Abstract
Background
Methylation of the promoter at CpG islands is a mechanism of silencing tumor suppressor genes and therefore enhances cancer progression. The study aimed to examine promoter methylation frequencies of five tumor suppressor genes in hepatocellular carcinoma and their implication on the first-year outcome of surgical resection of the tumor. Fifty specimens of hepatocellular carcinoma and the adjacent non-tumorous liver tissue were collected from the surgically resected hepatic tumor. The status of promoter methylation of tumor suppressor genes RASSF1A, CHFR, MGMT, GSTP1, and hMLH1 was investigated using methylation-specific polymerase chain reaction.
Results
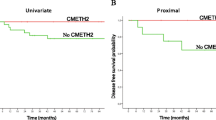
The frequency of promoter methylation of these tumor suppressors genes (TSG) genes in hepatocellular carcinoma was significantly higher than non-tumorous tissue all, P < 0.05, with a methylation rate of 80% in RASSF1A, 70% in CHFR, 46% in GSTP1, 56% in MGMT, and 10% in hMLH1. Methylation of RASSF1A, CHFR, and MGMT promoter genes was significantly associated with decreased first-year postoperative survival and increased recurrence of hepatocellular carcinoma, P < 0.05.
Conclusion
Methylated RASSF1A, CHRF, and MGMT promoters indicated poor prognosis among patients with hepatocellular carcinoma and may serve as potential prognostic indicators in patients with hepatocellular carcinoma.
Similar content being viewed by others
Background
Liver carcinoma is the fourth leading cause of cancer death worldwide, with hepatocellular carcinoma (HCC) being the histological subtype accounting for more than 75% of all cases. Geographical distribution affects the risk for the disease. HCV infection is the predominant predisposing factor for HCC in Egypt and Japan, whereas in China and Eastern Africa, aflatoxin exposure and HBV infection are the main risks. Coinfections of HBV with HCV or hepatitis δ virus are the most common risks found in Mongolia [1].
The molecular mechanisms of hepatocellular carcinogenesis are still predominantly unidentified despite the significant progress in its diagnosis and treatment [2]. Epigenetic alteration in the DNA with the resulting abnormal gene expression has been postulated to have a role in the different stages of hepatocellular carcinogenesis [3, 4].
In early stages, the transformation of the premalignant lesion to invasive carcinoma is usually associated with comprehensive DNA hypomethylation with hypermethylation only at certain CpG islands [5]. Epigenetic studies have shown that CpG islands which are rich in cytosine guanine dinucleotides are located in regulatory regions of more than 50% of human gene promoters [6]. Abnormal methylation of the CpG islands in the promoters region of genes involved in many cellular biological processes related to carcinogenesis such as DNA damage response, DNA repair, cell cycle control, and apoptosis has been documented [7].
In tumor tissues, promoter hypermethylation may result in silencing of TSGs such as RASSF1A, CHFR, GSTP1, MGMT, and hMLH1 [8, 9], that regulate cell signaling pathways involved in cell division, mitosis, and apoptosis in lung, breast, ovarian, and head and neck squamous cell carcinoma(HNSCC) [10, 11].
CHFR gene is involved in prophase checkpoint, and its promoter methylation appears to modulate microtubule function in cancer colon, lung, and gastrointestinal cancer [12, 13]. MGMT plays a vital role in preventing the initiation of mutations and, abnormalities of MGMT were found in the malignancies of the lung, colon, liver, and HNSCC [14]. GSTP1 and the mismatch repair gene hMLH1 have an anti-oxidative damage regulatory role, and their hypermethylation was detected in various malignant tumors, such as HCC, breast, lung, hereditary colon cancer, gastric, endometrium, prostate, and HNSCC [15, 16]. Existing evidence confirm the assumption that the methylation of GSTP1 and hMLH1might serve as screening for HCC, and HCC that possess a high frequency of methylation in the CpG island of the promoter regions tend to have accelerated hepato-carcinogenesis in the premalignant stages [17].
This study aimed to examine the methylation status of the promoter regions of five TSGs RASSF1A, CHFR, GSTP1, MGMT, and hMLH1 in HCC tissues and the adjacent normal tissue (ANT) in postoperative resection specimens and to check the association of the methylation status of these genes with some clinical and pathological features of HCC.
Methods
Patients and sample collection
Tumor and ANT specimens were collected from postoperative hepatic resection of HCC patients who had surgical resection at National Liver Institute Hospital between August 2017 and October 2019.
The study was approved by the Institutional Review Board of the National Liver Institute, and informed consent was obtained from all participants. HCC (n = 50) and ANT (n = 50) samples were immediately frozen in liquid nitrogen after surgical resection and stored at − 80 °C till the assay.
The inclusion criteria
The preoperative diagnosis of HCC was established by finding a single or multiple focal hepatic lesion(s) during imaging study and elevated serum AFP > 400 ng/ml and or detection of HCC by histological examination of the liver biopsy [18]. Child–Pugh, and Barcelona Clinic Liver Cancer (BCLC) were used for clinical classification and staging of HCC patients [19, 20]. All patients enrolled in the study had no history of alcohol intake or illicit drug abuse. The study excluded any patients with chronic cholestasis and extrahepatic obstructive gall bladder diseases. Histological examination of sections stained with H&E (Fig. 1) confirmed the presence of HCC with mild to moderately undifferentiated cells, with atypical enlarged nuclei, granular cytoplasm arranged in trabecular patterns with transgressing vessels. Histological grading of HCC: Grade I tumors show small cells arranged in trabeculae, with abundant cytoplasm and minimal nuclear irregularity. Grade II tumor cells have prominent nucleoli and hyperchromatic irregular nucleus. Grade III tumors display anaplastic giant cells with angulated nuclei and pleomorphic appearance more than grade II. ANT obtained from the safety margin of the resected tumor shows the normal-appearing hepatocytes with a low nuclear to cytoplasmic ratio without any nuclear atypia or prominent nucleoli.
The patients’ gender was 39 men and 11 women, and their age ranged from 33 to 64 years. Thirty-five patients had single HFL, 15 had multiple HFL, 40 patients had tumor size larger than 3 cm, and 37 patients had grade two lesions, 13 had grade three lesions. Twenty-three patients had LN invasion, 38 had associated liver cirrhosis. Serologic examinations revealed that 48 had positive anti-HCV antibodies, and four cases were positive for anti-HBVsAg antibodies.
Genomic DNA
DNA was extracted from frozen HCC and ANT tissue samples using the Qiagen kit (Qiagen, Valencia, CA) according to the manufacturer’s instructions. The extracted DNA concentration was determined by a Nanodrop 1000 spectrophotometer (Nanodrop Technologies, Wilmington, DE, USA) at 260 nm absorbance.
Bisulfite modification of the DNA
The principle of bisulfite conversion is that all unmethylated cytosines convert to uracils, whereas the methylated cytosines remain unchanged. DNA bisulfite modification was achieved by Intergen CpGenome DNA Modification Kit, according to the manufacturer’s protocol (Intergen Company, New York, NY) [21, 22]. Briefly, 2 µg of genomic DNA was denatured in 20 µl of 0.2 M NaOH for 20 min at 50 °C and then diluted in 500 µl of a new mix solution of 10 mM hydroquinone and 3 M sodium bisulfite and incubated for 3 h at 70 °C. The DNA sample was then desalted by eluting it through a DNA cleansing column primed with 0.3 M NaOH for 10 min at room temperature and precipitated with ethanol. The bisulfite-modified DNA was resuspended in 100 µl of H2O and stored at -80 °C. The ssDNA setting of the Nanodrop was used to measure the concentration of the bisulfite-converted DNA. The post-bisulfite conversion and the integrity of the bisulfite-converted DNA were examined by gel electrophoresis for DNA fragmentation which might disturb the expected amplification region and abolish its availability for PCR amplification [23, 24]. The housekeeping gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH) of the unconverted DNA was used as internal loading controls (Fig. 2A).
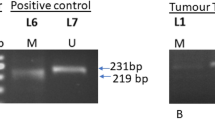
A DNA integrity after bisulfite conversion: Pre-amplification visualization on agarose gel electrophoresis. Two µl of the eluted bisulfite-converted DNA was loaded and run on 2% gel in TBS buffer for 60 min. Smears with equal intensities indicate the presence of the converted DNA. Lanes (1–3) good conversion, lanes (5 and 6) weak conversion, and lanes (4 and 7) no conversion. B The specificity of the primers. Bisulfite Modified (BM-DNA) and Unmodified DNA (UM-DNA) were amplified with primers specific for unmethylated (U) and methylated (M) DNA. Only modified DNA showed PCR amplicons. GAPDH of the UM-DNA used as a control for equal loading. C Localization of methylated and unmethylated PCR band of every TSG. Ethidium bromide-stained agarose gel electrophoresis of bisulfite modified DNA amplified with primers specific for unmethylated (U) and methylated (M) DNA. Lane 1 100 bp molecular marker, lane 2–3 PCR amplicons of RASSF1A promoter detected at 203 bp, lane 4-5 PCR amplicons of CHFR promoter at 144 bp, lane 6-7 PCR amplicons of GSTP1 promoter at 159 bp, lane 8-9 PCR amplicons of MGMT promoter detected at 93 bp, lane 10-11 PCR amplicons of hMLH1 promoter detected at 154 bp. GAPDH of the UM-DNA used as a control for equal loading. D MSP assay interpretation: Representative experiment showing molecular ladder marker, positive and negative controls (lanes 1–4), and bisulfite modified DNA amplified with primers specific for unmethylated (U) and methylated (M) DNA (lanes 5–10). Methylated promoter of a gene contains only the methylated amplicon (lane 5–6), the partially methylated promoter contains both methylated and unmethylated amplicons (lane 7–8), and the unmethylated promoter contains only the unmethylated amplicon (lane 9–10). (+ ve con.) positive control, (-ve con) negative control. M Marker, L 100 bp ladder. GAPDH of the UM-DNA was used as a control for equal loading. E Heat map of the TSGs promoter methylation in the HCC and ANTs. The intensity of the PCR bands reflecting the methylation status of the TSGs promoter in HCC and ATC were plotted in a heat map. Red and green colors represent relative high and low TSGs methylation values, respectively
Methylation-specific PCR (MSP)
MSP was accomplished with methylation-specific primers for the promoter regions of each gene that distinguished the unmethylated and methylated regions of the modified DNA. The forward and the reverse sequences of each primer are shown in Table 1. For each reaction, the PCR mixture consisted of one μl bisulfite-treated DNA, 10 µM of each primer in 0.15 μl, 9.6 μl nuclease-free water, and 10 μl of Hot-StarTaq Master Mix (Qiagen), consisting of Taq DNA polymerase, dNTPs mixture, and reaction buffer in a final volume of 20 μl. Thermal cycling (GeneAmp PCR system 2,400, Applied Biosystems, Foster City, CA, USA) [21] settings were initial heat denaturing step at 95 °C for 12 min; then, the second step comprises 40 cycles of 94 °C for 30 s, annealing temperature (AT) for 30 s (AT of PCR amplification for each gene is listed in (Table 1), 72 °C for 45 s, and a final extension at 72 °C for 10 min. PCR products were separated by electrophoresis on 2% agarose gel in TBS buffer and subsequently stained by ethidium bromide and visualized under UV illumination. PCR gel documentation system (Syngene InGenius3 Gel Documentation System, USA) was used to scan gels, and band intensities of each sample were determined using ImageJ software (National Institutes of Health, Bethesda, MD, USA).
Analysis of the methylation status of each TSG and the interpretation of the MS-PCR assay
The modified DNA was amplified with primers specific for unmethylated and methylated DNA. Both unmethylated and methylated primer pairs were tested using bisulfite-unconverted DNA to determine their specificity (no amplified PCR product, Fig. 2B). For each run of the MSP, the water of high molecular quality (RNase-free and DNase-free) was used as negative PCR control, and a tumor sample with known hypermethylation was used as a positive control. Any sample which did not show the unmethylated band was repeated, if it still not showing, it was discarded [20]. The PCR products were identified on gel electrophoresis after staining with ethidium bromide. Figure 2C presents a control experiment that shows the methylated or unmethylated amplicons of the five test gene promoters at the corresponding size relative to the DNA ladder. Figure 2D shows a control experiment that demonstrates the interpretation of MSP assay of any tested gene. The methylation status of a promoter was complete methylation when it shows only the methylated PCR product or partially methylated when it contains both methylated and unmethylated PCR products, or unmethylated when it shows only the unmethylated product.
Quantification of the Methylation status of the gene’s promoter
The intensity of the PCR bands reflecting the methylation status was measured and quantified as intensity units (IU) by ImageJ software (National Institutes of Health, Bethesda, MD, USA) [21]. A heat map generated from the band IU showing the methylation status of all genes in HCC and ANT samples (Fig. 2E).
Statistical analysis
Statistical analysis was carried out using SPSS V23 Software. The Graph Pad Prism version 9 was used to generate the heat map of methylation of different genes. The χ2 test and the Fisher’s exact test were used to compare frequencies of the methylation of promoters of genes. The level of significance was at P values of < 0.05.
Results
Frequency of tumor suppressor genes methylation in HCC and ANT
The frequencies of promoter methylation of RASSF1A, CHFR, GSTP1, MGMT, and hMLH1 genes in ANT and HCC tissue are summarized in Table 2. In HCC, RASSF1A was the most frequently affected (80%), followed by CHFR (70%), MGMT (56%), and GSTP1 (46%). The lowest frequency of methylation was noticed for hMLH1(14%) Fig. The frequency of methylation of RASSF1A CHFR, MGMT, GSTP1 and hMLH1 was significantly higher in HCC relative to its corresponding ANT, P = 0.046; P = 0.018; P = 0.001; P = 0.019; and P = 00.001, respectively.
Association between promoter methylation of TSGs and clinicopathological parameters of HCC
The association between gene promoter methylation and the clinicopathological characteristics of HCC is assessed and presented in Table 3. No significant relationship was observed between promotor methylation of the studied genes and the clinicopathological parameters, such as tumor number, tumor size, histological grade, serum AFP level, and liver cirrhosis (χ 2, P > 0.05). However, promoter hypermethylation of RASSF1A, CHFR, and MGMT, and GSTP1 was significantly associated with first-year recurrence of HCC (χ2, P < 0.05); promoter hypermethylation of RASSF1A, CHFR, and MGMT, but hypomethylation of the hMLH1 was significantly associated with a decrease in first-postoperative year survival (χ2, P < 0.05).
Discussion
In this study, a panel of five genes RASSF1A, CHFR, GSTP1, MGMT, and hMLH1 with known tumor suppressor activities were examined for the methylation status of their promoter regions in both HCC and its normal surrounding tissue obtained from surgical resection of the liver tumor. These TSGs are targets for epigenetic silencing in diverse human cancers. The study found that the frequencies of promoter methylation of these TSGs were more common in HCC than non-tumor liver tissues. Among the five genes, RASSF1A had the highest rate (80%) of promoter methylation, followed by CHFR (70%), MGMT (56%), GSTP1 (46%), and hMLH1 (10%). Several studies had shown that hypermethylation of these promoters was significantly higher in HCC tumor tissues than either ANT or normal liver tissues [25]. Li et al. found hypermethylation frequencies of RASSF1A, CHFR, GSTP1, and MGMT genes ranged from 78 to 32% for MGMT with no hypermethylation detected for hMLH1[26]. Lin et al. explored the methylation of the promoter areas of p15, p16, p21, p27, and RASSF1A genes in tour tissue of 50 HCC patients. The frequency of RASSF1A promoter methylation was the highest (96%) and most common among the studied gene [27]. Araujo et al. detected a rate of RASSF1A (88%) hypermethylation in HCC samples of Brazilian Patients with liver cancer [28]. Zhang et al. explored the diagnostic value of abnormal promoter hypermethylation of three TGS RASSF1A, p15, and p16 in the serum DNA for prediction of HCC and found RASSF1A had the highest frequency of hypermethylation (70%) of HCC cases [29]. Similarly, Dong et al. and Liu et al. studied the diagnostic performance of serum or plasma RASSF1A methylation as a noninvasive marker of HCC and found a RASSF1A methylation had a frequency of (64%) and 73% of HCC serum DNA samples [30, 31]. In the current study CHFR, promoter methylation was the second in frequency (50%) after RASSF1A. Sakai et al. found a frequency of CHFR methylation 35% in HCC relative to non-methylation in the noncancerous liver tissues. CHFR methylation was significantly associated with an infiltrative growth pattern and an advanced stage [32]. Chen et al. detected a moderate frequency of CHFR methylation in HCC tissues and a low frequency in corresponding noncancerous tissues (20% vs. 2%) [33]. In this study, the frequency of GSTP1 and MGMT hypermethylation was 56% and 46%; however, Lou et al. investigated the methylation frequencies of RASSF1A, MGMT, and GSTP1 in HCC found a methylation rate of 95% in RASSF1A, 73% in GSTP1, and 60% in MGMT. The methylation of these genes was more frequent in HCC than that ANT [34]. Li et al. showed that MGMT methylation was 15%, and there was neither significant difference in MGMT hypermethylation between HCC and adjacent tissues, [35]. Wang et al. explored the abnormal promoter CpG island methylation of the GSTP1 promotor gene as a biomarker for HCC and found the methylation rate of GSTP1 promoter hypermethylation was 88.5% in tumor tissues and 69% in the corresponding non-tumor tissue. GSTP1 promoter hypermethylation was identified in 50% of circulating tumor DNA in the serum from HCC patients, signifying its role in the pathogenesis of HCC and its potential as a biomarker for early diagnosis and follow-up of HCC [36]. In this study the hMLH1, promoter hypermethylation was 10% in both HCC and ANT. Matsukura et al. reported the frequency of hMLH1 promoter hypermethylation in HCCs was 11% [37]. In the current study, the methylation status of these genes was not significantly associated with the clinical parameters of the HCC such as the number of the hepatic focal lesion, burden of the tumor size, histological grade of the tumor, serum AFP level, and the presence of liver cirrhosis. However, the frequency of RASSF1A, CHFR, MGMT methylation was significantly related to recurrence of HCC tumor within one year of surgical resection and a decrease in the first-year disease-free survival. Lin et al. did not find a significant association between the frequency of methylation of promoter regions of the RASSF1A gene and the clinicopathological parameters in patients with HCC [27]. Dong et al. found serum RASSF1A hypermethylation was significantly related to the histological grading, tumor stage of HCC, but no significant relationship was observed with serum HBV, tumor number, tumor size, and liver cirrhosis [31]. Xu et al., in a large meta-analysis that included literature data from 34 studies comprising 2075 HCC and 2276 non-tumor, found that the frequency of RASSF1A gene promoter hypermethylation was significantly related to a high HCC risk [38]. Liu et al. examined the role of serum RASSF1A as a prognostic marker for early recurrence after curative HCC resection. The study detected a significant association between serum DNA RASSF1A promoter hypermethylation and lymph nodes metastasis, early recurrence, and poor prognosis after curative surgical resection of the tumor [30]. Similarly, Chan et al. showed patients with higher serum RASSF1A methylation at diagnosis during the first-year after tumor resection had poorer disease-free survival [39]. Nishida et al. detected hypermethylation of TSGs GSTP1 and RASSF1A in the early stages of HCC, and these genes were associated with the progression of chronic HCV to HCC [40]. Similarly, MGMT and GSTP1 promoter hypermethylation were found to be associated with an increased risk of HCC and a shorter disease-free survival [35, 41]. Thus, the change in the methylation of such genes may be critical in the early phases of carcinogenesis and would offer a potential prognostic role for estimating the risk of chronic HCV to develop HCC [28, 40]. Although the perception of promotor methylation as markers to detect HCC appears very well reasonable, yet promotor methylation of these genes is still mainly narrow to the research work, with limited sensitivity, and no ultimate grouping of genes has not yet been reached [42].
Nevertheless, markers that detect both methylated and unmethylated promoters can improve the prediction of postoperative recurrence of HCC [43]. Another ongoing use of DNA methylation biomarkers is the eventual capability to predict the response to chemoembolization or sorafenib treatments of HCC, in line with the previous use of MGMT promoter methylation as a predictive biomarker for temozolomide therapy in glioblastoma patients [44].
Conclusions
This study examined the epigenetic changes in the promoter regions of five tumor suppressor genes (RASSF1A, CHFR, MGMT, GSTP1, and hMLH1) in tumors and adjacent non-tumor liver tissues of HCC patients. The frequencies of promoter methylation of TSGs were more common in HCC than ANT but without any significant association with tumor number, tumor size, histological grade, or serum AFP. Among the five genes, RASSF1A and CHFR were the highest in methylation and hMLH1 was the lowest in methylation of these genes. Promotor hypermethylation of RASSF1A, CHFR, and MGMT was significantly associated with a decrease in the first-postoperative year survival and increased recurrence of HCC. These molecular changes may be potential prognostic biomarkers for monitoring the clinical outcome of patients after surgical resection of the HCC.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- ANT:
-
Adjacent non-tumorous tissue
- AFP:
-
Alpha-feto protein
- TSG:
-
Tumor suppressor gene
- RASSF1A :
-
Ras association domain family 1
- CHFR :
-
Checkpoint with forkhead and ring finger domains
- MGMT :
-
[O (6)-methylguanine-DNA methyltransferase]
- GSTP1 :
-
Glutathione-S-transferase-pi gene
- hMLH1 :
-
Human mutL homolog
- MSP:
-
Methylation-specific polymerase chain reaction
- GAPDH:
-
Glyceraldehyde 3-phosphate dehydrogenase
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Fix OK, Hameed B, Fontana RJ, Kwok RM, McGuire BM, Mulligan DC, Pratt DS, Russo MW, Schilsky ML, Verna EC, Loomba R, Cohen DE, Bezerra JA, Reddy KR, Chung RT (2020) Clinical Best Practice Advice for Hepatology and Liver Transplant Providers During the COVID-19 Pandemic: AASLD Expert Panel Consensus Statement. Hepatology 72(1):287–304
Khan FS, Ali I, Afridi UK, Ishtiaq M, Mehmood R (2017) Epigenetic mechanisms regulating the development of hepatocellular carcinoma and their promise for therapeutics. Hepatol Int 11(1):45–53
Danstrup CS, Marcussen M, Pedersen IS, Jacobsen H, Dybkaer K, Gaihede M (2020) DNA methylation biomarkers in peripheral blood of patients with head and neck squamous cell carcinomas. A systematic review. PLoS ONE 15(12):e0244101
Calvisi DF, Ladu S, Gorden A, Farina M, Lee JS, Conner EA, Schroeder I, Factor VM, Thorgeirsson SS (2007) Mechanistic and prognostic significance of aberrant methylation in the molecular pathogenesis of human hepatocellular carcinoma. J Clin Invest 117(9):2713–2722
Vucic EA, Brown CJ, Lam WL (2008) Epigenetics of cancer progression. Pharmacogenomics 9(2):215–234
Teodoridis JM, Strathdee G, Brown R (2004) Epigenetic silencing mediated by CpG island methylation: potential as a therapeutic target and as a biomarker. Drug Resist Updat 7(4–5):267–278
Tian Y, Wong VW, Chan HL, Cheng AS (2013) Epigenetic regulation of hepatocellular carcinoma in non-alcoholic fatty liver disease. Semin Cancer Biol 23(6 Pt B):471–482
Weng X, Wu J, Lv Z, Peng C, Chen J, Zhang C, He B, Tong R, Hu W, Ding C, Cao L, Chen D, Wu J, Zheng S (2019) Targeting Mybbp1a suppresses HCC progression via inhibiting IGF1/AKT pathway by CpG islands hypo-methylation dependent promotion of IGFBP5. EBioMedicine 44:225–236
Burbee DG, Forgacs E, Zochbauer-Muller S, Shivakumar L, Fong K, Gao B, Randle D, Kondo M, Virmani A, Bader S, Sekido Y, Latif F, Milchgrub S, Toyooka S, Gazdar AF, Lerman MI, Zabarovsky E, White M, Minna JD (2001) Epigenetic inactivation of RASSF1A in lung and breast cancers and malignant phenotype suppression. J Natl Cancer Inst 93(9):691–699
van der Weyden L, Tachibana KK, Gonzalez MA, Adams DJ, Ng BL, Petty R, Venkitaraman AR, Arends MJ, Bradley A (2005) The RASSF1A isoform of RASSF1 promotes microtubule stability and suppresses tumorigenesis. Mol Cell Biol 25(18):8356–8367
De Jong WK, Verpooten GF, Kramer H, Louwagie J, Groen HJ (2009) Promoter methylation primarily occurs in tumor cells of patients with non-small cell lung cancer. Anticancer Res 29(1):363–369
Shibata Y, Haruki N, Kuwabara Y, Ishiguro H, Shinoda N, Sato A, Kimura M, Koyama H, Toyama T, Nishiwaki T, Kudo J, Terashita Y, Konishi S, Sugiura H, Fujii Y (2002) Chfr expression is downregulated by CpG island hypermethylation in esophageal cancer. Carcinogenesis 23(10):1695–1699
Kato K, Hara A, Kuno T, Mori H, Yamashita T, Toida M, Shibata T (2006) Aberrant promoter hypermethylation of p16 and MGMT genes in oral squamous cell carcinomas and the surrounding normal mucosa. J Cancer Res Clin Oncol 132(11):735–743
Cui J, Li G, Yin J, Li L, Tan Y, Wei H, Liu B, Deng L, Tang J, Chen Y, Yi L (2020) GSTP1 and cancer: expression, methylation, polymorphisms and signaling (Review). Int J Oncol 56(4):867–878
Malhotra P, Anwar M, Kochhar R, Ahmad S, Vaiphei K, Mahmood S (2014) Promoter methylation and immunohistochemical expression of hMLH1 and hMSH2 in sporadic colorectal cancer: a study from India. Tumour Biol 35(4):3679–3687
Li QF, Li QY, Gao AR, Shi QF (2015) Correlation between promoter methylation in the GSTP1 gene and hepatocellular carcinoma development: a meta-analysis. Genet Mol Res 14(2):6762–6772
Heimbach JK (2017) Overview of the updated AASLD guidelines for the management of HCC. Gastroenterol Hepatol (N Y) 13(12):751–753
Hoffmann J (1983) Stapler transection of the oesophagus for bleeding oesophageal varices. Scand J Gastroenterol 18(6):707–711
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R (1973) Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 60(8):646–649
Herman JG, Graff JR, Myohanen S, Nelkin BD, Baylin SB (1996) Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. Proc Natl Acad Sci USA 93(18):9821–9826
Hoque MO, Begum S, Topaloglu O, Jeronimo C, Mambo E, Westra WH, Califano JA, Sidransky D (2004) Quantitative detection of promoter hypermethylation of multiple genes in the tumor, urine, and serum DNA of patients with renal cancer. Cancer Res 64(15):5511–5517
Ehrich M, Zoll S, Sur S, van den Boom D (2007) A new method for accurate assessment of DNA quality after bisulfite treatment. Nucleic Acids Res 35(5):e29
Holmes EE, Jung M, Meller S, Leisse A, Sailer V, Zech J, Mengdehl M, Garbe LA, Uhl B, Kristiansen G, Dietrich D (2014) Performance evaluation of kits for bisulfite-conversion of DNA from tissues, cell lines, FFPE tissues, aspirates, lavages, effusions, plasma, serum, and urine. PLoS ONE 9(4):e93933
Zhang C, Li J, Huang T, Duan S, Dai D, Jiang D, Sui X, Li D, Chen Y, Ding F, Huang C, Chen G, Wang K (2016) Meta-analysis of DNA methylation biomarkers in hepatocellular carcinoma. Oncotarget 7(49):81255–81267
Li Z, Zhang H, Yang J, Hao T, Li S (2012) Promoter hypermethylation of DNA damage response genes in hepatocellular carcinoma. Cell Biol Int 36(5):427–432
Lin JC, Wu YC, Wu CC, Shih PY, Wang WY, Chien YC (2015) DNA methylation markers and serum alpha-fetoprotein level are prognostic factors in hepatocellular carcinoma. Ann Hepatol 14(4):494–504
Araujo OC, Rosa AS, Fernandes A, Niel C, Villela-Nogueira CA, Pannain V, Araujo NM (2016) RASSF1A and DOK1 promoter methylation levels in hepatocellular Carcinoma, Cirrhotic and Non-Cirrhotic Liver, and Correlation with Liver Cancer in Brazilian Patients. PLoS ONE 11(4):e0153796
Zhang YJ, Wu HC, Shen J, Ahsan H, Tsai WY, Yang HI, Wang LY, Chen SY, Chen CJ, Santella RM (2007) Predicting hepatocellular carcinoma by detection of aberrant promoter methylation in serum DNA. Clin Cancer Res 13(8):2378–2384
Liu ZJ, Huang Y, Wei L, He JY, Liu QY, Yu XQ, Li ZL, Zhang J, Li B, Sun CJ, Liang WB, Sun AM, Qin Y (2017) Combination of LINE-1 hypomethylation and RASSF1A promoter hypermethylation in serum DNA is a non-invasion prognostic biomarker for early recurrence of hepatocellular carcinoma after curative resection. Neoplasma 64(5):795–802
Dong X, He H, Zhang W, Yu D, Wang X, Chen Y (2015) Combination of serum RASSF1A methylation and AFP is a promising non-invasive biomarker for HCC patient with chronic HBV infection. Diagn Pathol 10:133
Sakai M, Hibi K, Kanazumi N, Nomoto S, Inoue S, Takeda S, Nakao A (2005) Aberrant methylation of the CHFR gene in advanced hepatocellular carcinoma. Hepatogastroenterology 52(66):1854–1857
Chen H, Zhang T, Sheng Y, Zhang C, Peng Y, Wang X, Zhang C (2015) Methylation profiling of multiple tumor suppressor genes in hepatocellular carcinoma and the epigenetic mechanism of 3OST2 regulation. J Cancer 6(8):740–749
Lou C, Yang B, Gao YT, Wang YJ, Nie FH, Yuan Q, Zhang CL, Du Z (2008) Aberrant methylation of multiple genes and its clinical implication in hepatocellular carcinoma. Zhonghua Zhong Liu Za Zhi 30(11):831–836
Li CC, Yu Z, Cui LH, Piao JM, Liu M (2014) Role of P14 and MGMT gene methylation in hepatocellular carcinomas: a meta-analysis. Asian Pac J Cancer Prev 15(16):6591–6596
Wang J, Qin Y, Li B, Sun Z, Yang B (2006) Detection of aberrant promoter methylation of GSTP1 in the tumor and serum of Chinese human primary hepatocellular carcinoma patients. Clin Biochem 39(4):344–348
Matsukura S, Soejima H, Nakagawachi T, Yakushiji H, Ogawa A, Fukuhara M, Miyazaki K, Nakabeppu Y, Sekiguchi M, Mukai T (2003) CpG methylation of MGMT and hMLH1 promoter in hepatocellular carcinoma associated with hepatitis viral infection. Br J Cancer 88(4):521–529
Xu G, Zhou X, Xing J, Xiao Y, Jin B, Sun L, Yang H, Du S, Xu H, Mao Y (2020) Identification of RASSF1A promoter hypermethylation as a biomarker for hepatocellular carcinoma. Cancer Cell Int 20(1):547
Chan KC, Lai PB, Mok TS, Chan HL, Ding C, Yeung SW, Lo YM (2008) Quantitative analysis of circulating methylated DNA as a biomarker for hepatocellular carcinoma. Clin Chem 54(9):1528–1536
Nishida N, Kudo M, Nagasaka T, Ikai I, Goel A (2012) Characteristic patterns of altered DNA methylation predict emergence of human hepatocellular carcinoma. Hepatology 56(3):994–1003
Li Y, Cai Y, Chen H, Mao L (2018) Clinical significance and association of GSTP1 hypermethylation with hepatocellular carcinoma: a meta-analysis. J Cancer Res Ther 14(Supplement):S486–S489
Dekervel J, van Pelt J, Verslype C (2015) DNA methylation in hepatocellular carcinoma: What is the use? Hepat Oncol 2(4):321–323
Liu A, Wu Q, Peng D, Ares I, Anadon A, Lopez-Torres B, Martinez-Larranaga MR, Wang X, Martinez MA (2020) A novel strategy for the diagnosis, prognosis, treatment, and chemoresistance of hepatocellular carcinoma: DNA methylation. Med Res Rev 40(5):1973–2018
Hegi ME, Diserens AC, Godard S, Dietrich PY, Regli L, Ostermann S, Otten P, Van Melle G, de Tribolet N, Stupp R (2004) Clinical trial substantiates the predictive value of O-6-methylguanine-DNA methyltransferase promoter methylation in glioblastoma patients treated with temozolomide. Clin Cancer Res 10(6):1871–1874
Acknowledgements
The authors acknowledge the Department of Clinical Biochemistry and Molecular diagnostics, National Liver Institute, Menoufia University, providing the laboratory equipment, microscopy, and the chemicals required to complete the project.
Funding
The authors declare they do not have any financial disclosure.
Author information
Authors and Affiliations
Contributions
AT, DK performed and designed the MSP experiments. AM contributed to pathology reporting, collection of clinical data, and gaining ethical approval. ITS contributed to study concept and involved in protocol development. AK contributed to patient recruitment, evaluation analyzed the data, wrote and edited the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research and the protocols were reviewed by the ethics committees of the National Liver Institute (IRB00003418), Menouffia University and were permitted to comply with the standard international research guidelines. Informed written consents were obtained from all participants.
Consent for publication
Obtained from all participants.
Competing interests
The authors declare they do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tahoon, A., El-Khateeb, D., Mosbeh, A. et al. Significance of promoter methylation of multiple tumor suppressor genes in hepatocellular carcinoma. Egypt J Med Hum Genet 23, 22 (2022). https://doi.org/10.1186/s43042-022-00237-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-022-00237-5