703–33):vi
Rosen C, Donahue L, Hunter S (1994) Insulin-like growth factors and bone: the osteoporosis connection. Proc Soc Exp Biol Med 206:83–102
Kirk B, Feehan J, Lombardi G, Duque G (2020) Muscle, bone, and fat crosstalk: the biological role of myokines, osteokines, and adipokines. Curr Osteoporos Rep 18(4):388–400. https://doi.org/10.1007/s11914-020-00599-y. (PMID: 32529456)
Gouspillou G, Bourdel-Marchasson I, Rouland R, Calmettes G, Biran M, Deschodt-Arsac V, Miraux S, Thiaudiere E, Pasdois P, Detaille D, Franconi JM (2014) Mitochondrial energetics is impaired in vivo in aged skeletal muscle. Aging Cell 13(1):39–48
Migliavacca E, Tay SK, Patel HP, Sonntag T, Civiletto G, McFarlane C, Forrester T, Barton SJ, Leow MK, Antoun E, Charpagne A (2019) Mitochondrial oxidative capacity and NAD+ biosynthesis are reduced in human sarcopenia across ethnicities. Nat Commun 10(1):5808
Rantanen T, Harris T, Leveille SG et al (2000) Muscle strength and body mass index as long-term predictors of mortality in initially healthy men. J Gerontol Med Sci 55A:M168–M173
Rantanen T, Volpato S, Ferrucci L, Heikkinen E, Fried LP, Guralnik JM (2003) Handgrip strength and cause-specific and total mortality in older disabled women: exploring the mechanism. J Am - Geriatr Soc 51:636–641
Newman A, Kupelian V, Visser M et al (2006) Strength, but not muscle mass, is associated with mortality in the Health, Aging and Body Composition Study cohort. J Gerontol Biol Sci Med Sci 61A:72–77
Loeser RF (2010) Age-related changes in the musculoskeletal system and the development of osteoarthritis. Clin Geriatr Med 26(3):371–386
Demontiero O, Vidal C, Duque G (2012) Aging and bone loss: new insights for the clinician. Ther Adv Musculoskelet Dis 4(2):61–76
Agostini D, Gervasi M, Ferrini F, Bartolacci A, Stranieri A, Piccoli G (2023) An integrated approach to skeletal muscle health in aging. Nutrients 15(8):1802
Stuart-Jones V: Is ‘obese’ the new ‘big-boned’? British Journal of Cardiac Nursing. 2010;5:361 https://doi.org/10.12968/bjca.2010.5.8.66243.
Greco EA, Fornari R, Rossi F et al (2010) Is obesity protective for osteoporosis? Evaluation of bone mineral density in individuals with high body mass index. Int J Clin Pract 64(6):817–820. https://doi.org/10.1111/j.1742-1241.2009.02301.x
Kim KC, Shin DH, Lee SY et al (2010) Relation between obesity and bone mineral density and vertebral fractures in Korean postmenopausal women. Yonsei Med J 51(6):857–863
Ilich JZ, Kelly OJ, Inglis JE et al (2014) Interrelationship among muscle, fat, and bone: connecting the dots on cellular, hormonal, and whole body levels. Ageing Res Rev 15:51–60. https://doi.org/10.1016/j.arr.2014.02.007
Felson DT, Zhang Y, Hannan MT et al (1993) Effects of weight and body mass index on bone mineral density in men and women: the Framingham Study. J Bone Miner Res 8(5):567–573
Hotamisligil GS, Arner P, Caro JF et al (1995) Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest 95(5):2409–2415
Ferrante AW (2007) Obesity-induced inflammation: a metabolic dialogue in the language of inflammation. J Intern Med 262(4):408–414
Abdallah BM, Kassem M (2012) New factors controlling the balance between osteoblastogenesis and adipogenesis. Bone 50(2):540–545. https://doi.org/10.1016/j.bone.2011.06.030
Beresford JN, Bennett JH, Devlin C et al (1992) Evidence for an inverse relationship between the differentiation of adipocytic and osteogenic cells in rat marrow stromal cell cultures. J Cell Sci 102(Pt 2):341–351
Nuttall ME, Gimble JM (2004) Controlling the balance between osteoblastogenesis and adipogenesis and the consequent therapeutic implications. Curr Opin Pharmacol 4(3):290–294. https://doi.org/10.1016/j.coph.2004.03.002
Frayling TM, Timpson NJ, Weedon MN et al (2007) A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 316(5826):889–894. https://doi.org/10.1126/science.1141634
Guo Y, Liu H, Yang TL et al (2011) The fat mass and obesity associated gene, FTO, is also associated with osteoporosis phenotypes. PLoS ONE 6(11):e27312
Heo M, Faith MS, Pietrobelli A, Heymsfield SB (2012) Percentage of body fat cutoffs by sex, age, and race-ethnicity in the US adult population from NHANES 1999–2004. Am J Clin Nutr 95:594–602
Gallagher D et al (1998) Organ-tissue mass measurement allows modeling of REE and metabolically active tissue mass. Am J Physiol 275:E249–E258
Wilson MM, Morley JE (2003) Invited review: aging and energy balance. J Appl Physiol 95:1728–1736
Conley KE et al (2000) Ageing, muscle properties and maximal O2 uptake rate in humans. J Physiol 526:211–217
Conley KE, Jubrias SA, Esselman PC (2000) Oxidative capacity and ageing in human muscle. J Physiol 526:203–210
Barazzoni R, Bischoff S, Boirie Y, Busetto L, Cederholm T, Dicker D et al (2018) Sarcopenic obesity: time to meet the challenge. Obes Facts 11(4):294–305
Hong SH, Choi KM (2020) Sarcopenic obesity, insulin resistance, and their implications in cardiovascular and metabolic consequences. Int J Mol Sci 21(2):494
Lorenzo M. Donini, A , Luca Busetto, B Stephan C. Bischoff, B Tommy Cederholm, D Maria D. Ballesteros-Pomar, e John A. Batsis, et al. Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO Consensus Statement. Obes Facts. 2022;15(3): 321–335.
Klein-Nulend J, Bacabac RG, Bakker AD (2012) Mechanical loading and how it affects bone cells: the role of the osteocyte cytoskeleton in maintaining our skeleton. Eur Cell Mater 24:278–291. https://doi.org/10.22203/eCM.v024a20
Tong X, Chen X, Zhang S, Huang M, Shen X, Xu J et al (2019) The effect of exercise on the prevention of osteoporosis and bone angiogenesis. BioMed Res Int 2019:8171897. https://doi.org/10.1155/2019/8171897
Exercise and the regulation of endocrine hormones (2015) Hackney AC, Lane AR. Prog Mol Biol Transl Sci 135:293–311. https://doi.org/10.1016/bs.pmbts.2015.07.001. (Epub 2015 Aug 5)
Benedetti M, Furlini G, Zati A, Mauro G (2018) The effectiveness of physical exercise on bone density in osteoporotic patients. BioMed Res Int 2018
Bell KE, von Allmen MT, Devries MC, Phillips SM (2016) Muscle disuse as a pivotal problem in sarcopenia-related muscle loss and dysfunction. J Frailty Aging 5:33–41. https://doi.org/10.14283/jfa.2016.78
Welch C, Hassan-Smith ZK, Greig CA, Lord JM, Jackson TA (2018) Acute sarcopenia secondary to hospitalisation - an emerging condition affecting older adults. Aging Dis 9:151–164. https://doi.org/10.14336/AD.2017.0315
Alkner Björn A, Tesch Per A (2004) Knee extensor and plantar flexor muscle size and function following 90 days of bed rest with or without resistance exercise. Eur J Appl Physiol 93(3):294–305. https://doi.org/10.1007/s00421-004-1172-8
Gariballa SE (2000) Nutritional support in elderly patients. J Nutr Health Aging 4:25–27
Furman EF (2006) Undernutrition in older adults across the continuum of care: nutritional. J Gerontol Nurs 32:22–27
Giezenaar C, Chapman I, Luscombe-Marsh N, Feinle-Bisset C, Horowitz M, Soenen S (2016) Ageing is associated with decreases in appetite and energy intake—a meta-analysis in healthy adults. Nutrients 8(1):28
Volkert D (2013) Malnutrition in older adults – urgent need for action: a plea for improving the nutritional situation of older adults. Gerontology 59:328–333
Hickson M (2006) Malnutrition and ageing. Postgrad Med J 82:2–8
Chen YM, Ho SC, Woo JL (2006) Greater fruit and vegetable intake is associated with increased bone mass among. Br J Nutr 96:745–751
Reijnierse EM, Trappenburg MC, Leter MJ et al (2015) The association between parameters of malnutrition and diagnostic measures of sarcopenia in geriatric outpatients. PLoS ONE 10(8):e0135933
Deutz NEP, Bauer JM, Barazzoni R et al (2014) Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN expert group. Clin Nutr 33(6):929–936. https://doi.org/10.1016/j.clnu.2014.04.007
Tieland M, Borgonjen-Van den Berg K, Van Loon L, et al. Dietary protein intake in Dutch elderly people: a focus on protein sources. Nutrients. 2015;7(12):9697–706. https://doi.org/10.3390/nu7125496.
Vandewoude MFJ, Alish CJ, Sauer AC, et al. Malnutrition-sarcopenia syndrome: is this the future of nutrition screening and assessment for older adults? J Aging Res. 2012; 2012. https://doi.org/10.1155/2012/651570.
Evans WJ, Paolisso G, Abbatecola AM et al (2010) Frailty and muscle metabolism dysregulation in the elderly. Biogerontology 11(5):527–536. https://doi.org/10.1007/s10522-010-9297-0
National Institutes of Health (US) Dietary supplement fact sheet: calcium [Internet] Bethesda (MD): National Institutes of Health; 2013. [cited 2014 August 23]. Available from: http://ods.od.nih.gov/factsheets/Calcium/HealthProfessional/
Choi YS, Joung H, Kim J. Evidence for revising calcium dietary reference intakes (DRIs) for Korean elderly. FASEB J. 2013;27:1065.28.
Hilger J, Friedel A, Herr R et al (2014) A systematic review of vitamin D status in populations worldwide. Br J Nutr 111:23–45
Boucher BJ (2012) The problems of vitamin D insufficiency in older people. Aging Dis 3:313–329
Watson J, Lee M, Garcia-Casal M (2018) Consequences of inadequate intakes of vitamin A, vitamin B12, vitamin D, calcium, iron and folate in older persons. Current geriatric reports 7:103–113
Waters DL, Wayne SJ, Andrieu S et al (2014) Sexually dimorphic patterns of nutritional intake and eating behaviors in community-dwelling older adults with normal and slow gait speed. J Nutr Health Aging 18:228–233
Seo MH, Kim MK, Park SE et al (2013) The association between daily calcium intake and sarcopenia in older, non-obese Korean adults: the fourth Korea National Health and Nutrition Examination Survey (KNHANES IV) 2009. Endocr J 60:679–686
Ter Borg S, de Groot LC, Mijnarends DM et al (2016) Differences in nutrient intake and biochemical nutrient status between sarcopenic and nonsarcopenic older adults-results from the Maastricht Sarcopenia Study. J Am Med Dir Assoc 17:393–401
Verlaan S, Aspray TJ, Bauer JM et al (2017) Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: a case-control study. Clin Nutr 36:267–274
Brotto M (2011) Aging, sarcopenia and store-operated calcium entry: a common link? Cell Cycle 10:4201–4202
Fleet JC, Schoch RD (2010) Molecular mechanisms for regulation of intestinal calcium absorption by vitamin D and other factors. Crit Rev Clin Lab Sci 47:181–195
Dzik KP, Kaczor JJ (2019) Mechanisms of vitamin D on skeletal muscle function: oxidative stress, energy metabolism and anabolic state. Eur J Appl Physiol 9(119):825–839
Hirani V, Cumming RG, Naganathan V, Blyth F, Le Couteur DG, Hsu B, Handelsman DJ, Waite LM, Seibel MJ (2018) Longitudinal associations between vitamin D metabolites and sarcopenia in older Australian men: the concord health and aging in men project. J Gerontol: Series A 73(1):131–138
Hengeveld LM, Boer JMA, Gaudreau P, Harris TB, Heymans MW, Jagger C, Mendonça N, Ocké MC, Presse N, Sette S et al (2020) Prevalence of protein intake below recommended in community-dwelling older adults: a meta-analysis across cohorts from the PROMISS consortium. J Cachexia Sarcopenia Muscle 11(5):1212–1222
Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, Phillips S, Sieber C, Stehle P, Teta D et al (2013) Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc 14(8):542–559
Deer RR, Volpi E (2015) Protein intake and muscle function in older adults. Curr Opin Clin Nutr Metab Care 18(3):248–253
Rizzoli R, Bonjour J-P (2004) Dietary protein and bone health. J Bone Miner Res 19:527–531
Hannan MT, Tucker KL, Dawson-Hughes B et al (2000) Effect of dietary protein on bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res 15:2504–2512
Dawson-Hughes B, Harris SS (2002) Calcium intake influences the association of protein intake with rates of bone loss in elderly men and women. Am J Clin Nutr 75:773–779
Burd NA, Gorissen SH, van Loon LJ (2013) Anabolic resistance of muscle protein synthesis with aging. Exerc Sport Sci Rev 41(3):169–173. https://doi.org/10.1097/JES.0b013e318292f3d5
Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy-Westphal A, Cederholm T, Cruz-Jentoft A, Krznaric Z, Nair KS, Singer P, Teta D, Tipton K, Calder PC (2014) Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr 33(6):929–936. https://doi.org/10.1016/j.clnu.2014.04.007
Krok-Schoen JL, A. Archdeacon Price, M. Luo, O. J. Kelly, et al. Low dietary protein intakes and associated dietary patterns and functional limitations in an aging population: a NHANES analysis. J Nutr Health Aging. 2019; 23:338–347
Kuo CW, Chang TH, Chi WL, Chu TC (2008) Effect of cigarette smoking on bone mineral density in healthy Taiwanese middle-aged men. J Clin Densitom 11(4):518–524
Lee S, Kim KN, Shin DA, Ha Y (2014) Association between urine cotinine levels and bone mineral density in lumbar spine and femoral neck among adult males. Spine 39(4):311–317
Tamaki J, Iki M, Sato Y, Kajita E, Kagamimori S, Kagawa Y, Yoneshima H (2010) Smoking among premenopausal women is associated with increased risk of low bone status: the JPOS Study. J Bone Miner Metab 28:320–327
Cangussu LM, Nahas-Neto J, Petri Nahas EA, Rodrigues Barral AB, Buttros DD, Uemura G (2012) Evaluation of postural balance in postmenopausal women and its relationship with bone mineral density-a cross sectional study. BMC Musculoskelet Disord 13(1):1–7
Jutberger H, Lorentzon M, Barrett-Connor E, Johansson H, Kanis JA, Ljunggren Ö, Karlsson MK, Rosengren BE, Redlund-Johnell I, Orwoll E, Ohlsson C (2010) Smoking predicts incident fractures in elderly men: Mr OS Sweden. J Bone Miner Res 25(5):1010–1016
Thorin MH, Wihlborg A, Åkesson K, Gerdhem P (2016) Smoking, smoking cessation, and fracture risk in elderly women followed for 10 years. Osteoporos Int 27:249–255
Petersen AM, Magkos F, Atherton P, Selby A, Smith K, Rennie MJ, Pedersen BK, Mittendorfer B (2007) Smoking impairs muscle protein synthesis and increases the expression of myostatin and MAFbx in muscle. Am J Physiol Endocrinol Metab 293:E843–E848
Rom O, Kaisari S, Aizenbud D, Reznick AZ (2012) Identification of possible cigarette smoke constituents responsible for muscle catabolism. J Muscle Res Cell Motil 33:199–208
de Oca MM, Loeb E, Torres SH, De Sanctis J, Hernández N, Tálamo C (2008) Peripheral muscle alterations in non-COPD smokers. Chest 133(1):13–18
Kanis JA, Johansson H, Johnell O et al (2005) Alcohol intake as a risk factor for fracture. Osteoporos Int 16:737–742
Akyol AD (2007) Falls in the elderly: what can be done? Int Nurs Rev 54(2):191–196
Gale CR, Cooper C, Aihie SA (2016) Prevalence and risk factors for falls in older men and women: the English Longitudinal Study of Ageing. Age Ageing 45(6):789–794
Anne Felicia Ambrose, Geet Paul, Jeffrey M. Hausdorff. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013; 75(1):51–61
Belsky DW, Caspi A, Houts R, Cohen HJ, Corcoran DL, Danese A et al (2015) Quantification of biological aging in young adults. Proc Natl Acad Sci USA 112:E4104–E4110
Taaffe DR et al (1999) Once-weekly resistance exercise improves muscle strength and neuromuscular performance in older adults. J Am Geriatr Soc 47(10):1208–1214
Cermak NM, Res PT, de Groot LC, Saris WH, van Loon LJ (2012) Protein supplementation augments the adaptive response of skeletal muscle to resistance-type exercise training: a meta analysis. Am J Clin Nutr 96:1454–1464
Cadore Eduardo Lusa, Pinto Ronei Silveira, Bottaro Martim, Izquierdo Mikel et al (2014) Strength and endurance training prescription in healthy and frail elderly. Aging Dis 5(3):183–195
Consitt LA, Dudley C, Saxena G (2019) Impact of endurance and resistance training on skeletal muscle glucose metabolism in older adults. Nutrients 11(11):2636. https://doi.org/10.3390/nu11112636
Cress ME, Buchner DM, Prohaska T, Rimmer J, Brown M, Macera C, Chodzko-Zajko W (2005) Best practices for physical activity programs and behavior counseling in older adult populations. J Aging Phys Act 13(1):61–74
Harper C, Gopalan V, Goh J (2021) Exercise rescues mitochondrial coupling in aged skeletal muscle: a comparison of different modalities in preventing sarcopenia. J Transl Med 19:1–7
Zhang JG, Ishikawa-Takata K, Yamazaki H, Morita T, Ohta T (2006) The effects of Tai Chi Chuan on physiological function and fear of falling in the less robust elderly: an intervention study for preventing falls. Arch Gerontol Geriatr 42(2):107–116
Huston P, McFarlane B (2016) Health benefits of tai chi: what is the evidence? Can Fam Physician 62(11):881–890
Wayne PM (2012) The Harvard Medical School guide to tai chi: 12 weeks to a healthy body, strong heart, and sharp mind. Shambhala Publications Inc, Boston, MA
Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC et al (2007) Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 116(9):1094–1105
Gadallah N, El Miedany Y (2022) Operative secondary prevention of fragility fractures: national clinical standards for fracture liaison service in Egypt—an initiative by the Egyptian Academy of Bone Health. Egypt Rheumatol Rehabil 49:11. https://doi.org/10.1186/s43166-022-00111-7
El Miedany Y, M. El Gaafary, S. Mahran, W. Hassan, N. Gadallah, M. H. Abu-Zaid, et al. Health economics in the secondary prevention of fragility fractures: cost effectiveness analysis of fracture liaison services compared to standard fracture care in Egypt – an initiative by the Egyptian Academy of Bone Health. ESCEO 2023. https://www.wco-iof-esceo.org/sites/wco_23/pdf/WCO23-AbstractBook.pdf Accessed 14th May 2023
El Miedany Y, M. El Gaafary, S. Mahran, W. Hassan, N. Gadallah, M. H. Abu-Zaid, et al. Health economics: cost of hospitalisation for osteoporotic hip fracture: findings from the Egyptian hip fracture database – an initiative by the Egyptian Academy of Bone Health. ESCEO 2023. https://www.wco-iof-esceo.org/sites/wco_23/pdf/WCO23-AbstractBook.pdf Accessed 14 May 2023
El Miedany, Y., Hasab El Naby, M.M., Abu-Zaid, M.H. et al. Post-fracture care program in Egypt: merging subsequent fracture prevention and improving patients’ outcomes—an initiative by the Egyptian Academy of Bone Health. Egypt Rheumatol Rehabil 50, 7 (2023). https://doi.org/10.1186/s43166-023-00173-1
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
All authors shared in writing and reviewing the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El Miedany, Y., Mahran, S. & Elwakil, W. One musculoskeletal health: towards optimizing musculoskeletal health in Egypt—how to be a bone and muscle builder by the Egyptian Academy of Bone Health and Metabolic Bone Diseases. Egypt Rheumatol Rehabil 50, 33 (2023). https://doi.org/10.1186/s43166-023-00199-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-023-00199-5