Abstract
Neuropathic pain is a disease of the somatosensory system that is characterized by tingling, burning, and/or shooting pain. Medication is often the primary treatment, but it can be costly, thus there is an interest in understanding alternative low-cost treatments such as exercise. The following review includes an overview of the preclinical and clinical literature examining the influence of exercise on neuropathic pain. Preclinical studies support the hypothesis that exercise reduces hyperalgesia and allodynia in animal models of neuropathic pain. In human research, observational studies suggest that those who are more physically active have lower risk of developing neuropathic pain compared to those who are less active. Exercise studies suggest aerobic exercise training (e.g., 16 weeks); a combination of aerobic and resistance exercise training (e.g., 10–12 weeks); or high-intensity interval training (e.g., 15 weeks) reduces aspects of neuropathic pain such as worst pain over the past month, pain over the past 24 h, pain scores, or pain interference. However, not all measures of pain improve following exercise training (e.g., current pain, heat pain threshold). Potential mechanisms and future directions are also discussed to aid in the goal of understanding the role of exercise in the management of neuropathic pain. Future research using standardized methods to further understanding of the dose of exercise needed to manage neuropathic pain is warranted.
Similar content being viewed by others
Key Points
-
Animal studies demonstrate exercise training reduces pain behaviors (i.e., mechanical and thermal hyperalgesia and/or allodynia) in models of neuropathic pain.
-
Human studies suggest moderate aerobic exercise training, combined aerobic and resistance exercise training, or high-intensity interval training reduces some, but not all, measures of neuropathic pain.
-
Potential mechanisms of these effects include microglial activity, inflammatory markers, heat shock protein 72, neurotrophins, neurotransmitters, the opioid system, and the endocannabinoid system.
Background
According to the International Association for the Study of Pain, neuropathic pain “is caused by a lesion or disease of the somatosensory system” and is typically characterized by spontaneous numbness, tingling/shooting, or burning pain. Neuropathic pain is difficult to treat, and few patients experience full relief. The complicated treatment and symptom burden of chronic neuropathic pain often comes with high economic burden. In fact, annual costs related to neuropathic pain (i.e., painful diabetic neuropathy; small fiber neuropathy; and neuropathic pain resulting from human immunodeficiency virus, HIV; spinal cord injury, SCI; chronic low back pain; or surgery/trauma) in 2011–2012 were estimated to be 27,259 US dollars per patient [1]. Thus, it is imperative to determine low cost and effective treatments to lessen this burden.
Neuropathic pain arises from damage or threat of damage to the somatosensory system that leads to maladaptive nociception [2,3,4]. Under normal conditions, nociception is activated when one encounters a damaging stimulus (i.e., touching a hot stove), under threat of damage, or upon tissue injury which activates protective responses (i.e., hand withdrawal from stove, healing response to injured site). Once a damaging stimulus is sensed, nociceptive neurons send signals from the site of injury (i.e., peripheral nerves), through the dorsal root ganglion (DRG), to the spinal cord (i.e., dorsal horn), which ultimately transports signals to the brain (i.e., ascending control). These ascending inputs are processed centrally, and descending outputs are carried down through the spinal cord and back to the dorsal horn to modulate pain signals (i.e., descending control) through excitatory and inhibitory neurons. Typically, ascending nociceptive signals cease once the stimulus (i.e., heat, tissue injury) is gone; however, some individuals develop chronic pain (i.e., maladaptive nociception). In the case of neuropathic pain, maladaptive signaling develops from damage to central or peripheral neurons.
The defining feature of neuropathic pain is the experience of pain in the absence of a stimulus (i.e., ectopic signaling) which is thought to result from nerve damage from injury (e.g., nerve injury), disease processes (e.g., diabetes; HIV), or external insults (e.g., chemotherapy treatment) that cause peripheral nerve sensitization (i.e., hyperexcitability of peripheral nerves) and/or central sensitization (i.e., hyperexcitability of nociceptive spinal neurons) [2,3,4,5]. As damaged nerves degenerate, areas of sensory loss form when the nerve is completely severed; however, any remaining fibers or fibers near the damaged site can send ectopic signals [2]. In the periphery, changes in ion channel sensitivity allow action potentials to be generated in response to low level inputs that would not trigger a pain signal under normal conditions [2,3,4,5]. Thus, frequent and spontaneous signals are sent from the periphery to the dorsal horn of the spinal cord. This increased peripheral input sensitizes spinal neurons, increasing ascending nociceptive input (i.e., central sensitization). In addition, central sensitization can be caused by maladaptive descending control as well as the loss of inhibitory interneurons in the DRG, which are controlled by systems such as serotonin, opioid, and endocannabinoid systems [6]. It is also thought that there is a strong neuroimmune response to nerve damage which contributes to peripheral and central sensitization [7]. Central and peripheral sensitization lead to hyperalgesia (i.e., exaggerated pain response to a painful stimulus) and/or allodynia (i.e., presence of pain response to an innocuous stimulus).
Current clinical practice guidelines focus primarily on pharmacological treatment [8,9,10,11,12]. Specifically, first-line treatments include anti-epileptics, tricyclic anti-depressants, topical treatments, and serotonin-norepinephrine reuptake inhibitors. Other pharmacological treatments include lidocaine or capsaicin patches, opioid agonists, and botulinum toxin A [2]. There are also guidelines on non-pharmacological interventions [10, 13, 14] which include neural blockade, surgical interventions, and spinal cord stimulation; however, these treatments are not effective for all types of peripheral neuropathies and may come with risks such as infection [2]. Other non-pharmacological treatments may include cranial and/or deep brain stimulation and intrathecal therapies that deliver drugs directly to affected neurons; however, the safety of these interventions has not been fully determined. Similarly, psychotherapy or complementary techniques such as acupuncture, Tai Chi Chuan, or exercise may be employed; however, the efficacy of such techniques is largely unknown.
Exercise may be a particularly important treatment option for patients with neuropathic pain, due to its wide array of established health benefits, such as reduced risk of chronic diseases including cardiovascular disease, type 2 diabetes, and cancer; reduced depression and anxiety; and improved sleep, cognition, bone health, and physical function [15]. However, before exercise can be recommended, researchers must establish its efficacy for patients who experience neuropathic pain. Therefore, the purpose of this review is to summarize the preclinical and clinical research examining the effects of exercise on neuropathic pain.
Methodological Approach
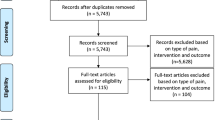
A narrative review format was chosen to present a general overview of the literature to date. Since this is a burgeoning area of research, this overview will be helpful for researchers and clinicians who are interested in advancing the literature base. To do this, the authors searched databases (Academic Search Premier, Google Scholar, PubMed, and Web of Science) from their inception to the present for relevant literature and the last search was conducted on 2 June 2020. Relevant literature included observational and experimental studies examining the influence of physical activity or exercise on neuropathic pain. Search terms included terms related to neuropathy (e.g., diabetic peripheral neuropathy, DPN; chemotherapy-induced peripheral neuropathy, CIPN; HIV), physical activity (e.g., exercise, resistance training, aerobic exercise), and pain (e.g., neuropathic pain, hyperalgesia, allodynia). Preclinical studies were included if the animals studied were models of neuropathy, if animals underwent nociceptive testing, and at least one group underwent exercise training. Additionally, meta-analyses of preclinical literature were included. Observational and experimental human studies were included if the condition being studied related to neuropathic pain. In addition, observational evidence needed to measure physical activity to be included. Experimental evidence was included if at least one treatment arm was an exercise training program. Further, it is important to note that a distinction between neuropathy and neuropathic pain was made for this review and only studies where the authors could comment specifically on the impact of the exercise training on pain were included. In total, 44 preclinical studies were identified through the search criteria; 4 studies were excluded because the exercise intervention was combined with other treatments (n = 3) or there were no nociceptive tests included (n = 1). A total of 26 clinical studies were found; 14 studies were excluded because the assessments were not specific to neuropathic pain (n = 5), the impact of pain could not be isolated from neuropathy symptoms (n = 4), the study examined the acute impact of exercise (n = 1), or the intervention was not considered an exercise stimulus (n = 4).
Preclinical Evidence
There is a plethora of preclinical evidence examining the influence of exercise on neuropathic nociception (i.e., responses to noxious stimuli), and this research is summarized in Table 1. Researchers use several animal models to understand the utility of exercise as a treatment for neuropathic pain by employing different behavioral tests to understand responses to noxious stimuli. Preclinical models include sciatic nerve injury (SNI), DPN, CIPN, complex regional pain syndrome (CRPS), and SCI. Common tests include applying mechanical (e.g., VonFrey filaments) and thermal (e.g., hot plates, acetone) stimuli and measuring the animals’ response. In general, aerobic exercise protocols reduce exaggerated responses (i.e., hypersensitivities) to these tests. In fact, recent meta-analyses concluded exercise training reduced nociceptive responses to mechanical and thermal tests compared to no exercise controls in animal models of peripheral nerve injury (i.e., SNI and DPN) [56] and SCI [57].
A brief look at the wider literature supports the conclusions of the aforementioned meta-analyses. Specifically, 1–6 weeks of treadmill running [17,18,19, 22,23,24, 27,28,29,30,31,32,33,34] and 6–39 days of swim training [16, 19,20,21] reduced mechanical and thermal indices of nociception in SNI models of neuropathic pain. Further, there is consistent evidence that 7–14 weeks of treadmill running reduced mechanical indices of nociception in SCI models of neuropathic pain [38, 39, 45]. While there is less literature in DPN, CIPN, and CRPS models, in general, 4–10 weeks of treadmill running [48, 49, 51, 52, 54], 4–10 weeks of swim training [47, 50, 53], and 23–28 days of wheel running [55] ameliorated abnormal nociception in these models. Other durations of exercise training are less conclusive [17, 24, 25, 40,41,42, 44], suggesting there may be an optimal exercise duration for effective neuropathic pain management. Further, one study demonstrated wheel running induced mechanical allodynia when it started 2 weeks after nerve injury [40], which requires further investigation. Also, it is important to note that animal models are not fully representative of the human pain experience [58]; thus, it is important to understand if human research demonstrates similar benefits of exercise. Accordingly, the purpose of the following section is to provide an overview of the clinical research to date.
Clinical Evidence
In the wider chronic pain (i.e., pain lasting more than 3 months or past normal tissue healing) literature, exercise is considered an important component of effective chronic pain management. In fact, treatment guidelines published by the Centers for Disease Control suggest including exercise as a part of the treatment plan for chronic pain that should be used before opioid-based pharmacological treatments [59]. Observational evidence suggests regular physical activity (i.e., 2–3 days per week of exercise) reduces the risk for chronic pain by 10–15% in those younger than 65 and by 20% in those 65 years or older [60]. Further, meta-analytic evidence suggests small to moderate reductions in pain in individuals with fibromyalgia [61, 62], moderate reductions in chronic low back pain [63], and small benefits for improving knee osteoarthritis [64, 65]. While there is consistent evidence that chronic exercise training is beneficial for reducing pain in chronic low back pain, fibromyalgia, and knee osteoarthritic samples, the clinical literature base for individuals with neuropathic pain is in its infancy.
Observational Evidence
Observational evidence suggests physical activity is associated with lower pain in colorectal cancer survivors treated with chemotherapy [66] and individuals with type 2 diabetes [67, 68] (see Table 2). Specifically, colorectal cancer survivors treated with chemotherapy and who were active (i.e., reported 150 min of moderate-intensity physical activity per week) were less likely than those who were inactive to report pain and other symptoms of CIPN such as trouble standing/walking, weakness, cramps, and loss of strength in their hands [66]. In addition, when only participants who reported CIPN scores in the top 30% (i.e., severe CIPN) were included, active participants reported experiencing less pain, lower fatigue scores, and higher function compared to individuals who were inactive. In individuals with diabetes, the evidence demonstrates that physical inactivity is a risk factor for painful diabetic neuropathy [67, 68]. For example, this was demonstrated in a cohort of individuals with diabetes following myocardial infarction in which participants reported their leisure time physical activity [67]. The results indicated that, in combination with smaller waist circumference and the absence of peripheral arterial disease, participants who reported at least 1 h per week of physical activity were less likely to have neuropathic pain. Chiang et al. (2016) examined different levels of exercise: no exercise, inactive (i.e., less than 30 min per day of exercise), or active (i.e., 30 min or more per day of exercise) [68]. Their results indicated that compared to active individuals, the no exercise and inactive groups were at a higher risk of having neuropathic pain. The body of observational research suggests that being physically active reduces the risk of experiencing neuropathic pain. Even so, experimental studies are needed to understand the direct impact of exercise on neuropathic pain and to begin to understand the dose (i.e., frequency, intensity, type, and time) needed to manage neuropathic pain.
Exercise Training and Neuropathic Pain in Adults
DPN
To date, the majority of exercise training studies have been conducted with participants diagnosed with diabetes or DPN [69,70,71,72,73,74]. Different exercise training programs have been examined including aerobic exercise training, combined aerobic and resistance exercise training, and high-intensity interval training (HIIT).
Single-Arm Studies
Two studies examined the influence of chronic exercise training using a single-arm study design [69, 71]. In one study, participants with DPN and metabolic syndrome reported significantly lower “worst pain over the past month,” reduced neuropathy symptoms (e.g., numbness, burning, tactile sensitivity, pain) and had significantly more intraepidermal nerve fiber branching following a 10-week progressive aerobic and resistance training program [69]. However, there were no changes in participant report of current pain, usual pain, or responses to quantitative sensory testing (i.e., vibration detection threshold, cold detection threshold, and hot pain threshold). The exercise prescription in this study was a supervised progressive program and started at 2 days per week of aerobic exercise (30 min at 50% VO2 reserve) and 1 day a week of resistance training (10 repetitions; reps) of 10 exercises targeting the abdominals, chest, back, and upper and lower extremities. Each week, the program progressed in training volume by increasing the time, intensity, or number of reps; by the end of the program, participants completed 50 min of aerobic exercise (70% VO2 reserve) on 2 days per week and 2 days per week of resistance training (20 reps of 10 resistance exercises). In another study, participants with painful DPN completed aerobic exercise (e.g., treadmill, stair steppers, or elliptical training) on 3 days per week and progressed from 30 min at 50% VO2 reserve to 50 min at 70% VO2 reserve [71]. Results indicated no changes in pain (i.e., average pain, worst pain, least pain, or current pain) from baseline to post-intervention; however, participants reported less pain interference following the training program, suggesting exercise reduced the amount pain interfered with their lives (e.g., mood, walking, relationships, sleep).
Multiple Group Studies
Two studies explored the impact of chronic exercise training on neuropathic pain using a two-arm study design [70, 72]. For example, female adults with DPN were randomly assigned to one of two 12-week interventions: (1) combined aerobic and resistance exercise training program and vitamin D supplementation or (2) vitamin D supplementation only [72]. The exercise program was progressive, and started at 20 min, and included low-intensity aerobic exercise (50% MHR) and resistance exercises (10–12 reps) at 50% of 10-repetition maximum (RM). By the end of the program, the exercise prescription consisted of 60 min of aerobic exercise at 70% MHR and the same resistance training protocol. Results indicated fewer participants in the exercise training program reported having pain (yes/no) compared to participants who completed vitamin D supplementation only. In another study, researchers conducted a randomized comparison trial to examine the influence of HIIT compared to moderate-intensity aerobic exercise [70]. Following 15 weeks of training, overweight women with DPN in the HIIT group reported significantly lower neuropathic pain scores than participants in the moderate-intensity group. There were no significant differences in neuropathic pain scores at baseline, thus this may indicate HIIT was more effective in reducing pain than moderate aerobic exercise. The HIIT program consisted of 20-min sessions on 3 days per week where participants completed a 5-min warm up followed by 8 s of vigorous-intensity sprinting (i.e., 85–95% of maximum heart rate, MHR) with 12 s of low-intensity cycling for up to 30 cycles. While HIIT training appears promising, patients with severe neuropathy and uncontrolled medical conditions were excluded from this study. Further, it took participants 2 weeks (6 sessions) to adapt to the full exercise protocol; thus, more work is needed to understand the generalizability of HIIT training.
One study used a three-arm randomized controlled trial design to examine the impact of 8 weeks of supervised combined aerobic and resistance moderate-intensity continuous training or combined HIIT on musculoskeletal and neuropathic pain compared to controls (i.e., usual care) in participants with type 2 diabetes [74]. Those in the combined aerobic and resistance continuous training intervention exercised on 4 days per week, with 2 days consisting of combined aerobic and resistance training and 2 days being aerobic exercise only. During the aerobic component, participants exercised at a moderate intensity (55–69% heart rate peak, HRpeak) for 22.5 min (combined aerobic and resistance days) or 52.5 min (aerobic only days). Resistance training was prescribed at a moderate level (i.e., fairly light to somewhat hard), lasted 30 min, and targeted the lower extremities, chest, back, shoulders, abdominals, and biceps. Participants in the combined HIIT group completed 3 sessions each week which included a 3-min aerobic exercise warm up (55–69% HRpeak), 4 min of high-intensity aerobic exercise (85–95% HRpeak), 1-min intervals of 8 high-intensity (i.e., very hard) resistance exercises with 1 min of rest between each exercise, and a 3-min aerobic exercise cool down (55–69% HRpeak). Results indicated significant reductions in musculoskeletal pain intensity from baseline to post-intervention in those who completed the combined HIIT program compared to individuals in the usual care control group. On the other hand, there were no significant changes in neuropathy symptoms or quantitative sensory testing outcomes (i.e., thermal detection thresholds, mechanical detection threshold, vibration detection threshold, and pressure pain threshold) for either exercise condition compared to controls, perhaps due to the low levels of neuropathy at baseline.
One study used a four-arm randomized controlled trial design to examine the influence of aerobic only, resistance only, or combined aerobic and resistance training programs on pain compared to controls in a sample of veterans with painful DPN [73]. In this study, participants were randomly assigned to one of four 12-week programs: aerobic exercise only, isokinetic resistance exercise only (i.e., a type of resistance training where the speed of movement is held constant throughout each rep), combined aerobic and resistance exercise, or health education. Exercise programs were held on 3 days per week while the health education program was held on 1 day per week. The aerobic exercise program progressed from 30 min (25 min at 60–70%VO2peak and 5 min at 71–80% VO2peak) to 45 min (17 min at 60–70% VO2peak, 20 min at 71–80% VO2peak, and 8 min at 81–90% VO2peak) and the resistance training program progressed from 3 to 6 sets of 10 reps of isokinetic leg extensions. Those in the combined aerobic and resistance training program completed both aerobic and strength training protocols. The results indicated no significant changes in pain or sensation determined via quantitative sensory testing (i.e., vibration detection threshold, cold detection threshold, and hot pain threshold) following the exercise interventions. However, physical health-related quality of life significantly improved following the aerobic exercise only training program.
Clinical Considerations and Limitations
It appears the influence of exercise training on neuropathic pain in participants with type 2 diabetes is equivocal. Two of the six studies were randomized controlled trials [73, 74], and the results from these studies demonstrated improvements in quality of life following 12 weeks of moderate aerobic exercise [73] or reductions in musculoskeletal pain following 8 weeks of combined HIIT [74], but no impact on neuropathic pain. Two other studies used a randomized comparison trial design and results indicated fewer participants who completed 12 weeks of combined exercise training and vitamin D supplementation reported pain compared to those who took vitamin D supplements only [72] or that participants who completed 15 weeks of HIIT had significantly lower neuropathic pain scores compared to those in the moderate aerobic training group [70]. There were two single-arm studies; one demonstrated reduced neuropathy symptoms and “worst pain over the past month” but no changes in other measures of pain following 10 weeks of combined aerobic and resistance exercise training [69]; and the other demonstrated no changes in neuropathic pain after 16 weeks of aerobic exercise training [71]. Taken together, the evidence to date indicates limited to modest effectiveness for exercise training to reduce pain associated with neuropathic conditions.
In turn, no studies reported significant increases in neuropathic pain from baseline to post-intervention, further suggesting the potential utility of exercise training in this population; however, caution is still needed when prescribing exercise for individuals with DPN. Separate from reductions in pain, one study demonstrated reductions in pain interference [71] while another demonstrated improvement in physical health-related quality of life following moderate-intensity aerobic training [73]. Thus, exercise may be beneficial for other health outcomes besides pain in this population. However, attention to adverse events and generalizability is needed. First, adverse events were likely underreported in these studies. In the studies which included information on adverse events [69, 73, 74], no serious event was reported. However, one study reported unanticipated serious events unrelated to the study [73] and two other studies reported mild adverse events such as hyper/hypoglycemia and pain in the back, hands, knees, or legs [69, 74]. In addition, exercise studies had strict criteria for inclusion and typically excluded individuals with comorbidities and those with severe neuropathy. Further, exercise compliance is an important consideration, as the presence of neuropathy may be an added barrier to participation. For example, a recent study demonstrated significantly higher diabetic neuropathy scores in patients who dropped out of an exercise training trial compared to those who completed the study [74].
Other Neuropathies: CIPN and HIV-Related Distal Symmetric Polyneuropathy
Three studies examined the influence of neuropathic pain resulting from conditions other than DPN (i.e., CIPN, HIV-related distal symmetric polyneuropathy) [75,76,77]. Two studies examined the influence of combined exercise training on pain in participants with CIPN [75, 76], and one study examined the influence of either aerobic exercise only or resistance exercise only in participants with HIV-related distal symmetric polyneuropathy [77].
CIPN
Two studies examined the impact of home-based combined exercise training on neuropathic pain in participants with CIPN [75, 76]. For example, in a randomized controlled trial, participants with CIPN undergoing treatment reported lower neuropathic pain scores following 10 weeks of home-based balance and strength exercises compared to individuals in the usual care group [76]. Researchers prescribed 30 min per day (7 days per week) of strength and balance exercises which consisted of exercises lying down for 7 min (ankle motion, hip abduction, and straight leg raises), sitting exercises for 13 min (digit movements, wrist motion, elbow flexion/extension, knee flexion extension, and toe tapping), and 10 min of standing balance exercises (one legged stance, toe stands, hip extensions, and tandem forward walking). In a single-arm trial, breast cancer survivors with CIPN underwent a 10-week moderate-intensity walking and resistance exercise program [75] to examine whether exercise training influenced CIPN symptoms (including pain characteristics) and quality of life (i.e., how troublesome their symptoms were). Participants were asked to complete home-based progressive exercise which consisted of walking at 55–65% MHR starting at 2 days per week for 10 min and ending with 30 min per day for 5 days per week. In addition, the exercise program consisted of resistance exercise on 3 days per week using resistance bands. By the end of the study, participants reported their symptoms were less troublesome and fewer individuals reported experiencing pain symptoms such as unpleasant sensations of the skin, abnormal sensitivity to touch, and sudden bursts of pain.
HIV-Related Distal Symmetric Polyneuropathy
One study examined the impact of exercise on HIV patients with distal symmetric polyneuropathy [77]. In this randomized controlled trial, participants engaged in 12 weeks of supervised moderate progressive aerobic exercise, or moderate progressive resistance exercise, or an HIV education control on 3 days per week for 30 min per day. The aerobic exercise program included stationary biking in three phases: warm-up (5 min with no resistance), aerobic (20 min with low-moderate resistance), and cool-down (5 min with no resistance). The aerobic phase progressed from 40% MHR for the first 6 weeks to 65% MHR for the last 6 weeks. The resistance exercise program consisted of three phases: warm-up (5 min stretching), resistance exercise (20 min exercises), and cool-down (5 min stretching). The resistance exercise protocol consisted of 2 sets of 10 reps of resistance exercises targeting the lower extremities (i.e., quadriceps, hamstrings, tibialis anterior, and gastrocnemius) at 40% 1-RM for the first 6 weeks and progressed to 2 sets of 10 reps of the same exercises at 65% 1-RM max for the remaining 6 weeks. Participants in both exercise groups reported reduced “pain over the last 24 h” following the intervention, whereas the control group reported no significant change in pain.
Clinical Considerations and Limitations
Preliminary evidence examining the utility of exercise training in reducing neuropathic pain in CIPN or HIV-related distal symmetric polyneuropathy is generally supportive, although there are important considerations. Two randomized controlled trials demonstrated exercise training reduced neuropathic pain following 10 weeks of combined balance and strength training [76] or following 12 weeks of either moderate aerobic exercise training or 12 weeks of moderate resistance exercise training [77]. As more evidence accumulates, future researchers should consider potential recruitment barriers. For example, patients were recruited through clinics or medical registries and out of those identified, only 28–67% were enrolled, in part due to stringent inclusion/exclusion criteria [76, 77] and/or an unwillingness to participate [75, 77]. Similarly, exercise compliance is an important consideration as there was low retention (42%) in one study yet high retention (88–96%) in two other studies. The studies with high retention were conducted in a clinical setting (day care unit of a tertiary care hospital [76]; rehabilitation clinics [77]), whereas the study with low retention was conducted outside of the clinical setting [75]. Thus, study setting may be an important factor for exercise compliance. Further work is needed to understand factors that contribute to enrollment, adherence, and retention of participants to exercise programs.
Summary
While the clinical literature base suggests exercise may be beneficial in populations with neuropathic pain, not all studies support this claim and there are several limitations that need to be understood when discussing the effect of exercise on neuropathic pain. There is evidence that exercise training reduced worst pain over the last month [69], pain over the past 24 h [77], pain or neuropathy scores [69, 70, 75, 76], the presence of pain [72], musculoskeletal pain [74], and pain interference [71] and improved quality of life [73]. At the same time, there is evidence that exercise training had no impact on neuropathic pain [73, 74] or that it only influenced one aspect of pain while others remained unchanged [69]. Further, randomized controlled trials were rare and it is therefore unclear if effects of the exercise intervention are due to exercise or other factors such as the attention given to participants or the natural course of time; thus, conclusions described in this summary are preliminary. Further, several studies included small sample sizes which may reflect the difficulty in recruiting patients with neuropathy to participate in exercise training. Similarly, stringent inclusion/exclusion criteria make it difficult to generalize to the population with neuropathic pain at large. Further, more work is needed to understand compliance to exercise programs in neuropathic pain populations. One factor may be transient increases in pain or other potential adverse events that may occur during exercise training [69, 74]. These events are likely underreported in the current literature and the literature base would benefit from reporting adverse events that can accompany exercise training, including, as suggested by Cox and associated (2020), rheumatological and musculoskeletal symptoms [78]. In general, there is a need for more systematic and rigorous investigations that include consistent pain measures to better compare across studies, larger sample sizes, control groups to account for common confounding variables, and comparison studies to help provide specific exercise prescriptions. Further, little is known about the mechanisms behind exercises’ effects on neuropathic pain in the clinical literature. An understanding of these mechanisms may shed light on the potential for exercise as a treatment option for neuropathic pain.
Mechanisms
The majority of mechanistic insight comes from preclinical data where specific mechanisms were measured in conjunction with nociceptive behavioral responses using different exercise programs. Preclinical evidence suggests that exercise may reduce neuropathic pain through normalizing microglia activation, balancing pro- and anti-inflammatory responses, upregulating heat shock protein 72, and producing alterations in neurotransmitter and neuromodulatory systems (see below).
Microglia
Activation of microglia in response to neuronal damage may stimulate a cascade of events leading to increased nociceptive neuronal excitability and ultimately the experience of neuropathic pain [34, 79]. Recent preclinical evidence demonstrated normalization of microglial activity [17, 21, 28, 44], as well a shift towards a healthy balance of inflammatory markers [32, 43] in the DRG in response to exercise training. Thus, exercise may promote pain reductions through normalizing microglial activity in the DRG. However, these changes often occur in conjunction with alterations in inflammatory markers.
Inflammation
Pro-inflammatory markers such as tumor necrosis factor-α, interleukin-1β, and interleukin-6 have been studied in the context of both neuropathic pain development and exercise. It is thought that markers such as these are released in response to microglial activation after nerve damage [79]. Interestingly, pro-inflammatory markers are elevated in response to acute exercise, however chronic exercise training stimulates an anti-inflammatory response [80]. Therefore, it is possible exercise influences pain through inflammatory marker change [81]. In fact, most preclinical evidence demonstrates an increase in pro-inflammatory markers following nerve injury and an attenuation of this increase after exercise [18, 26, 30,31,32, 43, 45, 52, 82]. Some studies demonstrate an increase [26, 31, 43] or a normalization [31] of interleukin-10, an anti-inflammatory cytokine, levels in response to exercise. Recent work implicated the role of interleukin-4 in this mechanism, as interleukin-4 antagonism or knockout mice reversed the analgesic effect of exercise training [32]. Therefore, exercise may lead to decreases in neuropathic pain by preventing pro-inflammatory cytokine upregulation and promoting anti-inflammatory cytokine release.
Heat Shock Protein 72
Heat shock protein 72 is a protein expressed in many organs, typically in response to stressful environments, with the primary function of aiding other proteins in healthy development [83]. Recent work demonstrated higher levels of heat shock protein 72 and lower levels of hyperalgesia (thermal, mechanical) and allodynia (mechanical) in exercised mice compared with non-exercised mice [19, 49]. Thus, demonstrating the potential role of Hsp72 as a mechanism for reduced hyperalgesia and allodynia following exercise training.
Neurotrophins
Exercise may facilitate healthy nerve growth in damaged pain sensory pathways through influencing neurotrophic proteins (e.g., brain derived neurotrophic factor). Upregulation of brain derived neurotrophic factor, stemming from microglial activation in the DRG, is thought to impair nociceptive processing, producing hyperalgesia and allodynia [72]. In SNI mice, exercise appeared to ameliorate these increases [21, 24, 32, 34, 35, 46, 84] leading to decreased hyperalgesia. Other neurotrophins have been shown to normalize in response to exercise as well [37, 84]. Some studies concluded exercise may prevent pathological nociceptive neuronal growth [54, 81] and promotion of healthy nerve regeneration in the nociceptive pathway [17, 46, 69].
Neurotransmitters (Dopamine, Epinephrine, Gamma-aminobutyric Acid, Serotonin)
There is evidence to support the involvement of neurotransmitters in attenuating neuropathic nociception following exercise training [22, 27, 29, 33]. Exercise-induced reductions in allodynia and hyperalgesia were prevented by inhibition of the dopaminergic pathway [29]. This suggests decreases in pain after chronic exercise in neuropathic pain may involve the dopaminergic system. At the same time, the serotonergic system was implicated after researchers documented increased levels of serotonin, upregulation of serotonergic receptors, and reduced serotonin transporters in the brainstem [22, 33]. In addition, exercise increased levels of adrenergic receptors (alpha and beta) found after nerve injury [33]. Further, recent research suggested gamma-aminobutyric acid (GABA) may play a mechanistic role, due to normalization of GABA in the nociceptive pathway in response to exercise [27]. Perhaps exercise training improves neurotransmitter tone in the dorsal horn.
Endogenous Opioids
Exercise effects in animal models of neuropathic pain may be mediated by changes in endogenous opioids. For example, exercise training reduced thermal and tactile hypersensitivity and increased opioid content in the rostral ventromedial medulla and the midbrain periaqueductal gray area in spinal nerve-ligated animals. However, exercise effects were reversed by administration of opioid receptor antagonists [36]. In animals with SNI, the effects of exercise-induced reductions in mechanical hypersensitivity were reversed by administration of naloxone (an opioid receptor antagonist) [34]. Also, exercise-induced analgesia in diabetic rats was reversed in a dose-dependent manner with the administration of naloxone [48]. Further, swimming exercise reduced mechanical allodynia in an animal model of CRPS-1 but the anti-allodynic effect of exercise was reversed by pretreatment of naloxone [53].
Endocannabinoids
Pharmacological manipulation of the endocannabinoid system reduces nociceptive behaviors such as mechanical allodynia, cold allodynia, mechanical hyperalgesia, or heat hyperalgesia in preclinical models of SNI (e.g., [85,86,87,88]), SCI (e.g., [89,90,91]), CIPN (e.g., [92,93,94,95,96,97,98]), and DPN (e.g., [99,100,101,102]). While no research to date has examined the endocannabinoid system as a mechanism for exercise-induced reductions in neuropathic pain, the endocannabinoid system has been implicated in exercise-induced hypoalgesia (i.e., acute pain reductions following exercise) in healthy humans performing isometric exercise [103]; thus, future research is warranted.
Conclusions
The previous sections summarized evidence examining the efficacy of exercise training to reduce neuropathic pain. Preclinical evidence demonstrated treadmill running protocols consisting of 30–60 min of exercise performed 3–5 days/week for 1–15 weeks were effective in reducing neuropathic nociception. Swimming protocols were also effective and consisted of 30–60 min/day of swimming performed 5–7 days/week for 4–10 weeks. Clinical evidence demonstrated 10–12 weeks of moderate-intensity combination training (i.e., aerobic and resistance exercise) or 15 weeks of HIIT reduced sensory (i.e., pain intensity, pain characteristics) or affective (i.e., how troublesome the pain is) components of neuropathic pain. One program consisting of 16 weeks of moderate-intensity aerobic exercise led to reductions in pain interference but not pain intensity [71]. Taken together, the preclinical and clinical evidence suggests further study is warranted. Randomized controlled trials are needed to further translate the preclinical evidence base to the clinical realm. Specifically, systematic investigations into the mode, intensity, frequency, and duration of exercise that reduce neuropathic pain are needed. In addition, consistent patient-reported and clinical outcomes as well as potential mechanisms should be included in future studies. As a result, the literature can move towards a consensus and practitioners may begin to provide specific exercise recommendations for patients experiencing neuropathic pain.
Availability of Data and Materials
Not applicable
Abbreviations
- CIPN:
-
Chemotherapy-induced peripheral neuropathy
- CRPS:
-
Complex regional pain syndrome
- DPN:
-
Diabetic peripheral neuropathy
- DRG:
-
Dorsal root ganglion
- GABA:
-
Gamma-aminobutyric acid
- HIIT:
-
High-intensity interval training
- HIV:
-
Human immunodeficiency virus
- HRpeak :
-
Peak heart rate
- MHR:
-
Maximum heart rate
- SCI:
-
Spinal cord injury
- SNI:
-
Sciatic nerve injury
- VO2 :
-
Oxygen uptake
References
Schaefer C, Sadosky A, Mann R, Daniel S, Parsons B, Tuchman M, et al. Pain severity and the economic burden of neuropathic pain in the United States: BEAT Neuropathic Pain Observational Study. Clinicoecon Outcomes Res. 2014;6:483–96. https://doi.org/10.2147/CEOR.S63323.
Colloca L, Ludman T, Bouhassira D, Baron R, Dickenson A, Yarnitsky D, et al. Neuropathic pain. Nat Rev Dis Primers. 2017;3:19. https://doi.org/10.1038/nrdp.2017.2.
Costigan M, Scholz J, Woolf CJ. Neuropathic Pain: A maladaptive response of the nervous system to damage. Ann Rev Neurosci. 2009;32:1–32.
Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet. 1999;353(9168):1959–64. https://doi.org/10.1016/s0140-6736(99)01307-0.
Woolf CJ. Central sensitization: Implications for the diagnosis and treatment of pain. Pain. 2011;152(3):S2–S15. https://doi.org/10.1016/j.pain.2010.09.030.
Millan MJ. Descending control of pain. Prog Neurobiol. 2002;66(6):355–474. https://doi.org/10.1016/s0301-0082(02)00009-6.
Scholz J, Woolf CJ. The neuropathic pain triad: Neurons, immune cells and glia. Nat Neurosci. 2007;10(11):1361–8. https://doi.org/10.1038/nn1992.
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162–73. https://doi.org/10.1016/s1474-4422(14)70251-0.
Attal N, Cruccu G, Baron R, Haanpää M, Hansson P, Jensen TS, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17:1113–23.
Deng YK, Luo L, Hu YH, Fang KY, Liu J. Clinical practice guidelines for the management of neuropathic pain: a systematic review. BMC Anesthesiol. 2016;16:10. https://doi.org/10.1186/s12871-015-0150-5.
Moulin DE, Boulanger A, Clark AJ, Clarke H, Dao T, Finley GA, et al. Pharmacological management of chronic neuropathic pain: Revised consensus statement from the Canadian Pain Society. Pain Res Manag. 2014;19(6):328–35.
(UK) CfCPaN. Neuropathic Pain: The Pharmacological Management of Neuropathic Pain in Adults in Non-specialist Settings. 2013.
Cruccu G, Aziz TZ, Garcia-Larrea L, Hansson P, Jensen TS, Lefaucheur JP, et al. EFNS guidelines on neurostimulation therapy for neuropathic pain. Eur J Neurol. 2007;14(9):952–70. https://doi.org/10.1111/j.1468-1331.2007.01916.x.
Mailis A, Taenzer P. Evidence-based guideline for neuropathic pain interventional treatments: Spinal cord stimulation, intravenous infusions, epidural injections and nerve blocks. Pain Res Manag. 2012;17(3):150–8. https://doi.org/10.1155/2012/794325.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320(19):2020–8. https://doi.org/10.1001/jama.2018.14854.
Kuphal KE, Fibuch EE, Taylor BK. Extended swimming exercise reduces inflammatory and peripheral neuropathic pain in rodents. J Pain. 2007;8(12):989–97.
Cobianchi S, Marinelli S, Florenzano F, Pavone F, Luvisetto S. Short- but not long-lasting treadmill running reduces allodynia and improves functional recovery after peripheral nerve injury. Neuroscience. 2010;168(1):273–87. https://doi.org/10.1016/j.neuroscience.2010.03.035.
Bobinski F, Martins DF, Bratti T, Mazzardo-Martins L, Winkelmann-Duarte EC, Guglielmo LG, et al. Neuroprotective and neuroregenerative effects of low-intensity aerobic exercise on sciatic nerve crush injury in mice. Neuroscience. 2011;194:337–48. https://doi.org/10.1016/j.neuroscience.2011.07.075.
Chen Y, Li Y, Chen Y, Li Z, Hung C. Exercise training attenuates neuropathic pain and cytokine expression after chronic constriction injury of rat sciatic nerve. Anesth Analg. 2012;114(6):1330–7.
Shen J, Fox LE, Cheng J. Swim therapy reduces mechanical allodynia and thermal hyperalgesia induced by chronic constriction nerve injury in rats. Pain Med. 2013;14(4):516–25.
Almeida C, DeMaman A, Kusuda R, Cadetti F, Ravanelli MI, Queiroz AL, et al. Exercise therapy normalizes BDNF upregulation and glial hyperactivity in a mouse model of neuropathic pain. Pain. 2015;156(3):504–13.
Bobinski F, Ferreira TAA, Cordova MM, Dombrowski PA, da Cunha C, Santo C, et al. Role of brainstem serotonin in analgesia produced by low-intensity exercise on neuropathic pain after sciatic nerve injury in mice. Pain. 2015;156(12):2595–606. https://doi.org/10.1097/j.pain.0000000000000372.
Kim Y-J, Byun J-H, Choi I-S. Effect of exercise on μ-Opioid receptor expression in the rostral ventromedial medulla in neuropathic pain rat model. Ann Rehabil Med. 2015;39(3):331–9.
López-Álvarez VM, Modol L, Navarro X, Cobianchi S. Early increasing-intensity treadmill exercise reduces neuropathic pain by preventing nociceptor collateral sprouting and disruption of chloride cotransporters homeostasis after peripheral nerve injury. Pain. 2015;156(9):1812–25.
Sheahan TD, Copits BA, Golden JP, Gereau RW IV. Voluntary exercise training: analysis of mice in uninjured, inflammatory, and nerve-injured pain states. PloS one. 2015;10(7):e0133191.
Grace PM, Fabisiak TJ, Green-Fulgham SM, Anderson ND, Strand KA, Kwilasz AJ, et al. Prior voluntary wheel running attenuates neuropathic pain. Pain. 2016;157(9):2012–23.
Kami K, Taguchi Ms S, Tajima F, Senba E. Improvements in impaired GABA and GAD65/67 production in the spinal dorsal horn contribute to exercise-induced hypoalgesia in a mouse model of neuropathic pain. Mol Pain. 2016;12. https://doi.org/10.1177/1744806916629059.
Kami K, Taguchi S, Tajima F, Senba E. Histone acetylation in microglia contributes to exercise-induced hypoalgesia in neuropathic pain model mice. J Pain. 2016;17(5):588–99.
Wakaizumi K, Kondo T, Hamada Y, Narita M, Kawabe R, Narita H, et al. Involvement of mesolimbic dopaminergic network in neuropathic pain relief by treadmill exercise: A study for specific neural control with Gi-DREADD in mice. Mol Pain. 2016;12:1–11. https://doi.org/10.1177/1744806916681567.
Safakhah HA, Kor NM, Bazargani A, Bandegi AR, Pourbadie HG, Khoshkholgh-Sima B, et al. Forced exercise attenuates neuropathic pain in chronic constriction injury of male rat: An investigation of oxidative stress and inflammation. J Pain Res. 2017;10:1457–66. https://doi.org/10.2147/jpr.s135081.
Tsai K-L, Huang P-C, Wang L-K, Hung C-H, Chen Y-W. Incline treadmill exercise suppresses pain hypersensitivity associated with the modulation of pro-inflammatory cytokines and anti-inflammatory cytokine in rats with peripheral nerve injury. Neurosci Lett. 2017;643:27–31.
Bobinski F, Teixeira JM, Sluka KA, Santos ARS. Interleukin-4 mediates the analgesia produced by low-intensity exercise in mice with neuropathic pain. Pain. 2018;159(3):437–50. https://doi.org/10.1097/j.pain.0000000000001109.
López-Álvarez VM, Puigdomenech M, Navarro X, Cobianchi S. Monoaminergic descending pathways contribute to modulation of neuropathic pain by increasing-intensity treadmill exercise after peripheral nerve injury. Exp Neurol. 2018;299:42–55. https://doi.org/10.1016/j.expneurol.2017.10.007.
Sumizono M, Sakakima H, Otsuka S, Terashi T, Nakanishi K, Ueda K, et al. The effect of exercise frequency on neuropathic pain and pain-related cellular reactions in the spinal cord and midbrain in a rat sciatic nerve injury model. J Pain Res. 2018;11:281–91. https://doi.org/10.2147/JPR.S156326.
Hutchinson KJ, Gomez-Pinilla F, Crowe MJ, Ying Z, Basso DM. Three exercise paradigms differentially improve sensory recovery after spinal cord contusion in rats. Brain. 2004;127:1403–14. https://doi.org/10.1093/brain/awh160.
Stagg NJ, Mata HP, Ibrahim MM, Henriksen EJ, Porreca F, Vanderah TW, et al. Regular exercise reverses sensory hypersensitivity in a rat neuropathic pain modelrole of endogenous opioids. Anesthesiology. 2011;114(4):940–8.
Detloff MR, Smith EJ, Molina DQ, Ganzer PD, Houlé JD. Acute exercise prevents the development of neuropathic pain and the sprouting of non-peptidergic (GDNF-and artemin-responsive) c-fibers after spinal cord injury. Exp Neurol. 2014;255:38–48.
Ward PJ, Herrity AN, Smith RR, Willhite A, Harrison BJ, Petruska JC, et al. Novel multi-system functional gains via task specific training in spinal cord injured male rats. J Neurotrauma. 2014;31(9):819–33. https://doi.org/10.1089/neu.2013.3082.
Dugan EA, Sagen J. An intensive locomotor training paradigm improves neuropathic pain following spinal cord compression injury in rats. J Neurotrauma. 2015;32(9):622–32.
Detloff MR, Quiros-Molina D, Javia A, Daggubati L, Nehlsen AD, Naqvi A, et al. Delayed exercise is ineffective at reversing aberrant nociceptive afferent plasticity or neuropathic pain after spinal cord injury in rats. Neurorehabil Neural Repair. 2016;30(7):685–700. https://doi.org/10.1177/1545968315619698.
Nees TA, Tappe-Theodor A, Sliwinski C, Motsch M, Rupp R, Kuner R, et al. Early-onset treadmill training reduces mechanical allodynia and modulates calcitonin gene-related peptide fiber density in lamina III/IV in a mouse model of spinal cord contusion injury. Pain. 2016;157(3):687–97. https://doi.org/10.1097/j.pain.0000000000000422.
Ward PJ, Herrity AN, Harkema SJ, Hubscher CH. Training-induced functional gains following SCI. Neural Plast. 2016;12. https://doi.org/10.1155/2016/4307694.
Gong X, Chen Y, Fu B, Jiang J, Zhang M. Infant nerve injury induces delayed microglial polarization to the M1 phenotype, and exercise reduces delayed neuropathic pain by modulating microglial activity. Neuroscience. 2017;349:76–86.
Chhaya SJ, Quiros-Molina D, Tamashiro-Orrego AD, Houlé JD, Detloff MR. Exercise-induced changes to the macrophage response in the dorsal root ganglia prevent neuropathic pain after spinal cord injury. J Neurotrauma. 2019;36(6):877–90. https://doi.org/10.1089/neu.2018.5819.
Dugan EA, Jergova S, Sagen J. Mutually beneficial effects of intensive exercise and GABAergic neural progenitor cell transplants in reducing neuropathic pain and spinal pathology in rats with spinal cord injury. Exp Neurol. 2020;327:17. https://doi.org/10.1016/j.expneurol.2020.113208.
Groover AL, Ryals JM, Guilford BL, Wilson NM, Christianson JA, Wright DE. Exercise-mediated improvements in painful neuropathy associated with prediabetes in mice. PAIN. 2013;154(12):2658–67.
Rossi DM, Valenti VE, Navega MT. Exercise training attenuates acute hyperalgesia in streptozotocin-induced diabetic female rats. Clinics. 2011;66(9):1615–9. https://doi.org/10.1590/s1807-59322011000900019.
Shankarappa SA, Piedras-Renteria ES, Stubbs EB Jr. Forced-exercise delays neuropathic pain in experimental diabetes: effects on voltage-activated calcium channels. J Neurochem. 2011;118(2):224–36. https://doi.org/10.1111/j.1471-4159.2011.07302.x.
Chen Y-W, Hsieh P-L, Chen Y-C, Hung C-H, Cheng J-T. Physical exercise induces excess hsp72 expression and delays the development of hyperalgesia and allodynia in painful diabetic neuropathy rats. Anesth Analg. 2013;116(2):482–90.
Aghdam AM, Shahabi P, Karimi-Sales E, Ghiasi R, Sadigh-Eteghad S, Mahmoudi J, et al. Swimming exercise induced reversed expression of miR-96 and its target gene NaV1.3 in diabetic peripheral neuropathy in rats. Chin J Physiol. 2018;61(2):124–9. https://doi.org/10.4077/CJP.2018.BAG531.
Golbar SJ, Gharekhanlu R, Kordi MR, Khazani A. Effects of Endurance Exercise Training on Kinesin - 5 and dynein motor proteins in sciatic nerves of male wistar rats with diabetic neuropathy. Int J Sport Stud Health. 2018:e67758. https://doi.org/10.5812/intjssh.67758.
Ma X, Liu S, Liu D, Wang Q, Li H, Zhao Z. Exercise intervention attenuates neuropathic pain in diabetes via mechanisms of mammalian target of rapamycin (mTOR). Arch Physiol Biochem. 2018:1–8. https://doi.org/10.1080/13813455.2018.1489851.
Martins D, Mazzardo-Martins L, Soldi F, Stramosk J, Piovezan A, Santos A. High-intensity swimming exercise reduces neuropathic pain in an animal model of complex regional pain syndrome type I: Evidence for a role of the adenosinergic system. Neuroscience. 2013;234:69–76.
Park JS, Kim S, Hoke A. An exercise regimen prevents development paclitaxel induced peripheral neuropathy in a mouse model. J Peripher Nerv Syst. 2015;20(1):7–14. https://doi.org/10.1111/jns.12109.
Slivicki RA, Mali SS, Hohmann AG. Voluntary exercise reduces both chemotherapy-induced neuropathic nociception and deficits in hippocampal cellular proliferation in a mouse model of paclitaxel-induced peripheral neuropathy. Neurobiol Pain. 2019;6:100035. https://doi.org/10.1016/j.ynpai.2019.100035.
Guo JB, Chen BL, Wang Y, Zhu Y, Song G, Yang Z, et al. Meta-Analysis of the Effect of Exercise on Neuropathic Pain Induced by Peripheral Nerve Injury in Rat Models. Front Neurol. 2019;10:12. https://doi.org/10.3389/fneur.2019.00636.
Palandi J, Bobinski F, de Oliveira GM, Ilha J. Neuropathic pain after spinal cord injury and physical exercise in animal models: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2020;108:781–95. https://doi.org/10.1016/j.neubiorev.2019.12.016.
Yezierski RP, Hansson P. Inflammatory and neuropathic pain from bench to bedside: What went wrong? J Pain. 2018;19(6):571–88. https://doi.org/10.1016/j.jpain.2017.12.261.
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. https://doi.org/10.15585/mmwr.rr6501e1.
Landmark T, Romundstad P, Borchgrevink PC, Kaasa S, Dale O. Associations between recreational exercise and chronic pain in the general population: Evidence from the HUNT 3 study. Pain. 2011;152(10):2241–7. https://doi.org/10.1016/j.pain.2011.04.029.
Hauser W, Klose P, Langhorst J, Moradi B, Steinbach M, Schiltenwolf M, et al. Efficacy of different types of aerobic exercise in fibromyalgia syndrome: A systematic review and meta-analysis of randomised controlled trials. Arthritis Res Ther. 2010;12(3):14. https://doi.org/10.1186/ar3002.
Sosa-Reina MD, Nunez-Nagy S, Gallego-Izquierdo T, Pecos-Martin D, Monserrat J, Alvarez-Mon M. Effectiveness of therapeutic exercise in fibromyalgia syndrome: a systematic review and meta-analysis of randomized clinical trials. Biomed Res Int. 2017;14. https://doi.org/10.1155/2017/2356346.
Searle A, Spink M, Ho A, Chuter V. Exercise interventions for the treatment of chronic low back pain: A systematic review and meta-analysis of randomised controlled trials. Clin Rehabil. 2015;29(12):1155–67. https://doi.org/10.1177/0269215515570379.
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: A Cochrane systematic review. Br J Sports Med. 2015;49(24):6. https://doi.org/10.1136/bjsports-2015-095424.
Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis. Arthritis Rheumatol. 2014;66(3):622–36. https://doi.org/10.1002/art.38290.
Mols F, Beijers AJM, Vreugdenhil G, Verhulst A, Schep G, Husson O. Chemotherapy-induced peripheral neuropathy, physical activity and health-related quality of life among colorectal cancer survivors from the PROFILES registry. J Cancer Surviv Res Pract. 2015;9(3):512–22. https://doi.org/10.1007/s11764-015-0427-1.
Ziegler D, Rathmann W, Meisinger C, Dickhaus T, Mielck A, Grp KS. Prevalence and risk factors of neuropathic pain in survivors of myocardial infarction with pre-diabetes and diabetes. The KORA Myocardial Infarction Registry. Eur J Pain. 2009;13(6):582–7. https://doi.org/10.1016/j.ejpain.2008.07.007.
Chiang SS, Lee CL, Liu HC, Wang JS, Lee IT, Song YM, et al. Physical activity and albuminuria were associated with painful diabetic polyneuropathy in type 2 diabetes in an ethnic Chinese population. Clin Chim Acta. 2016;462:55–9. https://doi.org/10.1016/j.cca.2016.08.022.
Kluding PM, Pasnoor M, Singh R, Jernigan S, Farmer K, Rucker J, et al. The effect of exercise on neuropathic symptoms, nerve function, and cutaneous innervation in people with diabetic peripheral neuropathy. J Diabetes Complications. 2012;26(5):424–9. https://doi.org/10.1016/j.jdiacomp.2012.05.007.
Hamed N, Raoof N. Effect of high intensity interval training on diabetic obese women with polyneuropathy: A randomized controlled clinical trial. Phys Ther Rehabil. 2014;1(4):1–8.
Yoo M, D'silva LJ, Martin K, Sharma NK, Pasnoor M, LeMaster JW, et al. Pilot study of exercise therapy on painful diabetic peripheral neuropathy. Pain Med. 2015;16(8):1482–9.
Nadi M, Marandi SM, Esfarjani F, Saleki M, Mohammadi M. The comparison between effects of 12 weeks combined training and vitamin D supplement on improvement of sensory-motor neuropathy in type 2 diabetic women. Adv Biomed Res. 2017;6:55. https://doi.org/10.4103/2277-9175.205528.
Stubbs EB, Fisher MA, Miller CM, Jelinek C, Butler J, McBurney C, et al. Randomized controlled trial of physical exercise in diabetic veterans with length-dependent distal symmetric polyneuropathy. Front Neurosci. 2019;13:19. https://doi.org/10.3389/fnins.2019.00051.
Cox ER, Gajanand T, Burton NW, Coombes JS, Coombes BK. Effect of different exercise training intensities on musculoskeletal and neuropathic pain in inactive individuals with type 2 diabetes- Preliminary randomised controlled trial. Diabetes Res Clin Pract. 2020;164:9.
Wonders KY, Whisler G, Loy H, Holt B, Bohachek K, Wise R. Ten weeks of home-based exercise attenuates symptoms of chemotherapy-induced peripheral neuropathy in breast cancer patients. Health Psychol Res. 2013;1(3):e28. https://doi.org/10.4081/hpr.2013.e28.
Dhawan S, Andrews R, Kumar L, Wadhwa S, Shukla G. A randomized controlled trial to assess the effectiveness of muscle strengthening and balancing exercises on chemotherapy-induced peripheral neuropathic pain and quality of life among cancer patients. Cancer Nurs. 2020. https://doi.org/10.1097/NCC.0000000000000693.
Maharaj SS, Yakasai AM. Does a rehabilitation program of aerobic and progressive resisted exercises influence HIV-induced distal neuropathic pain? Am J Phys Med Rehabil. 2018;97(5):364–9. https://doi.org/10.1097/phm.0000000000000866.
Cox ER, Coombes JS, Keating SE, Burton NW, Coombes BK. Not a painless condition: rheumatological and musculoskeletal symptoms in type 2 diabetes, and the implications for exercise participation. Curr Diabetes Rev. 2020;16(3):211–9. https://doi.org/10.2174/1573399815666190531083504.
Dobson JL, McMillan J, Li L. Benefits of exercise intervention in reducing neuropathic pain. Front Cell Neurosci. 2014;8:102. https://doi.org/10.3389/fncel.2014.00102.
Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11(9):607–15. https://doi.org/10.1038/nri3041.
Cooper MA, Kluding PM, Wright DE. Emerging relationships between exercise, sensory nerves, and neuropathic pain. Front Neurosci. 2016;10.
Hung C-H, Huang P-C, Tzeng J-I, Wang J-J, Chen Y-W. Therapeutic ultrasound and treadmill training suppress peripheral nerve injury–induced pain in rats. Phys Ther. 2016;96(10):1545–53.
De Maio A. Heat shock proteins: Facts, thoughts, and dreams. Shock 1999;11(1):1-12. doi:https://doi.org/10.1097/00024382-199901000-00001.
Cobianchi S, Casals-Diaz L, Jaramillo J, Navarro X. Differential effects of activity dependent treatments on axonal regeneration and neuropathic pain after peripheral nerve injury. Exp Neurol. 2013;240:157–67.
Desroches J, Guindon J, Lambert C, Beaulieu P. Modulation of the anti-nociceptive effects of 2-arachidonoyl glycerol by peripherally administered FAAH and MGL inhibitors in a neuropathic pain model. Br J Pharmacol. 2008;155(6):913–24. https://doi.org/10.1038/bjp.2008.322.
Fox A, Kesingland A, Gentry C, McNair K, Patel S, Urban L, et al. The role of central and peripheral Cannabinoid(1) receptors in the antihyperalgesic activity of cannabinoids in a model of neuropathic pain. Pain. 2001;92(1-2):91–100. https://doi.org/10.1016/s0304-3959(00)00474-7.
Kinsey SG, Mahadevan A, Zhao BJ, Sun H, Naidu PS, Razdan RK, et al. The CB2 cannabinoid receptor-selective agonist O-3223 reduces pain and inflammation without apparent cannabinoid behavioral effects. Neuropharmacology. 2011;60(2-3):244–51. https://doi.org/10.1016/j.neuropharm.2010.09.004.
Schlosburg JE, Blankman JL, Long JZ, Nomura DK, Pan B, Kinsey SG, et al. Chronic monoacylglycerol lipase blockade causes functional antagonism of the endocannabinoid system. Nat Neurosci. 2010;13(9):1113–U111. https://doi.org/10.1038/nn.2616.
LaBuda CJ, Little PJ. Pharmacological evaluation of the selective spinal nerve ligation model of neuropathic pain in the rat. J Neurosci Methods. 2005;144(2):175–81. https://doi.org/10.1016/j.neumeth.2004.11.008.
de Novellis V, Vita D, Gatta L, Luongo L, Bellini G, De Chiaro M, et al. The blockade of the transient receptor potential vanilloid type 1 and fatty acid amide hydrolase decreases symptoms and central sequelae in the medial prefrontal cortex of neuropathic rats. Mol Pain. 2011;7:19. https://doi.org/10.1186/1744-8069-7-7.
Bridges D, Ahmad K, Rice ASC. The synthetic cannabinoid WIN55,212-2 attenuates hyperalgesia and allodynia in a rat model of neuropathic pain. Br J Pharmacol. 2001;133(4):586–94. https://doi.org/10.1038/sj.bjp.0704110.
Khasabova IA, Khasabov S, Paz J, Harding-Rose C, Simone DA, Seybold VS. Cannabinoid type-1 receptor reduces pain and neurotoxicity produced by chemotherapy. J Neurosci. 2012;32(20):7091–101. https://doi.org/10.1523/JNEUROSCI.0403-12.2012.
Khasabova IA, Yao X, Paz J, Lewandowski CT, Lindberg AE, Coicou L, et al. JZL184 is anti-hyperalgesic in a murine model of cisplatin-induced peripheral neuropathy. Pharmacol Res. 2014;90:67–75. https://doi.org/10.1016/j.phrs.2014.09.008.
Harris HM, Sufka KJ, Gul W, ElSohly MA. Effects of delta-9-tetrahydrocannabinol and cannabidiol on cisplatin-induced neuropathy in mice. Planta Med. 2016;82(13):1169–72. https://doi.org/10.1055/s-0042-106303.
Deng LT, Guindon J, Vemuri VK, Thakur GA, White FA, Makriyannis A, et al. The maintenance of cisplatin- and paclitaxel-induced mechanical and cold allodynia is suppressed by cannabinoid CB2 receptor activation and independent of CXCR4 signaling in models of chemotherapy-induced peripheral neuropathy. Mol Pain. 2012;8:12. https://doi.org/10.1186/1744-8069-8-71.
Vera G, Cabezos PA, Martin MI, Abalo R. Characterization of cannabinoid-induced relief of neuropathic pain in a rat model of cisplatin-induced neuropathy. Pharmacol Biochem Behav. 2013;105:205–12. https://doi.org/10.1016/j.pbb.2013.02.008.
O'Hearn S, Diaz P, Wan BA, DeAngelis C, Lao N, Malek L, et al. Modulating the endocannabinoid pathway as treatment for peripheral neuropathic pain: A selected review of preclinical studies. Ann Pallliat Med. 2017;6:S209–S14. https://doi.org/10.21037/apm.2017.08.04.
Guindon J, Lai Y, Takacs SM, Bradshaw HB, Hohmann AG. Alterations in endocannabinoid tone following chemotherapy-induced peripheral neuropathy: Effects of endocannabinoid deactivation inhibitors targeting fatty-acid amide hydrolase and monoacylglycerol lipase in comparison to reference analgesics following cisplatin treatment. Pharmacol Res. 2013;67(1):94–109. https://doi.org/10.1016/j.phrs.2012.10.013.
Williams J, Haller VL, Stevens DL, Welch SP. Decreased basal endogenous opioid levels in diabetic rodents: Effects on morphine and delta-9-tetrahydrocannabinoid-induced antinociception. Eur J Pharmacol. 2008;584(1):78–86. https://doi.org/10.1016/j.ejphar.2007.12.035.
Bujalska M. Effect of cannabinoid receptor agonists on streptozotocin-induced hyperalgesia in diabetic neuropathy. Pharmacology. 2008;82(3):193–200. https://doi.org/10.1159/000156485.
Hasanein P, Parviz M, Keshavarz M, Roohbakhsh A. URB597, an inhibitor of fatty acid amide hydrolase, reduces hyperalgesia in diabetic rats. Can J Physiol Pharmacol. 2009;87(6):432–9. https://doi.org/10.1139/y09-026.
Niphakis MJ, Cognetta AB, Chang JW, Buczynski MW, Parsons LH, Byrne F, et al. Evaluation of NHS carbamates as a potent and selective class of endocannabinoid hydrolase inhibitors. ACS Chem Neurosci. 2013;4(9):1322–32. https://doi.org/10.1021/cn400116z.
Koltyn KF, Brellenthin AG, Cook DB, Sehgal N, Hillard C. Mechanisms of exercise-induced hypoalgesia. J Pain. 2014;15(12):1294–304. https://doi.org/10.1016/j.jpain.2014.09.006.
Acknowledgements
Not applicable
Funding
No sources of funding were used to assist in the preparation of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to generating the idea for the review. Literature searching was done by BL. Critical review of the material was performed by BL and KK. The first draft of the manuscript was written by BL. KK revised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable
Consent for Publication
Not applicable
Competing Interests
Brianna Leitzelar and Kelli Koltyn declare that they have no conflicts of interest relevant to the content of this review.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leitzelar, B.N., Koltyn, K.F. Exercise and Neuropathic Pain: A General Overview of Preclinical and Clinical Research. Sports Med - Open 7, 21 (2021). https://doi.org/10.1186/s40798-021-00307-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40798-021-00307-9