Abstract
Background
Magnetic resonance imaging (MRI) can be used to diagnose breast cancer. Diffusion weighted imaging (DWI) and the apparent diffusion coefficient (ADC) can reflect tumor microstructure in a non-invasive manner. The correct prediction of response of neoadjuvant chemotherapy (NAC) is crucial for clinical routine.
Our aim was to compare ADC values between patients with pathological complete response (pCR) and non-responders based upon a multi-center design to improve the correct patient selection, which patient would more benefit from NAC and which patient would not.
Methods
For this study, data from 4 centers (from Japan, Brazil, Spain and United Kingdom) were retrospectively acquired. The time period was overall 2003–2019. The patient sample comprises 250 patients (all female; median age, 50.5). In every case, pretreatment breast MRI with DWI was performed. pCR was assessed by experienced pathologists in every center using the surgical specimen in the clinical routine work up. pCR was defined as no residual invasive disease in either breast or axillary lymph nodes after NAC. ADC values between the group with pCR and those with no pCR were compared using the Mann–Whitney U test (two-group comparisons). Univariable and multivariabe logistic regression analysis was performed to predict pCR status.
Results
Overall, 83 patients (33.2%) achieved pCR. The ADC values of the patient group with pCR were lower compared with patients without pCR (0.98 ± 0.23 × 10− 3 mm2/s versus 1.07 ± 0.24 × 10− 3 mm2/s, p = 0.02). The ADC value achieved an odds ratio of 4.65 (95% CI 1.40–15.49) in univariable analysis and of 3.0 (95% CI 0.85–10.63) in multivariable analysis (overall sample) to be associated with pCR status. The odds ratios differed in the subgroup analyses in accordance with the molecular subtype.
Conclusions
The pretreatment ADC-value is associated with pathological complete response after NAC in breast cancer patients. This could aid in clinical routine to reduce treatment toxicity for patients, who would not benefit from NAC. However, this must be tested in further studies, as the overlap of the ADC values in both groups is too high for clinical prediction.
Similar content being viewed by others
Background
Breast cancer is a major global health problem and major cause of mortality in women [1]. The average annual female breast cancer incidence rate was 127.3 cases per 100,000 females [2]. Approximately 2.26 million new cases of invasive breast cancer and about 685,000 deaths are expected among women each year worldwide [1].
Imaging plays a major role in diagnosis and treatment planning of breast cancer [3, 4]. The diagnostic imaging gold standard is magnetic resonance imaging (MRI), which combines a high sensitivity and specificity to diagnose breast cancer and has superior accuracy compared to mammography and ultrasonography. It is especially important for surgical and radiation treatment planning.
The MRI protocol is not clearly standardized and there are sequence differences throughout the imaging centers. In daily clinical practice, MRI utilizes T2-weighted with or without fat saturation and dynamic-contrast enhanced T1-weighted sequences [3]. The addition of diffusion-weighted imaging (DWI) can be used as a functional imaging. DWI can be quantified by apparent diffusion coefficient (ADC) [5, 6]. There are still concerns with DWI in clinical routine with not yet standardized imaging technique with different b-values and the proneness for artefacts.
The diagnostic and prognostic benefits of ADC values have been shown in various tumor entities throughout oncologic imaging, including breast cancer [7, 8]. Importantly, ADC inversely correlates with cellularity and/or proliferation activity in different tumors [5]. As such, ADC can discriminate benign from malignant breast lesions [9]. With this approach, it was shown that the use of DWI in the diagnosis of breast cancer can reduce the number of biopsies by approximately 20% due to the correct categorization of benign tumors with a high ADC-value above 1.2 × 10− 3 mm2/s [10]. Moreover, a low value of less than 1.0 × 10− 3 mm2/s was reported to be highly suspicious for malignancy [9].
Furthermore, some authors suggested that ADC can be used for prediction of treatment response to neoadjuvant therapy [11, 12]. So far, Fangberget et al. proposed a cut off value of 1.42 × 10− 3 mm2/s [11]. Using this cut off, pCR can be predicted with sensitivity and specificity of 88% and 80%, respectively [11].
However, there were also negative reports regarding the possible use to predict treatment response to neoadjuvant treatment. For instance, a large meta analysis could not identify relevant differences between tumors with pathological complete response (pCR) and those without utilizing the pretreatment ADC value [13]. Yet, there are also reports that an increase of the ADC value during neoadjuvant therapy might be a valuable biomarker to correctly predict the patients with pCR [14]. Furthermore, the utilization of only the pretreatment ADC value would benefit patients to reduce possible treatment toxicity, which might not be needed in non-responders. Yet, the current most valuable aspect of ADC values is the increase under treatment in follow-up investigations to clearly depict a treatment response.
However, there is still lack of standardisation of ADC values in regard of sequence parameters, scanner technology and ADC measurement technique, which need to be addressed before ADC values are an additional biomarker in clinical routine [7]. This is also one reason why DWI and ADC values are not included into the BIRADS catalogue to date. Previous studies used ADC values to predict pCR status predominantly in single center designs with small patient samples, which reduces possible external translation due to the abovementioned limitations of ADC values. That is why there is need to test the possible clinical benefit in a multi-centric setting.
Therefore, the present study analyzed the pretreatment ADC values to predict breast cancer patients with pCR after neoadjuvant therapy based upon a large patient sample and whether there are differences regarding the molecular subtype of the breast cancer patients.
Methods
Patients and tumors
This study was approved by the institutional review board of the central study center (Ethic Commission of the Medical Faculty, Otto-von-Guericke University Magdeburg, Nr. 36/20). For each center there was an ethical approval regarding the investigation of breast MRI in patient undergoing NAC.
Overall, 250 patients (all females; median age, 50.5; range, 27–84 years, convenience sample) were included in the study. The data was comprised from the following centers: Center 1: A.C. Camargo Cancer Center, São Paulo, SP, Brazil; Center 2: Department of Radiology, Chiba University Graduate School of Medicine, Chiba, Japan; Center 3: Department of Radiology, School of Clinical Medicine, University of Cambridge, Box 218, Cambridge Biomedical Campus, Hills Road, Cambridge CB2 0QQ, UK; Center 4: Departments of Radiology, Hospital Clínic de Barcelona and University of Barcelona Medical School, Barcelona, Spain.
The patients were retrospectively analyzed in the centers including the image analysis. Central statistical analysis was performed. All patients were newly diagnosed breast cancer patients without any previous treatment.
The receptor status of the acquired breast carcinomas was classified according to the St. Gallen consensus meeting [15]. Luminal A carcinomas (hormone receptor positive carcinomas with a Ki-67 expression below 14%) were diagnosed in 41 patients (16.4%), Luminal B carcinomas (hormone receptor positive tumors with a Ki-67 expression over 14%) in 75 patients (30.0%), HER2-enriched carcinomas in 69 cases (27.6%), and triple negative carcinomas in 65 patients (26.0%).
Pathological differentiation of the carcinomas was as follows: well-differentiated (grade 1) was diagnosed in 13 cases (5.2%), moderately differentiated (grade 2) in 118 cases (47.2%) and poorly differentiated (grade 3) tumors in 107 cases (42.8%). In 12 cases no information regarding the differentiation was provided (4.8%).
Furthermore, the included tumors were staged as T1 in 28 cases (10.9%), T2 in 162 cases (64.8%), T3 in 53 cases (21.2%), and T4 in 7 cases (2.8%). T-stage was obtained before the treatment.
There were no tumors with distant metastases (M1 stage), as was confirmed by clinical routine within the centers.
In all cases, MRI with DWI was performed on 1.5 or 3.0 T clinical scanners with dedicated breast radiofrequency coils. Table 1 provides information regarding the utilized sequence parameters. MRI was performed in all centers before any form of treatment. NAC was chosen as a therapeutic avenue for selected high-risk breast cancers, tumours ≥2 cm and for locally advanced (including initially ineligible for resection) disease.
ADC values
The ADC values were measured on the ADC map with a region of interest (ROI) on the representative slide within the tumor boundaries defined by T1-weighted contrast enhanced images. The ROI was standardized placed within the whole tumor within the tumor boundaries. The measurements were performed in each center by an experienced radiologist.
Neoadjuvant chemotherapy regimen
Neoadjuvant chemotherapy regimen differed between the included centers. In center 1, the regimen consisted of four cycles of anthracycline and cyclophosphamide at intervals of 3–4 weeks followed by four cycles of weekly paclitaxel (AC-T) (n = 37). Trastuzumab was added to this regimen (AC-T) in the 16 cases with HER-2 overexpression. In center 2, neoadjuvant chemotherapeutic regimens consisted of adriamycin 60 mg/m2 and cyclophosphamide 600 mg/m2 once every 3 weeks, followed by 12 weekly doses of paclitaxel 80 mg/m2 (n = 18) and 4 cycles of 5-fluorouracil 500 mg/m2, epirubicin 100 mg/m2, and cyclophosphamide 500 mg/m2 (FEC100) once every 3 weeks, followed by 4 cycles of paclitaxel 175 mg/m2 once every 3 weeks (n = 38). In center 3, The regimen consisted of docetaxel 100 mg/m2 once every 21 days for three cycles, followed by fluorouracil 500 mg/m2, epirubicin 100 mg/m2, with cyclophosphamide 500 mg/m2 (FEC) once every 21 days for three cycles if the tumour was negative for human epidermal growth factor 2 (HER2−) on biopsy. Lastly, in center 4, HER2-negative tumors, either ER positive or ER negative, were treated with six cycles of anthracycline and taxane in combination over 5–6 months. In HER2-positive tumors, trastuzumab was added to the chemotherapy. The time interval between NAC and surgical therapy was 3 months.
pCR
pCR was assessed by experienced pathologists in every center using the surgical specimen in the clinical routine work up. PCR was defined as no residual invasive disease in either breast or axillary lymph nodes after NAC. PCR was defined in accordance to the Residual Cancer Burden (RCB) protocol in three centers [16] and in accordance to the Japanese Breast Cancer Society criteria [17] in one center.
Statistical analysis
For statistical analysis the SPSS statistical software package (SPSS 25, SPSS Inc., Chicago IL, USA) was used. Continuous variables were described using mean, median and standard deviation. Categorical variables were given as absolute and relative frequencies. ADC values between different groups were compared using the Mann–Whitney U test (two-group comparisons). Correlation analysis was performed with Pearson’s correlation coefficient. Univariable and multivariable logistic regression analysis was performed.
Results
Pretreatment ADC values
The pretreatment mean ADC value in the whole patient sample was 1.037 ± 0.24 × 10− 3 mm2/s, range 0.36–2.0 × 10− 3 mm2/s. Table 2 provides ADC values in accordance to the tumor molecular subtypes. Luminal B carcinomas had lower ADC values compared with Luminal A (p = 0.025), HER2-enriched carcinomas (p = 0.004) and with triple negative carcinomas (p = 0.004). No relevant differences were identified between Luminal A, HER2-enriched and triple negative carcinomas.
There was no correlation between ADC and T-Stage (r = 0.04, p = 0.50, Pearson’s correlation analysis). A weak inverse correlation was identified between ADC and histopathological tumor grade (r = − 0.14, p = 0.03).
pCR status
In the overall study sample, 83 patients (33.2%) achieved pCR. In the Luminal A subgroup, only 2 tumors (5%) achieved pCR and in 38 tumors (95%) no pCR was found. In the Luminal B subgroup, in 11 cases (14.7%) pCR was diagnosed and in 63 lesions (85.3%) residual tumor was identified. In the HER2-enriched subgroup, 34 tumors (49.3%) achieved pCR and in 35 cases (51.7%) residual tumors were detected. Finally, in the triple negative subgroup, in 36 lesions (55.4%) pCR and in 29 lesions (44.6%) residual tumors were diagnosed.
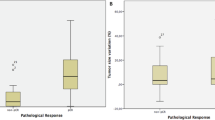
Associations between ADC and pCR
The ADC values of the patient group with pCR were lower compared with patients without pCR (0.98 ± 0.23 × 10− 3 mm2/s versus 1.07 ± 0.24 × 10− 3 mm2/s, p = 0.02). Figure 1 displays the corresponding scatter plot.
In regression analysis the ADC value achieved an odds ratio of 4.65 (95% CI 1.40–15.49) in univariable analysis and of 3.0 (95% CI 0.85–10.63) in multivariable analysis in the overall patient sample (Table 3). The odds ratios differed in the subgroup analyses in accordance with the molecular subtype (Table 3). The highest odds ratio was achieved for the HER2 enriched subtype.
Discussion
The present study investigated the ability of pretreatment ADC to predict pCR in breast cancer patients undergoing neoadjuvant chemotherapy. The prediction of treatment outcome could be very important for clinical care. In fact, accurate prediction of treatment response using imaging could help to individualize treatment and to avoid ineffective chemotherapy in patients.
A key finding of the present study was the dependence of the molecular subtype for the association between pCR and pretreatment ADC values. In fact, pCR is the best outcome for neoadjuvant chemotherapy in breast cancer patients [18, 19]. As reported previously, it is an important prognostic factor for both disease-free survival and overall survival in patients with breast cancer [18, 19]. So far, patients with pCR of breast cancer have an improved 5-year disease-free survival rate of 87% and a 5-year overall survival rate of 89% in comparison to patients without pCR [20].
Previously, a meta analysis including 13 studies with 575 patients identified that the pooled sensitivity and specificity of MRI in prediction of pCR was 0.88 (95% CI, 0.78; 0.94) and 0.69 (95% CI, 0.51; 0.83), respectively [21]. The included studies used morphological MRI data including T2 weighted and dynamic contrast enhanced (DCE-MRI) images but not DWI. In another meta analysis investigating only studies with DCE-MRI, a pooled sensitivity of 0.80 (95% CI, 0.70, 0.88) and a specificity of 0.84 (95% CI; 0.79, 0.88) was identified [22]. While the sensitivity can be considered as sufficient for clinical routine, there is still lack of specificity. Presumably, the addition of another diagnostic MRI sequence might improve diagnostic results.
The present study provides new data regarding the subtypes as well as multivariable analyses, which were not as clearly stated before. It was shown that ADC values have the highest statistical association with pCR prediction in the HER2 enriched subtype, which might be caused by the different treatment regimes for this subtype including the addition of trastuzumab. However, the exact underlying reasons for this behaviour remain elusive.
There are several reasons why ADC values might be able to predict pCR. Ideally, neoadjuvant chemotherapy reduces tumor cell count completely. Biologically aggressive tumors particularly benefit from neoadjuvant chemotherapy, as tumors are more vulnerable to chemotherapy when in a proliferation state. ADC correlates inversely with cell count and tumor aggressiveness [6, 9, 23]. The direct inverse associations between ADC values and proliferation potential, quantified by Ki-67 index was shown in several analyses, including for breast cancer patients [24,25,26,27].
It has already been shown that the ADC is a valuable imaging parameter to discriminate benign from malignant tumors, as the proposed threshold of 1.0 × 10− 3 mm2/s was identified in a large meta analysis based upon 13,847 lesions [9]. In another recent study, ADC values were also capable of reducing biopsies in BIRADS 4 lesions in up to 32.6% of cases [10].
One key fact is that ADC values increased during/after neoadjuvant chemotherapy as another important discriminating parameter to assess treatment response [14, 27]. Numerous studies confirmed this hypothesis including a large multicenter trial based in North America in a prospective setting [14]. Moreover, increase of ADC values during neoadjuvant chemotherapy was more useful than tumor size or volume change after therapy [28]. As such, most studies utilized the difference between the pretreatment ADC value and the ADC value after treatment to predict pCR.
However, a more important question is whether it is possible to predict the effect of neoadjuvant chemotherapy accurately based on pretreatment values. The reported data using pretreatment ADC are contradictory [13]. While some authors found an association between pretreatment ADC and pCR after neoadjuvant chemotherapy, others did not. Bedair et al. reported that responders had lower pretreatment ADC values (× 10− 3 mm2/s) in comparison to non-responders, namely 0.92 ± 0.02 and 1.20 ± 0.02, respectively (p < 0.001) [29]. Similar results were reported by Liu et al. based upon a large retrospective study with 176 patients [30]. In this study different cut-off values were also proposed in accordance with the molecular subtype. Thus, triple negative cancers had the highest ADC-cut off value with 1.43 × 10− 3 mm2/s, whereas Luminal B had the lowest with 1.33 × 10− 3 mm2/s [30]. One reason for the identified results for treatment response prediction could be seen in these reported inherent differences of ADC values according to the subtypes. Yet, there is definite need for further research in this regard.
However, in the study of Bufi et al. there were no relevant differences of pretreatment ADC values between responders and non-responders: 1.13 ± 0.19 vs 1.09 ± 0.19 (× 10− 3 mm2/s), respectively, concluding that pretreatment ADC values are not a useful imaging parameter to predict treatment response [31]. Of note, in this study, the most patients had the Luminal A subtype with 143 of 225 patients [31].
In short, the results of using pretreatment ADC values to reliably predict treatment response following neoadjuvant chemotherapy are still conflicting. One strength of our present analysis is the multivariable regression analysis to adjust for potential confounders, which was not performed previously. A recent study employed a multivariable regression analysis to predict pCR based upon 50 patients [32]. While clinical stage and T stage had high associations with pCR, for MRI findings, only the ADC value change below 15% after two cycles of chemotherapy was associated with pCR (OR= 9.865, 95%CI 1.024–95.021) [32].
Choi et al. investigated a novel ADC-parameter, called ADCdiff, which is the difference between the maximum and minimum ADC values [33]. With this approach, the ADCdiff was superior to ADCmean, ADCmax and ADCmin to predict pCR in this study based on 49 patients [33].
The present analysis based on a multicenter cohort showed that pretreatment ADC values are an independent parameter associated with pCR but the baseline ADC values of responders to NAC and non-responders overlapped in a relevant manner. This was also shown for the subgroups, which suggests that pretreatment ADC cannot be used as a reliable prognostic surrogate marker for pCR.
Our study used subgroup analyses to test for differences with regard to the immunohistochemical subtype. The correct classification of subtype is crucial due to differences in approach to treatment as well as prognostic implications.
One noteworthy study used 18F-labeled fluorodeoxyglucose positron emission tomography-computed tomography (PET-CT) to predict the response to trastuzumab or pertuzumab in HER2-positive breast cancer [34]. The primary endpoint was however not met and the area under the curve was only 0.72 (80% CI, 0.64 to 0.80) [34]. One can conclude that even FDG-PET-CT is not able to reliably predict treatment response in the HER-2-enriched subtype.
The present results are based upon large multi-center data, which identified distinctive differences of the associations between pretreatment ADC values and treatment response accordingly to the molecular subtype. Further prospective studies are needed to assess the discriminative power of pretreatment ADC values.
Our analysis has some limitations to address. First, the multi-center cohort was acquired in a retrospective manner with possible inherent bias. Second, the image reading was not performed in a centrally reading session. It was performed in each center by experienced radiologists. There might be some bias obtained by the different readers. However, it was shown that ADC is a reliable imaging biomarker with low interreader heterogeneity and high reproducibility [35, 36]. Third, the centers used different MRI scanners and different DWI sequences, which results in heterogeneity of the ADC values. Beyond that, an important point is that the diffusion time of the included DWI sequences differed between the centers, which could not be accounted for. Standardisation must be achieved to establish ADC values as an imaging biomarker into clinical routine. Fourth, pCR was defined using different classification criteria. This might result in bias but it represents daily clinical care, as these classifications are used in the different centers in clinical routine.
Conclusion
The pretreatment ADC is associated with pathological complete response after neoadjuvant therapy in breast cancer patients. This could aid in clinical routine to reduce treatment toxicity for patients, who would not benefit from NAC However, this must be tested in further studies, as the overlap of the ADC values between the groups is too high for clinical prediction.
Availability of data and materials
The data that support the findings of this study are available from professor Surov but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of professor Surov.
Abbreviations
- pCT:
-
Pathological complete response
- ADC:
-
Apparent diffusion coefficient
- PET-CT:
-
Positron emission tomography-computed tomography
- NAC:
-
Neoadjuvant chemotherapy
References
Barrios CH, Reinert T, Werutsky G. Global breast cancer research: moving forward. Am Soc Clin Oncol Educ Book. 2018;38:441–50.
Miller KD, Fidler-Benaoudia M, Keegan TH, Hipp HS, Jemal A, Siegel RL. Cancer statistics for adolescents and young adults, 2020. CA Cancer J Clin. 2020;70:443–59.
Leithner D, Wengert GJ, Helbich TH, Thakur S, Ochoa-Albiztegui RE, Morris EA, et al. Clinical role of breast MRI now and going forward. Clin Radiol. 2018;73:700–14.
Dialani V, Chadashvili T, Slanetz PJ. Role of imaging in neoadjuvant therapy for breast cancer. Ann Surg Oncol. 2015;22:1416–24.
Padhani AR, Liu G, Koh DM, Chenevert TL, Thoeny HC, Takahara T, et al. Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations. Neoplasia. 2009;11:102–25.
Surov A, Meyer HJ, Wienke A. Correlation between apparent diffusion coefficient (ADC) and cellularity is different in several tumors: a meta-analysis. Oncotarget. 2017;8:59492–9.
Baltzer P, Mann RM, Iima M, Sigmund EE, Clauser P, Gilbert FJ, et al. Diffusion-weighted imaging of the breast-a consensus and mission statement from the EUSOBI international breast diffusion-weighted imaging working group. Eur Radiol. 2020;30:1436–50.
Mannelli L, Nougaret S, Vargas HA, Do RK. Advances in diffusion-weighted imaging. Radiol Clin N Am. 2015;53:569–81.
Surov A, Meyer HJ, Wienke A. Can apparent diffusion coefficient (ADC) distinguish breast cancer from benign breast findings? A meta-analysis based on 13 847 lesions. BMC Cancer. 2019;19:955.
Clauser P, Krug B, Bickel H, Dietzel M, Pinker K, Neuhaus VF, et al. Diffusion-weighted imaging allows for downgrading MR BI-RADS 4 lesions in contrast-enhanced MRI of the breast to avoid unnecessary biopsy. Clin Cancer Res. 2021;27:1941–8.
Fangberget A, Nilsen LB, Hole KH, Holmen MM, Engebraaten O, Naume B, et al. Neoadjuvant chemotherapy in breast cancer-response evaluation and prediction of response to treatment using dynamic contrast-enhanced and diffusion-weighted MR imaging. Eur Radiol. 2011;21:1188–99.
Richard R, Thomassin I, Chapellier M, Scemama A, de Cremoux P, Varna M, et al. Diffusion-weighted MRI in pretreatment prediction of response to neoadjuvant chemotherapy in patients with breast cancer. Eur Radiol. 2013;23:2420–31.
Surov A, Wienke A, Meyer HJ. Pretreatment apparent diffusion coefficient does not predict therapy response to neoadjuvant chemotherapy in breast cancer. Breast. 2020;53:59–67.
Partridge SC, Zhang Z, Newitt DC, Gibbs JE, Chenevert TL, Rosen MA, et al. Diffusion-weighted MRI findings predict pathologic response in neoadjuvant treatment of breast cancer: the ACRIN 6698 multicenter trial. Radiology. 2018;289:618–27.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ, et al. Strategies for subtypes--dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–47.
Symmans WF, Peintinger F, Hatzis C, Rajan R, Kuerer H, Valero V, et al. Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J Clin Oncol. 2007;25:4414–22.
Kurosumi M, Akashi-Tanaka S, Akiyama F, Komoike Y, Mukai H, Nakamura S, et al. Histopathological criteria for assessment of therapeutic response in breast cancer (2007 version). Breast Cancer. 2008;15:5–7.
Cortazar P, Geyer CE Jr. Pathological complete response in neoadjuvant treatment of breast cancer. Ann Surg Oncol. 2015;22:1441–6.
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Brackstone M, Palma D, Tuck AB, Scott L, Potvin K, Vandenberg T, et al. Concurrent neoadjuvant chemotherapy and radiation therapy in locally advanced breast cancer. Int J Radiat Oncol Biol Phys. 2017;99:769–76.
Li H, Yao L, Jin P, Hu L, Li X, Guo T, et al. MRI and PET/CT for evaluation of the pathological response to neoadjuvant chemotherapy in breast cancer: a systematic review and meta-analysis. Breast. 2018;40:106–15.
Cheng Q, Huang J, Liang J, Ma M, Ye K, Shi C, et al. The diagnostic performance of DCE-MRI in evaluating the pathological response to neoadjuvant chemotherapy in breast Cancer: a Meta-analysis. Front Oncol. 2020;10:93.
Durando M, Gennaro L, Cho GY, Giri DD, Gnanasigamani MM, Patil S, et al. Quantitative apparent diffusion coefficient measurement obtained by 3.0Tesla MRI as a potential noninvasive marker of tumor aggressiveness in breast cancer. Eur J Radiol. 2016;85:1651–8.
Surov A, Meyer HJ, Wienke A. Associations between apparent diffusion coefficient (ADC) and KI 67 in different tumors: a meta-analysis. Part 1: ADCmean. Oncotarget. 2017;8:75434–44.
Mori N, Ota H, Mugikura S, Takasawa C, Ishida T, Watanabe G, et al. Luminal-type breast cancer: correlation of apparent diffusion coefficients with the Ki-67 labeling index. Radiology. 2015;274:66–73.
Zhang Y, Zhu Y, Zhang K, Liu Y, Cui J, Tao J, et al. Invasive ductal breast cancer: preoperative predict Ki-67 index based on radiomics of ADC maps. Radiol Med. 2020;125:109–16.
Luo N, Ji Y, Huang X, Liu Y, Liu L, Jin G, et al. Changes in apparent diffusion coefficient as surrogate marker for changes in Ki-67 index due to neoadjuvant chemotherapy in patients with invasive breast cancer. Acad Radiol. 2019;26:1352–7.
Pereira NP, Curi C, Osório CABT, Marques EF, Makdissi FB, Pinker K, et al. Diffusion-weighted magnetic resonance imaging of patients with breast Cancer following neoadjuvant chemotherapy provides early prediction of pathological response - a prospective study. Sci Rep. 2019;9:16372.
Bedair R, Priest AN, Patterson AJ, McLean MA, Graves MJ, Manavaki R, et al. Assessment of early treatment response to neoadjuvant chemotherapy in breast cancer using non-mono-exponential diffusion models: a feasibility study comparing the baseline and mid-treatment MRI examinations. Eur Radiol. 2017;27:2726–36.
Liu S, Ren R, Chen Z, Wang Y, Fan T, Li C, et al. Diffusion-weighted imaging in assessing pathological response of tumor in breast cancer subtype to neoadjuvant chemotherapy. J Magn Reson Imaging. 2015;42:779–87.
Bufi E, Belli P, Costantini M, Cipriani A, Di Matteo M, Bonatesta A, et al. Role of the apparent diffusion coefficient in the prediction of response to neoadjuvant chemotherapy in patients with locally advanced breast cancer. Clin Breast Cancer. 2015;15:370–80.
Lu N, Dong J, Fang X, Wang L, Jia W, Zhou Q, et al. Predicting pathologic response to neoadjuvant chemotherapy in patients with locally advanced breast cancer using multiparametric MRI. BMC Med Imaging. 2021;21:155.
Choi BB. Effectiveness of ADC difference value on pre-neoadjuvant chemotherapy MRI for response evaluation of breast Cancer. Technol Cancer Res Treat. 2021;20:15330338211039129.
Connolly RM, Leal JP, Solnes L, Huang CY, Carpenter A, Gaffney K, et al. Updated results of TBCRC026: phase II trial correlating standardized uptake value with pathological complete response to Pertuzumab and Trastuzumab in breast cancer. J Clin Oncol. 2021;39:2247–56.
Clauser P, Marcon M, Maieron M, Zuiani C, Bazzocchi M, Baltzer PA. Is there a systematic bias of apparent diffusion coefficient (ADC) measurements of the breast if measured on different workstations? An inter- and intra-reader agreement study. Eur Radiol. 2016;26:2291–6.
Newitt DC, Zhang Z, Gibbs JE, Partridge SC, Chenevert TL, Rosen MA, et al. Test-retest repeatability and reproducibility of ADC measures by breast DWI: results from the ACRIN 6698 trial. J Magn Reson Imaging. 2019;49:1617–28.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
AS made substantial contributions to conception and design, analysis and interpretation of the data; AS wrote the manuscript; GB, AGVB, HF, GS, FJG performed acquisition of the data; AW performed statistical analysis of the data. AS, MP, HJM, AW, GB, AGVB, HF, GS, FJG been involved in drafting the manuscript or revising it critically for important intellectual content; MP, HJM, AW, GB, AGVB, HF, GS, FJG given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content; and MP, HJM, AW, GB, AGVB, HF, GS, FJG MP, HJM, AW, GB, AGVB, HF, GS, FJG agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Surov, A., Pech, M., Meyer, HJ. et al. Evaluation of pretreatment ADC values as predictors of treatment response to neoadjuvant chemotherapy in patients with breast cancer - a multicenter study. Cancer Imaging 22, 68 (2022). https://doi.org/10.1186/s40644-022-00501-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40644-022-00501-2