Abstract
Background
To compare Gd-ethoxybenzyl diethylenetriamine pentaacetic acid (Gd-EOB-DTPA)-enhanced magnetic resonance imaging (MRI) and 99mTc-labelled mebrofenin hepatobiliary scintigraphy (HBS) as imaging-based liver function tests after unilateral radioembolisation (RE) in patients with primary or secondary liver malignancies.
Methods
Twenty-three patients with primary or secondary liver malignancies who underwent Gd-EOB-DTPA-enhanced MRI within a prospective study (REVoluTion) were evaluated. REVoluTion was a prospective open-label, non-randomised, therapy-optimising study of patients undergoing right-sided or sequential RE for contralateral liver hypertrophy at a single centre in Germany. MRI and hepatobiliary scintigraphy were performed before RE (baseline) and 6 weeks after (follow-up). This exploratory subanalysis compared liver enhancement on hepatobiliary phase MRI normalised to the spleen (liver-to-spleen ratio (LSR)) and the muscle (liver-to-muscle ratio (LMR)) with mebrofenin uptake on HBS for the total liver (TL) and separately for the right (RLL) and left liver lobe (LLL).
Results
Mebrofenin uptake at baseline and follow-up each correlated significantly with LSR and LMR on MRI for TL (≤ 0.013) and RLL (≤ 0.049). Regarding the LLL, mebrofenin uptake correlated significantly with LMR (baseline, p = 0.013; follow-up, p = 0.004), whereas with LSR, a borderline significant correlation was only seen at follow-up (p = 0.051; p = 0.046).
Conclusion
LSRs and LMR correlate with mebrofenin uptake in HBS. This study indicates that Gd-EOB-DTPA-enhanced MRI and 99mTc-labelled mebrofenin HBS may equally be used to assess an increase in contralateral liver lobe function after right-sided RE.
Relevance statement
MRI may be a convenient and reliable method for assessing the future liver remnant facilitating treatment planning and monitoring of patients after RE-induced hypertrophy induction.
Key points
• Both MRI and HBS can assess liver function after RE.
• Liver enhancement on MRI correlates with mebrofenin uptake on HBS.
• MRI might be a convenient alternative for estimating future liver remnants after hypertrophy induction.
Graphical Abstract

Similar content being viewed by others
Background
Liver surgery plays a vital role in treating liver malignancies. A significant number of patients lack an adequate future liver remnant (FLR) required for surgery, rendering them ineligible despite having resectable tumours [1]. FLR can be increased through a preoperative procedure to render them eligible, such as the established portal vein embolisation, portal vein ligation or associating liver partitioning with portal vein ligation in staged hepatectomy (ALPPS) [2,3,4]. Recent data indicate that unilateral radioembolisation (RE) is also effective in setting the stage for secondary operability in terms of hemihepatectomy with the advantage that it simultaneously represents a therapy of the tumour-affected liver [5,6,7,8,9,10]. Thus, in the case of aggressive tumours, the patient benefits from additional time while also indirectly acquiring predictive information regarding the potential benefits of secondary resection, acting as a “test of time”.
An adequate assessment of FLR after hypertrophy induction is crucial as posthepatectomy liver failure is the most dramatic complication following liver resection [11, 12]. Established methods include liver function testing and different clinical grading systems, such as the Child–Pugh score and the MELD score [13,14,15]. These methods are limited by the influence of extrahepatic factors on the assessments and the inability of attributing functional changes to specific liver regions [16]. The indocyanine green (ICG) clearance test quantifies the liver’s ability to eliminate ICG dye, often serving as a reference standard for global liver function evaluation [17,18,19]. However, this test relies on hepatic blood flow, which can be affected by factors like intrahepatic shunting and is unable to detect regional variations within the liver. Scintigraphic methods, mainly utilising tracers like 99mTc-iminodiacetate analogues such as mebrofenin, have become increasingly established in recent years in clinical practice for evaluating tracer uptake and biliary excretion preoperatively [20,21,22,23]. Dynamic 99mTc-mebrofenin hepatobiliary scintigraphy (HBS) or single-photon emission computed tomography (SPECT) can assess global and regional liver function and predict the FLR [24].
Besides scintigraphic methods, magnetic resonance imaging (MRI) and computed tomography (CT) volumetry are used to evaluate liver regional function with spatial information. However, the relationship between liver metabolic function and volume increase after hypertrophy-inducing procedures remained uncertain for some time [15, 25,26,27,28,29,30]. In the recent prospective REVoluTion study of 23 patients, it was shown that after unilobar RE, there is not only an increase in the volume of the contralateral lobe but also a significant increase in metabolic function as measured by HBS [7].
However, the assessment of liver function is not limited to these more complex methods but can also be estimated relatively easily by liver MRI with hepatocyte-specific contrast agents [19, 31]. MRI of the liver with gadoxetic acid (Gd-ethoxybenzyl diethylenetriamine pentaacetic acid (Gd-EOB-DTPA)) is a standard of care for detection, treatment planning, and follow-up of liver tumours. Several studies have already shown that conclusions about liver function can be drawn from the storage behaviour in the hepatocyte-specific phase, also after procedures like RE or radiation therapy [31,32,33,34,35,36,37,38]. Moreover, MRI measurements have been shown to correlate with HBS measurements, and the assessment of respectability after hypertrophy induction after portal vein embolisation seems possible [39,40,41]. However, it remains uncertain whether these findings can be extrapolated to the assessment of increased metabolic function FLR following one-sided RE.
Therefore, the objective of this post hoc analysis was to compare the utility of static gadoxetic-enhanced MRI and 99mTc-mebrofenin HBS in evaluating changes in liver function after inducing hypertrophy by unilateral RE.
Methods
Study population
This post hoc analysis included all twenty-three patients of the prospective open-label, non-randomised, single-centre, therapy-optimising REVoluTion study [7]. The study was approved by the institutional ethics committee at Otto von Guericke University, Magdeburg (Ref. 08/14) according to the Declaration of Helsinki of 2013, and written informed consent was acquired from each patient. Patients underwent right-sided 90Y-RE for liver malignancies without underlying liver disease or biliary obstruction. They were aged 18–85 with an Eastern Cooperative Oncology Group (ECOG) performance status of 0–2. The exclusion criteria encompassed baseline non-embolised lobe functional volume > 30% of total functional liver volume, liver cirrhosis, pre-existing portal vein thrombosis, primary liver malignancies with cirrhosis or biliary dilatation, prior left liver lobe therapy/surgery or planned within 6 weeks of right-lobar RE, > 10% tumour involvement in left lobe, and contraindications for MRI, 99mTc-mebrofenin HBS, or ICG test [7]. MRI and HBS were performed immediately before (baseline) and 6 weeks after RE (follow-up).
MRI
All patients underwent a standardised MRI protocol with 0.025 mmol/kg/body weight of Gd-EOB-DTPA (Primovist, Bayer Healthcare, Leverkusen, Germany,) on a 1.5-T scanner (Achieva, Philips Healthcare, Best, The Netherlands) using an 8-channel body-phased array coil. A standard axial T1-weighted high-resolution isotropic volume sequence, THRIVE (repetition time 4.0 ms, echo time 2.0 ms, and slice thickness 3 mm), was acquired 20 min after contrast injection (hepatobiliary phase) covering the entire liver. The contrast agent was manually injected in an anterior cubital vein, followed by a saline flush of 20 mL. Images were evaluated by a radiologist (M.S.) with over 15 years of experience in abdominal imaging using OsiriX v.8.0.2 (Pixmeo; Bernex, Switzerland). To prevent measurement bias, the radiologist was blinded to every other data. The mean signal intensity (SI) values of the liver, spleen, and paravertebral muscle were calculated using a manually placed circular region of interest (ROI) with a fixed size of 3 cm2, excluding major artefacts, liver lesions (including tumour), visible blood vessels, and biliary ducts. The mean SI of the liver was measured with four ROIs separately within the healthy parenchyma of each liver lobe (2 ROIs per liver lobe on different slices). One ROI each was located in the paravertebral muscle and spleen (Fig. 1). The mean SI was then calculated for the total liver (TL), the left liver lobe (LLL), and the right liver lobe (RLL). The liver-to-spleen (LSR) and the liver-to-muscle (LMR) ratios were calculated with the following formulas [34]:
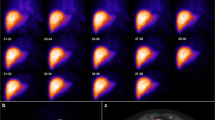
Case example of measurement of gadolinium ethoxy-benzyl diethylenetriamine pentaacetic acid (Gd-EOB-DTPA) uptake after radioembolisation. Regions of interest are placed in the left and right hepatic lobes (red circles), the spleen (not shown), and in the muscle in T1-weighted images obtained 20 min after Gd-EOB-DTPA, before (a) (baseline) and after RE (d) (follow-up). The measured mean signal intensities are used to calculate Gd-EOB-DTPA uptake according to Eqs. 1 and 2 (see the “Methods” section). The mean values at baseline (a) in RLL/LLL: LSR 1.9/1.9; LMR 1.8/1.8. The mean values measured at follow-up (d) in RLL/LLL: LSR 1.6/2.4; LMR 1.9/2.9. c The distribution of Y-90 microspheres in the right hepatic lobe in Bremsstrahlung SPECT/CT. b Baseline and e follow-up show the corresponding HBS SPECT/CT. HBS, Hepatobillary scintigraphy; LLL, Left liver lobe; LMR, Liver-to-muscle ratio; LSR, Liver-to-spleen ratio; RLL, Right liver lobe; SPECT/CT, Single-photon emission computed tomography/computed tomography
99mTc-mebrofenin HBS
HBS was performed using a single-photon emission computed tomography/computed tomography (SPECT/CT) with 99mTc-labelled-(2,4,6-trimethyl-3-bromo) iminodiacetic acid (99mTc-mebrofenin, Bridatec; GE Healthcare, Buchler GmbH & Co. KG, Braunschweig, Germany). After intravenous administration of 150–370 MBq of 99mTc-mebrofenin, dynamic planar imaging within 360 s, followed by rapid SPECT/CT imaging over 240 s, was used to determine the 99mTc-mebrofenin uptake rate (Figs. 2 and 3). SPECT/CT imaging determined the counts within the liver and FLR volume. The percentage of the counts in the FLR in relation to the entire liver was then multiplied by the 99mTc-mebrofenin uptake rate to obtain the actual metabolic function of the FLR. Calculations were performed to normalise the uptake rate to BSA and respective liver volumes (total, left, right) as described before [7]. Additionally, ICG (0.25 mg/kg) was administered intravenously to confirm the HBS findings, and ICG plasma disappearance rate and ICG retention at 15 min were measured non-invasively using a spectrophotometry clip attached to the patient’s index finger, with adjustments made for variations in cardiac output between baseline and follow-up measurements.
Statistical analysis
All statistical analyses were performed using the R statistics software (Version 4.2.3). Continuous and ordinal variables are reported as median (interquartile range) if not otherwise specified, and categorical variables are reported as counts and percentages. Correlations were tested by calculating Pearson correlation coefficients after the normal distribution was checked by normal plots. To indicate statistical significance, p-values < 0.05 were considered.
Results
Baseline characteristics of the analysed 23 patients are shown in Table 1. The median age was 66 (interquartile range 59–74) years, and most patients had metastatic colorectal cancer (11, 48%). The median time from baseline MRI to RE was 20 days (interquartile range 20–40), and the median time from RE to follow-up was 39 days (interquartile range 30–42). The average mebrofenin uptake normalised to body surface area in %/min/m2 dropped significantly between baseline and follow-up in the right liver lobe (5.0 versus 3.9, p = 0.023) whereas it increased in the left liver lobe after RE (1.3 versus 1.6, p = 0.048) (Table 2).
Correlation of LSR with HBS
LSR at baseline and follow-up correlated significantly with mebrofenin uptake for TL (baseline, r2 = 0.635, p < 0.001; follow-up, r2 = 0.462, p = 0.013) and RLL (r2 = 0.597, p = 0.001; r2 = 0.483, p = 0.010). Regarding the LLL, a significant correlation was only seen at follow-up (r2 = 0.349, p = 0.051; r2 = 0.359, p = 0.046) (Table 3).
Correlation of LMR with HBS
LMR at baseline and follow-up correlated significantly with mebrofenin uptake for TL (r2 = 0.473, p = 0.011; r2 = 0.679, p < 0.001), RLL (r2 = 0.353, p = 0.049; r2 = 0.644, p < 0.001), and LLL (r2 = 0.464, p = 0.013; r2 = 0.540, p = 0.004) (Table 3). Figures 2 and 3 show scatterplots.
Correlation between mebrofenin uptake and MRI liver enhancement at baseline. Scatter plots with linear regression lines showing liver-to-spleen-ratio (LSR) versus mebrofenin uptake for right (a) and left (b) liver lobes and total liver (c). Liver-to-muscle-ratio (LMR) for each volume is presented in the same order (d–f)
Correlation between mebrofenin uptake and MRI liver enhancement at follow-up. Scatter plots with linear regression lines showing liver-to-spleen-ratio (LSR) versus mebrofenin uptake for right (a) and left (b) liver lobes and total liver (c). Liver-to-muscle-ratio (LMR) for each volume is presented in the same order (d–f)
Discussion
The utilisation of reliable tests to assess regional liver function represents a desirable advancement, as it has the potential to enhance the accuracy of predicting postoperative liver function. Global liver function tests may not adequately capture regional dysfunction or variations in functional and non-functional liver volume distribution, thereby limiting their ability to accurately predict postoperative liver function after hypertrophy-inducing procedures. For this, image-based methods are of utmost importance whereby HBS has emerged as a type of reference standard in the last few years [42,43,44].
Our study demonstrated a significant correlation between LSR and LMR derived from gadoxetic acid-enhanced MRI and HBS measurements after RE-based hypertrophy induction, suggesting that MRI can serve as a convenient alternative method for estimating FLR. Only the lack of correlation between baseline LSR on MRI and scintigraphy imaging of the LLL raises questions. This could potentially be attributed to artefacts introduced by the proximity of vital organs such as the heart, lungs, and stomach to the relatively small LLL, which might lead to inconsistent signal intensities affecting the accuracy of liver function assessment.
Gadoxetic acid-enhanced MRI has previously shown promising results in predicting post-hepatectomy liver failure, providing accurate anatomical information and reliable assessment of global and regional liver function in a single comprehensive examination [45,46,47]. Moreover, MRI-based liver function evaluation can be seamlessly integrated into routine clinical practice without the need for additional sequences, making it accessible in various medical centres. This accessibility allows patients residing far from specialised liver centres to be monitored locally, minimising the need for travel and facilitating optimal timing of resection. Additionally, the lack of ionising radiation exposure in MRI is advantageous, and gadoxetic acid-enhanced MRI can also contribute to the diagnosis and grading of liver fibrosis, providing valuable information for surgical planning in major hepatectomies [48]. In this regard, gadoxetic acid-enhanced MRI holds the potential to surpass ICG and HBS in the preoperative evaluation of liver function. Back in 2015, Geisel et al. [39] showed a good correlation between HBS and MRI in a cohort and postulated that they may equally be used to separately determine right and left liver lobe function.
To the best of our knowledge, this is the first study to show that this can also be applied in the setting after RE-based hypertrophy induction. It is imperative to acknowledge that the present study can be considered as a preliminary investigation, given the inherent limitations and the need for caution in establishing definitive cutoff values pertaining to the MRI-derived parameters. Existing data in this has predominantly originated from relatively small cohorts, thereby warranting prudence in generalising the findings. Nonetheless, it is not obligatory to employ a mandatory approach, as it is possible to conduct a patient-specific assessment by juxtaposing pre- and post-hypertrophy induction images, thereby providing important information to the FLR estimation. Furthermore, the measurements are susceptible to the influence of multiple factors, encompassing patient-specific variables like patient positioning, technical disparities in MRI machines, differences in imaging protocols, and inherent variability in the measurement techniques employed. However, it is important to recognise that valuable information is embedded in the image data, and we should strive to make use of it. It should also be noted that even with methods considered as standard of care, fluctuations in the predictive power of FLR estimates have been observed. For instance, previous studies have indicated a discrepancy between liver volume growth and liver function, with faster functional increase than volumetric increase after portal vein embolisation, but the opposite trend after the first stage of ALPPS [29, 42, 43, 49].
It must be mentioned that the early assessment timeframe of 6 weeks after RE is atypical as many studies have shown that the volume increases induced in the contralateral lobe by unilobar RE continue to increase for up to 12 months [50,51,52]. The 6-week follow-up period adopted in this study may not have fully captured the peak volume and potential function enhancements, possibly posing a constraint on our findings, which was already discussed in the main study manuscript [4]. Nevertheless, since this was the first prospective study of its kind and considering that a standard waiting period of 6 weeks post-portal vein embolisation as the competing method is typical in preparation for major hepatectomy, the decision to conduct a 6-week follow-up was considered suitable.
In addition to the aforementioned limitations, it should be noted that our study utilised only one reader. However, multiple ROIs were placed and accounted for. Additionally, the assessment was quantitative and not qualitative, contributing to a low potential for interreader reproducibility. Furthermore, it is worth noting that gadoxetic acid-enhanced MRI offers the possibility to derive other quantitative liver function parameters, including T1 relaxometry-based data, which have the potential to provide absolute values for the purpose of broader applicability and therefore may play a pivotal role in further exploring this subject [34]. Regrettably, these sequences entail a higher level of complexity and are not standard in routine liver MRI protocols. Consequently, due to the non-inclusion of these sequences in our study protocol, the exploration of such values was precluded in our analysis. However, it is important to underscore that one of our primary aims was to demonstrate the efficacy of utilising a standard MRI protocol to acquire information about increasing liver function without elongating or complicating the examination duration and protocol. Besides, LMR and LSR are among the most commonly used parameters and are robust in their calculation with high intra- and interobserver reproducibility, as previous studies have demonstrated [53]. In addition, it is essential to establish a correlation between preoperative MRI and mebrofenin HBS parameters, with actual postoperative outcomes, since the association between such surrogate measures and clinically significant events like posthepatectomy liver failure still requires further research with larger cohorts.
In conclusion, our study demonstrates that hepatobiliary phase MRI exhibits a correlation with 99mTc-labelled mebrofenin uptake in HBS following RE-induced hypertrophy. This suggests that Gd-EOB-DTPA-enhanced MRI holds promise as an alternative to HBS, facilitating the assessment of contralateral liver lobe function enhancement after unilateral RE. This shift towards MRI has potential practical implications, as it offers a patient-friendly and environmentally conscious approach by eliminating the need for complex additional investigations.
Availability of data and materials
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
Abbreviations
- ALPPS:
-
Associating liver partition with portal vein ligation for staged hepatectomy
- CT:
-
Computed tomography
- FLR:
-
Future liver remnant
- HBS:
-
Hepatobiliary scintigraphy
- ICG:
-
Indocyanine green
- LLL:
-
Left liver lobe
- LMR:
-
Liver-to-muscle ratio
- LSR:
-
Liver-to-spleen ratio
- MRI:
-
Magnetic resonance imaging
- RLL:
-
Right liver lobe
- ROI:
-
Region of interest
- SI:
-
Signal intensity
- SPECT:
-
Single-photon emission computed tomography
- TL:
-
Total liver
References
Pulitano C, Crawford M, Joseph D, Aldrighetti L, Sandroussi C (2014) Preoperative assessment of postoperative liver function: the importance of residual liver volume. J Surg Oncol 110:445–450. https://doi.org/10.1002/jso.23671
Abulkhir A, Limongelli P, Healey AJ et al (2008) Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg 247:49–57. https://doi.org/10.1097/SLA.0b013e31815f6e5b
Azoulay D, Castaing D, Smail A et al (2000) Resection of nonresectable liver metastases from colorectal cancer after percutaneous portal vein embolization. Ann Surg 231:480–486. https://doi.org/10.1097/00000658-200004000-00005
May BJ, Talenfeld AD, Madoff DC (2013) Update on portal vein embolization: evidence-based outcomes, controversies, and novel strategies. J Vasc Interv Radiol 24:241–254. https://doi.org/10.1016/j.jvir.2012.10.017
Birgin E, Rasbach E, Seyfried S et al (2020) Contralateral liver hypertrophy and oncological outcome following radioembolization with (90)Y-microspheres: a systematic review. Cancers (Basel). https://doi.org/10.3390/cancers12020294
Elias D, De Baere T, Roche A, Mducreux LJ, Lasser P (1999) During liver regeneration following right portal embolization the growth rate of liver metastases is more rapid than that of the liver parenchyma. Br J Surg 86:784–788. https://doi.org/10.1046/j.1365-2168.1999.01154.x
Garlipp B, Amthauer H, Kupitz D et al (2021) The impact of unilateral 90Y-radioembolization on functional changes in the contralateral hepatic lobe: the prospective, open-label radioembolization, volumetry, and liver function measurements (REVoluTion) study. Ann Surg Open 2:e095. https://doi.org/10.1097/as9.0000000000000095
Garlipp B, de Baere T, Damm R et al (2014) Left-liver hypertrophy after therapeutic right-liver radioembolization is substantial but less than after portal vein embolization. Hepatology 59:1864–1873. https://doi.org/10.1002/hep.26947
Hoekstra LT, van Lienden KP, Doets A, Busch OR, Gouma DJ, van Gulik TM (2012) Tumor progression after preoperative portal vein embolization. Ann Surg 256:812–818. https://doi.org/10.1097/SLA.0b013e3182733f09
Teo JY, Allen JC, Ng DCE et al (2018) Prospective study to determine early hypertrophy of the contra-lateral liver lobe after unilobar, yttrium-90, selective internal radiation therapy in patients with hepatocellular carcinoma. Surgery 163:1008–1013. https://doi.org/10.1016/j.surg.2017.10.014
Le Roy B, Dupré A, Gallon A, Chabrot P, Gagnière J, Buc E (2018) Liver hypertrophy: underlying mechanisms and promoting procedures before major hepatectomy. J Visc Surg 155:393–401. https://doi.org/10.1016/j.jviscsurg.2018.03.005
van den Broek MA, Olde Damink SW, Dejong CH et al (2008) Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver Int 28:767–780. https://doi.org/10.1111/j.1478-3231.2008.01777.x
Nagashima I, Takada T, Okinaga K, Nagawa H (2005) A scoring system for the assessment of the risk of mortality after partial hepatectomy in patients with chronic liver dysfunction. J Hepatobiliary Pancreat Surg 12:44–48. https://doi.org/10.1007/s00534-004-0953-0
Schroeder RA, Marroquin CE, Bute BP, Khuri S, Henderson WG, Kuo PC (2006) Predictive indices of morbidity and mortality after liver resection. Ann Surg 243:373–379. https://doi.org/10.1097/01.sla.0000201483.95911.08
Rassam F, Olthof PB, Bennink RJ, van Gulik TM (2017) Current modalities for the assessment of future remnant liver function. Visc Med 33:442–448. https://doi.org/10.1159/000480385
Roberts KJ, Bharathy KG, Lodge JP (2013) Kinetics of liver function tests after a hepatectomy for colorectal liver metastases predict post-operative liver failure as defined by the International Study Group for Liver Surgery. HPB (Oxford) 15:345–351. https://doi.org/10.1111/j.1477-2574.2012.00593.x
Okochi O, Kaneko T, Sugimoto H, Inoue S, Takeda S, Nakao A (2002) ICG pulse spectrophotometry for perioperative liver function in hepatectomy. J Surg Res 103:109–113. https://doi.org/10.1006/jsre.2001.6328
Paumgartner G (1975) The handling of indocyanine green by the liver. Schweiz Med Wochenschr 105:1–30
Yoon JH, Lee JM, Kang HJ et al (2019) Quantitative assessment of liver function by using gadoxetic acid-enhanced MRI: hepatocyte uptake ratio. Radiology 290:125–133. https://doi.org/10.1148/radiol.2018180753
de Graaf W, van Lienden KP, van Gulik TM, Bennink RJ (2010) (99m)Tc-mebrofenin hepatobiliary scintigraphy with SPECT for the assessment of hepatic function and liver functional volume before partial hepatectomy. J Nucl Med 51:229–236. https://doi.org/10.2967/jnumed.109.069724
Gupta M, Choudhury PS, Singh S, Hazarika D (2018) Liver functional volumetry by Tc-99m mebrofenin hepatobiliary scintigraphy before major liver resection: a game changer. Indian J Nucl Med 33:277–283. https://doi.org/10.4103/ijnm.IJNM_72_18
de Graaf W, Bennink RJ, Veteläinen R, van Gulik TM (2010) Nuclear imaging techniques for the assessment of hepatic function in liver surgery and transplantation. J Nucl Med 51:742–752. https://doi.org/10.2967/jnumed.109.069435
de Graaf W, van Lienden KP, Dinant S et al (2010) Assessment of future remnant liver function using hepatobiliary scintigraphy in patients undergoing major liver resection. J Gastrointest Surg 14:369–378. https://doi.org/10.1007/s11605-009-1085-2
Erdogan D, Heijnen BH, Bennink RJ et al (2004) Preoperative assessment of liver function: a comparison of 99mTc-mebrofenin scintigraphy with indocyanine green clearance test. Liver Int 24:117–123. https://doi.org/10.1111/j.1478-3231.2004.00901.x
Memeo R, Conticchio M, Deshayes E et al (2021) Optimization of the future remnant liver: review of the current strategies in Europe. Hepatobiliary Surg Nutr 10:350–363. https://doi.org/10.21037/hbsn-20-394
Nishiyama Y, Yamamoto Y, Hino I, Satoh K, Wakabayashi H, Ohkawa M (2003) 99mTc galactosyl human serum albumin liver dynamic SPET for pre-operative assessment of hepatectomy in relation to percutaneous transhepatic portal embolization. Nucl Med Commun 24:809–817. https://doi.org/10.1097/00006231-200307000-00011
Hirai I, Kimura W, Fuse A, Suto K, Urayama M (2003) Evaluation of preoperative portal embolization for safe hepatectomy, with special reference to assessment of nonembolized lobe function with 99mTc-GSA SPECT scintigraphy. Surgery 133:495–506. https://doi.org/10.1067/msy.2003.138
Yumoto Y, Yagi T, Sato S et al (2010) Preoperative estimation of remnant hepatic function using fusion images obtained by (99m)Tc-labelled galactosyl-human serum albumin liver scintigraphy and computed tomography. Br J Surg 97:934–944. https://doi.org/10.1002/bjs.7025
Olthof PB, Tomassini F, Huespe PE et al (2017) Hepatobiliary scintigraphy to evaluate liver function in associating liver partition and portal vein ligation for staged hepatectomy: liver volume overestimates liver function. Surgery 162:775–783. https://doi.org/10.1016/j.surg.2017.05.022
van der Velden S, Braat M, Labeur TA et al (2019) A pilot study on hepatobiliary scintigraphy to monitor regional liver function in (90)Y radioembolization. J Nucl Med 60:1430–1436. https://doi.org/10.2967/jnumed.118.224394
Yamada A, Hara T, Li F et al (2011) Quantitative evaluation of liver function with use of gadoxetate disodium-enhanced MR imaging. Radiology 260:727–733. https://doi.org/10.1148/radiol.11100586
Kukuk GM, Schaefer SG, Fimmers R et al (2014) Hepatobiliary magnetic resonance imaging in patients with liver disease: correlation of liver enhancement with biochemical liver function tests. Eur Radiol 24:2482–2490. https://doi.org/10.1007/s00330-014-3291-x
Öcal O, Peynircioglu B, Loewe C et al (2022) Correlation of liver enhancement in gadoxetic acid-enhanced MRI with liver functions: a multicenter-multivendor analysis of hepatocellular carcinoma patients from SORAMIC trial. Eur Radiol 32:1320–1329. https://doi.org/10.1007/s00330-021-08218-9
Haimerl M, Verloh N, Zeman F et al (2017) Gd-EOB-DTPA-enhanced MRI for evaluation of liver function: comparison between signal-intensity-based indices and T1 relaxometry. Sci Rep 7:43347. https://doi.org/10.1038/srep43347
Powerski MJ, Scheurig-Münkler C, Hamm B, Gebauer B (2014) Impaired hepatic Gd-EOB-DTPA enhancement after radioembolisation of liver malignancies. J Med Imaging Radiat Oncol 58:472–480. https://doi.org/10.1111/1754-9485.12187
Shimamoto D, Nishie A, Asayama Y et al (2015) MR prediction of liver function and pathology using Gd-EOB-DTPA: effect of liver volume consideration. Biomed Res Int 2015:141853. https://doi.org/10.1155/2015/141853
Sun XL, Jiang X, Kuang Y et al (2019) Potential of Gd-EOB-DTPA as an imaging biomarker for liver injury estimation after radiation therapy. Hepatobiliary Pancreat Dis Int 18:354–359. https://doi.org/10.1016/j.hbpd.2019.05.005
Verloh N, Haimerl M, Zeman F et al (2014) Assessing liver function by liver enhancement during the hepatobiliary phase with Gd-EOB-DTPA-enhanced MRI at 3 Tesla. Eur Radiol 24:1013–1019. https://doi.org/10.1007/s00330-014-3108-y
Geisel D, Lüdemann L, Fröling V et al (2015) Imaging-based evaluation of liver function: comparison of 99mTc-mebrofenin hepatobiliary scintigraphy and Gd-EOB-DTPA-enhanced MRI. Eur Radiol 25:1384–1391. https://doi.org/10.1007/s00330-014-3536-8
Rassam F, Zhang T, Cieslak KP et al (2019) Comparison between dynamic gadoxetate-enhanced MRI and (99m)Tc-mebrofenin hepatobiliary scintigraphy with SPECT for quantitative assessment of liver function. Eur Radiol 29:5063–5072. https://doi.org/10.1007/s00330-019-06029-7
Geisel D, Lüdemann L, Keuchel T et al (2013) Increase in left liver lobe function after preoperative right portal vein embolisation assessed with gadolinium-EOB-DTPA MRI. Eur Radiol 23:2555–2560. https://doi.org/10.1007/s00330-013-2859-1
Tomassini F, D’Asseler Y, Linecker M et al (2020) Hepatobiliary scintigraphy and kinetic growth rate predict liver failure after ALPPS: a multi-institutional study. HPB (Oxford) 22:1420–1428. https://doi.org/10.1016/j.hpb.2020.01.010
Guiu B, Quenet F, Panaro F et al (2020) Liver venous deprivation versus portal vein embolization before major hepatectomy: future liver remnant volumetric and functional changes. Hepatobiliary Surg Nutr 9:564–576. https://doi.org/10.21037/hbsn.2020.02.06
Deshayes E, Piron L, Bouvier A et al (2020) Study protocol of the HYPER-LIV01 trial: a multicenter phase II, prospective and randomized study comparing simultaneous portal and hepatic vein embolization to portal vein embolization for hypertrophy of the future liver remnant before major hepatectomy for colo-rectal liver metastases. BMC Cancer 20:574. https://doi.org/10.1186/s12885-020-07065-z
Wang Q, Wang A, Sparrelid E et al (2022) Predictive value of gadoxetic acid–enhanced MRI for posthepatectomy liver failure: a systematic review. Eur Radiol 32:1792–1803. https://doi.org/10.1007/s00330-021-08297-8
Iimuro Y (2017) ICG clearance test and 99mTc-GSA SPECT/CT fusion images. Visc Med 33:449–454. https://doi.org/10.1159/000479046
Wang Q, Brismar TB, Gilg S et al (2022) Multimodal perioperative assessment of liver function and volume in patients undergoing hepatectomy for colorectal liver metastasis: a comparison of the indocyanine green retention test, (99m)Tc mebrofenin hepatobiliary scintigraphy and gadoxetic acid enhanced MRI. Br J Radiol 95:20220370. https://doi.org/10.1259/bjr.20220370
Norén B, Forsgren MF, Dahlqvist Leinhard O et al (2013) Separation of advanced from mild hepatic fibrosis by quantification of the hepatobiliary uptake of Gd-EOB-DTPA. Eur Radiol 23:174–181. https://doi.org/10.1007/s00330-012-2583-2
Sparrelid E, Jonas E, Tzortzakakis A et al (2017) Dynamic evaluation of liver volume and function in associating liver partition and portal vein ligation for staged hepatectomy. J Gastrointest Surg 21:967–974. https://doi.org/10.1007/s11605-017-3389-y
Goebel J, Sulke M, Lazik-Palm A et al (2017) Factors associated with contralateral liver hypertrophy after unilateral radioembolization for hepatocellular carcinoma. PLoS One 12:e0181488. https://doi.org/10.1371/journal.pone.0181488
Ong F, Tibballs J (2020) Hepatic volume changes post-selective internal radiation therapy with (90) Y microspheres. J Med Imaging Radiat Oncol 64:347–352. https://doi.org/10.1111/1754-9485.13040
Orcutt ST, Abuodeh Y, Naghavi A et al (2018) Kinetic analysis of contralateral liver hypertrophy after radioembolization of primary and metastatic liver tumors. Surgery 163:1020–1027. https://doi.org/10.1016/j.surg.2017.11.020
Beer L, Mandorfer M, Bastati N et al (2019) Inter- and intra-reader agreement for gadoxetic acid-enhanced MRI parameter readings in patients with chronic liver diseases. Eur Radiol 29:6600–6610. https://doi.org/10.1007/s00330-019-06182-z
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
BG, MF, OÖ, RS, FG, and MS did the study design, literature research, data collection, data analysis, data interpretation, article writing, and editing. HA did the data collection, data interpretation, and article review. DK did the data collection, data analysis, data interpretation, and article review. JO, TG, DP-W, AH, OG, DK, JR, and MP did the data collection, data interpretation, and article review.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study, which was conducted according to the Helsinki Declaration of 2013, was approved by the Ethics Committee of Otto von Guericke University, Magdeburg. Informed patient consent was waived due to the retrospective nature of the study.
Preliminary results (abstract) of this study were presented at the European Congress of Radiology, Vienna, Austria, 2023.
Consent for publication
Not applicable.
Competing interests
BG has received research grants from Sirtex Medical as well as lecture honoraria and travel grants from Sirtex Medical, Amgen, Merck, Roche, Novartis, and B. Braun Travacare and received honoraria for participation on the advisory boards from Sirtex Medical and Amgen. HA receives lecture fees from Norgine, Pfizer, Novartis, GE, and Sirtex Medical as well as research grants from Pfizer. JR declares consulting, advisory arrangements, research grants, and travel grants from Sirtex Medical and consulting, advisory arrangements and receiving travel grants from BTG. OO receives honoraria from Bayer. RD receives lecture honoraria from Sirtex Medical. MP declares consulting, served on a speaker’s bureau, and receiving travel grants from Sirtex. MS receives research grants from Bayer and Sirtex Medical and lecture honoraria from Siemens, Cook, Boston Scientific, Sirtex Medical, Falk Foundation, and Bayer. The remaining authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fabritius, M.P., Garlipp, B., Öcal, O. et al. Assessing regional hepatic function changes after hypertrophy induction by radioembolisation: comparison of gadoxetic acid-enhanced MRI and 99mTc-mebrofenin hepatobiliary scintigraphy. Eur Radiol Exp 8, 15 (2024). https://doi.org/10.1186/s41747-023-00409-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41747-023-00409-x