Abstract
Background
Nanoplastics (NPs) have emerged as significant environmental pollutants, raising concerns due to their ubiquitous presence and potential adverse effects on human health. The migration and fate of NPs in the environment are subjects of intense study, with human exposure pathways expanding through ingestion, inhalation, and dermal contact.
Body
Studies indicate that NPs can infiltrate the cardiovascular system, potentially causing adverse effects. Mechanistic insights from in vitro and animal studies suggest that oxidative stress, inflammation, apoptosis, and mitochondrial dysfunction contribute to nanoplastic-induced cardiovascular toxicity. Animal models demonstrate altered heart rate, myocardial fibrosis, and dysfunction following NPs exposure, with specific adverse effects observed in cardiac valves and mitochondrial structure. Clinical studies provide further evidence of NPs accumulation in cardiovascular tissues, with implications for cardiovascular pathologies such as atherosclerosis and myocardial infarction. Notably, patients with higher levels of nanoplastics in carotid plaque exhibit an increased risk of adverse cardiovascular outcomes.
Conclusion
However, challenges in studying nanoplastics persist, including methodological limitations, ethical considerations, and the need for standardized detection methods. Addressing these challenges requires interdisciplinary collaboration, innovative research approaches, and robust regulatory measures to mitigate NPs pollution and protect cardiovascular health.
Similar content being viewed by others
Introduction
Microplastics (MPs) are among the newly recognized persistent organic pollutants (POPs), emerging as critical environmental concerns in recent years [1]. Described by Thompson et al. in 2004 as plastic debris less than 5 mm in diameter [2], MPs have dual origins: degradation of larger plastic debris and pre-production pellets used for the already limited size [3]. Environmental factors such as physical processes, chemical weathering, and biological activity can further degrade MPs into even smaller nanoparticles (NPs) ranging from 1 to 1000 nm. Due to their diminutive size, extensive surface area, and high tissue affinity, these NPs are readily ingested by organisms, potentially disrupting various biological processes [4,5,6].
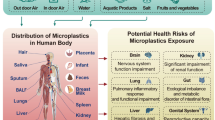
Currently, microplastic (nano)plastics (MNPs) represent a novel form of environmental pollution, garnering considerable research attention. Their migration and ultimate fate in nature are subjects of intense study. Of greater concern is their impact on human health; some studies suggest possible adverse outcomes [7,8,9]. As environmental concentrations of MNPs rise, human exposure pathways expand, with inhalation, ingestion, and dermal penetration identified as primary routes of entry into the body [7]. While a significant portion of current research focuses on the health hazards associated with ingesting NPs from aquatic sources, such as drinking water and seafood [8, 9], the complexity of human exposure is increasing [10]. For example, NPs have been found in lakes, rivers, and even treated drinking water [10, 11], potentially leading to human ingestion post-consumption [12]. Moreover, marine organisms like fish, shellfish, and crustaceans have been shown to accumulate MNPs, thus entering the human diet upon consumption [13, 14]. Notably, MNPs have been detected in seemingly unrelated food items such as table salt and beer [15], indicating their potential presence in a variety of foods.
Inhalation serves as another exposure route for NPs, originating from various sources like clothing fibers, building materials, 3D printing, tire wear, waste incineration, and urban dust [16]. Their small size allows easy airborne transport, with oceanic microplastics also contributing to atmospheric dispersion [17, 18]. COVID-19 mask usage has intensified respiratory exposure [19]. While ingestion is primary, dermal absorption is notable [20, 21]. Research confirms MNPs' translocation from the digestive tract and lungs to various organs, including the heart [7]. These multiple pathways underscore the significant health risks, demanding further investigation.
Cardiovascular disease (CVD) remains a leading global health concern, with air pollution being a significant contributing factor. Investigations indicate that air particulate matter (PM) negatively impacts cardiovascular activity, leading to vascular dysfunction, hypertension, and myocardial infarction [22, 23]. Oxidative stress induced by PM exposure is believed to play a key role in this process [22,23,24]. Emerging evidence suggests that NPs, as a novel environmental pollutant, also pose a threat to cardiovascular health [23]. A growing body of research indicates the heart as a potential target site for NP accumulation, potentially establishing it as a new cardiovascular risk factor [25]. Studies using mammalian models have demonstrated that nanoparticle exposure can adversely affect cardiac function [7]. The proposed mechanism involves interactions between NPs and ion channels within cardiac muscle cells (cardiomyocytes), ultimately disrupting their function [7]. While the potential for NPs to impact the cardiovascular system is gaining recognition, current research primarily focuses on elucidating the underlying mechanisms. The broader impacts of NP exposure on various aspects of cardiovascular health remain largely unexplored. This study aims to contribute to this critical area by providing new insights into the cardiotoxic potential of NPs.
Methodology
Literature search strategy
A literature search was conducted to identify relevant studies examining the cardiovascular hazards of nanoplastics (Table 1). Electronic databases including PubMed/MEDLINE, Scopus, Web of Science, and Google Scholar were searched using relevant keywords and Medical Subject Headings (MeSH) terms. Key search terms included “nanoplastics,” “microplastics,” “cardiovascular effects,” “heart disease,” and related variations. Boolean operators (AND, OR) were utilized to refine search queries and broaden the scope of relevant articles. The search was limited to articles published in English up to February 2024 to ensure the currency of the review.
Study selection criteria
Studies were included in the review if they met the following inclusion criteria:
-
Published in peer-reviewed journals.
-
Investigated the cardiovascular effects of nanoplastics.
-
Provided relevant data or insights into the mechanisms underlying nanoplastic-induced cardiovascular toxicity.
-
Included experimental studies and observational studies.
The exclusion criteria were as follows:
-
Non-English language articles.
-
Studies focusing solely on other environmental pollutants without specific mention of nanoplastics.
-
Studies lacking relevance to cardiovascular health or lacking mechanistic insights into nanoplastic toxicity.
-
Reviews, metanalyses, and conference papers.
Data extraction and synthesis
Two reviewers independently performed data extraction to ensure accuracy and reliability. Any discrepancies between reviewers were resolved through discussion and consensus. Following data extraction, a narrative synthesis approach was employed to summarize the findings of the included studies. Results were organized thematically based on the cardiovascular outcome assessed (e.g., cardiac function, vascular health) and the experimental model utilized (in vitro, in vivo). Mechanistic insights into nanoplastic-induced cardiovascular toxicity were synthesized to provide a comprehensive overview of the current understanding in the field.
Nanoplastics and cardiovascular system
Despite a substantial body of animal-based studies validating the adverse health effects of NPs, there remains to be more data on their impacts on various human organ systems [26] (Fig. 1). While many of the published studies have explored the forms of MPs, their routes of entry into human systems, and their toxicity, significant gaps persist in understanding the mechanisms underlying these NPs’ toxicity [27, 28]. NPs can gain entry into the human body through several means, including ingestion, inhalation, and skin contact [29]. Evidence of NPs in human stool validates their entry through diet, drinking water, and food packaging [30]. Moreover, NPs have been detected in both indoor and outdoor particulates, such as synthetic textiles, construction materials, and abrasions of plastic materials, supporting their entry through inhalation [31]. While the skin membrane typically presents a barrier to MP and NP penetration, studies suggest that NPs can penetrate through wounds, sweat glands, or hair follicles [32].
Following absorption into the body, NPs and NPs may bind to cells and biological molecules, leading to the formation of coronated nanoplastic particles for absorption [33]. Endocytic pathways, including phagocytosis, micropinocytosis, as well as clathrin- and caveolae-mediated endocytosis, have been identified as crucial for cellular uptake of nanoparticles [34]. NPs are hypothesized to enter the gastrointestinal system through lymphatic tissue and infiltrate the microfold (M) cells in the Peyer’s patches [35]. In the pulmonary route, NPs can permeate the thin alveolar tissue barrier and disperse throughout the body. In the dermal route, NPs leverage the weakening effects of radiation on the skin and the ingredients in body lotions to penetrate the skin barrier [36].
Upon entry into the body, MNPs and NPs can invade the heart and blood vessels, potentially causing adverse effects [37]. While the pathophysiology of nanoplastic-induced cardiovascular toxicity is not fully understood, in vitro studies suggest oxidative stress, inflammation, and apoptosis in vascular cells, while animal models indicate altered heart rate, myocardial fibrosis, and dysfunction [38, 39]. Exposure to PS-MPs has been linked to atrioventricular valve defects, cellular inflammation, mitochondrial lesions, and myocardial fiber destruction [1]. Nanoplastics can pass through the rodent placenta and directly harm the fetal heart, bypassing the protective barrier. Additionally, exposure of human blastocysts to polystyrene nanoplastics during early development can hinder the formation of atrioventricular heart valves in newborns [7].
In vitro studies have shed light on the cellular responses to nanoplastic exposure within the cardiovascular system [40, 41]. One of the primary mechanisms implicated in nanoplastic-induced cardiovascular toxicity is oxidative stress, wherein excessive production of reactive oxygen species (ROS) overwhelms the antioxidant defense mechanisms of vascular cells [40]. This imbalance leads to oxidative damage to cellular components, including lipids, proteins, and DNA, ultimately contributing to cellular dysfunction and death [38]. Additionally, NPs exposure has been associated with inflammation within the vascular endothelium [41]. Inflammatory mediators, such as cytokines and chemokines, are upregulated in response to nanoplastic exposure, triggering an inflammatory cascade that can disrupt normal vascular homeostasis [29]. Persistent inflammation within the blood vessels can contribute to endothelial dysfunction, impaired vasodilation, and the development of atherosclerosis [30]. Moreover, studies have demonstrated that NPs exposure can induce apoptosis, or programmed cell death, in vascular cells [32]. This cellular response is mediated by various signaling pathways activated in response to nanoplastic-induced oxidative stress and inflammation [35]. Apoptosis of vascular cells can compromise the structural integrity of blood vessels, impairing their function and predisposing to cardiovascular disorders [33]. A study found that patients with carotid artery plaque containing MNPs had a higher risk of experiencing a combined outcome of myocardial infarction, stroke, or death within 34 months of follow-up, compared to those without MNPs in their plaque [33].
Animal studies have provided valuable insights into the systemic effects of NPs exposure on cardiovascular function [21]. These studies have demonstrated altered heart rate, impaired cardiac contractility, and myocardial fibrosis following chronic nanoplastic exposure [28, 42]. Myocardial fibrosis, characterized by excessive deposition of collagen fibers in the heart muscle, can impair cardiac function and contribute to the development of heart failure [36]. Furthermore, exposure to polystyrene microplastics (PS-MPs) has been linked to structural abnormalities in cardiac valves, specifically atrioventricular valve defects [43, 44]. These defects can disrupt normal blood flow within the heart chambers, leading to functional impairments and potentially predisposing to cardiovascular complications [45]. Additionally, animal models have revealed mitochondrial lesions in cardiac cells following nanoplastic exposure. Mitochondrial dysfunction can compromise cellular energy production and contribute to oxidative stress-mediated damage, exacerbating cardiovascular pathology [46]. Reviewing available epidemiological studies linking particulate matter exposure to specific cardiovascular outcomes (morbidity, mortality, or hospitalizations), the evidence strongly supports a causal relationship with ischemic heart disease. For heart failure and ischemic stroke, the evidence is moderate and growing. The link to peripheral vascular disease and cardiac arrhythmia/arrest is currently modest or inconsistent [22].
While the precise molecular mechanisms underlying nanoplastic-induced cardiovascular toxicity require further elucidation, likely, a complex interplay of oxidative stress, inflammation, apoptosis, and mitochondrial dysfunction contributes to the observed adverse effects [31]. NPs directly interact with vascular cells, triggering intracellular signaling cascades that culminate in cellular dysfunction and tissue damage [33]. Moreover, nanoplastic-induced alterations in systemic inflammation and oxidative stress exacerbate pre-existing cardiovascular risk factors, such as hypertension, dyslipidemia, and diabetes, further predisposing individuals to cardiovascular disease development [46].
Current evidence
Preclinical studies
Studies have explored the risks of various NPs and the potential association with cardiovascular events (Table 2). Laboratory-based experimental studies detailing the results of different cardiac manifestations from cardiac fibrosis in rats exposed to polystyrene, thrombosis, and impairment of myocardial contractility (Table 3). In 2020, an experimental study was carried out by Li Zekang et al. [1] to ascertain the effect of polystyrene NPs causing fibrosis of the cardiac tissue by activating the Wnt/β-catenin signaling pathway and promoting cardiomyocyte apoptosis in 32 male Wister rats. They found out that among the exposure group, oxidative stress was significantly increased compared to the control. There was also evidence of collagen fiber expression; this was assessed by integrated optical density of collagen under Masson’s trichrome staining and Sirius red staining. Among the exposure group, this was statistically significant compared to the control group. Additionally, fibronectin was elevated, and Troponin I and CK-MB were increased in rats exposed to microplastics.
In the following year, Sun et al. [47] attempted to examine the level of cardiovascular toxicity among developing zebrafish embryos exposed to polyethylene nanoplastics. 30 zebrafish embryos in each experimental group were used and pericardial toxicity, hemodynamic changes, thrombosis, ROS generation, and inflammation were examined. The results showed that with treatment with 48 hpf (high-performance films) the group treated with polyethylene, exhibited elevated heart rates averaging 173 beats per minute, although there was no statistically significant difference compared to the control group. Atrial rates and ventricular rates were unchanged in the concentration group, demonstrating that nanoplastics have no effect on the heart rates of zebrafish embryos. Additionally, it did not induce atrioventricular block. Conversely, with increased dose to 96 hpf led to pericardial edema.
NPs have been hypothesized to impair the cardiac contractility of cardiac myocytes. In 2021, Amir et al. [7], performed a laboratory-based experiment in neonatal rats. The study focused on tracing surface charge-dependent nanoplastics in the cytosol of neonatal rats ventricular myocytes (NRVMs) and also to measure the contractile force. The outcome showed that the higher internalization of positively charged nanoplastics during the acute exposure resulted in reduced contractility of the myocardium due to alterations in the intracellular calcium levels. NPs are also known to promote senescence of the endothelial cells of coronary arteries. To assess the possibility of this, Saugat et al. (2022) used a pig’s heart in a laboratory-based experimental study [40]. Nanoplastics were internalized and accumulated in endothelial cells in a time-dependent manner, increasing the Senescence-associated beta-galactosidase activity in a concentration-dependent manner highlighting its capability to cause senescence in coronary arteries. Noteworthily, nanoplastics preferentially affect the endothelium rather than the smooth muscles. The exposure also increased the formation of reactive active species (ROS) leading to oxidative-induced aging of endothelial cells.
In another experimental study, Zhang, Tianyi et al. (2023) sorted to evaluate cardiotoxicity in mice after respiratory exposure to polystyrene nana-plastics [41]. 72 mice were grouped with exposure to low, medium, and high doses. At 4 and 12 weeks of exposure, In-Vivo Imaging System (IVIS) showed an accumulation of nano-plastics in the abdomen and chest of mice. It was noted that after 12 weeks of exposure, the weight of the heart in mice as well as body weight was significantly reduced. Swollen mitochondria, disrupted myocardial fibers, and disappearing cristae were revealed on ultrastructural analysis.
Clinical studies
As the potential implications of nanoplastic exposure on CVS pathologies become a growing concern, numerous studies are presently underway to elucidate the presence and impact of nanoplastics on CVS. Marfella et al. [33] conducted a prospective, multicenter, observational study to collect carotid plaque specimens from patients undergoing carotid endarterectomy and study them for the presence of NPs with the use of pyrolysis–gas chromatography–mass spectrometry, stable isotope analysis, and electron microscopy. Out of the 257 patients, 150 patients (58.4%) exhibited detectable quantities of polyethylene (PE) within the excised carotid plaque while Polyvinyl chloride (PVC) was found in measurable quantities in 31 (12.1%) of these individuals. A positive correlation was found between the presence of NPs and levels of inflammatory markers, suggesting NP’s role in inducing the proinflammatory pathways. Notably, it was observed during the 34 month follow-up period, within the cohort demonstrating evidence of NPs, 30 out of 150 patients (20.0%) experienced nonfatal myocardial infarction, nonfatal stroke, or succumbed to mortality from any cause. Conversely, in the subgroup lacking detectable NPs, 8 out of 107 patients (7.5%) experienced such adverse events. These findings establish that patients with higher levels of NPs in the carotid plaque are at greater risk of developing adverse cardiovascular outcomes.
An ACS cohort study suggested an association between prolonged PM2.5 exposure and increased risk of death from arrhythmias, heart failure, and cardiac arrest (relative risk 1.13, 95% confidence interval 1.05 to 1.21 per 10 μg/m3), though the effect was weaker than for ischemic heart disease mortality [22].
Another study conducted by Yang et al. [45] focused on the detection of NPs within human cardiac tissues and adjacent structures. The study involved the collection of five distinct types of normal tissue samples from patients undergoing various cardiac surgical procedures. These tissue types comprised pericardium, epicardial adipose tissue (EAT), pericardial adipose tissue (PAT), myocardium, and the left atrial appendage (LAA). NPs were detected in all five types of samples, ranging from 20 to 469 μm in diameter. However, particles smaller than 20 μm could not be identified due to limitations in the methods used.
Nine different types of MPs were found in the tissue samples, with the most common being polyethylene terephthalate (PET) constituting 77% and polyurethane (PU) making up 12%, accounting for approximately 90% of the total MPs detected. PE was present in all tissue types, although it comprised only 1% of the total MP count. The investigation also extended to the examination of venous blood samples obtained prior to and following surgical procedures. Notably, NPs were detected in all blood samples, with sizes ranging from 20 to 184 μm. Concerningly, alterations in the composition of NPs were noted between pre- and post-surgery blood samples. These findings suggest the possibility of the introduction of NPs into the bloodstream during the invasive medical procedures and surgery.
To study the presence of NPs in the arterial system, Liu et al. [46] collected samples of carotid arteries, coronary arteries, and aorta from patients undergoing vascular surgeries. NPs were found in each of the 17 arterial samples, with concentrations varying between 52.62 and 225.23 μg/g of tissue, and averaging at 118.66 ± 53.87 μg/g of tissue. Mainly four kinds of NPs were found in the arterial samples, of which PET was predominant (73.70%), followed by PA-66 (15.54%), PVC (9.69%), and PE was the least (1.07%). The study also investigated the demographic characteristics of the donors, including factors such as age, body mass index, and blood pressure, along with their daily habits related to plastic use, such as smoking, consumption of bottled water, take-out food, and prepackaged food. Additionally, the ambient air quality of their residence was examined for its potential effect on NPs concentrations in arterial tissues. However, the results of Spearman’s correlation analysis indicated no significant correlation between these factors and microplastic concentrations within arterial tissues.
Current challenges in studying nanoplastics
Studying NPs presents a multifaceted challenge that demands meticulous attention and innovative solutions [43, 44, 48]. With plastic production surging to unprecedented levels, concerns regarding environmental contamination and potential health risks have escalated proportionally [43, 48]. A primary obstacle in studying NPs lies in their interactions with biological systems and their diverse routes of exposure [43, 48]. While efforts have focused on identifying their presence in organs like the intestine and placenta, direct in vivo evidence remains limited [43, 48]. Moreover, the methods used for detection, such as the Laserdirect infrared (LDIR) chemical imaging system, may underestimate their prevalence, necessitating the development of more sensitive techniques [43, 48]. Additionally, correlating exposure to health outcomes poses challenges due to limited sample sizes and the absence of robust epidemiological data [43, 48].
Methodological limitations further hinder accurate detection and characterization of NPs [43, 44, 48]. Techniques like pyrolysis–gas chromatography–mass spectrometry have been employed, but inconsistencies in results and limitations in distinguishing between different types of plastics remain [44, 48]. Moreover, understanding the sources and pathways of these particles in the human body requires longitudinal studies and interdisciplinary collaborations [44, 48]. The complexity of the research is compounded by ethical considerations surrounding human exposure to microplastics and the translation of findings from animal models [46]. Addressing these challenges necessitates collaborative efforts to standardize methodologies, prioritize funding, and develop innovative research approaches [46]. Only through concerted action can we unravel the intricate interplay between nanoplastics, microplastics, and human health [46].
The escalating production of plastics, reaching a staggering 390 million tons in 2021 from 1.5 million tons in 1950, underscores the urgency for robust regulatory measures [2]. Despite efforts, recycling rates in Europe remain low, with only 34.6% recycled in 2020, posing significant ecological risks [3]. Examining the effectiveness of current regulatory frameworks reveals limitations in addressing the proliferation of NPs [45]. While regulations exist, their enforcement and efficacy in curbing plastic pollution remain questionable [45], compounded by the complex nature of NP pollution and its transboundary transport [45].
Advancements in analytical techniques, like laser direct infrared (LDIR) chemical imaging systems, offer promise in detecting NPs in human tissues [22]. However, current regulatory frameworks have yet to adapt to incorporate such innovative methodologies [25], highlighting the critical need to update regulations to encompass emerging technologies [36]. The identification of NPs in the human cardiovascular system underscores the urgency of enhancing regulatory measures [28], especially considering the diverse chemical composition of NPs and their potential health implications [31].
Global regulatory frameworks governing plastic production and disposal vary, with fragmented approaches to addressing the challenges posed by MPs [45]. While some jurisdictions have implemented bans or restrictions on single-use plastics, regulation of nanoplastics remains underexplored [33]. Existing measures primarily focus on macroplastics and microplastics, overlooking the unique hazards associated with NPs [33], exacerbated by the lack of standardized detection methods [33]. Coordinated international efforts are necessary to develop comprehensive regulatory frameworks targeting NPs [33], emphasizing the need for adaptive and proactive approaches [25].
Despite efforts to mitigate macroplastic pollution, limited attention is directed towards NPs specifically [46]. Regulatory measures, such as bans on single-use plastics and initiatives promoting waste management, represent crucial steps [46]. However, challenges in detecting, quantifying, and characterizing nanoplastics hinder the effectiveness of these measures [46]. Standardized methodologies for NPs detection are lacking, complicating risk assessment and management strategies, showing the need for enhanced regulatory capacity and interdisciplinary collaboration [46].
Conclusion and future directions
Studies into NPs research show the interplay between environmental pollutants and human health, particularly cardiovascular well-being. From their initial origins as environmental contaminants to their pathways of exposure and subsequent cardiovascular effects, NPs represent a multifaceted challenge demanding comprehensive investigation and proactive measures. Experimental studies utilizing animal models and clinical observations in human subjects have provided evidence of the cardiovascular risks associated with NPs exposure, ranging from altered heart rate and myocardial fibrosis to structural abnormalities in cardiac valves and endothelial dysfunction. Moreover, the presence of NPs within human cardiovascular tissues, from the arterial system to cardiac tissues and adjacent structures, underscores their pervasive impact on human health. Despite significant progress, numerous challenges persist in studying NPs and addressing their implications for cardiovascular health. Methodological limitations, ethical considerations, and gaps in regulatory frameworks pose substantial hurdles to advancing our understanding and implementing effective mitigation strategies. Moreover, the escalating production and inadequate management of plastics shows the urgent need for robust regulatory measures and interdisciplinary collaborations to safeguard both environmental and human health.
Moving forward, concerted efforts are needed to standardize methodologies, prioritize funding, and develop innovative research approaches to unravel the interplay between NPs and cardiovascular health. Enhancing regulatory frameworks, promoting sustainable plastic management practices, and fostering global cooperation are essential steps toward mitigating the cardiovascular risks posed by NPs.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- MPs:
-
Microplastics
- NPs:
-
Nanoparticles
- MNPs:
-
Microplastic nanoparticles
- POPs:
-
Persistent organic pollutants
- CVD:
-
Cardiovascular disease
- PM:
-
Particulate matter
- ROS:
-
Reactive oxygen species
- PS-MPs:
-
Polystyrene microplastics
- MeSH:
-
Medical Subject Headings
- IVIS:
-
In-Vivo Imaging System
- NRVMs:
-
Neonatal rats ventricular myocytes
- PET:
-
Polyethylene terephthalate
- PU:
-
Polyurethane
- PA:
-
Polyamide
- PVC:
-
Polyvinyl chloride
- PE:
-
Polyethylene
- SEM:
-
Scanning electron microscopy
- LDIR:
-
Laserdirect infrared
- EAT:
-
Epicardial adipose tissue
- PAT:
-
Pericardial adipose tissue
- LAA:
-
Left atrial appendage
References
Li Z, Zhu S, Liu Q, Wei J, Jin Y, Wang X, Zhang L (2020) Polystyrene microplastics cause cardiac fibrosis by activating Wnt/β-catenin signaling pathway and promoting cardiomyocyte apoptosis in rats. Environ Pollut 265:115025. https://doi.org/10.1016/j.envpol.2020.115025
Thompson RC, Olsen Y, Mitchell R, Davis A, Rowland S, John A, Mcgonigle D, Russell A (2004) Lost at sea: where is all the plastic? Science 304:838. https://doi.org/10.1126/science.1094559
Cole M, Lindeque P, Halsband C, Galloway TS (2011) Microplastics as contaminants in the marine environment: a review. Mar Pollut Bull 62:2588–2597. https://doi.org/10.1016/j.marpolbul.2011.09.025
Forte M, Iachetta G, Tussellino M, Carotenuto R, Prisco M, De Falco M, Laforgia V, Valiante S (2016) Polystyrene nanoparticles internalization in human gastric adenocarcinoma cells. Toxicol In Vitro 31:126–136. https://doi.org/10.1016/j.tiv.2015.11.006
Song YK, Hong SH, Jang M, Han GM, Jung SW, Shim WJ (2017) Combined effects of UV exposure duration and mechanical abrasion on microplastic fragmentation by polymer type. Environ Sci Technol 51:4368–4376. https://doi.org/10.1021/acs.est.6b06155
Xu M, Halimu G, Zhang Q, Song Y, Fu X, Li Y, Li Y, Zhang H (2019) Internalization and toxicity: a preliminary study of effects of nanoplastic particles on human lung epithelial cell. Sci Total Environ 694:133794. https://doi.org/10.1016/j.scitotenv.2019.133794
Roshanzadeh A, Oyunbaatar NE, Ganjbakhsh SE, Park S, Kim DS, Kanade PP, Lee S, Lee DW, Kim ES (2021) Exposure to nanoplastics impairs collective contractility of neonatal cardiomyocytes under electrical synchronization. Biomaterials 278:121175. https://doi.org/10.1016/j.biomaterials.2021.121175
Xu S, Ma J, Ji R, Pan K, Miao AJ (2020) Microplastics in aquatic environments: occurrence, accumulation, and biological effects. Sci Total Environ 703:134699. https://doi.org/10.1016/j.scitotenv.2019.134699
Rahman MN, Shozib SH, Akter MY, Islam ARMT, Islam MS, Sohel MS, Kamaraj C, Rakib MRJ, Idris AM, Sarker A, Malafaia G (2023) Microplastic as an invisible threat to the coral reefs: sources, toxicity mechanisms, policy intervention, and the way forward. J Hazard Mater 454:131522. https://doi.org/10.1016/j.jhazmat.2023.131522
Zhang K, Su J, Xiong X, Wu X, Wu C, Liu J (2016) Microplastic pollution of lakeshore sediments from remote lakes in Tibet Plateau, China. Environ Pollut 219:450–455. https://doi.org/10.1016/j.envpol.2016.05.048
Pivokonsky M, Cermakova L, Novotna K, Peer P, Cajthaml T, Janda V (2018) Occurrence of microplastics in raw and treated drinking water. Sci Total Environ 643:1644–1651. https://doi.org/10.1016/j.scitotenv.2018.08.102
Li J, Liu H, Paul Chen J (2018) Microplastics in freshwater systems: A review on occurrence, environmental effects, and methods for microplastics detection. Water Res 137:362–374. https://doi.org/10.1016/j.watres.2017.12.056
Eerkes-Medrano D, Thompson RC, Aldridge DC (2015) Microplastics in freshwater systems: a review of the emerging threats, identification of knowledge gaps and prioritisation of research needs. Water Res 75:63–82. https://doi.org/10.1016/j.watres.2015.02.012
Güven O, Gökdağ K, Jovanović B, Kıdeyş AE (2017) Microplastic litter composition of the Turkish territorial waters of the Mediterranean Sea, and its occurrence in the gastrointestinal tract of fish. Environ Pollut 223:286–294. https://doi.org/10.1016/j.envpol.2017.01.025
Waring RH, Harris RM, Mitchell SC (2018) Plastic contamination of the food chain: a threat to human health? Maturitas 115:64–68. https://doi.org/10.1016/j.maturitas.2018.06.010
Allen S, Allen D, Baladima F, Phoenix VR, Thomas JL, Le Roux G, Sonke JE (2021) Evidence of free tropospheric and long-range transport of microplastic at Pic du Midi Observatory. Nat Commun 12:7242. https://doi.org/10.1038/s41467-021-27454-7
Shiu RF, Chen LY, Lee HJ, Gong GC, Lee C (2022) New insights into the role of marine plastic-gels in microplastic transfer from water to the atmosphere via bubble bursting. Water Res 222:118856. https://doi.org/10.1016/j.watres.2022.118856
Lindeque PK, Cole M, Coppock RL, Lewis CN, Miller RZ, Watts AJR, Wilson-McNeal A, Wright SL, Galloway TS (2020) Are we underestimating microplastic abundance in the marine environment? A comparison of microplastic capture with nets of different mesh-size. Environ Pollut 265(Pt A):114721. https://doi.org/10.1016/j.envpol.2020.114721
Yang S, Cheng Y, Liu T, Huang S, Yin L, Pu Y, Liang G (2022) Impact of waste of COVID-19 protective equipment on the environment, animals and human health: a review. Environ Chem Lett 20(5):2951–2970. https://doi.org/10.1007/s10311-022-01462-5
Chang X, Xue Y, Li J, Zou L, Tang M (2020) Potential health impact of environmental micro- and nanoplastics pollution. J Appl Toxicol 40(1):4–15. https://doi.org/10.1002/jat.3915
Prata JC, da Costa JP, Lopes I, Duarte AC, Rocha-Santos T (2020) Environmental exposure to microplastics: an overview on possible human health effects. Sci Total Environ 702:134455. https://doi.org/10.1016/j.scitotenv.2019.134455
Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC Jr, Whitsel L, Kaufman JD; American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism (2010) Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 121(21):2331-78. https://doi.org/10.1161/CIR.0b013e3181dbece1.
Miller MR (2022) The cardiovascular effects of air pollution: prevention and reversal by pharmacological agents. Pharmacol Ther 232:107996. https://doi.org/10.1016/j.pharmthera.2021.107996
Kelly FJ, Fussell JC (2017) Role of oxidative stress in cardiovascular disease outcomes following exposure to ambient air pollution. Free Radic Biol Med 110:345–367. https://doi.org/10.1016/j.freeradbiomed.2017.06.019
Lett Z, Hall A, Skidmore S, Alves NJ (2021) Environmental microplastic and nanoplastic: Exposure routes and effects on coagulation and the cardiovascular system. Environ Pollut 291:118190. https://doi.org/10.1016/j.envpol.2021.118190
Ali N, Katsouli J, Marczylo EL, Gant TW, Wright S, Bernardino de la Serna J (2024) The potential impacts of micro-and-nano plastics on various organ systems in humans. EBioMedicine 99:104901. https://doi.org/10.1016/j.ebiom.2023.104901
Yee MS, Hii LW, Looi CK, Lim WM, Wong SF, Kok YY, Tan BK, Wong CY, Leong CO (2021) Impact of microplastics and nanoplastics on human health. Nanomaterials (Basel) 11:496. https://doi.org/10.3390/nano11020496
Wikipedia contributors (2024) Microplastics effects on human health. In: Wikipedia, The Free Encyclopedia. Available via DIALOG. https://en.wikipedia.org/w/index.php?title=Microplastics_effects_on_human_health&oldid=1225829120. Accessed 1 June 2024.
Enyoh CE, Devi A, Kadono H, Wang Q (2023) The plastic within: microplastics invading human organs and bodily fluids systems. Environments 194:1–18. https://doi.org/10.3390/environments10110194
Amato-lourenço LF, Galvão S, De Weger LA, Hiemstra PS (2020) Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. Sci Total Environ 749:1–8. https://doi.org/10.1016/j.scitotenv.2020.141676
Cheng W, Li X, Zhou Y, Yu H, Xie Y, Guo H, et al. (2022) Corrigendum to “Polystyrene microplastics induce hepatotoxicity and disrupt lipid metabolism in the liver organoids” [Sci. Total Environ. 806 [2022] 150328][S004896972105405X][https://doi.org/10.1016/j.scitotenv.2021.150328]. Sci Total Environ 851:158139. https://doi.org/10.1016/j.scitotenv.2022.158139.
Hua T, Kiran S, Li Y, Sang QA (2022) Microplastics exposure affects neural development of human pluripotent stem cell-derived cortical spheroids. J Hazard Mater 435:128884. https://doi.org/10.1016/j.jhazmat.2022.128884
Marfella R, Prattichizzo F, Sardu C, Fulgenzi G, Graciotti L, Spadoni T, D’Onofrio N et al (2024) Microplastics and nanoplastics in atheromas and cardiovascular events. N Engl J Med 390:900–910. https://doi.org/10.1056/NEJMoa2309822
Bojic S, Falco MM, Stojkovic P, Ljujic B, Gazdic Jankovic M, Armstrong L, Markovic N, Dopazo J et al (2020) Platform to study intracellular polystyrene nanoplastic pollution and clinical outcomes. Stem Cells 38:1321–1325. https://doi.org/10.1002/stem.3244
Zhang Y, Yin K, Wang D, Wang Y, Lu H, Zhao H, Xing M (2022) Polystyrene microplastics-induced cardiotoxicity in chickens via the ROS-driven NF-κB-NLRP3-GSDMD and AMPK-PGC-1α axes. Sci Total Environ 840:156727. https://doi.org/10.1016/j.scitotenv.2022.156727
Wei J, Wang X, Liu Q, Zhou N, Zhu S, Li Z, Li X, Yao J, Zhang L (2021) The impact of polystyrene microplastics on cardiomyocytes pyroptosis through NLRP3/Caspase-1 signaling pathway and oxidative stress in Wistar rats. Environ Toxicol 36:935–944. https://doi.org/10.1002/tox.23095
Barshtein G, Arbell D, Yedgar S (2011) Hemolytic effect of polymeric nanoparticles: role of albumin. IEEE Trans Nanobiosci 10:259–261. https://doi.org/10.1109/TNB.2011.2175745
Lee SE, Yoon HK, Kim DY, Jeong TS, Park YS (2024) An Emerging Role of Micro- and Nanoplastics in Vascular Diseases. Life (Basel) 14:255. https://doi.org/10.3390/life14020255
Persiani E, Cecchettini A, Ceccherini E, Gisone I, Morales MA, Vozzi F (2023) Microplastics: a matter of the heart (and vascular system). Biomedicines 11:264. https://doi.org/10.3390/biomedicines11020264
Shiwakoti S, Ko JY, Gong D, Dhakal B, Lee JH, Adhikari R, Gwak Y, Park SH, Jun Choi I, Schini-Kerth VB, Kang KW, Oak MH (2022) Effects of polystyrene nanoplastics on endothelium senescence and its underlying mechanism. Environ Int 164:107248. https://doi.org/10.1016/j.envint.2022.107248
Zhang T, Yang S, Ge Y, Wan X, Zhu Y, Yang F, Li J, Gong S, Cheng Y, Hu C, Chen Z, Yin L, Pu Y, Liang G (2023) Multi-dimensional evaluation of cardiotoxicity in mice following respiratory exposure to polystyrene nanoplastics. Part Fibre Toxicol 20:46. https://doi.org/10.1186/s12989-023-00557-3
Paul-Pont I, Tallec K, Gonzalez-Fernandez C, Lambert C, Vincent D, Mazurais D, Zambonino-Infante JL et al (2018) Constraints and priorities for conducting experimental exposures of marine organisms to microplastics. Front Mar Sci 5:252. https://doi.org/10.3389/fmars.2018.00252
Li Q, Yan J, Li Y, Liu Y, Andom O, Li Z (2024) Microplastics alter cadmium accumulation in different soil-plant systems: Revealing the crucial roles of soil bacteria and metabolism. J Hazard Mater 474:134768. https://doi.org/10.1016/j.jhazmat.2024.134768
Liu S, Li Y, Wang F, Gu X, Li Y, Liu Q, Li L, Bai F (2024) Temporal and spatial variation of microplastics in the urban rivers of Harbin. Sci Total Environ 910:168373. https://doi.org/10.1016/j.scitotenv.2023.168373
Yang Y, Xie E, Du Z, Peng Z, Han Z, Li L, Zhao R, Qin Y, Xue M, Li F, Hua K, Yang X (2023) Detection of Various Microplastics in Patients Undergoing Cardiac Surgery. Environ Sci Technol 57:10911–10918. https://doi.org/10.1021/acs.est.2c07179
Liu S, Wang C, Yang Y, Du Z, Li L, Zhang M, Ni S, Yue Z, Yang K, Wang Y, Li X, Yang Y, Qin Y, Li J, Yang Y, Zhang M (2024) Microplastics in three types of human arteries detected by pyrolysis-gas chromatography/mass spectrometry (Py-GC/MS). J Hazard Mater 5(469):133855
Sun M, Ding R, Ma Y, Sun Q, Ren X, Sun Z, Duan J (2021) Cardiovascular toxicity assessment of polyethylene nanoplastics on developing zebrafish embryos. Chemosphere 282:131124. https://doi.org/10.1016/j.chemosphere.2021.131124
Dhakal B, Shiwakoti S, Park EY, et al (2023) SGLT2 inhibition ameliorates nano plastics-induced premature endothelial senescence and dysfunction. Sci Rep 13(1):6256. Published 2023 Apr 17. https://doi.org/10.1038/s41598-023-33086-2
Acknowledgements
None.
Funding
No funding was received for this study
Author information
Authors and Affiliations
Contributions
GO conceptualized the study; all authors were involved in the literature review; GO and NA extracted the data from the reviewed studies; all authors wrote the final and first drafts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Olatunji, G., Kokori, E., Ogieuhi, I.J. et al. Nanoplastics as emerging cardiovascular hazards: a narrative review of current evidence. Egypt J Intern Med 36, 62 (2024). https://doi.org/10.1186/s43162-024-00329-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-024-00329-1