Abstract
Background
Despite a broad spectrum of effective anti-osteoporosis therapies and a growing number of older adults worldwide, the number of people receiving appropriate secondary fracture prevention is not yet optimum or achieved its expected target, i.e., avoiding refracture.
Main body
To close this gap in the patients’ care, and in concordance with the International Osteoporosis Foundation (IOF) as well as international organizations recommendations, the Egyptian Academy of Bone Health and Metabolic Bone Diseases has launched specialised healthcare system for fracture liaison services (FLSs). FLS is a small team of healthcare professionals who identify, investigate, initiate therapy and arrange for follow-up plan over time, for people aged 50 and above presenting with a fragility fracture. Such comprehensive service requires operative clinical standards which would help to standardise the service across the different centres to become effective and sustainable. An estimated 71.8% of the Egyptian population currently have access to a local FLSs. This article aims at setting up evidence-based standards of post-fracture care and provide the necessary index for efficient implementation of secondary fracture prevention in the different FLS centres in Egypt.
Conclusion
The Egyptian FLS clinical standards agree with the international protocols and are an effective approach to target interventions to the properly identified patients at risk. The Egyptian model has identified 19 key performance indicators to measure the effectiveness of fracture liaison services and guide quality improvement.
Similar content being viewed by others
Background
Osteoporosis is the most common chronic bone disease that affects the bones’ structure as well as the strength and makes them prone to fractures. These fractures are usually called fragility fractures as they tend to occur after low trauma which normally would not cause a bone to break [1]. The World Health Organization (WHO) has identified a fragility fracture as “one which occurs due to forces equivalent to a fall from a standing height or less”. Recently, the new concept of imminent fracture risk has been introduced into the osteoporosis field. Imminent fracture risk has been defined as a significantly higher risk of sustaining a fracture within the 12–24 months after the initial (first) fracture [2,3,4].
Fragility fractures cause significant negative impact on the person’s life which is attributed to the significant drop in the subject’s mobility, quality of life as well as ability to work or function [5, 6]. The rise in morbidities linked to fragility fractures is greater than can be associated with just aging and therefore represents a major clinical challenge [7]. On another front, an increase in mortality has been linked to the fragility fractures too [8,9,10,11,12]. Consequently, an understanding of the factors leading to fracture is an important research point, which in turn would facilitate management approaches to identify those subjects at high risk of sustaining a fracture and effectively lessen the disease clinical burden.
Worldwide it is estimated that one in two women and one in five men will sustain a fragility fracture after the age of 50 years [13]. In Egypt, the prevalence of osteoporosis was reported at 28.4% in women and 21.9% in men; whilst 26% of men and 53.9% of women were reported to have osteopenia [14]. In a cross-sectional study [15] carried out, in the year 2016, to assess fracture risk among older adults living in geriatric homes in Egypt, results revealed that the prevalence of fractures was 21%. The most prevalent risk factor of fractures was recurrent falls (49%). The recently published consensus on treat-to-target approach for osteoporosis in Egypt [16] endorsed the Fracture liaison service, with a high level of agreement amongst its recommendations. This was in concordance with the Capture the Fracture® initiative launched by the International Osteoporosis Foundation to facilitate the implementation of coordinated multi-disciplinary models of care for secondary fracture prevention. Secondary prevention of fractures is recognized as the single most important step in directly improving patient care and reducing spiralling fracture-related healthcare costs worldwide. The global program includes 49 countries and 682 fracture liaison services. On the first of September 2021, 13 FLS centers have started providing their services in Egypt for the patients presenting with fragility fractures all over the country. FLSs have been reinforced by the evidence signifying that they are clinically and cost effective.
The objective of this article is to set evidence-based standards of post-fracture care that both the patients as well as healthcare professionals expect. The standards are projected to address the entire FLS pathway.
Main text
Fracture liaison service (FLS): the concept
FLS is a crucial constituent of a comprehensive and integrated strategy to minimize the risk of fractures and falls among people older than 50 years old. Assessment within FLS should be offered to every patient admitted or presented with low trauma fracture. The most common skeletal sites of fragility fractures are the hip, spine, wrist, humerus or pelvis. It should be highlighted that a significant percentage of vertebral fractures do not come to clinical attention and they are reported as incidental finding in the radiology reports [17].
The structure of the FLS must be set up to deliver optimum secondary preventive care in the local setting. Internationally, FLSs have been established in the hospital setting [18], in primary care organisations [19] and, in Health Maintenance Organisations (HMOs) [in the United States] [20]. Locally, in Egypt, the optimal FLS model of care has been agreed to be in the secondary care—hospital setting, where most, if not all, of the fractured patients receive their orthopedic surgery management.
FLS is centred around an FLS Lead Clinician who would establish a multi-disciplinary group to design the local FLS model of care; and a devoted FLS coordinator who operates to pre-agreed protocol to case-finding and consequently assessment of the patients who present with a fragility fracture. An integrated care pathway should be agreed with other specialities dealing with patient fractures such as orthopedic and radiology departments. A quality improvement process to develop the FLS should be monitored with ongoing auditing of the FLS to confirm that the fragility fracture sufferers receive appropriate assessment and long-term care (Fig. 1).
Clinical standards for fracture liaison service
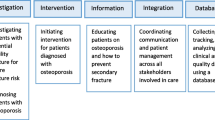
All relevant professional organisations [21, 22], have recognised the need for universal access to FLSs. In 2015, the Royal Osteoporosis Society (ROS) in the UK published standards drafted by a multidisciplinary group which were endorsed by all relevant national professional organizations and IOF [23]. The ROS standards were based on the ‘5IQ’ approach, relating to the key functions of an FLS including the following: (1) identification; (2) investigation; (3) information; (4) intervention; (5) integration and quality. In concordance, the clinical standards for FLS in Egypt have adopted similar approach with some amendments (Table 1).
Key performance indicators
The identification of the parameters that reflect the service performance and outcomes are not only the key factors for the service improvement, but also indicators for aspects of the service that require further development. Consequently, the impact of these developments on the service delivery can be evaluated in a later assessment. The Egyptian framework identified 19 key performance indictors to assess the Egyptian FLSs at the organisational level (Fig. 2). Among these are the 13 standards proposed by The Capture the Fracture Best Practice Framework (BPF) [29] and identified as key performance indicators for measuring the FLS scope.
Other values of these key performance indicators are comparative analysis of the FLSs across different organizations at the global level, namely the global rates of identification, fracture as well as falls risk assessment, categories of management, communication, and monitoring. These standards are helpful for recognizing major gaps in the delivery of the service such as types of the identified patients presenting with fractures and the continuity of the follow up process. On the other hand, they are less helpful for supporting established FLSs achieve their peak potential targets for preventing secondary fractures.
The clinical Standards in Lay-man’s terms for the people receiving the care
Education for patients, family and carers are vital to achieve optimum FLSs utilization and should be incorporated into the contemporary clinical standards. Representing one of the evidence-based care parameters, these clinical standards should be available for patients in simplified style. Each unit should describe what each standard means to adults over the age of 50 who sustain a fragility fracture. By clarifying the main standards of the service, the patients will be able to have informed dialogue with their healthcare professionals. Figure 3 shows the FLS clinical standards in a patient-friendly format.
Data base
Egyptian Academy of Bone Health and Metabolic Bone Diseases has commissioned its own electronic data recording for the FLSs in Egypt. The Fracture Liaison Service Database (EABoM) is a clinically led, web-based national software for secondary fracture prevention in Egypt. The EABoM comprises 9 Components: patient’s data, survey, DXA results, lab results, fracture and falls risk, sarcopenia risk, reports, demographics, and statistical analysis. It facilitates not only recording of the patients’ data in their initial visit, but also all their data in the follow up visits. Its statistical analysis tool facilitates the auditing process and evaluation of the services provided against the clinical standards as well as the FLS agreed key performance indicators/outcomes as well as the national guidelines for osteoporosis management.
Implementing the FLS standards
Several factors should be considered when setting up a model for FLS. These include the presence of current pathways, the local network as well as the facility of collaborative work with other departments such as orthopedic surgery, geriatrics, and radiology. Also, it may vary depending on local resources and the local health system facilities as well as priorities. However, the advantage is that adopting these standards is expected to facilitate the opportunity of replicating the principles of evidenced-based best practice effectively across the country. Setting up any new service necessitates time and dedication. Over the past 2 years, the Egyptian Academy of Bone Health has provided bespoke and expert support to launch the FLS in different centers across Egypt. This was carried out through online virtual meetings and in other occasions through inviting international speakers as well as the IOF masters with experience in setting up the FLS centers. Locally, the academy also provided assistance with induction and training of the FLS coordinator; advice regarding relevant protocols and care pathways for the service; as well as advice regarding data collection and methods of analysis, reporting and evaluation.
An estimated 71.8% of the Egyptian population currently have access to a local FLS. However, the strategies implemented for providing the service may vary according the resources and staffing.
Working with national guidelines
These FLS clinical standards have been set up to be implemented adopting the national guidelines [16] for the assessment and prevention of fragility fractures as well as falls, in addition to management of osteoporosis. Also, to prevent the development of any further fractures after the primary one. Clinical protocol has been developed and shared across the country to be implemented locally. The osteoporosis management algorithm set in the guidelines provide a road map which support all the 5 FLS clinical standards identified in this report. This ensures harmony and equivalence of the management approaches all over the country.
Discussion
The gap in osteoporosis care recognized after fragility fractures is noticeably growing. The cause for this care gap to exist and continue is multifaceted [21]. One of the major contributing factors is the un-clarity concerning where clinical responsibility lies [30]. Neither orthopedic surgeons who manage the acute fractures nor the primary care health care professionals who are responsible for provide long-term patient management, appear to be interested in getting engaged in secondary fracture prevention [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26, 29, 30]. The net result is poor provision of proper pre-emptive measures to prevent subsequent fractures. By developing and applying these clinical standards, evidence-based best practice can be implemented and effectively simulated across the country. This will help to enhance the patients’ outcomes, reduce the future fractures burden and ensure operative and proper use of health resources. FLS may also reduce post-fracture mortality [8,9,10,11].
Clinical Standards for Fracture Liaison Services have been developed in Canada [28] and the UK [21, 23]. The International Osteoporosis Foundation (IOF) has also developed internationally endorsed standards for FLS in the form of the Capture the Fracture® Best Practice Framework [21, 23, 31]. The purpose of these documents is to set evidence-based standards of post-fracture care that health professionals and patients should expect. The Egyptian FLS clinical standards are in agreement with the international recommendations and were based on the ‘5IQ’ approach, relating to the key functions of the FLS. However, the Key performance indicators identified in the Egyptian model have included 6 more parameters. Four items for risk assessment namely: bone health evaluation, functional assessment, sarcopenia assessment, cognition evaluation; and 2 items for management namely, strengthening/balance exercise, and rehabilitation management program. Fractures have a significant negative impact on the patients’ functional abilities as well as health-related quality of life. Fractures are also associated with high rates of morbidity and mortality [32]. The strategy to osteoporotic fracture management should be comprehensive and includes a combination of medical therapy, nutritional management as well as a rehabilitation program tailored to the individual patient’s fracture type and risk factor [33]. The target is to improve activities of daily living, reduce the risk of falling and increase safety while reducing the degree of bone mass loss. Therefore, the added parameters are relevant to the FLS clinical standards as it will help in minimizing the risk of having a re-fracture.
Conclusion
Whilst fracture occurrence can be a life-changing experience at the individual’s level, with significant negative impact on the persons’ mobility as well as consequent negative impact on the subject’s quality of life causing social isolation and possibly depression, FLSs present a golden opportunity to minimize these risks and reduce the likelihood sustaining another (i.e., a secondary fracture). The Egyptian FLS clinical standards are in agreement with the international protocols and are an effective approach to target interventions to the properly identified patients at risk.
Availability of data and materials
NA
Abbreviations
- IOF:
-
International Osteoporosis Foundation
- FLSs:
-
Fracture liaison services
- DXA:
-
Dual X-ray absorptiometry
- A&E:
-
Accident and emergency
References
Mauck KF, Clarke BL (2006) Diagnosis, Screening, Prevention, and Treatment of Osteoporosis. Mayo Clin Proc 81(5):662–672
Bonafede M, Shi N, Barron R, Li X, Crittenden DB, Chandler D (2016) Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch Osteoporos 11:26
Kanis JA, Cooper C, Rizzoli R, Abrahamsen B, Al-Daghri NM, Brandi ML, Cannata-Andia J, Cortet B, Dimai HP, Ferrari S, Hadji P, Harvey NC, Kraenzlin M, Kurth A, McCloskey E, Minisola S, Thomas T, Reginster JY (2017) European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Identification and management of patients at increased risk of osteoporotic fracture: outcomes of an ESCEO expert consensus meeting. Osteoporos Int 28:2023–2034
Van Geel TACM, van Helden S, Geusens PP, Winkens B, Dinant GJ (2009) Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis 68:99–102
Bentler SE, Liu L, Obrizan M, Cook EA, Wright KB, Geweke JF, Chrischilles EA, Pavlik CE, Wallace RB, Ohsfeldt RL, Jones MP, Rosenthal GE, Wolinsky FD (2009) The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol 170:1290–1299
Leibsen CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ (2002) Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriat Soc 50:1644–1650
International Osteoporosis Foundation. Capture the Fracture Report 2012. https://www.iofbonehealth.org/capture-fracturereport-2012. Accessed 21 November 2021
Bliuc D, Alarkawi D, Nguyen TV, Eisman JA, Center JR (2015) Risk of subsequent fractures and mortality in elderly women and men with fragility fractures with and without osteoporotic bone density: the Dubbo osteoporosis epidemiology study. J Bone Miner Res 30:637–646
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of osteoporotic fractures research group. Arch Intern Med 159:1215–1220
Katsoulis M, Benetou V, Karapetyan T, Feskanich D, Grodstein F, Pettersson-Kymmer U, Eriksson S, Wilsgaard T, Jørgensen L, Ahmed LA, Schöttker B, Brenner H, Bellavia A, Wolk A, Kubinova R, Stegeman B, Bobak M, Boffetta P, Trichopoulou A (2017) Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med 281:300–310
Klop C, van Staa T, Cooper C, Harvey N, de Vries F (2017) The epidemiology of mortality after fracture in England: variation by age, sex, time, geographic location, and ethnicity. Osteoporos Int 28:161–168
von Friesendorff M, McGuigan FE, Wizert A, Rogmark C, Holmberg AH, Woolf AD, Akesson K (2016) Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int 27:2945–2953
Van Staa TP, Dennison EM, Leufkens HGM, Cooper C (2001) Epidemiology of fractures in England and Wales. Bone 29(6):517–522
Gheita T, Hammam N (2018) Epidemiology and awareness of osteoporosis: a viewpoint from the Middle East and North Africa. Int. J. Clin. Rheumatol 13(3):134–147
El-Kawaly WH, Amer MS, Hamza SA, Arif ER (2016) Fracture risk assessment in geriatric homes in Egypt. Indian J Med Res Pharmaceutical Sci 3(10):4–14
El Miedany Y, Abu-Zaid MH, El Gaafary M et al (2021) Egyptian consensus on treat-totarget approach for osteoporosis: a clinical practice guideline from the Egyptian Academy of bone health and metabolic bone diseases. Egypt Rheumatol Rehabil 48:5
Delmas PD, van de Langerijt L, Watts NB et al (2005) Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 20(4):557–563
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14(12):1028–1034
Chan T, de Lusignan S, Cooper A, Elliott M (2015) Improving Osteoporosis Management in Primary Care: An Audit of the Impact of a Community Based Fracture Liaison Nurse. PLoS One 10(8):e0132146
Dell R (2011) Fracture prevention in Kaiser Permanente Southern California. Osteoporos Int 22 Suppl 3:457–460
International Osteoporosis Foundation. Map of best practice. http://www.capturethefracture.org/map-of-best-practice. (Accessed 21th November 2021)
Akesson K, Marsh D, Mitchell PJ et al (2013) Capture the Fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24(8):2135–2152
Javaid MK, Kyer C, Mitchell PJ et al (2015) Effective secondary fracture prevention: implementation of a global benchmarking of clinical quality using the IOF Capture the Fracture(R) Best Practice Framework tool. Osteoporos Int 26(11):2573–2578
Gittoes N, McLellan AR, Cooper A et al (2019) Effective Secondary Prevention of Fragility Fractures: Clinical Standards for Fracture Liaison Services. National Osteoporosis Society, Camerton https://theros.org.uk/media/1eubz33w/ros-clinical-standards-for-fracture-liaisonservices-august-2019.pdf
Javaid MK, Sami A, Lems W, Mitchell P, Thomas T, Singer A, Speerin R, Fujita M, Pierroz DD, Akesson K, Halbout P, Ferrari S, Cooper C (2020) A patient-level key performance indicator set to measure the effectiveness of fracture liaison services and guide quality improvement: a position paper of the IOF Capture the Fracture Working Group, National Osteoporosis Foundation and Fragility Fracture Network. Osteoporos Int 31(7):1193–1204
Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int 15:767–778
Hoang-Kim A, Schemitsch E, Sale JE, Beaton D, Warmington K, Kulkarni AV, Reeves S (2014) Understanding osteoporosis and fractures: an introduction to the use of qualitative research. Arch Orthop Trauma Surg 134(2):207–217
Vaculik J, Stepan JJ, Dungl P, Majerní M, Alexander Č (2017) Secondary fracture prevention in hip fracture patients requires cooperation from general practitioners. Arch Osteoporos 12(1):49
Harrington JT, Broy SB, Derosa AM, Licata AA, Shewmon DA (2002) Hip fracture patients are not treated for osteoporosis: a call to action. Arthritis Rheum 47:651–654
Osteoporosis Canada (2014) Quality Standards for Fracture Liaison Services in Canada. Osteoporosis Canada, Toronto https://fls.osteoporosis.ca/fls-tools-and-resources/
British Orthopaedic Association, National Osteoporosis Society. BOAST 9: Fracture Liaison Services. London 2014.
International Osteoporosis Foundation. Capture the Fracture® Programme website. http://www.capturethefracture.org/. Accessed 23 November 2021.
Erhan B, Ataker Y (2020) Rehabilitation of Patients With Osteoporotic Fractures. J Clin Densitom 23(4):534–538
Acknowledgements
NA
Funding
NA
Author information
Authors and Affiliations
Contributions
Both authors contributed to the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors of the manuscript have participated in this work.
Consent for publication
Approved
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gadallah, N., El Miedany, Y. Operative secondary prevention of fragility fractures: national clinical standards for fracture liaison service in Egypt—an initiative by the Egyptian Academy of Bone Health. Egypt Rheumatol Rehabil 49, 11 (2022). https://doi.org/10.1186/s43166-022-00111-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-022-00111-7