Abstract
Background
Amyotrophic lateral sclerosis (ALS) is a degenerative disease that affects the upper and lower motor neurons. The onset of the disease is frequently focal, usually involving the distal segments of the extremities. A dissociated pattern of muscle atrophy is commonly found in the hands and feet. This study aims to investigate the presence (if any) of split indices in ALS patients and to correlate these indices with confounding factors. A total of 48 people were studied. The control group consists of 24 ALS patients and another 24 age- and gender-matched patients. To assess functional status and muscle strength, the ALS functional rating scale (ALSFRS) and the Medical Research Council (MRC) were used, respectively. Sensory and motor nerve conduction, as well as compound muscle action potential (CMAP) amplitude, were recorded from the muscles of the upper and lower limbs. The electromyographic (EMG) activity of 20 motor unit action potentials (MUAPs) from four different areas was also studied.
Results
Distal CMAP amplitude was reduced in all tested muscles (especially noticed when comparing the reciprocal muscles). In ALS patients, the split foot index (SFI) is significantly higher, while the split elbow index (SEI) is significantly lower. The split foot index (SFI) was found to be negatively related to disease duration, but positively related to ALSFRS scores. The CMAP amplitude was found to be positively related to the MRC score.
Conclusion
Ankle dorsiflexion muscles are more involved (dissociated) than plantar flexor muscles, and elbow flexors are more involved than extensors. SFI correlates significantly with disease duration and ALSFRS scores.
Similar content being viewed by others
Background
Amyotrophic lateral sclerosis (ALS) is a progressive neurological disease that causes muscle weakness and paralysis. As a result of the disease, upper and lower motor neurons degenerate. In limb-onset ALS patients, atrophied muscles and weakness are frequently focal [1]. Early upper motor neuron abnormalities in ALS are mysterious and difficult to identify [2], but they are critical for early prognosis and enrollment in healing treatment trials [3].
Split phenotypes are probably unique to ALS and are distinguished by a shared peripheral input of affected and unaffected muscles. This points to a rostral origin for the spinal cord, most likely within the cerebral cortex. As a result, split phenotypes may indicate ALS upper motor neuron disease [4].
Several split phenotypes have been described, including the split hand, which prefers thenar weakness/wasting over hypothenar weakness/wasting [5], and the split hand plus, which has selective flexor pollicis longus weakness/wasting [6]. Patients who have upper motor neuron involvement may develop a pyramidal pattern of weakness affecting the upper limb flexor muscles [7]. According to recent research, the biceps brachii (BB) muscle in the upper limbs is invariably weaker than the triceps muscle [8,9,10]. A larger study has confirmed the presence of the split elbow phenomenon, albeit contradicting findings have been reported [11, 12].
Lower limb split syndromes (split leg and foot) have received a lot of attention. While some studies [13, 14] emphasize plantar-flexion weakness/wasting over dorsiflexion, others have found the opposite [15, 16].
Our study's goal was to see if ALS patients had any split indices (foot, leg, and elbow). These indices should be correlated with confounding factors (gender, age, location of symptom onset, and disease duration), as well as the ALS Functional Rating Scale (ALSFRS) and MRC scores as clinical tests for muscle power. The amplitude of compound muscular action potentials (CMAPs) recorded from dorsi and planti-flexor leg muscles, as well as elbow flexors and extensors, and their relationship to the various spilt indicators, are investigated.
Methods
From September 2020 to December 2021, a case–control study was conducted in the department of neurology and neurophysiology at Baghdad Teaching Hospital. The Iraqi Board for Medical Specialization approved the study (Decision No. 291; Date 21/1/2021). All participants gave their informed consent.
This study enrolled a total of 48 people. According to the revised El Escorial criteria, 24 of them were diagnosed with ALS by a senior neurologist. They were 16 men and 8 women, with an average age of 56.25 ± 7.72 years. Out of the total 24 patients, 5 were chronic cases and the rest 19 were newly diagnosed. The control group consists of another 24 participants, 14 males and 10 females with a mean age of 55.17 ± 6.76 years. Patients with cervical or lumbosacral root lesions, or those with peripheral neuropathy, diabetes mellitus, alcoholism, or carpal tunnel syndrome, were excluded from the study.
A clinical and neurological examination was performed to determine the duration and location of disease onset, whether it began in the upper limb, lower limb, or bulbar region. The Awaji-Shima consensus group's revised El Escorial criteria were used to categorize the patients as having definite, possible, or probable ALS. Upper motor neuron signs in the upper limbs included increased muscle tone, clonus, increased tendon reflexes, and positive Hoffman signs.
The revised ALSFRS, which has 12 items with 5 scores ranging from 0 to 4, was used to assess patients' functional status over time [17]. The strength of key muscles in the upper and lower extremities was graded on a 0 to 5 scale using the Medical Research Council (MRC) scale against the examiner's resistance [18].
The Nihon Kohden (Japan) EMG machine was used for neurophysiologic testing. During the test procedures, the room temperature was kept between (25–28 °C) and the skin temperature was kept between (32–34 °C) using a skin thermometer.
The tibial and fibular nerves' motor nerve conduction and the median, ulnar, and sural nerves' sensory nerve conduction were studied using standard methods [19]. The musculocutaneous/radial CMAP amplitude ratio measured in the BB and triceps muscles, the tibialis anterior (TA) and gastrocnemius (GC) muscles, and the peroneal/tibial CMAP amplitude ratio measured in the extensor digitorum brevis (EDB) and abductor hallucis (AH) muscles, respectively.
The following were the electrophysiological settings: For motor studies, the band-pass filter was set to 10 Hz to 10 kHz, the sweep speed was set to 5 ms/division, and the sensitivity for recording CMAP responses was set to 5 mV. For sensory studies, the frequency-filter ranges from 20 Hz to 2 kHz, the sweep speed is 2 ms per division, and the sensitivity is 20 V per division.
Concentric needle EMG electrodes were used to study the EMG activity of cranio-bulbar, cervical, thoracic, and lumbosacral muscles, and 20 MUAPs were analyzed for duration and amplitude during rest, minimal, and maximal volitional effort. The following was the setup used in this test: Gain of 200 mV/cm, sweep speed of 20 ms/cm, and band-pass filter frequency range of 20 Hz to 10 kHz.
Statistical analysis
For statistical analysis, Microsoft Excel 2016 and SPSS (statistical package for social sciences) version 25 were used. Continuous data were presented as mean standard deviation, and the unpaired student t-test was used to compare the means of study groups. Receiver operating characteristic (ROC) curve of SFI, SLI, and SEI used to discriminate between patients with ALS and healthy subjects. A p value of less than 0.05 was deemed significant.
Results
The demographic and clinical data of the study population are shown in Table 1. The two groups had comparable age at examination and gender ratios with no significant difference (p = 0.738 and p = 0.551, respectively).
When ALS patients were compared to the control group, the distal CMAP amplitude recorded from all muscles tested was significantly lower (Table 2). When comparing the reciprocal muscles, Table 3 reveals significantly lower distal CMAP amplitude from EDB compared to AH (p < 0.001), TA compared to GC (p < 0.001), and BB compared to triceps (p = 0.017).
Neurophysiological indices were collected from 48 limbs in both the control and patient groups. The median split foot index (SFI) of ALS patients is 0.27, which is significantly lower than the control group's SFI of 0.31 (p = 0.013). Similarly, the median split elbow index (SEI) of ALS patients is 0.75, which is significantly lower than the control group's 1.02 (p < 0.001). On the contrary, the split leg index (SLI) did not differ significantly between the two groups as indicated in Table 4.
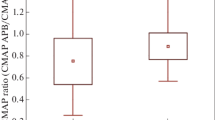
The three indices were not associated with either gender or location of symptom onset (Tables 5). The potential relationships between the three indices and clinical variables were investigated. The SLI and SEI were not related to age at examination, disease duration, or ALSFRS scores. SFI, on the other hand, showed a significant negative correlation with disease duration (r = − 0.311; p = 0.031) and a significant positive correlation with ALSFRS scores (r = 0.351; p = 0.014), but no correlation with age at examination. Furthermore, as shown in Fig. 1, the SFI was positively correlated with the MRC scale score for planter flexion and extension (r = 0.377; p = 0.008 and r = 0.413; p = 0.004, respectively).
The TA muscle's CMAP amplitude was positively correlated with its MRC score (r = 0.573; p < 0.001). Furthermore, the CMAP amplitude recorded from the GC muscle correlates with its MRC score (r = 0.667; p < 0.001). Similarly, the BB muscle's CMAP amplitude correlated positively with its MRC score (r = 0.326; p = 0.024).
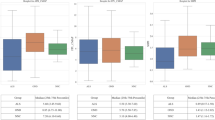
Furthermore, as shown in Fig. 2, the CMAP amplitude recorded from the triceps muscle had a significant positive correlation with its MRC score (r = 0.404; p = 0.004).
The ROC curve of SFI, SLI, and SEI was used in the context of discrimination between patients with ALS and healthy subjects. The area under the curve (AUC) for SFI was 0.645, 95%CI = 0.530–0.759, p = 0.015. The sensitivity and specificity of the test was 60% and 60%, respectively. The best cut-off value of SFI was 0.31. The AUC for SLI was 0.426, 95%CI = 0.307–0.544, p = 0.209. The sensitivity and specificity of the test was 40% and 60%, respectively. The best cut-off value of SLI was 0.44. The AUC for SEI was 0.732, 95%CI = 0.630–0.834, p ≤ 0.001. The sensitivity and specificity of the test was 73% and 60%, respectively. The best cut-off value of SEI was 0.83, as indicated in Fig. 3.
Discussion
Split leg and foot sign is reduced in sufferers with ALS, and the degree of EDB and TA involvement became extra extreme than that of AH and GC muscle tissues involvement. This pattern of dissociated involvement is regular with the findings that patients with ALS had drastically weaker dorsiflexion than plantar flexion. These findings have been also consistent with the commentary that sufferers with ALS generally exhibit foot drop [14].
However, the current study's findings contradict those of Simon and colleagues [15]. The plantar flexors (soleus innervated by the tibial nerve) were found to be more involved in the ALS split-leg pattern than the dorsiflexors (TA innervated by the peroneal nerve).
Our research demonstrated split leg in two versions (leg and foot) with reduced SFI but not SLI in ALS patients versus controls. Despite the fact that studies on this topic are scarce, they generally yield contradictory results to this study [13,14,15,16].
The pathophysiological mechanism that causes more extensive EDB involvement than AH involvement in ALS is unknown. Recent research suggests that ALS has a cortical origin [20] and that corticomotoneuronal (CM) hyperexcitability is a key pathophysiological mechanism of the disease. This backs up Ludolph and colleagues' [11] recent observation that muscles with a stronger CM influence, such as dorsiflexion of the foot, are preferentially affected in ALS. Anterograde glutamate-induced excitotoxicity caused by CM hyperexcitability may result in spinal anterior horn cell degeneration [21, 22].
Jankowska et al. [23] discovered in nonhuman primates that the mean amplitude of monosynaptic excitatory postsynaptic potentials of gastrocnemius–soleus motoneurons was roughly half that of deep peroneal motoneurons, including those of the TA and EDB. This finding implies that the corticospinal projections to peroneal motoneurons were stronger than those to tibial motoneurons.
In men, the population of cortical neurons projecting to TA and EDB motoneurons was more easily stimulated by magnetic stimulation than the population projecting to soleus motoneurons. This finding implies that corticospinal projection densities to the TA and EDB were greater than those to the soleus [24, 25]. Overall, it was hypothesized that differences in corticospinal projection density contribute to the differential involvement of the EDB and AH in ALS.
Previous research has found fewer functional motoneurons innervating the EDB [26] and faster lower motor neuron degeneration in the EDB [27] in ALS, which may be related to the differential lower limb muscle involvement.
Furthermore, a functional magnetic resonance imaging study found that, when compared to plantar flexion, ankle dorsiflexion recruits significantly more of the contralateral primary motor area and supplementary motor area [28].
Furthermore, spinal motoneurons for ankle dorsiflexors, like wrist extensors, have much stronger CM connections than motoneurons for ankle plantar flexion [29]. Furthermore, when walking on a treadmill, studies in normal subjects using transcranial magnetic stimulation show that the TA muscle receives more CM input than the GC [30].
Similarly, for the split elbow sign and index, the BB's CMAP amplitude was lower than the triceps', and the degree of BB involvement was greater than the degree of triceps involvement. This pattern of dissociated involvement is consistent with the discovery that ALS patients had significantly weaker elbow flexion than elbow extension [31].
Several studies found conflicting evidence of the split elbow sign in ALS patients. According to Khalaf and colleagues [8] and Thakore and colleagues [10], the split elbow sign is a feature of ALS, clinically characterized by preferential weakness of the BB muscle over the triceps. Furthermore, MRC scores determined from the BB were significantly lower than triceps MRC scores, and the frequency of preferential BB weakness was significantly higher than triceps muscle weakness. Another study found that ALS patients had a higher proclivity for elbow flexion weakness when compared to elbow extensor weakness [11]. The split elbow sign, on the other hand, was not reported to be a clinical feature in an ALS cohort from Asia [12].
In terms of the mechanism underlying the split elbow phenomenon, CM excitation occurs mono-synaptically to the upper arm BB and triceps, but the connections to the BB are much stronger. The triceps receives a greater proportion of non-CM polysynaptic connections [32, 33]. This distinction explains the split elbow, in which the BB has preferential weakness when compared to the triceps [8, 9].
The mechanisms underlying the development of the split elbow phenomenon are still unknown at the pathophysiological level, though a cortical mechanism has previously been proposed [8, 9, 11]. The "dying forward hypothesis" was proposed as a possible pathogenic mechanism in ALS, in which CM hyperexcitability was thought to mediate neurodegeneration via an anterograde glutaminergic mechanism [34].
Cortical hyperexcitability has been identified as an early and intrinsic feature of ALS [35, 36], correlating with motor neurodegeneration [35] and disease progression patterns [37], and underpinning the development of the split hand phenomenon [38].
Electrophysiological studies in nonhuman primates have established strong CM projection to the BB muscle, which is relevant to the split elbow phenomenon [39]. Transcranial magnetic stimulation studies in humans have revealed that the BB muscle has a higher density of CM inputs than the triceps muscle [40]. Given the BB muscle's greater cortical representation, the possibility of cortical hyperexcitability underlying the development of the split elbow sign in ALS is appealing.
Peripheral mechanisms for the development of the split elbow sign, on the other hand, are not ruled out. Axonal hyperexcitability caused by increased persistent Na + conductance has been proposed as a potential pathogenic mechanism for the split hand sign in ALS [41]. Furthermore, increased physiological dysfunction at the neuromuscular junction and specific metabolic abnormalities at the spinal motor neuron level have been proposed as potential mechanisms for the development of the split hand sign in ALS.
Ludolph and colleagues [11] assessed MRC strength in upper and lower limb muscle pairs, one of which is known to receive a stronger CM drive, in a large cohort of ALS patients. The findings revealed a typical pattern of paresis, with the muscle with the strongest CM input, for example more monosynaptic connections, being weaker (lower MRC score).
Thumb abductors were therefore weaker than elbow extensors, hand extensors were weaker than hand flexors, elbow flexors were weaker than elbow extensors, knee flexors were weaker than extensors, and plantar extensors were weaker than plantar flexors. Preliminary data also show that for the upper limb, muscles with stronger CM connectivity become weaker before other muscles, regardless of onset [10].
Finally, this preferential weakness could reflect cerebral somatotopic muscle representation, which is larger for the BB and EDB muscles. The SEI and SFI would then could reflect a more vulnerability in correlation to the size of the cortical map, supporting a wider concept of a corticofugal mode of neurodegeneration in ALS [25, 34].
The SFI is the lonely index which has a significant relationship with disease duration, ALSFRS-R, and MRC score for plantar flexion and dorsiflexion. Other researchers, on the other hand, discovered no link between SFI and disease duration or ALSFRS-R score [13, 14].
In this study, the CMAP was found to be significantly correlated with the MRC scale. Onesti and colleagues also noticed this [44]. Because the MRC scale measures muscle strength, MUAP dropout results in lower MUAP recruitment [45]. Because fewer anterior horn cells are available to be activated as effort increases, the recruitment frequency (the rate of discharge of one motor unit when an additional motor unit begins to discharge) increases in ALS. The number of motor units firing at any given firing rate is reduced when recruitment is reduced (low MRC scale) due to the loss of anterior horn cells [45].
Conclusion
According to our findings, the ankle dorsiflexion muscle was more involved (dissociated) than the plantar flexor muscle, and the elbow flexors were more involved than the extensors. In ALS patients, total MRC scale scores, ALSFRS scores, and CMAP amplitude were all reduced. The SEI, SFI, and SLI were unrelated to gender or location of symptom onset. The SLI and SEI were not related to age at examination, disease duration, or ALSFRS scores. SFI, on the other hand, demonstrated a significant negative and positive correlation with disease duration and ALSFRS scores, respectively.
One limitation of our study is the small sample size, which could explain the negative statistical results. The study recommends using SFI at the early stages of the disease process because it reaches its peak level earlier as the disease progress. The authors hope that the split phenomenon will prompt non-neuromuscular neurologists to exercise caution when examining a patient with focal weakness and atrophy of the lower or upper extremities.
Availability of data and materials
All data generated or analyzed during this study are included in this published article. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AH:
-
Abductor halluces
- AHC:
-
Anterior horn cell
- ALS:
-
Amyotrophic lateral sclerosis
- ALSFRS:
-
ALS functional rating scale
- AUC:
-
Area under the curve
- BB:
-
Biceps brachii
- CM:
-
Corticomotoneuronal
- CMAP:
-
Compound muscle action potential
- EDB:
-
Extensor digitorum brevis
- GC:
-
Gastrocnemius
- MRC:
-
Medical Research Council
- MUAP:
-
Motor unit action potentials
- ROC:
-
Receiver operating characteristics
- SEI:
-
Split elbow index
- SFI:
-
Split foot index
- SLI:
-
Split leg index
- TA:
-
Tibialis anterior
References
Corcia P, Bede P, Pradat P, Couratier P, Vucic S, de Carvalho M. Split-hand and split-limb phenomena in amyotrophic lateral sclerosis: pathophysiology, electrophysiology and clinical manifestations. J Neurol Neurosurg Psychiatry. 2021;92:1126–30.
Swash M. Why are upper motor neuron signs difficult to elicit in amyotrophic lateral sclerosis? J Neurol Neurosurg Psychiatry. 2012;83:659–62.
Hannaford A, Pavey N, Bos M, Geevasinga N, Menon P, Shefner JM, et al. Diagnostic utility of gold coast criteria in amyotrophic lateral sclerosis. Ann Neurol. 2021;89:979–86.
Eisen A, Bede P. The strength of corticomotoneuronal drive underlies ALS split phenotypes and reflects early upper motor neuron dysfunction. Brain Behav. 2021;11(12): e2403.
Eisen A, Kuwabara S. The split hand syndrome in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2012;83:399–403.
Menon P, Bae JS, Mioshi E, Kiernan MC, Vucic S. Split-hand plus sign in ALS: differential involvement of the flexor pollicis longus and intrinsic hand muscles. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14:315–8.
Wiles CM. Pyramidal weakness. Pract Neurol. 2017;17(3):241–2.
Khalaf R, Martin S, Ellis C, Burman R, Sreedharan J, Shaw C, et al. Relative preservation of triceps over biceps strength in upper limb-onset ALS: The ‘split elbow.’ J Neurol Neurosurg Psychiatry. 2019;90:730–3.
Vucic S. Split elbow sign: more evidence for the importance of cortical dysfunction in ALS. J Neurol Neurosurg Psychiatry. 2019;90:729.
Thakore NJ, Drawert BJ, Lapin BR, Pioro EP. Progressive arm muscle weakness in ALS follows the same sequence regardless of onset site: use of TOMS, a novel analytic method to track limb strength. Amyotroph Lateral Scler Frontotemporal Degener. 2021;22(5–6):380–7.
Ludolph AC, Emilian S, Dreyhaupt J, Rosenbohm A, Kraskov A, Lemon RN, et al. Pattern of paresis in ALS is consistent with the physiology of the corticomotoneuronal projections to different muscle groups. J Neurol Neurosurg Psychiatry. 2020;91:991–8.
Liu J, Wang Z, Shen D, Yang X, Liu M, Cui L. Split phenomenon of antagonistic muscle groups in amyotrophic lateral sclerosis: relative preservation of flexor muscles. Neurol Res. 2021;43:372–80.
Hu F, Jin J, Chen Q, Kang L, Jia R, Qin X, et al. Dissociated lower limb muscle involvement in amyotrophic lateral sclerosis and its differential diagnosis value. Sci Rep. 2019;9:17786.
Wang Z-L, Cui L, Liu M, Zhang K, Liu S, Ding Q, et al. Reassessment of split-leg signs in amyotrophic lateral sclerosis: differential involvement of the extensor digitorum brevis and abductor hallucis muscles. Front Neurol. 2019;10:565.
Simon NG, Lee M, Bae JS, Mioshi E, Lin CS, Pfluger CM, et al. Dissociated lower limb muscle involvement in amyotrophic lateral sclerosis. J Neurol. 2015;262:1424–32.
Min YG, Choi S-J, Hong Y-H, Kim SM, Shin JY, Sung JJ. Dissociated leg muscle atrophy in amyotrophic lateral sclerosis/motor neuron disease: the ’split-leg’ sign. Sci Rep. 2020;10:15661.
Swash M. New ideas on the ALS functional rating scale. J Neurol Neurosurg Psychiatry. 2017;88(5):371–2.
Ciesla N, Dinglas V, Fan E, Kho M, Kuramoto J, Needham D. Manual muscle testing: a method of measuring extremity muscle strength applied to critically ill patients. J Vis Exp. 2011;12(50):3632. https://doi.org/10.3791/2632.
Preston DC, Shapiro BE. Electromyography in neuromuscular disorders. In: Chapter 20: Clinical-Electrophysiologic Correlations. 4th Edn., New York: Elsevier Inc., 2020; p. 329.
Menon P, Kiernan MC, Vucic S. Cortical hyperexcitability precedes lower motor neuron dysfunction in ALS. Clin Neurophysiol. 2015;126:803–9.
Weber M, Eisen A, Stewart H, Hirota N. The split hand in ALS has a cortical basis. J Neurol Sci. 2000;180(1–2):66–70.
Shibuya K, Park SB, Geevasinga N, Menon P, Howells J, Simon NG, et al. Motor cortical function determines prognosis in sporadic ALS. Neurology. 2016;87(5):513–20.
Jankowska E, Padel Y, Tanaka R. Projections of pyramidal tract cells to alpha-motoneurones innervating hind-limb muscles in the monkey. J Physiol. 1975;249(3):637–67.
Brouwer B, Ashby P. Corticospinal projections to lower limb motoneurons in man. Exp Brain Res. 1992;89(3):649–54.
Eisen A, Braak H, Del Tredici K, Lemon R, Ludolph AC, Kiernan MC. Cortical influences drive amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2017;88(11):917–24.
Chroni E, Tendero IS, Punga AR, Stålberg E. Usefulness of assessing repeater F-waves in routine studies. Muscle Nerve. 2012;45(4):477–85.
Baumann F, Henderson RD, Gareth Ridall P, Pettitt AN, McCombe PA. Quantitative studies of lower motor neuron degeneration in amyotrophic lateral sclerosis: evidence for exponential decay of motor unit numbers and the greatest rate of loss at the site of onset. Clin Neurophysiol. 2012;123(10):2092–8.
Trinastic JP, Kautz SA, Mcgregor K, Gregory C, Bowden M, Benjamin MB, et al. An fMRI study of the differences in brain activity during active ankle dorsiflexion and plantarflexion. Brain Imaging Behav. 2010;4(2):121–31.
Bawa P, Chalmers GR, Stewart H, Eisen AA. Responses of ankle extensor and flexor motoneurons to transcranial magnetic stimulation. J Neurophysiol. 2002;88(1):124–32.
Petersen NT, Butler JE, Marchand-Pauvert V, Fisher R, Ledebt A, Pyndt HS, et al. Suppression of EMG activity by transcranial magnetic stimulation in human subjects during walking. J Physiol. 2001;537(Pt2):651–6.
Pavey N, Higashihara M, van den Bos MAJ, Menon P, Vucic S. The split-elbow index: a biomarker of the split elbow sign in ALS. Clin Neurophysiol Pract. 2021;7:16–20.
Brouwer B, Ashby P. Corticospinal projections to upper and lower limb spinal motoneurons in man. Electroencephalogr Clin Neurophysiol. 1990;76(6):509–19.
Palmer E, Ashby P. Corticospinal projections to upper limb motoneurons in humans. J Physiol. 1992;448:397–412.
Eisen A, Kim S, Pant B. Amyotrophic lateral sclerosis (ALS): a phylogenetic disease of the corticomotoneuron? Muscle Nerve. 1992;15(2):219–24.
Vucic S, Kiernan MC. Novel threshold tracking techniques suggest that cortical hyperexcitability is an early feature of motor neuron disease. Brain. 2006;129(Pt 9):2436–46.
Vucic S, Kiernan MC. Cortical excitability testing distinguishes Kennedy’s disease from amyotrophic lateral sclerosis. Clin Neurophysiol. 2008;119(5):1088–96.
Menon P, Geevasinga N, van den Bos M, Yiannikas C, Kiernan MC, Vucic S. Cortical hyperexcitability and disease spread in amyotrophic lateral sclerosis. Eur J Neurol. 2017;24(6):816–24.
Menon P, Kiernan MC, Vucic S. Cortical dysfunction underlies the development of the split-hand in amyotrophic lateral sclerosis. PLoS ONE. 2014;9(1): e87124.
Lemon RN. Descending pathways in motor control. Ann Rev Neurosci. 2008;31(1):195–218.
Neige C, Massé-Alarie H, Gagné M, Bouyer LJ, Mercier C. Modulation of corticospinal output in agonist and antagonist proximal arm muscles during motor preparation. PLoS ONE. 2017;12(11): e0188801.
Shibuya K, Misawa S, Nasu S, Sekiguchi Y, Mitsuma S, Beppu M, et al. Split hand syndrome in amyotrophic lateral sclerosis: different excitability changes in the thenar and hypothenar motor axons. J Neurol Neurosurg Psychiatry. 2013;84(9):969–72.
Kuwabara S, Sonoo M, Komori T, Shimizu T, Hirashima F, Inaba A, et al. Dissociated small hand muscle atrophy in amyotrophic lateral sclerosis: frequency, extent, and specificity. Muscle Nerve. 2008;37(4):426–30.
de Carvalho M, Swash M. The split hand in amyotrophic lateral sclerosis: a possible role for the neuromuscular junction. Amyotroph Lateral Scler Frontotemporal Degener. 2019;20(5–6):368–75.
Onesti E, Gori MC, Ceccanti M, Tartaglia G, Petrucci A, Frasca V, et al. The compound muscle action potential as neurophysiological marker for amyotrophic lateral sclerosis. EC Neurol. 2016;3:509–19.
Joyce NC, Carter GT. Electrodiagnosis in amyotrophic lateral sclerosis. PM R. 2013;5(5 Suppl):S89-95.
Acknowledgements
We thank assistant professor Dr. Qasim Al-Mayah from the Research Medical Unit/College of Medicine/Al-Nahrain University for helping in statistical analysis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All the authors have directly participated in the preparation of this manuscript and have approved the final version submitted. ‘AA’ clinically examined and referring patients with ALS. ‘DM’ did the electrodiagnostic tests. ‘DM’ drafted the manuscript. ‘DM’, ‘AA', conceived the study and participated in its design and interpretation. Both authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Iraqi Board for Medical Specialization (Decision No. 291; Date 21/1/2021). Written consent for participation from all subjects was ensured.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdul-wahab, D.M.A., Al-Mahdawi, A. Split limb phenomenon in amyotrophic lateral sclerosis: electrophysiologic study. Egypt J Neurol Psychiatry Neurosurg 59, 70 (2023). https://doi.org/10.1186/s41983-023-00671-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00671-1