Abstract
An aging population and the increasing prevalence of lifestyle-related diseases have led to a worldwide increase in the rate of chronic kidney disease requiring renal replacement therapy. The mean age of individuals requiring dialysis therapy has been increasing, and Japanese patients are aging more rapidly than those in the USA and Europe. Patients undergoing renal replacement therapy are at increased risk of sarcopenia/frailty compared with people with normal kidney function due to comorbid burden, long-standing malnutrition, chronic inflammation, metabolic acidosis, anabolic resistance, hormonal changes, physical inactivity and amino acid loss via dialysis treatment in addition to aging. Sarcopenia and frailty are serious global health problems that can decrease access to kidney transplantation and lead to various adverse health outcomes, including functional dependence, hospitalizations and deaths in patients on dialysis treatment. However, sarcopenia/frailty fortunately is potentially modifiable by early identification of poor physical functioning, sustainment and enhancement of daily physical activity, and participation in exercise treatments. The Japanese Society of Renal Rehabilitation was established in 2011 and published a clinical practice guideline for “Renal Rehabilitation” targeting nondialysis-dependent and dialysis-dependent patients and renal transplant recipients, in 2019. The guideline emphasized the importance of physical management for patients with kidney diseases in addition to nutritional supports and anemia management. Kidney health professionals should manage sarcopenia and physical frailty as a part of routine clinical care for patients undergoing hemodialysis to improve poor physical functioning, functional dependence, decreased quality of life and poor prognosis.
Similar content being viewed by others
Introduction
An aging population and the increasing prevalence of lifestyle-related diseases have led to a worldwide increase in the rate of chronic kidney disease requiring renal replacement therapy [1]. The mean age of individuals undergoing dialysis therapy has been increasing due to the aging population, improved survival in this patient population, and reduced availability of transplants for older patients. Significant increases in the age of dialysis patients were observed in almost all 12 nations included in the Dialysis Outcomes and Practice Patterns Study (DOPPS), an international cohort study [2]. The DOPPS data also revealed that Japanese patients on dialysis are aging more rapidly than those patients in the USA and Europe [3]. According to the nationwide data of the Japanese Society for Dialysis Therapy, the mean age of the Japanese dialysis population was 68.75 years at the end of 2018, demonstrating a 14.22-year increase since the end of 1990. Furthermore, 78.5% of patients aged 60 years and older started dialysis therapy in 2014, representing 76.7% of the entire dialysis population [4].
The health management of these older patients on hemodialysis poses serious questions, which are not only limited to clinical issues but also involve social issues. The advisory board of the European Renal Best Practice published the guideline on the management of older patients with chronic kidney disease in 2016 [5]. The Japanese Society of Renal Rehabilitation, which was established in 2011, also published a clinical practice guideline for “Renal Rehabilitation” targeting patients who were nondialysis dependent and dialysis dependent and renal transplant recipients in 2019 [6]. In recent years, the concept of renal rehabilitation has become widely known among kidney health providers. However, this information is currently still not included in routine clinical care for patients with chronic kidney disease. This review focused on the understanding of sarcopenia/frailty as a limiting factor of functional status and prognostic factor and management strategies including the evaluation and exercise treatment that kidney health professionals can employ in routine clinical practice.
Functional status
The mortality rate among patients on hemodialysis is approximately 10% for 2018 [4] and still high despite continual improvements in dialysis technology. One of the potential contributors to poor survival status might be the high burden of functional dependence [7], which is defined as an individual’s inability to perform fundamental day-to-day life tasks associated with personal care and maintaining a household. A previous study that included almost all 12 nations demonstrated a high level of disability in daily activities in most patients undergoing hemodialysis, and a dose–response association was noted between poor functional status and adverse clinical outcomes in this population [8]. Furthermore, we examined the association of a change in functional status over a 1-year period with all-cause mortality among 817 Japanese patients who required hemodialysis therapy [9]. Among the patients free of disabilities at baseline, 19.9% experienced a functional decline in their functional status during the 1-year observation, and this reduction was strongly associated with poor prognosis. Importantly, even after adjustment for baseline characteristics, including functional status, the reduction over a 1-year observation period still had a negative effect on survival in patients with end-stage renal disease. We underscored the importance of regular monitoring of patients’ functional status and interventions to prevent deterioration in functional status over time. Impaired mobility, poor physical functioning and muscle weakness, which are the main component elements of physical frailty, contribute to an increased likelihood of disabilities in not only community-dwelling older adults [10, 11] but also patients on hemodialysis [12].
Cycle of frailty
Frailty is generally considered an age-related fragile state characterized by physiologic vulnerability to stress associated with an increased risk of adverse health outcomes [13, 14]. The frailty phenotype was first defined by Fried and colleagues based on the following five criteria: shrinking, weakness, poor endurance and energy, slowness and a low physical activity level [13]. Frailty is identified by the presence of three or more of the above components, and an intermediate frailty phenotype is commonly defined as having one or two of these conditions. Satake et al. proposed the revised Japanese version of the Cardiovascular Health Study criteria (the J-CHS criteria) (Table 1) [15], which was constructed by modifying the original CHS criteria to be simpler and suited to Japanese older adults.
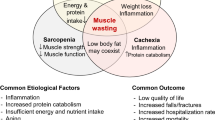
Frailty is highly prevalent in patients with chronic kidney disease who require hemodialysis therapy, and the prevalence rate of frailty in this population was 36.8% based on a previously performed meta-analysis [16] compared with 7.4% in Japanese older individuals without kidney diseases [17]. Many factors are mutually connected and can be unified theoretically into a cycle of frailty [13] (Fig. 1). Patients with kidney diseases are at increased risk of sarcopenia and physical frailty compared with individuals with normal kidney function due to comorbid burden, long-standing malnutrition, chronic inflammation, metabolic acidosis, anabolic resistance, hormonal changes, physical inactivity and amino acid loss via dialysis treatment [18,19,20,21]. Sarcopenia and physical frailty are serious global health problems that can decrease access to kidney transplantation [22] and lead to various adverse health outcomes, including hospitalizations [23] and death [24] in patients on hemodialysis. Thus, early identification and early treatment of sarcopenia and physical frailty are especially needed for these populations to interrupt the vicious cycle.

modified from Fried et al. [13])
Cycle of frailty in patients on hemodialysis (
Management of physical frailty
The European Renal Best Practice guideline development group underscored the importance of managing older patients with chronic kidney disease in 2016, especially with routine assessment of physical function and physical activity [5]. Early identification of poor physical function and physical inactivity is essential to establish a comprehensive management plan for patients on hemodialysis. We have recommended the clinical algorithm of management of physical frailty for patients who require hemodialysis therapy (Fig. 2) [25]. This algorithm is a modified version of Roshanravan’s algorithm [26] tailored to Japanese populations. The algorithm consists of understanding a patient’s physical function and physical activity level and exercise interventions. In patients with decreased physical function and/or a sedentary lifestyle who were screened by routine evaluation, we encouraged them to participate in supervised and/or home-based exercise programs. We had previously evaluated the effects of participation in a program for regular management of physical frailty, which consists of routine assessment of physical function and activity with feedback, on the results on all-cause mortality and cardiovascular events in patients on hemodialysis [27]. As a result, a lower proportion of program attendance was strongly associated with increased risks of mortality and cardiovascular events compared to those who attended the program more regularly. These results emphasized the importance of managing their physical function and activity regularly as part of routine care to improve their prognosis.
Physical function
Poor physical functioning, especially leg muscle strength, is common among patients treated with hemodialysis and strongly associated with decreased walking ability and increased risks of developing disability in basic and instrumental activities of daily living [28], which is associated with an elevated risk of mortality [9]. We previously evaluated lower extremity muscle strength using a handheld dynamometer in 190 patients undergoing hemodialysis who were clinically stable and did not require walking assistance, and approximately half of participants had muscle strength less than the cutoff value [29], and this value is used to determine whether patients are able to walk independently or dependently. This finding indicates that decreased muscle strength is already be present in patients undergoing hemodialysis before they exhibit walking difficulty. Given that lower extremity muscle strength was strongly and positively correlated with gait speed and standing balance function [29], maintaining leg muscle strength seems to be a critical factor in the prevention of fall incidence, fall-related fracture and bedridden status. Fortunately, poor muscle strength is modifiable by resistance training in patients on hemodialysis. Low-intensity strength training with ankle weights during dialysis sessions was shown to improve physical performance, physical activity and functional status in aged patients requiring hemodialysis via the improvement of leg muscle strength [12].
Physical activity
Patients on hemodialysis remain substantially less active than the general population with normal kidney function. Decreased physical activity assessed by questionnaire [30,31,32,33,34] or accelerometer-based methods [35, 36] is strongly associated with higher mortality risk among patients who require maintenance hemodialysis therapy. Goal setting is well known as a key motivational factor for increasing physical activity levels and is absolutely essential for successful intervention. We propose 4,000 steps per nondialysis day as an initial minimum recommendation of physical activity for mobility disability-free patients who require no assistance in walking from another person (Fig. 3) [36]. This is a realistic and specific goal consistent with the recommendations of the American College of Sports Medicine, which recommends 4,000 steps per day for older adults [37]. In addition, a decline in physical activity over time, which was defined as a decrease in activity of > 30% compared to activity at 1 year before, was observed in almost one-quarter of patients undergoing hemodialysis and was associated with elevated mortality risk independent of patient characteristics and baseline activity level [38]. On the other hand, we recently revealed that a lower physical activity level on “dialysis days” was also associated with higher risks of cardiovascular events and all-cause death independent of that on nondialysis days [39]. Physical activity on dialysis days is restricted due to large fluctuations in vital signs during hemodialysis treatment or symptoms, such as fatigue [40], and it is necessary to investigate in detail the cause of decreased physical activity on dialysis days and to fully consider whether intradialytic exercise could be safely performed to cover the shortfall.
Kaplan–Meier analysis of survival for 282 patients on hemodialysis. The thick dark line shows patients with physical activity greater than 4000 steps per nondialysis day at baseline, and the dotted line indicates those with lower values (Matsuzawa et al. [36])
Evidence of exercise intervention
Regarding the various risk factors for sarcopenia and physical frailty, poor physical functioning can be modified by any exercise interventions. A previously reported multicenter, randomized trial in patients on dialysis called the “EXCITE trial” revealed that a simple, personalized, low-intensity, home-based exercise program improved functional status, including muscle strength and exercise capacity, compared with standard care in these populations [41]. Additionally, the analysis restricted to patients who completed the 6-month intervention revealed that hospitalization-free survival was significantly lower in the exercise group than in the control group [41]. Home-based exercise produces the same degree of improvement as supervised intradialytic exercise in the physical functioning of patients on hemodialysis [42]. However, even if adherence control and motivation support were included in this home-based exercise program, the study participants completed only 53% of the proposed sessions [42]. Hence, when we encourage patients on hemodialysis with sarcopenia, physical frailty, any disabilities in activities of daily living or low adherence/motivation to exercise, it would be better for these patients to adopt a supervised exercise program that does not involve home-based exercise.
Our systematic review conducted in 2017 focused on the efficacy of supervised exercise intervention and included 30 comparisons. The main goals of our review were (1) to update the evidence of supervised exercise interventions for patients undergoing hemodialysis by adding data from recent research studies and (2) to compare the benefits of supervised exercise training programs on exercise tolerance, walking ability, lower extremity muscle strength and health-related quality of life between nonelderly and elderly people [43]. Although we could not establish evidence of exercise treatment for aged patients given the limited number of trials, we confirmed that supervised exercise training had significant beneficial effects on exercise tolerance, walking ability, muscle strength and quality of life in the overall population on hemodialysis (Figs. 4, 5, 6, 7). As of late 2019, there were at least 19 systematic reviews and meta-analyses examining the efficacy of exercise interventions for patients with end-stage renal disease, which consistently showed the availability of the intervention [6, 43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58]. The Japanese Society of Renal Rehabilitation strongly recommends exercise therapy for patients on hemodialysis based on previous evidence [6].
Recent studies have evaluated the effect of neuromuscular electrical stimulation applied during hemodialysis (30 to 60 min per session, two to three times weekly) on functional capacity and lower extremity muscle strength in patients with kidney disease and represented an overall safe and effective strategy for the improvement of these outcomes [59, 60]. Furthermore, protein energy wasting cannot be disregarded, and it is likely to predispose patients to sarcopenia/frailty via loss of skeletal muscle mass and strength. Our study confirmed that physical function slightly improved with nutritional support alone for patients on hemodialysis [61]. To improve physical function more effectively in patients on hemodialysis, exercise intervention should be administered in combination with nutritional interventions [62, 63].
The best method among resistance and aerobic training, nutritional support, exercise during or pre/postdialysis, and neuromuscular electrical stimulation must be selected to improve patient clinical outcomes based on patients’ characteristics, including physical function, comorbid condition, nutritional status, and motivation/adherence to exercise.
Summary
The mortality rates among patients on hemodialysis remain high, and one of the potential contributors to this high rate might be the high burden of functional dependence. This is caused by impaired mobility, poor physical functioning and muscle weakness, which are the main component elements of sarcopenia and physical frailty. We showed that active attendance at routine evaluation of physical function and activity reduced mortality and resulted in fewer fatal and nonfatal cardiovascular events compared with those who do not participate in such evaluation. We also showed the positive effects of exercise training on exercise capacity, walking ability, muscle strength and quality of life in patients on hemodialysis. Although the concept of Renal Rehabilitation has become widely known among kidney health providers in recent years, effort still has not been focused on routine clinical care for patients with chronic kidney disease. Kidney health professionals should take serious efforts to manage sarcopenia and physical frailty based on strategies consisting of evaluation of their physical function/activity and exercise treatment as a part of routine clinical care to improve the poor physical functioning, functional dependence, decreased quality of life and poor prognosis of patients with chronic kidney disease.
Availability of data and materials
Not applicable.
Abbreviations
- CKD:
-
Chronic kidney disease
- DOPPS:
-
Dialysis Outcomes and Practice Patterns Study
- CHS:
-
Cardiovascular Health Study
References
Hamer RA, El Nahas AM. The burden of chronic kidney disease. BMJ. 2006;332:563–4.
Canaud B, Tong L, Tentori F, Akiba T, Karaboyas A, Gillespie B, et al. Clinical practices and outcomes in elderly hemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Clin J Am Soc Nephrol. 2011;6:1651–62.
Kimata N, Tsuchiya K, Akiba T, Nitta K. Differences in the characteristics of dialysis patients in Japan compared with those in other countries. Blood Purif. 2015;40:275–9.
Nitta K, Goto S, Masakane I, Hanafusa N, Taniguchi M, Hasegawa T, et al. Annual dialysis data report for 2018, JSDT Renal Data Registry: survey methods, facility data, incidence, prevalence, and mortality. Renal Replacement Ther. 2020;6:41.
Farrington K, Covic A, Aucella F, Clyne N, de Vosfaf L, Findlay A, et al. Clinical Practice Guideline on management of older patients with chronic kidney disease stage 3b or higher (eGFR <45 mL/min/1.73 m2). Nephrol Dial Transplant. 2016;31:1–66.
Yamagata K, Hoshino J, Sugiyama H, Hanafusa N, Shibagaki Y, Komatsu Y, et al. Clinical practice guideline for renal rehabilitation: systematic reviews and recommendations of exercise therapies in patients with kidney diseases. Renal Replacement Ther. 2019. https://doi.org/10.1186/s41100-019-0209-8.
Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med. 2009;361:1539–47.
Jassal SV, Karaboyas A, Comment LA, Bieber BA, Morgenstern H, Sen A, et al. Functional dependence and mortality in the international Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2016;67:283–92.
Matsuzawa R, Kamitani T, Roshanravan B, Fukuma S, Joki N, Fukagawa M. Decline in the functional status and mortality in patients on hemodialysis: results from the Japan Dialysis Outcome and Practice Patterns Study. J Ren Nutr. 2019;29:504–10.
Heiland EG, Welmer AK, Wang R, Santoni G, Angleman S, Fratiglioni L, et al. Association of mobility limitations with incident disability among older adults: a population-based study. Age Ageing. 2016;45:812–9.
Goto R, Watanabe H, Haruta J, Tsutsumi M, Yokoya S, Maeno T. Identification of prognostic factors for activities of daily living in elderly patients after hospitalization for acute infectious disease in Japan: a 6-month follow-up study. Geriatr Gerontol Int. 2017. https://doi.org/10.1111/ggi.13227.
Chen JL, Godfrey S, Ng TT, Moorthi R, Liangos O, Ruthazer R, et al. Effect of intra-dialytic, low-intensity strength training on functional capacity in adult haemodialysis patients: a randomized pilot trial. Nephrol Dial Transplant. 2010;25:1936–43.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:146–56.
Walston J, Hadley EC, Ferrucci L, Guralnik JM, Newman AB, Studenski SA, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc. 2006;54:991–1001.
Satake S, Arai H. The revised Japanese version of the Cardiovascular Health Study criteria (revised J-CHS criteria). Geriatr Gerontol Int. 2020;20:992–3.
Kojima G. Prevalence of frailty in end-stage renal disease: a systematic review and meta-analysis. Int Urol Nephrol. 2017;49:1989–97.
Kojima G, Iliffe S, Taniguchi Y, Shimada H, Rakugi H, Walters K. Prevalence of frailty in Japan: a systematic review and meta-analysis. J Epidemiol. 2017;27:347–53.
Hendriks FK, Smeets JSJ, van der Sande FM, Kooman JP, van Loon LJC. Dietary protein and physical activity interventions to support muscle maintenance in end-stage renal disease patients on hemodialysis. Nutrients. 2019;11:2972.
Vettoretti S, Caldiroli L, Armelloni S, Ferrari C, Cesari M, Messa P. Sarcopenia is associated with malnutrition but not with systemic inflammation in older persons with advanced CKD. Nutrients. 2019;11:1378.
Kim JK, Choi SR, Choi MJ, Kim SG, Lee YK, Noh JW, et al. Prevalence of and factors associated with sarcopenia in elderly patients with end-stage renal disease. Clin Nutr. 2014;33:64–8.
Gungor O, Ulu S, Hasbal NB, Anker SD, Kalantar-Zadeh K. Effects of hormonal changes on sarcopenia in chronic kidney disease: where are we now and what can we do? J Cachexia Sarcopenia Muscle. 2021. https://doi.org/10.1002/jcsm.12839.
Haugen CE, Chu NM, Ying H, Warsame F, Holscher CM, Desai NM, et al. Frailty and access to kidney transplantation. Clin J Am Soc Nephrol. 2019;14:576–82.
McAdams-DeMarco MA, Law A, Salter ML, Boyarsky B, Gimenez L, Jaar BG, et al. Frailty as a novel predictor of mortality and hospitalization in individuals of all ages undergoing hemodialysis. J Am Geriatr Soc. 2013;61:896–901.
Alfaadhel TA, Soroka SD, Kiberd BA, Landry D, Moorhouse P, Tennankore KK. Frailty and mortality in dialysis: evaluation of a clinical frailty scale. Clin J Am Soc Nephrol. 2015;10:832–40.
Matsuzawa R, Roshanravan B. Management of physical frailty in patients requiring hemodialysis therapy. Contrib Nephrol. 2018;196:101–9.
Roshanravan B, Gamboa J, Wilund K. Exercise and CKD: skeletal muscle dysfunction and practical application of exercise to prevent and treat physical impairments in CKD. Am J Kidney Dis. 2017;69:837–52.
Yamamoto S, Matsuzawa R, Abe Y, Hoshi K, Yoneki K, Harada M, et al. Utility of regular management of physical activity and physical function in hemodialysis patients. Kidney Blood Press Res. 2018;43:1505–15.
Kojima G. Quick and simple FRAIL Scale predicts incident Activities of Daily Living (ADL) and Instrumental ADL (IADL) disabilities: a systematic review and meta-analysis. J Am Med Dir Assoc. 2018;19:1063–8.
Matsuzawa R, Matsunaga A, Wang G, Yamamoto S, Kutsuna T, Ishii A, et al. Relationship between lower extremity muscle strength and all-cause mortality in Japanese patients undergoing dialysis. Phys Ther. 2014;94:947–56.
Johansen KL, Kaysen GA, Dalrymple LS, Grimes BA, Glidden DV, Anand S, et al. Association of physical activity with survival among ambulatory patients on dialysis: the Comprehensive Dialysis Study. Clin J Am Soc Nephrol. 2013;8:248–53.
Lopes AA, Lantz B, Morgenstern H, Wang M, Bieber BA, Gillespie BW, et al. Associations of self-reported physical activity types and levels with quality of life, depression symptoms, and mortality in hemodialysis patients: the DOPPS. Clin J Am Soc Nephrol. 2014;9:1702–12.
O’Hare AM, Tawney K, Bacchetti P, Johansen KL. Decreased survival among sedentary patients undergoing dialysis: results from the dialysis morbidity and mortality study wave 2. Am J Kidney Dis. 2003;41:447–54.
Stack AG, Molony DA, Rives T, Tyson J, Murthy BV. Association of physical activity with mortality in the US dialysis population. Am J Kidney Dis. 2005;45:690–701.
Tentori F, Elder SJ, Thumma J, Pisoni RL, Bommer J, Fissell RB, et al. Physical exercise among participants in the Dialysis Outcomes and Practice Patterns Study (DOPPS): correlates and associated outcomes. Nephrol Dial Transplant. 2010;25:3050–62.
Matsuzawa R, Matsunaga A, Wang G, Kutsuna T, Ishii A, Abe Y, et al. Habitual physical activity measured by accelerometer and survival in maintenance hemodialysis patients. Clin J Am Soc Nephrol. 2012;7:2010–6.
Matsuzawa R, Roshanravan B, Shimoda T, Mamorita N, Yoneki K, Harada M, et al. Physical activity dose for hemodialysis patients: where to begin? Results from a prospective cohort study. J Ren Nutr. 2018;28:45–53.
Chodzko-Zajko WJ. ACSM’s exercise for older asults. 1st ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2014.
Shimoda T, Matsuzawa R, Yoneki K, Harada M, Watanabe T, Matsumoto M, et al. Changes in physical activity and risk of all-cause mortality in patients on maintence hemodialysis: a retrospective cohort study. BMC Nephrol. 2017;18:154.
Yamamoto S, Matsuzawa R, Hoshi K, Harada M, Watanabe T, Suzuki Y, et al. Impact of physical activity on dialysis and nondialysis days and clinical outcomes among patients on hemodialysis. J Ren Nutr. 2021;31:380–8.
Debnath S, Rueda R, Bansal S, Kasinath BS, Sharma K, Lorenzo C. Fatigue characteristics on dialysis and non-dialysis days in patients with chronic kidney failure on maintenance hemodialysis. BMC Nephrol. 2021;22:112.
Manfredini F, Mallamaci F, D’Arrigo G, Baggetta R, Bolignano D, Torino C, et al. Exercise in patients on dialysis: a multicenter, randomized clinical trial. J Am Soc Nephrol. 2017;28:1259–68.
Ortega-Perez de Villar L, Martinez-Olmos FJ, Perez-Dominguez FB, Benavent-Caballer V, Montanez-Aguilera FJ, Mercer T, et al. Comparison of intradialytic versus home-based exercise programs on physical functioning, physical activity level, adherence, and health-related quality of life: pilot study. Sci Rep. 2020;10:8302.
Matsuzawa R, Hoshi K, Yoneki K, Harada M, Watanabe T, Shimoda T, et al. Exercise training in elderly people undergoing hemodialysis: a systematic review and meta-analysis. Kidney Int Rep. 2017;2:1096–110.
Zhao QG, Zhang HR, Wen X, Wang Y, Chen XM, Chen N, et al. Exercise interventions on patients with end-stage renal disease: a systematic review. Clin Rehabil. 2019;33:147–56.
Salhab N, Karavetian M, Kooman J, Fiaccadori E, El Khoury CF. Effects of intradialytic aerobic exercise on hemodialysis patients: a systematic review and meta-analysis. J Nephrol. 2019;32:549–66.
Pu J, Jiang Z, Wu W, Li L, Zhang L, Li Y, et al. Efficacy and safety of intradialytic exercise in haemodialysis patients: a systematic review and meta-analysis. BMJ Open. 2019;9:e020633.
Lu Y, Wang Y, Lu Q. Effects of exercise on muscle fitness in dialysis patients: a systematic review and meta-analysis. Am J Nephrol. 2019;50:291–302.
Huang M, Lv A, Wang J, Xu N, Ma G, Zhai Z, et al. Exercise training and outcomes in hemodialysis patients: systematic review and meta-analysis. Am J Nephrol. 2019;50:240–54.
Ferreira GD, Bohlke M, Correa CM, Dias EC, Orcy RB. Does intradialytic exercise improve removal of solutes by hemodialysis? A systematic review and meta-analysis. Arch Phys Med Rehabil. 2019;100:2371–80.
Clarkson MJ, Bennett PN, Fraser SF, Warmington SA. Exercise interventions for improving objective physical function in patients with end-stage kidney disease on dialysis: a systematic review and meta-analysis. Am J Physiol Renal Physiol. 2019;316:856–72.
Young HML, March DS, Graham-Brown MPM, Jones AW, Curtis F, Grantham CS, et al. Effects of intradialytic cycling exercise on exercise capacity, quality of life, physical function and cardiovascular measures in adult haemodialysis patients: a systematic review and meta-analysis. Nephrol Dial Transplant. 2018;33:1436–45.
Gomes Neto M, de Lacerda FFR, Lopes AA, Martinez BP, Saquetto MB. Intradialytic exercise training modalities on physical functioning and health-related quality of life in patients undergoing maintenance hemodialysis: systematic review and meta-analysis. Clin Rehabil. 2018;32:1189–202.
Shimoda T, Matsuzawa R, Hoshi K, Yoneki K, Harada M, Watanabe T, et al. Effects of supervised exercise on depressive symptoms in hemodialysis Patients: 2 a systematic review and meta-analysis of randomized controlled trials. Renal Replacement Ther. 2017. https://doi.org/10.1186/s41100-017-0136-5.
Chung YC, Yeh ML, Liu YM. Effects of intradialytic exercise on the physical function, depression and quality of life for haemodialysis patients: a systematic review and meta-analysis of randomised controlled trials. J Clin Nurs. 2017;26:1801–13.
Heiwe S, Jacobson SH. Exercise training in adults with CKD: a systematic review and meta-analysis. Am J Kidney Dis. 2014;64:383–93.
Smart N, Steele M. Exercise training in haemodialysis patients: a systematic review and meta-analysis. Nephrology (Carlton). 2011;16:626–32.
Bogataj S, Pajek M, Pajek J, Buturovic Ponikvar J, Paravlic A. Exercise-based interventions in hemodialysis patients: a systematic review with a meta-analysis of randomized controlled trials. J Clin Med. 2019;9:43.
Ferrari F, Helal L, Dipp T, Soares D, Soldatelli A, Mills AL, et al. Intradialytic training in patients with end-stage renal disease: a systematic review and meta-analysis of randomized clinical trials assessing the effects of five different training interventions. J Nephrol. 2020;33:251–66.
Schardong J, Stein C, Della Mea Plentz R. Neuromuscular electrical stimulation in chronic kidney failure: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2020;101:700–11.
Valenzuela PL, Morales JS, Ruilope LM, de la Villa P, Santos-Lozano A, Lucia A. Intradialytic neuromuscular electrical stimulation improves functional capacity and muscle strength in people receiving haemodialysis: a systematic review. J Physiother. 2020;66:89–96.
Matsuzawa R, Yamamoto S, Suzuki Y, Abe Y, Harada M, Shimoda T, et al. The effects of amino acid/protein supplementation in patients undergoing hemodialysis: a systematic review and meta-analysis of randomized controlled trials. Clin Nutr ESPEN. 2021;44:114–21.
Jeong JH, Biruete A, Tomayko EJ, Wu PT, Fitschen P, Chung HR, et al. Results from the randomized controlled IHOPE trial suggest no effects of oral protein supplementation and exercise training on physical function in hemodialysis patients. Kidney Int. 2019;96:777–86.
Martin-Alemany G, Valdez-Ortiz R, Olvera-Soto G, Gomez-Guerrero I, Aguire-Esquivel G, Cantu-Quintanilla G, et al. The effects of resistance exercise and oral nutritional supplementation during hemodialysis on indicators of nutritional status and quality of life. Nephrol Dial Transplant. 2016;31:1712–20.
Acknowledgements
Not applicable.
Funding
This work was supported by research funding from the Hyogo University of Health Sciences, Japan (RM) and the JSPS KAKENHI: 20K19332, Japan (RM).
Author information
Authors and Affiliations
Contributions
The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent participate
No ethical approval is required because this study does not include confidential personal data and does not involve patient intervention.
Consent for publication
The author consents to publish the entire text of this dissertation.
Competing interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Matsuzawa, R. Renal rehabilitation as a management strategy for physical frailty in CKD. Ren Replace Ther 8, 3 (2022). https://doi.org/10.1186/s41100-022-00393-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-022-00393-9