Abstract
Objective
The sleep of healthcare students is worth discovering. Mental health and self-rated health are thought to be associated with sleep quality. As such, valid instruments to assess sleep quality in healthcare students are crucial and irreplaceable. This study aimed to investigate the measurement properties of the Sleep Quality Questionnaire (SQQ) for Chinese healthcare students.
Methods
Two longitudinal assessments were undertaken among healthcare students, with a total of 595, between December 2020 and January 2021. Measures include the Chinese version of the SQQ, Patient Health Questionnaire-4 (PHQ-4), Self-Rated Health Questionnaire (SRHQ), and sociodemographic questionnaire. Structural validity through confirmatory factor analysis (CFA) was conducted to examine factor structure of the SQQ. T-tests and ANOVAs were used to examine sociodemographic differences in sleep quality scores. Multi Group CFA and longitudinal CFA were respectively used to assess cross-sectional invariance and longitudinal invariance across two-time interval, i.e., cross-cultural validity. Construct validity, internal consistency, and test–retest reliability were correspondingly examined via Spearman correlation, Cronbach’s alpha and McDonald’s omega, and intraclass correlation coefficient. Multiple linear regression analysis was performed to examine incremental validity of the SQQ based on the PHQ-4 and SRHQ as indicators of the criterion variables.
Results
CFA results suggested that the two-factor model of the SQQ-9 (item 2 excluded) had the best fit. The SQQ-9 scores differed significantly by age, grade, academic stage, hobby, stress coping strategy, anxiety, depression, and self-rated health subgroups. Measurement invariance was supported in terms of aforesaid subgroups and across two time intervals. In correlation and regression analyses, anxiety, depression, and self-rated health were moderately strong predictors of sleep quality. The SQQ-9 had good internal consistency and test–retest reliability.
Conclusion
Good measurement properties suggest that the SQQ is a promising and practical measurement instrument for assessing sleep quality of Chinese healthcare students.
Similar content being viewed by others
Introduction
Sleep health has become an important public health concern and is composed of six dimensions: regularity, satisfaction or quality, alertness or sleepiness, timing, efficiency or continuity, and duration [1]. “Sleep quality” is defined as an individual’s self-satisfaction in all aspects of sleep, and is used to refer to subtle aspects of the sleep experience, which cannot be captured by objective sleep parameters [2, 3]. To date, the concept of sleep quality does not have a consensus definition, but it is generally believed to be comprised of several factors: sleep continuity, sleep efficiency, sleep latency, sleep duration, awakening, and wakefulness after falling asleep [4, 5]. Even though the fact that polysomnographic parameters are considered the gold standard for measuring sleep [5, 6], common sentiment is that sleep quality considered as “subjective perception of sleep” [7]. In other words, a subjective evaluation of sleep quality may better explain everyday psychological and behavioral performance which is not captured by objective measurements [8].
Poor sleep quality has arisen as a widespread issue, with nearly one-third of adults claiming to experience dissatisfaction with their sleep [9, 10]. Numerous previous studies have found that university students and healthcare workers are at increased risk for sleep problems [11, 12]. Healthcare students, a subgroup of university students, have a significantly higher prevalence of poor sleep quality than non-medical students and general population [13, 14]. Healthcare students experience noticeable sleep issues which were primarily related to their intense academic requirements and high achievement expectations [15]. COVID-19 pandemic and associated lockdown may have contributed to a higher prevalence of sleep problems in healthcare students [13, 16, 17]. Despite healthcare students as a clinical or research sample have a significant risk for sleep disorders, did not lead to academic circles adequate attention [18].
Quality sleep is an essential part of a healthy lifestyle. Factors that influence sleep quality in healthcare students include physiological (e.g., age, BMI), psychological (e.g., stress, anxiety, and depression) [19,20,21], environmental (e.g., bedroom light, room temperature, and noise), and family/social expectations [4]. Importantly, psychological distress and sleep problems demonstrate a bidirectional relationship [17]. To mitigate negative effects of poor quality on their psychosomatic health, accurate monitoring and prompt diagnosis are vital, particularly in healthcare students [22, 23].
As noted previously, objective sleep measures have trouble applying in widespread applicability [6]. Scales for subjective measurement of sleep quality are widely used in research and clinical practice, with common scales including the Pittsburgh Sleep Quality Index (PSQI) [24], the Sleep Quality Scale [25], the Sleep Quality Index [26], and the Sleep Satisfaction Tool [27]. In China, existing sleep-related scales focused on assessing nighttime sleep or were designed for explicitly for clinical settings and patients. The assessment of sleep quality is not limited to nocturnal symptoms and includes many daytime consequences of poor nighttime sleep [28]. The Sleep Quality Questionnaire (SQQ) is a concise psychometrically sound instrument developed specifically for evaluating sleep quality across two core dimensions (Sleep Difficulty and Daytime Sleepiness) via 10 items among non-clinical populations [29].
The Chinese version of the SQQ (SQQ-C) has been translated, adapted, and validated, demonstrating equivalence between the two versions while maintaining original measurement properties [30,31,32]. The SQQ demonstrated a two-factor structure in both the original Japanese and Chinese versions. Credibility and applicability of the SQQ has been established via the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) guidelines [33, 34]. Nonetheless, discriminant validitsy of the SQQ-C has not been fully established, and some discrepancies exist regarding factor loadings. The original version suggested that sleep quality measured by the SQQ was a strong predictor of general health; however, less was known about its association with anxiety and depressive symptoms. This study aims to further establish measurement properties of the SQQ among Chinese healthcare students. We examined discriminant validity of the SQQ-C with other constructs including anxiety, depression, and self-rated health. Furthermore, we performed multiple linear regression analysis to examine incremental validity of the SQQ with the Generalized Anxiety Disorder-2 (GAD-2), Patient Health Questionnaire-2 (PHQ-2), and Self-Rated Health Questionnaire (SRHQ).
Methods
Participants and procedures
This study focuses on freshman to junior undergraduate and freshman postgraduate students who are attending regular classes at university. College seniors are at a developmentally distinct phase of their educational journeys. Considering that seniors are facing more stressful life events such as graduation, job search, and clinical internship, as they are making a shift from student to worker, we excluded this population. More specifically, for undergraduate students: a group of students from the first to the third year of health management, nursing, pharmacy, clinical medicine, preventive medicine, and health services management majors were selected as a teaching class; and for postgraduate students: all first-year students in health management, health services management, and public health majors. All study data was collected via short paper-and-pencil questionnaires in two waves between December 2020 and January 2021 at a university in Hangzhou, China (an area at low risk for COVID-19 infection during data collection). Data collection was conducted during breaks between classes. Only full-time students attending classes on-site were recruited; students on suspension and long-term sick leave were excluded. Following the instructions of the study protocol, informed consent was obtained from each participant.
Baseline assessment (Time 1, T1) included a brief sociodemographic questionnaire and a small packet of scales, as described below. A follow-up assessment (Time 2, T2) was conducted approximately one week after T1 and included all measures at T1 except for the demographic survey. The average time interval between T1 and T2 was 7 days + 16.62 hours. The reproducibility of health measurements is optimized at intervals of 1–2 weeks [35]. Six hundred and thirty-seven (N1 = 637) and six hundred and sixteen (N2 = 616) valid data were obtained at T1 and T2, respectively. Both assessments included unique student ID of each respondent. The last author manually matched with ID across two assessment questionnaires via Microsoft Excel, thereby resulting in a matched sample (N = 595).
The study protocol was approved by the Institutional Review Board of Hangzhou Normal University Division of Health Sciences, China (Reference No. 20190076). The process was carried out following the principles of the Declaration of Helsinki [36].
Measures
Sociodemographic questionnaire
During the baseline, participants were asked to provide demographic information, including gender, age, grade, academic stage (undergraduate, postgraduate), home location (urban, rural, suburban), being only child (yes, no), monthly household income (1 CNY ≈ 0.160 US dollars), part-time job (yes, no), physical exercise [purposeful exercise with the goal of improving health (yes, no)], hobby [regularly and frequently engage in activities or projects of their preference (yes, no)], frequency of visiting home (once per week, twice per week, once per month, once per quarter, once per semester, and once per academic year), and stress coping strategy [the most customary way of coping when faced with stress (emotion-focused, solution-focused, avoidance coping)].
To facilitate meaningful data analysis, we grouped age, monthly household income, and frequency of visiting home as follows: 1) Age: < 20 years and ≥ 20 years, 2) Monthly household income: below and above the average household income (10 000 CNY) of a three-member family in China in 2021 [37], 3) Frequency of visiting home: frequently versus occasionally.
Sleep Quality Questionnaire (SQQ)
The original SQQ is a 10-item scale consisting of the Sleep Difficulty Subscale (SDS, e.g., “I had trouble sleeping”) and Daytime Sleepiness Subscale (DSS, e.g., “I sometimes felt sleepy during the day”), which is used to assess subjective sleep quality over the past month in non-clinical samples [29]. Responses are recorded on a five-point Likert scale ranging from 0 to 4 (with 0 indicating “strongly disagree” and 4 indicating “strongly agree”). Global scores range from 0 to 40 with a higher score indicating poorer subjective sleep quality. Previous studies have demonstrated that the SDS was stably loaded by three items (items 1, 4, 9), while the DSS was loaded by six items (items 3, 5, 6, 7, 8, 10). Item 2 of the SQQ showed cross-loading in both the original and Chinese versions. The strong psychometric properties observed in previous studies have promoted wide usage of the SQQ-C as a practical measurement instrument in research and survey sites [30, 32].
Patient Health Questionnaire‑4 (PHQ‑4)
The PHQ is a self-report version of the Primary Care Evaluation of Mental Disorders (PRIME-MD) [38], both the original and derived scales are available from the ‘Patient Health Questionnaire (PHQ) Screeners website’ [39]. The PHQ-4 [40], consisting of the PHQ-2 (e.g., “Little interest or pleasure in doing things”) and GAD-2 (e.g., “Feeling nervous, anxious, or on edge”), are two extensively used ultra-short screening tools to measure depressive disorder and anxiety symptoms. In fact, the PHQ-4 was originally designed for patients, yet subsequent studies have continued to advance the validation and applicability of the PHQ-4 in the general population [41, 42]. Each item of the PHQ-4 is scored on a four-point Likert scale ranging from 0 (not at all) to 3 (nearly every day), with higher global scores being indicative of higher levels of depressive and anxiety symptoms. For the PHQ-2 and GAD-2, a scale score of ≥ 3 is recommended as a cut-off point between the normal range and possible cases of depression or anxiety, respectively.
Self-Rated Health Questionnaire (SRHQ)
The SRHQ is a simple questionnaire consisting of two items that assess self-rated physical health and mental health, respectively [43]. The SRHQ utilizes a five-point Likert scale from 1 (excellent) to 5 (extremely poor), with higher total scores implying poorer self-rated health status.
Statistical Analyses
All statistical analyses were completed with R (4.1.3) and JASP (0.16.1). R packages of “lavvan (0.6–11)” [44], “MBESS (4.9.1)” [45], “irr (0.84.1)” [46], and “semTools (0.5–6)” [47] were applied. The missing rate of data was smaller than 5% (ranged from 0.168% to 1.681%), therefore the mean (continuous variables) or median (categorical variables) was used to impute missing values, treating the same methods as in our previously publications. Differences in sleep quality levels based on sociodemographic characteristics were analyzed using t-tests and ANOVA. Multiple regression models were used to examine incremental validity of the SQQ with the PHQ-4 and SRHQ as indicators of criterion variables. Following the COSMIN guidelines, different metrics were applied to assess measurement properties of the SQQ [33, 34], a brief description is provided with undermentioned items.
Structural validity
Based on a previous study [30], we conducted CFA on three alternative models of the SQQ: item 2 loading on the SDS (Factor 2), item 2 loading on the DSS (Factor 1), and the SQQ-9 (item 2 excluded). The weighted least squares mean and variance adjustment (WLSMV) method was used for all CFA analyses, given that the data were ordinal [48]. The indexes of goodness-of-fit used were the chi-square (χ²) value, P value, comparative fit index (CFI), Tucker-Lewis index (TLI), Akaike information criterion (AIC), Bayesian information criterion (BIC), and root means square error of approximation (RMSEA). For interpretation purposes: smaller values of AIC and BIC suggest a better model fit, CFI and TLI ≥ 0.90, RMSEA ≤ 0.08 are considered adequate and CFI and TLI ≥ 0.95, RMSEA ≤ 0.05 are considered good [49,50,51]. χ² is considered as sensitive in large samples and tends to reject the optimal model as the sample size increases, we do not use it as the only criterion for the goodness-of-fit judgment.
Cross-cultural validity/measurement invariance
Multi Group CFA and longitudinal CFA were conducted for testing measurement invariance (MI) of the SQQ-C for sociodemographic variables and across time intervals, respectively. In cross-population and cross-time applications of the scale, the establishment of MI means that construct measured by instrument does not change with population heterogeneity and over time. MI will be established on unbiased latent construct comparisons across groups and time. Increasingly constrained and nested models are stacked and tested against each other. That is, the SQQ has the same interpretation: the measurement structure and domain are relatively stable [52], with strict model invariance being well-validated [53].
Four nested models including configural, metric, scalar, and strict models were tested. Configural invariance requires only the same basic structural relations between observed variables. Metric invariance implies similar measurement constructs and limits factor loading to be equivalent across groups. Scalar invariance limits factor loadings and intercepts, meaning that the systematic bias of measurement content is consistent across groups and time. Strict invariance proves that group differences are caused by latent variables by limiting item residuals [54]. The fit indexes CFI, TLI, and RMSEA were applied on evaluating the goodness of model fit, changes (Δ) in CFI were used to assess whether there was invariance between progressively constrained models, where ΔCFI ≤ 0.010 was considered satisfactory [51, 55].
Construct/discriminant validity
Spearman correlation coefficient was calculated to evaluate construct/discriminant validity of the SQQ total and subscales with the GAD-2, PHQ-2, and SRHQ [56]. Considering the bidirectional association between sleep quality and psychosomatic health, we hypothesized that the SQQ would have a moderately strong correlation (0.30 < r ≤ 0.50) with the GAD-2, PHQ-2, and SRHQ [57].
Internal consistency and test–retest reliability
Ordinal Cronbach’s alpha and McDonald’s omega were calculated to estimate internal consistency of the SQQ and were considered good when they were equal to or greater than 0.70 [45, 55]. Test–retest reliability of the scale was assessed using intraclass correlation coefficient (ICC), with values between 0.50 and 0.75 indicative of moderate reliability, and values between 0.75 and 0.90 indicate good reliability [58]. Meanwhile, standard error of measurement (SEM) was used as a supplementary index to determine measurement accuracy in the evaluation of test–retest reliability [59].
Multivariate regression analyses
Sleep difficulty and daytime sleepiness were used as potential influences on negative symptoms (anxiety and depression) and self-rated health for further multiple linear regression analysis. Baseline sleep quality scores were applied to predict anxiety, depression, and self-rated health scores at follow-up to examine the incremental validity of the SQQ. Confirmation of linear relationship between variables, autocorrelation statistics were performed with the Durbin-Watson test. The variance inflation factor (VIF) was used to evaluate the multicollinearity between variables, and less than 10 was considered to be the absence of collinearity [60].
Results
Participants
The final 595 participants (Table 1) included in this study ranged in age from 17 to 31, with an average age of 19.857 ± 1.625 years. Among respondents, 554 (93.109%) were undergraduates and 41 (6.891%) were postgraduates. The average score of the SQQ-9, SQQ, PHQ-4, and SRHQ at each timepoint was 15.968 ± 5.449, 18.111 ± 6.102, 3.726 ± 2.390, and 4.598 ± 1.210 at T1, 16.114 ± 5.438, 18.237 ± 6.095, 3.508 ± 2.107, and 4.418 ± 1.120 at T2, separately. Table S1 (Additional file) lists the description of item and factor scores for the main variables.
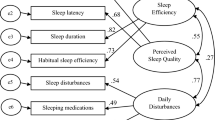
Structural validity
We tested three alternative models (i.e., item 2 in the SDS, item 2 in the DSS, and item 2 excluded) for CFA (Table 2). It is evident that the item 2 in the SDS model (original model) obtained an inadequate fit, while the SQQ-9 (item 2 excluded) model slightly outperformed the item 2 in the DSS model in terms of fit indices (except RMSEA). The smaller AIC and BIC values of the SQQ-9 model imply that there is greater stability and applicability of the SQQ toward Chinese healthcare students.
Sociodemographic factors related to sleep quality
There were no significant differences in sleep quality scores between genders, but differences in the SQQ-9 scores between age, grade, and academic stage groups (Table 1). Students who had a hobby and responded to stressful events with a positive attitude had better sleep quality. Meanwhile, students with anxiety symptoms, depressive tendencies, or poor self-rated health had high scores on the SQQ-9.
Cross-cultural validity/measurement invariance
Table 3 presents the results of examining cross-sectional measurement invariance (CMI) among different subgroups. The four models with constrained stepwise invariance assumptions were well-fitted in subgroups for both the baseline and follow-up data: CFI was from 0.953 to 0. 997, TLI was from 0.958 to 0.998, and all REMSA values were less than 0.080. Further, except that the ΔCFI of the metric model in the baseline SRHQ subgroup (-0.011), all the other ΔCFI were in threshold levels. The complete fitting information can be accessed in Additional file: Table S2. Δχ² indicated no significant difference in the invariance of models in nearly all subgroups.
Longitudinal measurement invariance (LMI) across time intervals (Table 4) also shows an excellent fit, with all fit indexes within critical values (CFI: 0.981–0.990, TLI: 0.982–0.989, RMSEA: 0.037–0.047, and SRMR: 0.039–0.042). The change in fit indexes were also in the acceptable range.
Construct/discriminant validity
Parts i and ii of Fig. 1 show the results of Spearman correlation analysis between the SQQ, PHQ-4, and SRHQ items, total scores, and subdomains at T1 and T2, respectively. The coefficients on the left side of the black line are the items, factors and total correlations within the SQQ, and the coefficients on the right side of the black line are discriminative validity estimates between the SQQ with the PHQ-4 and SRHQ. Whether it is 9 items or 10 items, the correlation coefficients between the SQQ with the GAD-2, PHQ-2, PHQ-4, and SRHQ are all moderate in strength (0.30–0.50). Table S3 (Additional file) displays the results of the correlation coefficients combining the two assessments.
Item–factor, factor–total, and discriminant correlations between the SQQ, PHQ-4, and SRHQ (N = 595). Note: Spearman correlations, T1 Time 1, T2 Time 2, SQQ Sleep Quality Questionnaire, SQQ01-10 item 1–10, SDS Sleep Difficulty Subscale, DSS Daytime Sleepiness Subscale, DSS (-) item 2 excluded from the DSS, SQQ-9 item 2 excluded from the SQQ, GAD Generalized Anxiety Disorder, PHQ Patient Health Questionnaire, SRHQ Self-Rated Health Questionnaire
Internal consistency and test–retest reliability
Although the previous CFA suggested that the SQQ-9 was a better model than the original SQQ-10, we still estimated reliability of the original scale and its subscales (Table 5). All ordinal Cronbach’s alpha and McDonald’s omega values are greater than 0.800, and ICC values suggested that the subscales and total scale have excellent reliability except for the SDS (ICC = 0.741). In this study, the GAD-2, PHQ-2, PHQ-4, and SRHQ all showed good reliability (T1: 0.814, 0.747, 0.844, 0.704; T2: 0.784, 0.743, 0.831, 0.710).
Multivariate regression analyses
Multiple linear regression analysis (Table 6) was performed based on the scores of the SDS and DSS for the PHQ-4 and SRHQ. There is a linear relationship between the independent and dependent variables, and VIF value recommended little multicollinearity. Sleep quality as measured by the SQQ predicted 20.7% of anxiety and depressive symptoms and 10.8% of self-rated health, respectively. Overall, β weights for both daytime sleepiness and sleep difficulty scores were significant at the 0.001 level.
Discussion
This study auxiliary examined measurement properties of the SQQ-C in healthcare students. Our findings indicated good structural, cross-cultural, and discriminant validity, adequate internal consistency, and stability of the SQQ-9. CMI was established based on sociodemographic variables that may affect sleep quality. LMI models across time intervals further suggested that the SQQ-9 is a promising and practical measurement instrument for assessing sleep quality. Multiple linear regression results demonstrated that sleep quality measured by the SQQ can be used to predict short-term negative symptoms (anxiety and depression) and self-rated health status.
CFA results suggested that the two-factor SQQ-9 structure fits the data best. Interestingly, such a factor structure is inconsistent with the originally proposed factor structure [29], the same factor structure appeared in our previous study using the SQQ to measure sleep quality in Chinese samples [30]. These studies yielded the SQQ-9 in suggesting that comprehension discrepancy might be due to cross-cultural differences and translation issues.
MI of the SQQ-9 held perfectly for most cross-sectional subgroups and longitudinal interval, as demonstrated by configural, metric, scalar, and strict invariances regardless of gender, age, grade, academic stage, hobby, stress coping strategy, anxiety symptoms, depressive tendencies, self-assessed health status, and across time intervals. In a previous study of healthcare students, it was found that age and gender were not significantly associated with sleep quality or daytime sleepiness [61]. This conclusion was confirmed through our invariance tests, but it was possible due to sampling homogeneity and the narrow range of age. Lastly, we showed the SQQ-9 has strict LMI across two-time intervals, indicating that the SQQ-9 is a stable scale with high reliability.
Our results, as in previous studies, revealed that sleep quality in healthcare students was moderately associated with negative mental states (anxiety and depression) [62, 63]. The findings were also consistent with a previous study on medical students in Malaysia, where daytime sleepiness was more pronounced among medical students who reported poor sleep quality and psychological distress [64].
Cronbach’s alpha, McDonald’s omega, ICC, and SEM were used to measure the reliability of the SQQ. Given that Cronbach’s alpha as an indicator of reliability is still contested [65,66,67], we further demonstrated high internal consistency of the SQQ and its subscales through McDonald’s omega. Both indicators demonstrated a high homogeneity between the SQQ items. Retest intervals of 1 or 2 weeks are considered typical intervals used to validate the reproducibility of health status measures used longitudinally [35, 68]. ICC is a relative measure of reliability and SEM is an indicator of absolute reliability, both showed good test–retest reliability [59]. Collectively, the evidence indicated the SQQ has good reliability.
Multiple linear regression analysis demonstrated that poor sleep quality was a predictor of negative mood (anxiety and depression) and self-rated health status. Sleep problems and mental health issues are common in modern society. Generally, good sleep can relieve psychological problems (e.g., depression, anxiety, and stress), while poor sleep may have negative effects on quality-of-life and academic performance, or vice versa [69, 70]. The relationship between sleep quality and mental health is well documented, in terms of primary prevention, thus sleep improvement represents a viable therapeutic goal that can provide significant benefits to mental health [71].
The importance of sleep to public health and the contribution of insufficient sleep to health disparities deserves to be emphasized. The development of healthy sleep education, especially early intervention on campus, contributes to the development of good sleep habits [72]. Cognitive behavioral therapy for insomnia is considered a first-line treatment for sleep improvement and standardized protocols have been developed [73]. Moreover, this has been found to be effective in reducing psychological problems and improving sleep-related quality of life [74, 75].
The SQQ-9 is a slightly short form determined from factor analysis results. However, the development of ultrashort measurement instruments is a priority and has been recognized as necessary for large-scale population screening (e.g., PHQ-2, GAD-2). In terms of sleep quality assessments, the previously developed single-item Sleep Quality Scale [76], the two-item Sleep Condition Indicator (SCI) [77, 78], and the six-item PSQI [79] suggest that short questionnaires are a potential possibility.
Strengths and limitations
Discriminant validity and incremental validity of the SQQ-C were complemented in this study, we were able to retest almost all participants to examine the stability and establish LMI of the SQQ-C. This study has some limitations. First, generalizability may be limited by the type of university and overrepresentation of female respondents. As such, the extrapolation of conclusions may require more consideration and caution towards other samples. Second, since the survey was conducted during the COVID-19 epidemic and the university was in lockdown (students are not allowed to enter or leave the campus when it is not necessary), students may have been experiencing higher levels of psychological distress and sleep problems. Third, objective measures were not used in the study, and thus results are limited by the self-report nature of the data.
Future directions
The stability and reliability of the SQQ-C should be examined across samples (e.g., occupational population, floating population), locations (e.g., multicenter or multilocation), and settings (e.g., communities, worksites). Similarly, the SQQ-C should be administered with other sleep assessment scales (e.g., PSQI, SCI) that yield cutoff values for good and poor sleep quality, allowing for estimation cutoff points for the SQQ-C. Additionally, including objective sleep measurements (e.g., wristwatch activity recorder, portable sleep monitoring device) in future studies could yield additional insights about sleep quality. Applying the SQQ-C routine monitoring and exploring response shifts in multi-wave would help to further investigate risk or preventive factors related to sleep health [1, 80, 81].
Conclusions
The SQQ-C is a practical psychometrically sound instrument to assess sleep quality, including sleep difficulty and daytime sleepiness, amongst healthcare students. This study demonstrates that the SQQ-9-C has good psychometric properties and measurement invariance. Sleep quality as measured by the SQQ-9-C associated with short-term negative symptoms (i.e., anxiety and depression) and self-rated health status. Our previous and current findings combined suggests that the SQQ-C can be used to accurately measure sleep quality in community and research settings.
Availability of data and materials
All data generated or analyzed during this study are not publicly available due to restrictions imposed by the ethics committee. The dataset supporting the conclusions is available upon reasonable request to the last author. Anyone interested in using the formatted SQQ-C and its scoring rubric should be directed to the last author when ready to initiate research collaboration.
Abbreviations
- AIC:
-
Akaike information criterion
- BIC:
-
Bayesian information criterion
- CFA:
-
confirmatory factor analysis
- CFI:
-
comparative fit index
- CMI:
-
cross-sectional measurement invariance
- COSMIN:
-
COnsensus-based Standards for the selection of health Measurement INstruments
- COVID-19:
-
Corona Virus Disease 2019
- DSS:
-
Daytime Sleepiness Subscale
- GAD:
-
Generalized Anxiety Disorder
- ICC:
-
intraclass correlation coefficient
- KMO:
-
Kaiser–Meyer–Olkin
- LMI:
-
longitudinal measurement invariance
- MI:
-
measurement invariance
- PHQ:
-
Patient Health Questionnaire
- PRIME-MD:
-
Primary Care Evaluation of Mental Disorders
- PSQI:
-
Pittsburgh Sleep Quality Index
- RMSEA:
-
root means square error of approximation
- SCI:
-
Sleep Condition Indicator
- SD:
-
standard deviation
- SDS:
-
Sleep Difficulty Subscale
- SEM:
-
standard error of measurement
- SQQ:
-
Sleep Quality Questionnaire
- SRHQ:
-
Self-Rated Health Questionnaire
- T1:
-
Time1, Baseline
- T2:
-
Time2, Follow-up
- TLI:
-
Tucker-Lewis Index
- VIF:
-
variance inflation factor
- WLSMV:
-
weighted least squares mean and variance adjustment
References
Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17. https://doi.org/10.5665/sleep.3298.
Kline C: Sleep quality. In: Encyclopedia of Behavioral Medicine. edn. Edited by Marc D. Gellman JRT; 2013: 1811–1813 https://doi.org/10.1007/978-1-4419-1005-9_849.
Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med. 2008;9:S10–7. https://doi.org/10.1016/S1389-9457(08)70011-X.
Nelson KL, Davis JE, Corbett CF. Sleep quality: An evolutionary concept analysis. Nurs Forum. 2022;57(1):144–51. https://doi.org/10.1111/nuf.12659.
Ohayon M, Wickwire EM, Hirshkowitz M, Albert SM, Avidan A, Daly FJ, Dauvilliers Y, Ferri R, Fung C, Gozal D, et al. National Sleep Foundation’s sleep quality recommendations: first report. Sleep Health. 2017;3(1):6–19. https://doi.org/10.1016/j.sleh.2016.11.006.
Mendonça F, Mostafa SS, Morgado-Dias F, Ravelo-García AG, Penzel T. A Review of Approaches for Sleep Quality Analysis. IEEE Access. 2019;7:24527–46. https://doi.org/10.1109/ACCESS.2019.2900345.
Pilz LK, Keller LK, Lenssen D, Roenneberg T. Time to rethink sleep quality: PSQI scores reflect sleep quality on workdays. Sleep. 2018;41(5):zsy029. https://doi.org/10.1093/sleep/zsy029.
Manzar MD, BaHammam AS, Hameed UA, Spence DW, Pandi-Perumal SR, Moscovitch A, Streiner DL. Dimensionality of the Pittsburgh Sleep Quality Index: a systematic review. Health Qual Life Outcomes. 2018;16(1):89. https://doi.org/10.1186/s12955-018-0915-x.
Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379(9821):1129–41. https://doi.org/10.1016/S0140-6736(11)60750-2.
Simonelli G, Marshall NS, Grillakis A, Miller CB, Hoyos CM, Glozier N. Sleep health epidemiology in low and middle-income countries: a systematic review and meta-analysis of the prevalence of poor sleep quality and sleep duration. Sleep Health. 2018;4(3):239–50. https://doi.org/10.1016/j.sleh.2018.03.001.
Gardani M, Bradford DRR, Russell K, Allan S, Beattie L, Ellis JG, Akram U. A systematic review and meta-analysis of poor sleep, insomnia symptoms and stress in undergraduate students. Sleep Med Rev. 2022;61:101565. https://doi.org/10.1016/j.smrv.2021.101565.
Parry DA, Oeppen RS, Amin MSA, Brennan PA. Sleep: its importance and the effects of deprivation on surgeons and other healthcare professionals. Br J Oral Maxillofac Surg. 2018;56(8):663–6. https://doi.org/10.1016/j.bjoms.2018.08.001.
Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, Turin TC. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med. 2015;11(1):69–74. https://doi.org/10.5664/jcsm.4370.
Li L, Wang Y, Wang S, Zhang L, Li L, Xu D, Ng CH, Ungvari GS, Cui X, Liu Z. Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res. 2018;27(3):e12648. https://doi.org/10.1111/jsr.12648.
Mishra T, Mohapatra D, Behera M, Mishra S. Association between short sleep duration and obesity in medical students. Asian J Pharm Clin Res. 2017;10(1):242–4. https://doi.org/10.22159/ajpcr.2017.v10i1.15067.
Alimoradi Z, Gozal D, Tsang HWH, Lin CY, Broström A, Ohayon MM, Pakpour AH. Gender-specific estimates of sleep problems during the COVID-19 pandemic: Systematic review and meta-analysis. J Sleep Res. 2022;31(1):e13432. https://doi.org/10.1111/jsr.13432.
Alimoradi Z, Broström A, Tsang HWH, Griffiths MD, Haghayegh S, Ohayon MM, Lin C-Y, Pakpour AH: Sleep problems during COVID-19 pandemic and its’ association to psychological distress: A systematic review and meta-analysis. EClinicalMedicine 2021, 36:100916. https://doi.org/10.1016/j.eclinm.2021.100916.
Wang F, Bíró É. Determinants of sleep quality in college students: A literature review. EXPLORE. 2021;17(2):170–7. https://doi.org/10.1016/j.explore.2020.11.003.
Lemma S, Gelaye B, Berhane Y, Worku A, Williams MA. Sleep quality and its psychological correlates among university students in Ethiopia: a cross-sectional study. BMC Psychiatry. 2012;12(1):237. https://doi.org/10.1186/1471-244X-12-237.
Peltzer K, Pengpid S. Nocturnal sleep problems among university students from 26 countries. Sleep Breath. 2015;19(2):499–508. https://doi.org/10.1007/s11325-014-1036-3.
Cheng SH, Shih C-C, Lee IH, Hou Y-W, Chen KC, Chen K-T, Yang YK, Yang YC. A study on the sleep quality of incoming university students. Psychiatry Res. 2012;197(3):270–4. https://doi.org/10.1016/j.psychres.2011.08.011.
Rao W-W, Li W, Qi H, Hong L, Chen C, Li C-Y, Ng CH, Ungvari GS, Xiang Y-T. Sleep quality in medical students: a comprehensive meta-analysis of observational studies. Sleep Breath. 2020;24(3):1151–65. https://doi.org/10.1007/s11325-020-02020-5.
Jahrami H, Dewald-Kaufmann J. Faris MeA-I, AlAnsari AMS, Taha M, AlAnsari N: Prevalence of sleep problems among medical students: a systematic review and meta-analysis. J Public Health. 2020;28(5):605–22. https://doi.org/10.1007/s10389-019-01064-6.
Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4.
Yi H, Shin K, Shin C. Development of the Sleep Quality Scale. J Sleep Res. 2006;15(3):309–16. https://doi.org/10.1111/j.1365-2869.2006.00544.x.
Urponen H, Partinen M, Vuori I, Hasan J: Sleep Quality and Health: Description of the Sleep Quality Index. In: Sleep and Health Risk. edn. Edited by Peter JH, Penzel T, Podszus T, von Wichert P. Berlin, Heidelberg: Springer Berlin Heidelberg; 1991: 555–558 https://doi.org/10.1007/978-3-642-76034-1_63.
Ohayon MM, Paskow M, Roach A, Filer C, Hillygus DS, Chen MC, Langer G, Hirshkowitz M. The National Sleep Foundation’s Sleep Satisfaction Tool. Sleep Health. 2019;5(1):5–11. https://doi.org/10.1016/j.sleh.2018.10.003.
Gandhi KD, Mansukhani MP, Silber MH, Kolla BP. Excessive Daytime Sleepiness: A Clinical Review. Mayo Clin Proc. 2021;96(5):1288–301. https://doi.org/10.1016/j.mayocp.2020.08.033.
Kato T. Development of the sleep quality questionnaire in healthy adults. J Health Psychol. 2014;19(8):977–86. https://doi.org/10.1177/1359105313482168.
Meng R, Kato T, Mastrotheodoros S, Dong L, Fong DYT, Wang F, Cao M, Liu X, Yao C, Cao J, et al. Adaptation and validation of the Chinese version of the Sleep Quality Questionnaire. Qual Life Res. 2023;32(2):569–82. https://doi.org/10.1007/s11136-022-03241-9.
Meng R, Lau EYY, Spruyt K, Miller CB, Dong L. Assessing Measurement Properties of a Simplified Chinese Version of Sleep Condition Indicator (SCI-SC) in Community Residents. Behav Sci. 2022;12(11):433. https://doi.org/10.3390/bs12110433.
Luo Y, Fei S, Gong B, Sun T, Meng R. Understanding the Mediating Role of Anxiety and Depression on the Relationship Between Perceived Stress and Sleep Quality Among Health Care Workers in the COVID-19 Response. Nat Sci Sleep. 2021;13:1747–58. https://doi.org/10.2147/NSS.S313258.
Mokkink LB, De Vet HC, Prinsen CA, Patrick DL, Alonso J, Bouter LM, Terwee CB. COSMIN risk of bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1171–9. https://doi.org/10.1007/s11136-017-1765-4.
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HCW. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737–45. https://doi.org/10.1016/j.jclinepi.2010.02.006.
Deyo RA, Diehr P, Patrick DL. Reproducibility and responsiveness of health status measures statistics and strategies for evaluation. Control Clin Trials. 1991;12(4, Supplement):S142–S158. https://doi.org/10.1016/S0197-2456(05)80019-4.
World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA. 2013;310(20):2191–4. https://doi.org/10.1001/jama.2013.281053.
Households’ Income and Consumption Expenditure in 2019. https://data.stats.gov.cn/easyquery.htm?cn=C01. Accessed 7 July 2021.
Spitzer RL, Kroenke K, Williams JB. Group PHQPCS, Group PHQPCS: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282(18):1737–44. https://doi.org/10.1001/jama.282.18.1737.
Patient Health Questionnaire (PHQ) Screeners. https://www.phqscreeners.com/. Accessed 29 Aug 2019.
Kroenke K, Spitzer RL, Williams JBW, Löwe B. An Ultra-Brief Screening Scale for Anxiety and Depression: The PHQ–4. Psychosomatics. 2009;50(6):613–21. https://doi.org/10.1016/S0033-3182(09)70864-3.
Stanhope J. Patient Health Questionnaire-4. Occup Med. 2016;66(9):760–1. https://doi.org/10.1093/occmed/kqw165.
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, Schneider A, Brähler E. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1–2):86–95. https://doi.org/10.1016/j.jad.2009.06.019.
Zhu Y, Jiang C, Yang Y, Dzierzewski JM, Spruyt K, Zhang B, Huang M, Ge H, Rong Y, Ola BA, et al. Depression and Anxiety Mediate the Association between Sleep Quality and Self-Rated Health in Healthcare Students. Behav Sci. 2023;13(2):82. https://doi.org/10.3390/bs13020082.
Rosseel Y. lavaan: An R Package for Structural Equation Modeling. J Stat Softw. 2012;48(2):1–36. https://doi.org/10.18637/jss.v048.i02.
Meade AW, Johnson EC, Braddy PW. Power and sensitivity of alternative fit indices in tests of measurement invariance. J Appl Psychol. 2008;93(3):568–92. https://doi.org/10.1037/0021-9010.93.3.568.
irr: Various Coefcients of Interrater Reliability and Agreement. R package version 0.84.1. https://CRAN.R-project.org/package=irr.
Svetina D, Rutkowski L, Rutkowski D. Multiple-Group Invariance with Categorical Outcomes Using Updated Guidelines: An Illustration Using M plus and the lavaan/semTools Packages. Struct Equ Modeling. 2019;27:1–20. https://doi.org/10.1080/10705511.2019.1602776.
Li C-H. Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods. 2016;48(3):936–49. https://doi.org/10.3758/s13428-015-0619-7.
Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis: Pearson new international edition. 7th ed. London: Pearson Higher Education; 2014.
McDonald RP. Ho M-HR: Principles and practice in reporting structural equation analyses. Psychol Methods. 2002;7(1):64–82. https://doi.org/10.1037/1082-989x.7.1.64.
Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res. 2003;8(2):23–74.
Edwards MC, Houts CR, Wirth RJ. Measurement invariance, the lack thereof, and modeling change. Qual Life Res. 2018;27(7):1735–43. https://doi.org/10.1007/s11136-017-1673-7.
Meredith W. Measurement invariance, factor analysis and factorial invariance. Psychometrika. 1993;58(4):525–43. https://doi.org/10.1007/BF02294825.
Millsap RE: Statistical approaches to measurement invariance. New York: Routledge; 2011 https://doi.org/10.4324/9780203821961.
Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Modeling. 2007;14(3):464–504. https://doi.org/10.1080/10705510701301834.
Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126(5):1763–8. https://doi.org/10.1213/ANE.0000000000002864.
Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, Terwee CB. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–57. https://doi.org/10.1007/s11136-018-1798-3.
Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15(2):155–63. https://doi.org/10.1016/j.jcm.2016.02.012.
Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Conditioning Res. 2005;19(1):231–40.
Uyanık GK, Güler N. A study on multiple linear regression analysis. Procedia Soc Behav Sci. 2013;106:234–40. https://doi.org/10.1016/j.sbspro.2013.12.027.
Sun Y, Wang H, Jin T, Qiu F, Wang X. Prevalence of Sleep Problems Among Chinese Medical Students: A Systematic Review and Meta-Analysis. Front Psychiatry. 2022;13:753419. https://doi.org/10.3389/fpsyt.2022.753419.
Ghrouz AK, Noohu MM, Dilshad Manzar M, Warren Spence D, BaHammam AS, Pandi-Perumal SR. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. 2019;23(2):627–34. https://doi.org/10.1007/s11325-019-01780-z.
Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiat Res. 2020;288:112954. https://doi.org/10.1016/j.psychres.2020.112954.
Zailinawati AH, Teng CL, Chung YC, Teow TL, Lee PN, Jagmohni KS. Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia. 2009;64(2):108–10.
Crutzen R, Peters G-J. Scale quality: alpha is an inadequate estimate and factor-analytic evidence is needed first of all. Health Psychol Rev. 2015;11:1–14. https://doi.org/10.1080/17437199.2015.1124240.
Dunn TJ, Baguley T, Brunsden V. From alpha to omega: A practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. 2014;105(3):399–412. https://doi.org/10.1111/bjop.12046.
Viladrich C, Angulo-Brunet A, Doval E. A journey around alpha and omega to estimate internal consistency reliability. Ann Psychol. 2017;33(3):755–82. https://doi.org/10.6018/analesps.33.3.268401.
Polit DF. Getting serious about test–retest reliability: a critique of retest research and some recommendations. Qual Life Res. 2014;23(6):1713–20. https://doi.org/10.1007/s11136-014-0632-9.
Rodrigues RND, Viegas CAA. Abreu e Silva AAA, Tavares P: Daytime sleepiness and academic performance in medical students. Arq Neuropsiquiatr. 2002;60:6–11. https://doi.org/10.1590/s0004-282x2002000100002.
Pengpid S, Peltzer K. Anxiety-induced sleep disturbances among in-school adolescents in the United Arab Emirates: Prevalence and associated factors. Asian J Health Soc Behav. 2022;5(1):18–23. https://doi.org/10.4103/shb.shb_120_21.
Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med Rev. 2021;60:101556. https://doi.org/10.1016/j.smrv.2021.101556.
Ramar K, Malhotra RK, Carden KA, Martin JL, Abbasi-Feinberg F, Aurora RN, Kapur VK, Olson EJ, Rosen CL, Rowley JA, et al. Sleep is essential to health: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2021;17(10):2115–9. https://doi.org/10.5664/jcsm.9476.
Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, Espie CA, Garcia-Borreguero D, Gjerstad M, Gonçalves M, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700. https://doi.org/10.1111/jsr.12594.
Espie CA, Emsley R, Kyle SD, Gordon C, Drake CL, Siriwardena AN, Cape J, Ong JC, Sheaves B, Foster R, et al. Effect of Digital Cognitive Behavioral Therapy for Insomnia on Health, Psychological Well-being, and Sleep-Related Quality of Life: A Randomized Clinical Trial. JAMA Psychiat. 2019;76(1):21–30. https://doi.org/10.1001/jamapsychiatry.2018.2745.
Alimoradi Z, Jafari E, Broström A, Ohayon MM, Lin CY, Griffiths MD, Blom K, Jernelöv S, Kaldo V, Pakpour AH. Effects of cognitive behavioral therapy for insomnia (CBT-I) on quality of life: A systematic review and meta-analysis. Sleep Med Rev. 2022;64:101646. https://doi.org/10.1016/j.smrv.2022.101646.
Snyder E, Cai B, DeMuro C, Morrison MF, Ball W. A New Single-Item Sleep Quality Scale: Results of Psychometric Evaluation in Patients With Chronic Primary Insomnia and Depression. J Clin Sleep Med. 2018;14(11):1849–57. https://doi.org/10.5664/jcsm.7478.
Luik AI, Machado PF, Siriwardena N, Espie CA. Screening for insomnia in primary care: using a two-item version of the Sleep Condition Indicator. Br J Gen Pract. 2019;69(679):79–80. https://doi.org/10.3399/bjgp19X701045.
Espie CA, Kyle SD, Hames P, Gardani M, Fleming L, Cape J: The Sleep Condition Indicator: a clinical screening tool to evaluate insomnia disorder. BMJ Open 2014, 4(3):e004183. https://doi.org/10.1136/bmjopen-2013-004183.
Sancho-Domingo C, Carballo JL, Coloma-Carmona A, Buysse DJ. Brief version of the Pittsburgh Sleep Quality Index (B-PSQI) and measurement invariance across gender and age in a population-based sample. Psychol Assess. 2021;33(2):111–21. https://doi.org/10.1037/pas0000959.
Meng R, Dong L, Dzierzewski JM, Mastrotheodoros S, Cao M, Yu B, Wang J, Gong B, Li J, Spruyt K. The RU_SATED as a measure of sleep health: cross-cultural adaptation and validation in Chinese healthcare students. BMC Psychology. 2023;11(1):200. https://doi.org/10.1186/s40359-023-01203-5.
Rapkin BD, Schwartz CE. Toward a theoretical model of quality-of-life appraisal: Implications of findings from studies of response shift. Health Qual Life Outcomes. 2004;2:14. https://doi.org/10.1186/1477-7525-2-14.
Acknowledgements
The authors would like to thank the research assistants and the study respondents. The authors are grateful to two editors and three peer reviewers for their precious opinions and suggestions.
Funding
This study was supported by the Medical Research Fund of Zhejiang Province, Grant No. 2023RC073 and the Research Initiation Fund of Hangzhou Normal University, Grant No. RWSK20201003.
Author information
Authors and Affiliations
Contributions
Mengyi Huang: Formal Analysis, Software, Validation, Visualization, Writing—Original Draft, Writing—Review & Editing. Haiyan Ma: Project Administration, Resources, Supervision, Validation. Karen Spruyt: Validation, Writing—Review & Editing. Joseph M. Dzierzewski: Validation, Writing—Review & Editing. Chen Jiang: Software, Validation, Writing—Review & Editing. Jiaxuan He: Writing—Review & Editing. Nongnong Yang: Validation. Yiwei Ying: Validation. Bolanle Adeyemi Ola: Writing—Review & Editing. Runtang Meng: Conceptualization, Data Curation, Funding Acquisition, Investigation, Methodology, Project Administration, Resources, Software, Supervision, Validation, Writing—Review & Editing. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study has been reviewed and approved by the Institutional Review Board of Hangzhou Normal University Division of Health Sciences, China (Reference No. 20190076), thus ensuring that it adhered to the standards set by the Helsinki Declaration. All healthcare students freely consented to answer the questionnaires and provided their informed consent prior to their inclusion into this longitudinal survey. The authors confirmed full respect and protection of individual privacy rights before, during and after the data collection and processing.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Score distribution for each item and factor of the SQQ, PHQ-4, and SRHQ (N = 595). Table S2. Cross-sectional measurement invariances of the SQQ (N = 595). Table S3. Spearman correlation of the SQQ with the PHQ and SRHQ across two assessments (N = 595).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, M., Ma, H., Spruyt, K. et al. Assessing psychometric properties and measurement invariance of the Sleep Quality Questionnaire among healthcare students. BMC Psychol 12, 41 (2024). https://doi.org/10.1186/s40359-023-01276-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40359-023-01276-2