Abstract
Background
Caesarean scar disorders (CSDi) are an increasingly recognized consequence of caesarean sections, which can present with secondary infertility. Currently, there is limited data on the management of CSDi, and the subsequent fertility and pregnancy outcomes. Our aim was to examine different treatment methods and outcomes in a cohort of women with secondary infertility.
Study design
This study involved a retrospective case series for patients (n = 26) diagnosed with and treated for a CSDi between 2008 and 2019 at a tertiary care centre in British Columbia, Canada, by one of three gynecologists with expertise in CSDi repair. Surgical repair was performed via laparoscopy for residual myometrial thickness (RMT) < 3.0 mm, and via hysteroscopy otherwise. Postoperative pregnancy rates and reproductive outcomes are reported. This study also included a search of the literature to gain an overview of the indications, outcomes, advantages, disadvantages, and risks associated with four surgical approaches (hysteroscopic, laparoscopic, vaginal, abdominal) used in the management of CSDi. A Medline and manual searches of referenced articles were conducted for this purpose.
Results
Twenty-six patients with CSDi were diagnosed with secondary infertility (mean age = 36.4 years) during the study period. Twenty of these patients underwent surgical management, with 12 receiving hysteroscopic resection or ablation, and 8 receiving laparoscopic repair. Six patients had no treatment or are still awaiting management at this time. Postoperatively, 11/20 patients (55%) were able to successfully conceive at least once. 8/11 patients were from the hysteroscopy group (66% pregnancy rate) and 10/11 pregnancies resulted in live births at term. In the laparoscopy group, there were 3 pregnancies (37.5% pregnancy rate), including 2 term live births, and 1 preterm live birth at 26 weeks. With respect to our review of the literature, a total of 49 articles were included in our final review of surgical techniques used in the management of CSDi.
Conclusions
This study suggests that surgical repair can improve pregnancy rates in patients with secondary infertility in the context of a confirmed CSDi.
Similar content being viewed by others
Background
The global rate of caesarean sections increased from 7 to 21% between the years 1990 and 2023, which has led to increasing importance in awareness of the complications and sequelae of the procedure [1]. While some complications are well known, others have only more recently become apparent and still require further study to appreciate their clinical significance and guide best management. Such is the case for caesarean scar disorders (CSDi), which has also been referred to as isthmocele niche, uterine scar insufficiency, or scar dehiscence [2,3,4,5].
CSDi have been variably defined until recently, but most reports described a discontinuity or triangular hypoechoic defect in the myometrium of the anterior uterine wall at the site of previous hysterotomy, typically visualized via transvaginal ultrasound (TVUS) or saline contrast sonohysterography (SCSHG) [2, 6]. However, through a recently conducted modified Delphi procedure, many experts agreed that CSDi should be defined as an “indentation at the site of the CS scar with a depth of at least 2 mm” [7, 8]. Most experts felt that gel or saline infusion provides additional value to the diagnosis in the absence of pre-existing intrauterine fluid [7]. The definition of caesarian scar disorder is classified as the above sonographic finding with one primary symptom (postmenstrual spotting, painful uterine bleeding, difficult catheter insertion in embryo transfer, unexplained infertility with intrauterine fluid) or two secondary symptoms (dyspareunia, abnormal vaginal discharge, avoiding sexual intercourse, chronic pelvic pain, secondary unexplained infertility) [8]. The classification of CSDi severity also varies between studies and imaging modalities but is generally based on degree of myometrial thinning [9]. Important parameters in their characterization include the niche length, depth, and width, the residual myometrial thickness, and adjacent myometrial thickness [10]. Depending on the type of imaging, the prevalence of CSDi has been estimated to be between 24–70% and 56–84% in women with at least 1 prior C-section when imaged by TVUS and SCSHG, respectively [9, 11]. Incidence has been estimated at approximately 15% using TVUS following caesarean section [12].
Several risk factors for the development of CSDi have been proposed, including multiple C-sections, a retroflexed uterus, and failure to identify previous C-section scars during repeat C-sections, elevated body mass index (BMI), gestational diabetes, pre-eclampsia, smoking, and elevated maternal age [10, 13]. Duration of labor prior to C-section, cervical diameter, stage of the presenting part, and lower C-section hysterotomy are also suggested predisposing factors, with cervical dilation > 5 cm related to larger defects [14]. CSDi have been associated with a number of symptoms, including abnormal uterine bleeding (AUB), dysmenorrhea, dyspareunia, secondary infertility, and caesarean scar ectopic pregnancy, although some patients are asymptomatic [2, 9, 15,16,17,18]. Even in patients who are free of symptoms, CSDi confer increased risk of complications during gynecologic procedures [19, 20].
The symptoms of a CSDi have been attributed to the accumulation of intracavitary blood, either through menstrual blood accumulation or capillary bleeding at the site of the scar [9, 21, 22]. Patients with confirmed CSDi were found to be three times as likely to experience abnormal vaginal bleeding compared to those without [23]. It is hypothesized that abnormal bleeding also contributes to secondary infertility, as blood may be embryotoxic, reduce endometrial receptivity to implantation, provide a physical barrier to implantation due to excessive fluid, hinder sperm motility by altering cervical mucus, or a combination of the above [9, 21, 22, 24].
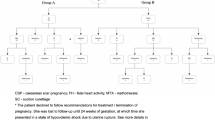
The proposed mechanisms of CSDi-associated symptoms suggest that surgical removal of the defect would lead to resolution of gynecologic symptoms and infertility, and as such is an important component of management. There are four primary surgical techniques used in the treatment of a CSDi (Table 1): hysteroscopic repair (Fig. 1), laparoscopic repair (Fig. 2), vaginal repair, and abdominal repair. Figure 3 demonstrates a CSDi on ultrasound pre- and post-surgical repair. There remains no published consensus on the indications for the use hysteroscopic vs laparoscopic vs vaginal repair vs abdominal repair. Some treatment algorithms have suggested that those with residual myometrial thickness below 3 mm or with multifocal disease are more suited to laparoscopic repairs versus other approaches [10]. However, features of the CSDi (such as residual myometrial thickness or presence of fluid), patients’ primary symptomatic concern, future goals with respect to fertility, local resources, and/or surgeon preference may be considered when determining an approach. It has been suggested that the ideal patients for surgical repair are those with persistent intrauterine fluid, or in those where in vitro fertilization procedures are impaired by the niche [10].
Hysteroscopic surgical repair of caesarean scar disorder (CSDi). A Identification of the anatomy of the CSDi. B Excision of the cephalad edge of the fibrosis to smoothen the contour between the CSDi and the uterine cavity. The caudad edge of the fibrosis is also excised to smooth the contour between the CSDi and the cervical canal. This process is started midline, then laterally, only on the anterior wall. C, D Further hysteroscopic resection
Laparoscopic surgical repair of caesarean scar disorder (CSDi). A As adhesions are often in the midline, opening and dissection of paravesicular spaces is done. B After dissecting the bladder from the posterior leaf of the broad ligament, the cervix is reached and dissection of the midline towards the funnel part of the uterus is safely completed. The dense fibrotic adhesions are lysed with scissors with or without use of monopolar current. C As the defect is often at the level of the uterine arteries, identification and dissection are completed. This allows for eventual safe coagulation if needed. D The thinnest point of the defect is incised using a monopolar hook and then resected using a hook, cold scissors, or another energy device. E The entire defect, as well as all fibrotic tissue, is removed until the thickness of the myometrium on either side is similar. The removal is carried out circumferentially taking care to remove all abnormal tissue. F The borders of the defect are pre-emptively coagulated and delineated using a monopolar hook. Coagulation marks are placed around the defect allowing for maintenance of orientation, as well as hemostasis. G The border is then incised using the surgeon’s preferred instrument. The uterine probe is advanced and retracted throughout the resection in order to keep the orientation of the cavity and borders of the defect visualized. H Closure of the myometrial defect is done with barbed sutures, interrupted, or running multifilament sutures. An adhesion barrier is then placed. A double layered closure is performed
In this study, we provide further evidence for the utility of surgical intervention in the treatment of CSDi-associated infertility through a review of the literature, and by characterizing a series of patients who have been evaluated and treated for a CSDi at a tertiary centre in Vancouver, Canada, with a specific focus on fertility and reproductive outcomes.
Materials and methods
This study was reviewed and approved by the Institutional Review Board (H19-02324).
This study included a scoping review of the literature to understand the indications, outcomes, advantages, and disadvantages/risks associated with four surgical approaches used in the management of CSDi: hysteroscopy, laparoscopy, vaginal repair, and abdominal repair. Our primary PICO question was, “How are women with secondary infertility due to CSDi who desire fertility restoration impacted after surgical management in terms of their rate subsequent fertility outcomes and intermenstrual bleeding.” A review of Medline and manual searches of referenced articles was conducted. The following MeSH terms and keywords were included: ‘((caesarean section or caesarean section or c-section) adj2 (defect* or wound* or scar* or repair*)).mp.’ OR ‘isthmocele.mp.’ AND ‘exp hysteroscopy/’ OR ‘hysteroscop*.mp.’ OR ‘exp laparoscopy/’ OR ‘laparoscop*.mp.’ OR ‘exp gynecologic surgical procedures/’ OR ‘(vaginal repair or surgical repair or surger* or surgical management).mp.’ OR ‘Laparotomy/’ OR ‘(laparotom* or abdom* repair).mp.’ After articles were identified, articles had both abstract and full text review to ensure they met the following criteria: (1) discussed the treatment of CSDi in terms of fertility outcomes or management of intermenstrual bleeding and (2) discussed at least one of our four identified surgical management approaches—hysteroscopy, laparoscopy, vaginal repair, and abdominal repair. Articles that did not meet these criteria were excluded from analysis. Additional articles identified by reviewing the sources of articles found in the search were included if they met the above criteria.
The retrospective case series investigated reproductive outcomes of all patients who presented with a CSDi and secondary infertility at a tertiary care centre in Vancouver, Canada. Patients were identified through the records of three surgeons who provided surgical management for these patients between 2008 and 2019. CSDi were diagnosed after imaging (ultrasonography, sonohysterogram, or magnetic resonance imaging) revealed isthmoceles 2 mm or more following patient presentation with clinical symptoms of CSDi. These charts were then reviewed in depth, and data was collected on patient and defect characteristics, interventions, and management outcomes. Duration of follow-up was calculated either from time of surgery to time of data collection, or from time of CSDi diagnosis to time of data collection for those patients that declined surgical intervention. The inclusion criterion was a diagnosis of CSDi likely to be contributing to secondary infertility. Patients were excluded if restoration of fertility was not a desired treatment goal, or if they did not have secondary infertility.
Hysteroscopic repair
To perform a hysteroscopic diagnosis and repair of a CSDi, the procedure begins with the sequential dilation of the cervix to accommodate the diameter of the hysteroscope. The hysteroscope was then inserted into the uterine cavity, and the cavity was distended using a hypotonic distention medium. The entire cavity was inspected, and attention was turned to the defect at the anterior lower uterine segment. Depending on surgeon preference, either a hysteroscopic resection of the upper and the lower edge of the fibrosis followed by rollerball cauterization or solely a rollerball cauterization was performed. Hysteroscopic resection involves using a resection loop to excise the fibrotic tissue at the proximal and distal edges of the defect. Once the fibrotic tissue is resected, the rollerball was used to gently cauterize the entire base of the defect and resected tissue.
Laparoscopic repair
The laparoscopic repair surgical approach begins with hysteroscopic visualization of the uterine defect, after dilation of the cervix and distention of the uterine cavity. After entry into the abdomen and placement of the laparoscopic ports, dissection was performed, to safely isolate the lower uterine segment for resection of the defect. Next, with the use of the hysteroscope in the uterine cavity, the defect was visualized using transillumination. The borders were then demarcated and the defect was removed entirely using the monopolar hook. A double layer closure of the uterus was then completed using a barbed suture, ensuring complete myometrial re-approximation.
Results
A total of 494 articles were produced from our search of the Medline database. Our review of the literature included a total of 49 articles which were published between 2005 and 2023 (Table 2), 32 of which were from our original database search, and 17 that were found via a review of referenced articles (Fig. 4).
Selection of sources of evidence using the preferred reporting items for systematic reviews and meta-analyses protocol [64]
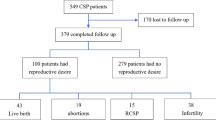
Of the 28 consecutive patients initially identified as having been diagnosed with infertility in our case series, two were excluded as they did not have secondary infertility. The remaining 26 patients were identified as experiencing secondary infertility with a diagnosis of a CSDi and were included in the study. The mean follow-up duration was 33.3 ± 2.7 (mean ± SEM) months with only two patients followed for less than 1 year and one patient (Case 26) lost to follow-up.
Baseline characteristics and surgical technique
The mean age of the included patients was 36.4 ± 0.9 years. Most of the women were asymptomatic apart from secondary infertility, with no other identifiable cause. Prior to their presentation, three of the patients had two prior caesarean sections, while the remainder had only one prior caesarean section. Caesarean scar ectopic pregnancy had previously occurred in 3/26 (12%) of the included patients. The full baseline characteristics of the patients and available data from their operative history are displayed in Table 3. CDI characteristics are displayed in Table 4.
Surgical outcomes
A total of 20 out of the 26 included patients opted for surgical management, with the goal of improving their fertility. A hysteroscopic approach was used for 12 of the 20 patients, in the form of ablation with or without resection of the upper edge of fibrosis. The other eight patients who chose surgical repair underwent laparoscopic repair. The remaining six patients chose to be managed expectantly. Among all 20 surgical procedures, there were no intraoperative complications, and no blood transfusions were required.
Reproductive outcomes
In the patients who underwent hysteroscopy, 8/12 (66%) patients were able to successfully become pregnant at least once after surgery, accounting for 10 pregnancies which all resulted in a live birth at term. The average time to pregnancy for hysteroscopic treatment was 7.0 ± 2.3 months. Postoperative adverse events consisted of new onset of intermenstrual bleeding after surgery in 2/12 (17%) patients, which was not an issue pre-operatively; however, one of these patients still achieved pregnancy 16 months postoperatively.
After laparoscopic resection and repair, 3/8 (37.5%) patients achieved pregnancy. The average time to pregnancy for laparoscopic treatment was 7.7 ± 2.3 months. All three of these pregnancies resulted in a live birth, with two occurring at term and one at 26 weeks gestation following preterm premature rupture of membranes and severe intrauterine growth restriction. One patient had persistent endometrial fluid postoperatively and has not conceived again thus far.
Combining both surgical methods, 11/20 patients (55%) successfully conceived after surgery and had a live born infant. Assisted reproductive treatment (ART) was used by 7/11 (64%) of the patients that achieved pregnancy. The overall intraoperative complication rate was 0/20 (0%), and the overall postoperative complication rate was 2/20 (10%) in the form of new intermenstrual bleeding. The features of these patients and their pregnancies are presented in Table 5. Of the six patients that were managed expectantly, one patient (17%) became pregnant without any treatment (Case 19).
No postoperative abnormal placentation or scar dehiscence in subsequent pregnancies were reported in this sample.
Discussion
As caesarean section rates continue to rise, CSDi are an emerging entity which will likely increase in prevalence and diagnosis. When evaluating patients presenting with infertility and a history of caesarean section, it is important to evaluate for presence of a defect at the caesarean scar site in addition to the routine infertility workup. It thus becomes imperative to be familiar with available management options and their effects on fertility, pregnancy, and rates of live birth.
The simplest diagnostic method available is transvaginal ultrasound. In the absence of endogenous intrauterine fluid, many experts have established that the use of saline/gel infusion to distend the uterine cavity increases sensitivity [7]. Although measurements of the entire defect are important, the key dimensions include the length, depth, and width, as well as the adjacent myometrial thickness and residual myometrial thickness (RMT) [7].
Surgical management of caesarean scar disorder
Hysteroscopic repair
There is agreement that the hysteroscopic approach is limited by RMT [33]; however, specific recommendations vary in the literature. Marotta et al. recommend a RMT > 3 mm [46], whereas Chang et al. note that a RMT ≥ 2 mm can be used as a threshold [28]. Other studies recommend a RMT of > 3.5 mm be used in patients with desire for future fertility versus > 2.5 mm for those without [43]. In contrast, some studies indicate that hysteroscopic repair should only be considered for patients who do not desire future fertility [26, 51]. Other studies cautiously state that a residual myometrium < 3 mm and a desire to maintain fertility should serve as a contraindication to hysteroscopic repair due to the high risk of bladder injury, uterine perforation, and uterine rupture in subsequent pregnancies [32, 65]. Zhu et al. recommend a hysteroscopic approach for patients with a longer pre-operative menstrual duration, as this is correlated with an improved chance of a reduction in menstrual duration post-surgery [63].
The reported outcomes of hysteroscopic repair include the resolution and/or improvement of the [20], with an increase in the residual myometrium thickness [24, 43, 52]. Additionally, resolution and/or improvement of symptoms of abnormal uterine bleeding [20, 25, 27, 31, 50, 53, 54, 62, 66, 67] and pain [20, 27, 53, 66] are reported, as is a reduction in menstrual cycle duration [50]. Despite hysteroscopic intervention, there are reports of insufficient clinical improvement of symptoms [31]. Fatehnejad et al. report higher rates of dyspareunia and dysmenorrhea 1 year following surgery when compared to laparoscopic intervention [37]. Pregnancy rates following a history of secondary infertility range from 40 to 100% with hysteroscopy [24, 27, 31, 36, 38,39,40, 50, 52, 53, 60, 66,67,68]; however, there are incidences of placenta previa in subsequent pregnancies [34]. Based on a systematic review conducted by Harjee et al., the overall complication rate with hysteroscopic repair is 0% [40]. Vitale et al. report that hysteroscopic repair has a lower complication rate that laparoscopic or vaginal repair [56].
Hysteroscopic repair involves less operative and hospitalization time, as well as less expenses when compared to laparoscopic repair [62]. Zhang et al. also report less intraoperative blood loss [62]. Studies do indicate a risk of uterine perforation [2, 9, 44], risk of bladder injury, and a risk of uterine rupture with subsequent pregnancy [44]. Proximal resection may also theoretically increase the risk of cervical incompetence [55]. Additionally, recurrences long term are reported [44]. Of clinical relevance, improvement rates are worse in patients with a retroflexed uterus [28, 36, 38, 48].
Laparoscopic repair
There is conflicting opinions on the indications for laparoscopic repair, with some studies noting that it is appropriate for all patients regardless of fertility desire [44], and others limiting its use for larger defects described as a RMT of < 3 mm [26]. More broadly, laparoscopic repair is described as appropriate for patients with a history of infertility, ectopic pregnancy, lower gravidity, lower parity, and a lower number of previous caesarean sections [37, 47].
The reported outcomes of laparoscopic repair include an increased thickness of the residual myometrium [34, 43, 55]. Additionally, resolution and/or improvement of abnormal uterine bleeding [34, 41, 44, 49, 55, 62, 67, 69] and pain [41, 49] are reported. However, some patients remain symptomatic despite laparoscopic intervention [44], with pain described as an ongoing concern postoperatively for some patients [49]. According to Vervoort et al., laparoscopy allows for resolution of fluid in the uterine cavity [55]. Pregnancy rates following a history of secondary infertility range from 37.5 to 90% with laparoscopic intervention [24, 34, 40, 41, 49, 67]; however, placenta previa can occur with subsequent pregnancy [62]. The overall complication rate using a laparoscopic technique is reported at 16.7% [40].
Laparoscopic repair allows for the exploration of the pelvis and direct access to the CSDi [33], facilitating better visualization [44, 51]. This technique also enables lysis of adhesions as required [33]. It is easily applicable in many hospitals and for many uterine diseases (e.g., endometrial polyps, submucosal myoma, hyperplastic endometrium, ovarian cysts or myoma) which can be concurrently treated [44]. This technique facilitates the restoration of the anatomy of the lower uterine segment, as well as allows for antefixation in the cases of a retroverted uterus [70]. Laparoscopy has a low complication rate and necessitates a short hospital stay [44]. There is a risk of incomplete excision of the diverticulum and lack of accurate localization of the CSDi leading to continued symptoms, as well as a potential for recurrence [44].
Within the umbrella of laparoscopic repair, robotic-assisted surgery has been applied to the repair of CSDi defects [51]. In a report of two cases of caesarean scar defect repaired with robotic assistance, postoperatively both patients conceived within a year (3 and 11 months) and had no complications [59]. Additional reports of robotic repairs of these defects have also been reported to successfully treat other scar symptoms, including persistent vaginal spotting [71]. In a review of 34 cases robotically repaired by Gkegkes et al., the rate of subsequent pregnancy was found to be 47.1% with an intraoperative complicate rate of 2.9%. In their analysis, this made the treatment comparable to other techniques for CSDi repair [72].
Vaginal repair
Studies note that vaginal repair is appropriate for all patients, regardless of future fertility desire [45]. This method of repair is deemed appropriate in regions where laparoscopy or hysteroscopy is unavailable, or when surgeons are not proficient in either of the above techniques [69]. Additionally, it is preferred when the CSDi is located at a lower level [42, 69].
An increase in residual myometrial thickness following repair [30, 33, 69] and therefore resolution/improvement of the uterine defect [45, 69] is observed with vaginal repair. Strengthening of the uterine wall is also described [45], as is clinical improvement of abnormal uterine bleeding [29, 45, 69]. Additionally, vaginal repair shortens the duration of menstruation [29, 30, 57, 61]. However, there are reports of unsuccessful initial repair, necessitating further surgery [35]. Based on our review of the literature, pregnancy rates following a history of secondary infertility are between 22 and 80% [9, 35]. Studies report an overall complication rate of 0–33% [29, 40, 69].
Vaginal repair is described as a less invasive technique as the repair is conducted outside of the peritoneal cavity [45, 73] and requires a shorter operative time when compared to laparoscopy [51, 69]. However, Xie et al. describe a longer operative time and greater blood loss when compared to hysteroscopic repair [58]. A greater therapeutic effect is described when compared to hysteroscopic repair [58]. Vaginal repair facilitates the restoration of the anatomy of the lower uterine segment [70]. Hospitalization expense is also noted to be low [51, 69]. Additionally, general anesthesia is not always needed with this technique [61]. However, surgical expertise is required to avoid damaging adjacent structures and to correctly localize the CSDi with the limited surgical view afforded [44, 45, 69]. There is a risk of incomplete excision, hematoma, and pelvic infection [45].
Abdominal repair
Based on our review, there remains limited published data on the indications, advantages, and disadvantages/risks associated with abdominal repair of CSDi. Resolution and/or improvement of abnormal uterine bleeding and pelvic pain are noted in the literature [35]. However, there are reports of initial abdominal repair being unsuccessful, subsequently requiring further surgery [35]. Pregnancy rates following a history of secondary infertility are 67–75% [35, 40]. Studies report the complication rate with laparotomy is 0% [40, 49].
Case series
In this study, we were able to analyze patients treated for CSDi-associated secondary infertility with either hysteroscopic or laparoscopic management. Similar to the trend in currently available data, the majority of patients in this study were treated via hysteroscopy. Although statistical analyses were not appropriate for our sample, we observed a clear improvement in fertility outcomes following surgical intervention, particularly in the hysteroscopy group. Two thirds of patients treated with hysteroscopy and over one third of patients treated laparoscopically became pregnant postoperatively, while only 1/6 (17%) of expectantly managed patients achieved pregnancy.
Additionally, conception rates correlated well with live birth rates, with two thirds of hysteroscopy patients and one quarter of laparoscopy patients achieving at least one live birth. Given that hysteroscopic management involves cauterization or resection at the defect site, it is important to know about possible complications given the theoretical decreased integrity and scarring of the uterine wall at the site of the previous defect. In all 10 pregnancies that resulted from hysteroscopy, no cases of uterine rupture or abnormal placentation ensued, and all pregnancies were carried to term.
Strengths and limitations of the study
The strengths of our study include a long average duration of follow-up that approached 3 years, as well as a relatively low loss-to-follow-up after surgical intervention, allowing for accurate assessment of postoperative complications and conception rates. In addition, for all patients who became pregnant, we were able to have clear follow-up of all patients and their associated pregnancy outcomes.
There are a number of limitations to this study, given its retrospective and observational nature as well as relatively small sample size. Our sample size was limited by the number of patients seen for secondary infertility with CSDi by three physicians and excluded any patients who did not wish to have fertility restoration. This may limit the extent that we are able to draw from our analysis. However, it does accurately describe the experience of the 26 patients discussed and may highlight key information regarding treatment of this condition. In terms of patient characteristics, we cannot fully assess the risk factors for CSDi development as well as specific measurements of the CSDi. In addition, many of these patients did not have a SCSHG to aid in diagnosis, but instead had a TVUS, and in some cases a subsequent magnetic resonance imaging (MRI) to better characterize the scar. Furthermore, some of the patients in the series may have had other contributing factors impacting fertility. While this does not allow for isolation of CSDi as the sole cause of infertility in every case, it does more accurately reflect the real-world circumstances of many patients with multiple factors contributing to impaired fertility, and thus may be a relatively accurate representation of the efficacy of surgical intervention for the treatment of secondary infertility with suspected contribution due to CSDi. Limitations of our scoping review include that the review was not prospectively registered with a database prior to conducting the literature review. This may contribute to bias in our article, which we have worked to address through transparency regarding the search strategy used, the exclusion and the inclusion criteria utilized. In addition to the limitations of the current evidence, it is important to stress the fact that the option of “no treatment” was not properly evaluated. As such, this option may end up being the best management of CSDi. Until further evidence is available, we recommend a shared decision making on a case-by-case basis.
Despite these limitations, this study provides evidence that appropriate surgical intervention may improve reproductive outcomes.
Conclusion
Our case study highlights that for patients treated for CSDi for secondary infertility both hysteroscopic and laparoscopic interventions are adequate and successful in the improvement of fertility outcomes in these patients, and more successful than expectant management in this group. Our case series was supported by conclusions drawn in our scoping review, which demonstrated that hysteroscopic and laparoscopic operative approaches are successfully able to address patient concerns. When comparing the four techniques in our review, we found that vaginal repairs had the widest range of complication rates, but that laparoscopic surgery had the highest reported complication rate. Furthermore, hysteroscopic surgery had the highest rate of postoperative pregnancy, followed by abdominal repair and then laparoscopy. Vaginal repair, however, had the widest range in postoperative pregnancy. This brings to light different options for surgical techniques for these patients.
This study suggests that appropriate surgical treatment can improve pregnancy and live birth rates in patients with secondary infertility in the context of a confirmed CSDi. There are limitations given the retrospective design of this study, and additional prospective studies or randomized controlled trials would be useful in confirming these findings.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to patient confidentiality but are available from the corresponding author on reasonable request.
Abbreviations
- CSDi:
-
Caesarean scar disorders
- RMT:
-
Residual myometrial thickness
- TVUS:
-
Transvaginal ultrasound
- SCSHG:
-
Saline contrast sonohysterography
- CS:
-
Caesarean section
- BMI:
-
Body mass index
- AUB:
-
Abnormal uterine bleeding
- ART:
-
Assisted reproductive treatment
- SEM:
-
Standard error of the mean
- MeSH:
-
Medical Subject Headings
- MRI:
-
Magnetic resonance imaging
References
Angolile CM, Max BL, Mushemba J, Mashauri HL (2023) Global increased cesarean section rates and public health implications: a call to action. Health Sci Rep 6(5):e1274
Kremer TG, Ghiorzi IB, Dibi RP (2019) Isthmocele: an overview of diagnosis and treatment. Rev Assoc Med Bras (1992) 65(5):714–721
Naji O, Abdallah Y, Bij De Vaate AJ, Smith A, Pexsters A, Stalder C et al (2012) Standardized approach for imaging and measuring cesarean section scars using ultrasonography. Ultrasound Obstet Gynecol 39(3):252–259
Bakavičiūtė G, Špiliauskaitė S, Meškauskienė A, Ramašauskaitė D (2016) Laparoscopic repair of the uterine scar defect - successful treatment of secondary infertility: a case report and literature review. Acta Med Litu 23(4):227–231
Setubal A, Alves J, Osório F, Guerra A, Fernandes R, Albornoz J et al (2018) Treatment for uterine isthmocele, a pouchlike defect at the site of a cesarean section scar. J Minim Invasive Gynecol 25(1):38–46
Vervoort AJ, Uittenbogaard LB, Hehenkamp WJ, Brölmann HA, Mol BW, Huirne JA (2015) Why do niches develop in caesarean uterine scars? Hypotheses on the aetiology of niche development. Hum Reprod 30(12):2695–2702
Jordans IPM, de Leeuw RA, Stegwee SI, Amso NN, Barri-Soldevila PN, van den Bosch T et al (2019) Sonographic examination of uterine niche in non-pregnant women: a modified Delphi procedure. Ultrasound Obstet Gynecol 53(1):107–115
Klein Meuleman SJM, Murji A, van den Bosch T, Donnez O, Grimbizis G, Saridogan E et al (2023) Definition and criteria for diagnosing cesarean scar disorder. JAMA Netw Open 6(3):e235321
Tulandi T, Cohen A (2016) Emerging manifestations of cesarean scar defect in reproductive-aged women. J Minim Invasive Gynecol 23(6):893–902
MacGregor B (2023) Diagnosis and management of cesarean scar disorder. VGH OBGYN Grand Rounds
Bij de Vaate AJ, Brölmann HA, van der Voet LF, van der Slikke JW, Veersema S, Huirne JA (2011) Ultrasound evaluation of the cesarean scar: relation between a niche and postmenstrual spotting. Ultrasound Obstet Gynecol 37(1):93–99
Karlı PŞB, Kara F (2018) The incidence of isthmocele may be higher than reported. J Surg Med 2(3):283–287
Ofili-Yebovi D, Ben-Nagi J, Sawyer E, Yazbek J, Lee C, Gonzalez J et al (2008) Deficient lower-segment cesarean section scars: prevalence and risk factors. Ultrasound Obstet Gynecol 31(1):72–77
Bij de Vaate AJ, van der Voet LF, Naji O, Witmer M, Veersema S, Brölmann HA et al (2014) Prevalence, potential risk factors for development and symptoms related to the presence of uterine niches following cesarean section: systematic review. Ultrasound Obstet Gynecol 43(4):372–382
Wang CB, Chiu WW, Lee CY, Sun YL, Lin YH, Tseng CJ (2009) Cesarean scar defect: correlation between cesarean section number, defect size, clinical symptoms and uterine position. Ultrasound Obstet Gynecol 34(1):85–89
Florio P, Filippeschi M, Moncini I, Marra E, Franchini M, Gubbini G (2012) Hysteroscopic treatment of the cesarean-induced isthmocele in restoring infertility. Curr Opin Obstet Gynecol 24(3):180–186
Tower AM, Frishman GN (2013) Cesarean scar defects: an underrecognized cause of abnormal uterine bleeding and other gynecologic complications. J Minim Invasive Gynecol 20(5):562–572
Ash A, Smith A, Maxwell D (2007) Caesarean scar pregnancy. BJOG 114(3):253–263
Pérez-Medina T, Sancho-Saúco J, Ríos M, Pereira A, Argila N, Cabezas E et al (2014) Hysteroscopy in pregnancy-related conditions: descriptive analysis in 273 patients. J Minim Invasive Gynecol 21(3):417–425
Raimondo G, Grifone G, Raimondo D, Seracchioli R, Scambia G, Masciullo V (2015) Hysteroscopic treatment of symptomatic cesarean-induced isthmocele: a prospective study. J Minim Invasive Gynecol 22(2):297–301
Allornuvor GF, Xue M, Zhu X, Xu D (2013) The definition, aetiology, presentation, diagnosis and management of previous caesarean scar defects. J Obstet Gynaecol 33(8):759–763
Florio P, Gubbini G, Marra E, Dores D, Nascetti D, Bruni L et al (2011) A retrospective case-control study comparing hysteroscopic resection versus hormonal modulation in treating menstrual disorders due to isthmocele. Gynecol Endocrinol 27(6):434–438
Murji A, Sanders AP, Monteiro I, Haiderbhai S, Matelski J, Walsh C et al (2022) Cesarean scar defects and abnormal uterine bleeding: a systematic review and meta-analysis. Fertil Steril 118(4):758–766
Tanimura S, Funamoto H, Hosono T, Shitano Y, Nakashima M, Ametani Y et al (2015) New diagnostic criteria and operative strategy for cesarean scar syndrome: endoscopic repair for secondary infertility caused by cesarean scar defect. J Obstet Gynaecol Res 41(9):1363–1369
Abacjew-Chmylko A, Wydra DG, Olszewska H (2017) Hysteroscopy in the treatment of uterine cesarean section scar diverticulum: a systematic review. Adv Med Sci 62(2):230–239
Bujold E, Jastrow N, Simoneau J, Brunet S, Gauthier RJ (2009) Prediction of complete uterine rupture by sonographic evaluation of the lower uterine segment. Am J Obstet Gynecol 201(3):320.e1–6
Calzolari S, Sisti G, Pavone D, Ciocia E, Bianchini N, Cozzolino M (2019) Prevalence of infertility among patients with isthmocele and fertility outcome after isthmocele surgical treatment: a retrospective study. Ochsner J 19(3):204–209
Chang Y, Tsai EM, Long CY, Lee CL, Kay N (2009) Resectoscopic treatment combined with sonohysterographic evaluation of women with postmenstrual bleeding as a result of previous cesarean delivery scar defects. Am J Obstet Gynecol 200(4):370.e1–4
Chen Y, Chang Y, Yao S (2014) Transvaginal management of cesarean scar section diverticulum: a novel surgical treatment. Med Sci Monit 20:1395–1399
Chen H, Wang H, Zhou J, Xiong Y, Wang X (2019) Vaginal repair of cesarean section scar diverticula diagnosed in non-pregnant women. J Minim Invasive Gynecol 26(3):526–534
Cohen SB, Bouaziz J, Bar On A, Orvieto R (2020) Fertility success rates in patients with secondary infertility and symptomatic cesarean scar niche undergoing hysteroscopic niche resection. Gynecol Endocrinol 36(10):912–916
Demers S, Roberge S, Bujold E (2013) Laparoscopic repair of post-cesarean uterine scar defect. J Minim Invasive Gynecol 20(4):537
Dominguez JA, Pacheco LA, Moratalla E, Carugno JA, Carrera M, Perez-Milan F et al (2023) Diagnosis and management of isthmocele (Cesarean scar defect): a SWOT analysis. Ultrasound Obstet Gynecol 62(3):336–344
Donnez O, Donnez J, Orellana R, Dolmans MM (2017) Gynecological and obstetrical outcomes after laparoscopic repair of a cesarean scar defect in a series of 38 women. Fertil Steril 107(1):289–96.e2
Enderle I, Dion L, Bauville E, Moquet PY, Leveque J, Lavoue V et al (2020) Surgical management of isthmocele symptom relief and fertility. Eur J Obstet Gynecol Reprod Biol 247:232–237
Fabres C, Arriagada P, Fernández C, Mackenna A, Zegers F, Fernández E (2005) Surgical treatment and follow-up of women with intermenstrual bleeding due to cesarean section scar defect. J Minim Invasive Gynecol 12(1):25–28
Fatehnejad M, Hadizadeh A, Tayebi A, Ayati A, Marjani N, Gheshlaghi P et al (2023) Assessment of the clinical outcomes and complications of hysteroscopic and laparoscopic approaches in the treatment of symptomatic isthmocele: an observational study. Int J Gynaecol Obstet 163(3):965–971
Gubbini G, Casadio P, Marra E (2008) Resectoscopic correction of the “isthmocele” in women with postmenstrual abnormal uterine bleeding and secondary infertility. J Minim Invasive Gynecol 15(2):172–175
Gubbini G, Centini G, Nascetti D, Marra E, Moncini I, Bruni L et al (2011) Surgical hysteroscopic treatment of cesarean-induced isthmocele in restoring fertility: prospective study. J Minim Invasive Gynecol 18(2):234–237
Harjee R, Khinda J, Bedaiwy MA (2021) Reproductive outcomes following surgical management for isthmoceles: a systematic review. J Minim Invasive Gynecol 28(7):1291–302.e2
Karampelas S, Salem Wehbe G, de Landsheere L, Badr DA, Tebache L, Nisolle M (2021) Laparoscopic isthmocele repair: efficacy and benefits before and after subsequent cesarean section. J Clin Med 10(24):5785
Kulshrestha V, Agarwal N, Kachhawa G (2020) Post-caesarean niche (isthmocele) in uterine scar: an update. J Obstet Gynaecol India 70(6):440–446
Li C, Guo Y, Liu Y, Cheng J, Zhang W (2014) Hysteroscopic and laparoscopic management of uterine defects on previous cesarean delivery scars. J Perinat Med 42(3):363–370
Liu SJ, Lv W, Li W (2016) Laparoscopic repair with hysteroscopy of cesarean scar diverticulum. J Obstet Gynaecol Res 42(12):1719–1723
Luo L, Niu G, Wang Q, Xie HZ, Yao SZ (2012) Vaginal repair of cesarean section scar diverticula. J Minim Invasive Gynecol 19(4):454–458
Marotta ML, Donnez J, Squifflet J, Jadoul P, Darii N, Donnez O (2013) Laparoscopic repair of post-cesarean section uterine scar defects diagnosed in nonpregnant women. J Minim Invasive Gynecol 20(3):386–391
Piriyev E, Schiermeier S, Römer T (2022) Laparoscopic Isthmocele (Niche) correction as prevention in patients with fertility desire. Ginekol Pol 93(12):954–961
Rajiah P, Eastwood KL, Gunn MLD, Dighe M (2009) Uterine diverticulum. Obstet Gynecol 113(2 Pt 2):525–527
Schepker N, Garcia-Rocha GJ, von Versen-Höynck F, Hillemanns P, Schippert C (2015) Clinical diagnosis and therapy of uterine scar defects after caesarean section in non-pregnant women. Arch Gynecol Obstet 291(6):1417–1423
Shapira M, Mashiach R, Meller N, Watad H, Baron A, Bouaziz J et al (2020) Clinical success rate of extensive hysteroscopic cesarean scar defect excision and correlation to histologic findings. J Minim Invasive Gynecol 27(1):129–134
Sipahi S, Sasaki K, Miller CE (2017) The minimally invasive approach to the symptomatic isthmocele - what does the literature say? A step-by-step primer on laparoscopic isthmocele - excision and repair. Curr Opin Obstet Gynecol 29(4):257–265
Tsuji S, Kimura F, Yamanaka A, Hanada T, Hirata K, Takebayashi A et al (2018) Impact of hysteroscopic surgery for isthmocele associated with cesarean scar syndrome. J Obstet Gynaecol Res 44(1):43–48
Vegas Carrillo de Albornoz A, López Carrasco I, Montero Pastor N, Martín Blanco C, Miró Matos M, Alonso Pacheco L et al (2019) Outcomes after hysteroscopic treatment of symptomatic isthmoceles in patients with abnormal uterine bleeding and pelvic pain: a prospective case series. Int J Fertil Steril 13(2):108–112
Vervoort A, van der Voet LF, Hehenkamp W, Thurkow AL, van Kesteren P, Quartero H et al (2018) Hysteroscopic resection of a uterine caesarean scar defect (niche) in women with postmenstrual spotting: a randomised controlled trial. BJOG 125(3):326–334
Vervoort A, Vissers J, Hehenkamp W, Brölmann H, Huirne J (2018) The effect of laparoscopic resection of large niches in the uterine caesarean scar on flopr, ultrasound findings and quality of life: a prospective cohort study. BJOG 125(3):317–325
Vitale SG, Ludwin A, Vilos GA, Török P, Tesarik J, Vitagliano A et al (2020) From hysteroscopy to laparoendoscopic surgery: what is the best surgical approach for symptomatic isthmocele? A systematic review and meta-analysis. Arch Gynecol Obstet 301(1):33–52
Wang Y, Li J, Wang H, Wang X (2020) Vaginal repaired cesarean section diverticulum is beneficial in women with two prior cesarean sections. BMC Womens Health 20(1):81
Xie H, Wu Y, Yu F, He M, Cao M, Yao S (2014) A comparison of vaginal surgery and operative hysteroscopy for the treatment of cesarean-induced isthmocele: a retrospective review. Gynecol Obstet Invest 77(2):78–83
Yalcinkaya TM, Akar ME, Kammire LD, Johnston-MacAnanny EB, Mertz HL (2011) Robotic-assisted laparoscopic repair of symptomatic cesarean scar defect: a report of two cases. J Reprod Med 56(5–6):265–270
Zeller A, Villette C, Fernandez H, Capmas P (2021) Is hysteroscopy a good option to manage severe cesarean scar defect? J Minim Invasive Gynecol 28(7):1397–1402
Zhang X, Yang M, Wang Q, Chen J, Ding J, Hua K (2016) Prospective evaluation of five methods used to treat cesarean scar defects. Int J Gynaecol Obstet 134(3):336–339
Zhang Q, Lei L, Zhang A, Zou L, Xu D (2021) Comparative effectiveness of laparoscopic versus hysteroscopic approach in patients with previous cesarean scar defect: a retrospective cohort study. Ann Transl Med 9(20):1529
Zhu Q, He X, Jiang L, Liang G, Zhu C, Pan H et al (2020) Effectiveness of hysteroscopic resection of a uterine caesarean niche can be predicted: a prospective cohort study. Sci Rep 10(1):17424
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D et al (2018) PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473
Nezhat C, Falik R, Li A (2017) Surgical management of niche, isthmocele, uteroperitoneal fistula, or cesarean scar defect: a critical rebirth in the medical literature. Fertil Steril 107(1):69–71
Al Mutairi BH, Alrumaih I (2020) Hysteroscopy in the treatment of myometrial scar defect (diverticulum) following cesarean section delivery: a systematic review and meta-analysis. Cureus 12(11):e11317
Mashiach R, Burke YZ (2021) Optimal isthmocele management: hysteroscopic, laparoscopic, or combination. J Minim Invasive Gynecol 28(3):565–574
Abdou AM, Ammar IMM (2018) Role of hysteroscopic repair of cesarean scar defect in women with secondary infertility. Middle East Fertil Soc J 23(4):505–509
Zhang Y (2016) A comparative study of transvaginal repair and laparoscopic repair in the management of patients with previous cesarean scar defect. J Minim Invasive Gynecol 23(4):535–541
Brown K, Tkacz Z (2018) Hysteroscopic and laparoscopic management of caesarean scar (niche) defects in symptomatic patients. J Obstet Gynaecol 38(5):730
La Rosa MF, McCarthy S, Richter C, Azodi M (2013) Robotic repair of uterine dehiscence. Jsls 17(1):156–160
Gkegkes ID, Psomiadou V, Minis E, Iavazzo C (2023) Robot-assisted laparoscopic repair of cesarean scar defect: a systematic review of clinical evidence. J Robot Surg 17(3):745–751
Baekelandt JF, Kapurubandara S (2023) A novel approach using vaginal natural orifice transluminal endoscopic surgery to repair a symptomatic uterine isthmocele. Fertil Steril 119(2):328–330
Acknowledgements
We would like to acknowledge Dr. Natasha Simula, Dr. Neeraj Mehra, and Dr. Jon Havelock for their help with this project.
Funding
Not applicable. There were no funding sources for this study.
Author information
Authors and Affiliations
Contributions
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript. Furthermore, each author certifies that this material or similar material has not been and will not be submitted to or published in any other publication. RH and JK completed the chart reviews and obtained ethics approval. JD performed the literature review and drafting of the manuscript. EB updated, edited and collated the manuscript for publication. NM and JH performed surgical repairs for included patients. MB is the primary investigator for this project.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was provided by the UBC Research and Ethics Institutional Review Board (H19-02324). Participants were consented following the institutional protocols.
Consent for publication
We have received consent to publish these results from all relevant participants or organizations.
Competing interests
Dr. Bedaiwy reports grants and personal fees from Abbvie Inc, grants and personal fees from Allergan Inc, personal fees from Heron Inc, grants from Ferring Inc, and grants from Canadian Institute of Health Research, outside the submitted work. The remainder of the authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Harjee, R., Devji, J., Barrett-Chan, E.K. et al. Surgical management of caesarean scar disorder using different techniques: a scoping review and case series. Middle East Fertil Soc J 29, 25 (2024). https://doi.org/10.1186/s43043-024-00183-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-024-00183-9