Abstract
Background
The Sleep Condition Indicator (SCI), an insomnia measurement tool based on the updated Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria with sound psychometric properties when applied in various populations, was evaluated here among healthcare students longitudinally, to demonstrate its measurement properties and invariance in this particularly high-risk population.
Methods
Healthcare students of a Chinese university were recruited into this two-wave longitudinal study, completing the simplified Chinese version of the SCI (SCI-SC), Chinese Regularity, Satisfaction, Alertness, Timing, Efficiency, Duration (RU_SATED-C) scale, Chinese Patient Health Questionnaire-4 (PHQ-4-C), and sociodemographic variables questionnaire (Q-SV) between September and November 2022. Structural validity, measurement invariance (MI), convergent and discriminant validity, internal consistency, and test–retest reliability of the SCI-SC were examined. Subgroups of gender, age, home location, part-time job, physical exercise, and stress-coping strategy were surveyed twice to test cross-sectional and longitudinal MI.
Results
We identified 343 valid responses (62.9% female, mean age = 19.650 ± 1.414 years) with a time interval of seven days. The two-factor structure was considered satisfactory (comparative fit index = 0.953–0.989, Tucker–Lewis index = 0.931–0.984, root means square error of approximation = 0.040–0.092, standardized root mean square residual = 0.039–0.054), which mostly endorsed strict invariance except for part-time job subgroups, hence establishing longitudinal invariance. The SCI-SC presented acceptable convergent validity with the RU_SATED-C scale (r ≥ 0.500), discriminant validity with the PHQ-4-C (0.300 ≤ r < 0.500), internal consistency (Cronbach’s alpha = 0.811–0.835, McDonald’s omega = 0.805–0.832), and test–retest reliability (intraclass correlation coefficient = 0.829).
Conclusion
The SCI-SC is an appropriate screening instrument available for assessing insomnia symptoms among healthcare students, and the promising measurement properties provide additional evidence about validity and reliability for detecting insomnia in healthcare students.
Similar content being viewed by others
Background
Insomnia disorder is defined as a persistent difficulty with sleep initiation, duration, or consolidation that occurs despite adequate opportunities and circumstances for sleep and results in concern, dissatisfaction, or perceived daytime impairment, such as fatigue, decreased mood or irritability, general malaise, or cognitive impairment [1]. To date, insomnia is globally considered one of the most prevalent sleep disorders and costly public health problems [2]. As estimated, up to 10% of the general population met the diagnostic criteria for insomnia, while up to 30% experienced some symptoms of insomnia [3]. Given its pervasiveness, the detrimental effects of insomnia have been increasingly documented. Several studies identified insomnia as a significant risk factor for depression and anxiety and even documented association with suicidality [4,5,6]. A meta-analysis showed that insomniacs have a severely impaired quality of life, greatly affecting their ability to function well at work, in their health, and in their social lives [7]. However, independently assessing insomnia is rarely straightforward, often involving multiple interacting psychiatric and medical comorbidities [8]. Given its high prevalence and harmful effects, an effective diagnosis of insomnia should be considered a key step in promoting optimal sleep health.
Insomnia can only be assessed via subjective measures, and objective measures may be useful for uncovering further sleep disorders. Historically, three primary sources of information have been utilized in diagnosing insomnia: (i) sleep history, including quantitative and qualitative sleep information, and perspectives of patients about waking function; (ii) typical two-week sleep diary, as a collection of nightly sleep estimates; (iii) polysomnography, which provides objective sleep assessments and may detect the presence of further sleep disorders [9]. Epidemiologic studies have indicated that in population where dissatisfaction with sleep is prevalent, clinical diagnoses of sleep disorders are often synchronized [10]. Thus, subjective patient reports offer precise diagnostic information given symptom-based definitions [9]. In addition, objective measuring is a time-consuming and costly process [11]. To work around this, there is a greater need for a reliable, valid, and brief screening instrument to provide further empirical support for insomnia evaluation.
A plethora of subjective measurements exist for the identification of insomnia [12,13,14,15,16], some examples are the Pittsburgh Sleep Quality Index (PSQI) and Insomnia Severity Index (ISI), both of which are of different natures and purposes. Nevertheless, the PSQI assesses general sleep quality in the general population [17], while the ISI measures insomnia symptoms not according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), hence without including the aspect of duration [18]. There is currently a lack of scale developed specifically on the updated DSM-5 criteria. The Sleep Condition Indicator (SCI) is a versatile, user-friendly, and brief instrument developed on the updated DSM-5 criteria [19]. It is designed for subjective self-reporting of insomnia and monitors a dimensional perspective on sleep quality, a visual profile of night-time and daytime symptoms, and indicative cut-off points for clinically significant insomnia [19].
Since the release of the English version in 2012, the SCI has been adapted and validated in over 12 languages, including Romanian (2013) [20], English (2014) [19], Italian (2015) [21], traditional Chinese (2017) [11], French (2017) [22], Korean (2018) [23], Swedish (2019) [24], Persian (2019) [25], Arabic (2021) [26], simplified Chinese (2022) [27], Indonesian (2023) [28], and Turkish (2024) [29]. However, there has yet to be validation of longitudinal measurement invariance (LMI) in all existing versions, nor has there been any evaluation in healthcare students. A previous study reported some key measurement properties of the simplified Chinese version of the SCI (SCI-SC) through COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN), containing promising structural validity, construct (convergent and divergent) validity, internal consistency, and the most key―cross-sectional measurement invariance (MI) [27]. Nonetheless, longitudinal evidence for the SCI-SC has not been provided, and establishing construct validity with the Chinese Sleep Quality Questionnaire (SQQ-C) solo is insufficient [11].
Healthcare students exhibit particularly serious insomnia symptoms [30], including daytime somnolence, sleep deprivation, and poor sleep quality compared to non-medical students and the general population [27, 31,32,33]. Alarmingly, the prevalence of insomnia continues to increase among Chinese healthcare students [34], resulting in reduced learning capacity, declarative and procedural learning, and neurocognitive functioning [35]. Excessive academic stress often worsens daytime impact on healthcare students, resulting in absence, tardiness, falling asleep during class and interference with academic achievement [36]. While these symptoms appear to be consistent with the Sleep Pattern Subscale (SPS) and Daytime Impact Subscale (DIS) of the SCI, it would be important to look into the psychometric properties empirically because Swedish undergraduate students have reported contradictory findings of unidimensionality in structural validity [24].
Three overarching goals of this study are to: (i) fill the gap in the validation of measurement properties of the SCI in healthcare students; (ii) provide psychometrics evidence of the SCI-SC, including structural validity, cross-sectional and longitudinal MI, internal consistency and test–retest reliability; (iii) explore criterion validity with the correlation between the SCI-SC and two external variables.
Methods
Sample and procedure
Participant recruitment took place from September to November 2022 at a university in Hangzhou, China. The study included conveniently sampled freshman, junior, and senior undergraduate students majoring in clinical medicine and preventive medicine. We used the rule of thumb of 20 subjects per item [37], along with a minimum of 300 respondents to conduct the factor analysis [38]. The inclusion criteria were healthcare students who were capable of reading simplified Chinese and communicating in Mandarin. Exclusion criteria were those who: (i) had difficulty with study process; (ii) were on long-term medical internship leave or suspension; (iii) were taking medication for sleep disorders, had psychiatric diagnoses, or had substance abuse.
This study was performed under an interval of approximately seven days, due to recommended longitudinal use of 2 to 14 days [39,40,41]; the below three measures and sociodemographic variables questionnaire (Q-SV) were administered at baseline (Time 1, T1) and follow-up (Time 2, T2) assessment [19, 42,43,44]. Well-trained investigators maintained quality control of the data collection process. Respondents filled out self-administered paper-and-pencil surveys, with their student IDs for matching questionnaires at two assessments.
This study followed the ethical standards in accordance with the Declaration of Helsinki [45].
Measures
Sociodemographic variables questionnaire
The Q-SV gathered sociodemographic characteristics including gender (male and female), age, major (clinical medicine and preventive medicine), home location (urban, rural, and suburban), part-time job (yes and no), physical exercise (yes and no), stress-coping strategy [the most customary way of coping when faced with great stress (emotion-focused, solution-focused, and avoidance coping) [46]].
Sleep Condition Indicator (Chinese version)
The SCI is a five-point Likert scale (0–4), comprising two subscales of five items probing Sleep Pattern (SP) and three items exploring Daytime Impact (DI) [19]. Scores lie in the point range from 0 to 32, with a higher score reflecting better sleep and a lower likelihood of insomnia. An SCI score of 16 or lower may define insomnia disorder and indicate four main DSM-5 criteria are met: difficulty initiating or maintaining sleep, significant distress, frequency of sleep disturbances, and duration of sleep disturbances [26]. The SCI-SC is a reliable measure with promising psychometric properties in community residents [27].
Regularity, Satisfaction, Alertness, Timing, Efficiency, Duration scale (Chinese version)
The Regularity, Satisfaction, Alertness, Timing, Efficiency, Duration (RU_SATED) scale, a six-item/dimension scale consisting of sleep Regularity, Satisfaction with sleep, Alertness during waking hours, Timing of sleep, sleep Efficiency, and sleep Duration, is a generic instrument measuring sleep health and emphasizing positive effects of sleep on overall health [43, 47]. Respondents expressed their level of agreement or disagreement with each item using a five-point Likert scale (0 = never, 1 = rarely, 2 = sometimes, 3 = usually, 4 = always), summed up ranging from 0 to 24, where a higher score indicates better sleep health. Previous results supported satisfactory measurement properties of the Chinese RU_SATED (RU_SATED-C) scale [48].
Patient Health Questionnaire-4 (Chinese version)
The Patient Health Questionnaire (PHQ), a self-report version of the Primary Care Evaluation of Mental Disorders (PRIME-MD), was developed to assist primary care clinicians in making efficient psychiatric diagnoses [49]. As a form with fewer items, the Patient Health Questionnaire-4 (PHQ-4) consists of the Patient Health Questionnaire-2 (PHQ-2) about the diagnosis of depressive disorders and the Generalized Anxiety Disorder scale-2 (GAD-2) about two core criteria for anxiety symptoms [44]. Scored on a four-point Likert scale (0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day), composite scores range from 0 to 12, with higher scores indicating worse anxiety and depression symptoms [44]. Assessed directly from the PHQ Screeners website [50], the Chinese Patient Health Questionnaire-4 (PHQ-4-C) had shown adequate measurement properties in Chinese adults [51].
Statistical approach
We applied EpiData (version 3.1) to build the database. Statistical analyses were conducted using R software (version 4.1.3) with several packages (“lavvan (0.6–11)” [52], “MBESS (4.9.1)” [53], “irr (0.84.1)” [54], “semTools (0.5–6)” [55]) and JASP software (version 0.16.1). Measurement properties were assessed compliant with COSMIN methodology [56]. The missing values were imputed with the mean (continuous variables) or median (categorical variables) when produced < 1% of total missing values [57].
Structural validity
The primary role of exploratory factor analysis (EFA) is to explore and identify factors that define the construct, while confirmatory factor analysis (CFA) follows EFA and theoretical knowledge to examine factor structure further [58]. In previous studies, both traditional and simplified Chinese versions showed stable and identical solutions with two dimensions (SP and DI) [11, 27], supporting in conducting CFA rather than EFA.
CFA was applied on the one-factor (obtained in the Swedish version [24]), two-factor (suggested in the traditional and simplified Chinese versions [11, 27]), and second-order factor models. We used the Maximum Likelihood Robust Estimator (MLR) method that is appropriate for ordinal data to separately determine which of the three proposed models could achieve the best goodness of fit [59]. The recommended two-indicator strategy was used to select indices [60]: (i) the chi-square (χ2) and P value; since to be sensitive in a large sample, they only were treated as secondary indicators; (ii) comparative fit index (CFI), Tucker–Lewis index (TLI), root means square error of approximation (RMSEA), and standardized root mean square residual (SRMR); threshold values of CFI and TLI ≥ 0.900, RMSEA ≤ 0.100, SRMR ≤ 0.080 were indicative of model employment [61,62,63].
Measurement invariance
MI requires that the structure of scale should not depend on measurement groups, equally reflecting constructs of interest under different groups of individuals [64]. Compared the SCI scores across subgroups based on sociodemographic variables that are closely associated with insomnia in general population (i.e., gender, age, and home location [65,66,67]) or in healthcare students (i.e., part-time job, physical exercise, and stress-coping strategy [68,69,70,71,72,73,74,75,76,77]). LMI was examined using longitudinal CFA (LCFA) across two occasions.
Cumulatively adding constraints, we tested configural, metric, scalar, and strict invariance, which correspondingly require the same factor structure, factor loadings, item intercepts, and item residual between subgroups [78]. The unstandardized regression coefficients, and regression coefficients and means of latent structures are comparable when metric and scalar invariance are confirmed, respectively [79]. Relied on the conventional recognized standards, changes in CFI (ΔCFI) ≤ 0.010, changes in TLI (ΔTLI) ≤ 0.010, changes in RMSEA (ΔRMSEA) ≤ 0.015, and changes in SRMR (ΔSRMR) ≤ 0.030 were considered acceptable model [80]. We have also considered changes in chi-square (Δχ2), but only as a secondary indicator [81]. For all models, if at least two out of three fit indices comply with the cut-off criteria, it indicates no significant degradation in model, suggesting that MI is held [82].
Convergent and discriminant validity
Evidence of convergent and discriminant validity based on Spearman correlation coefficient was provided by correlating the SCI-SC scores with RU_SATED-C scale and PHQ-4-C scores, respectively. Following the COSMIN guideline, at least 75% of the hypothesis need to be within range [83]. We hypothesized:
-
(i)
The SCI-SC scores would have a strong correlation (|r|≥ 0.500) with the RU_SATED-C scale scores, given that both instruments measure related constructs concerning sleep [58, 84].
-
(ii)
The SCI-SC scores would have a moderate correlation (0.300 ≤ |r| < 0.500) with the PHQ-4-C scores, given that two instruments measure theoretically different constructs [58, 84].
Internal consistency and test–retest reliability
Internal consistency means the degree of interrelatedness between items [84]. We assessed internal consistency of the SCI-SC scores and two sub-scores using Cronbach’s alpha and McDonald’s omega [81]. Cronbach’s alpha and McDonald’s omega values > 0.700 indicated adequacy [85].
To test stability of the SCI-SC for the same respondents in the same test at different times [58], we studied test–retest reliability using intraclass correlation coefficient (ICC); in doing so, generally, ICC > 0.700 was sufficient [86]. Standard error of measurement (SEM) was evaluated as a supplement to measurement precision [86].
Results
Sample description
A total of 343 healthcare students were analyzed, with a total missing data rate of 0.066% and a dropout rate of less than 5%; 62.974% were female, and the mean age was 19.650 ± 1.414 (mean ± standard deviation) years. The average time interval between two occasions was 7 days + 2 h. Except for item 2, scores of seven items on the SCI-SC contented a multivariate normal distribution by checking skewness and kurtosis [87]. Additional sociodemographic characteristics can be found in Table 1, and the distribution of scores is presented in Supplementary 1: Table S1.
Structural validity
The fit indices indicated a better fit of both baseline and follow-up data to the two-factor structure (SP and DI) (CFI and TLI ≥ 0.900, RMSEA ≤ 0.100, SRMR ≤ 0.080), as presented in Table 2. Although RMSEAs approaching the critical value in the follow-up sample were cautionary, they were still within a reasonable range.
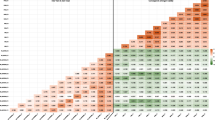
Measurement invariance
Cross-sectional measurement invariance
An evaluation of cross-sectional measurement invariance on two-factor model, the best-fitting model within three alternative SCI-SC models, was tested. Results showed evidence for well-fixed configural, metric, scalar, and strict invariance across gender, age, home location, physical exercise, and stress-coping strategy (CFI and TLI ≥ 0.900, RMSEA ≤ 0.100, SRMR ≤ 0.080; ΔCFI and ΔTLI ≤ 0.010, ΔRMSEA ≤ 0.015, ΔSRMR ≤ 0.030) (Table 3). Although cut-off values exceeded, scalar invariance in age subgroups was still supported due to negligible changes in fit indices for strict invariance. Compared with the baseline assessment, RMSEAs in the follow-up assessment were increased to different degrees and partly fell outside the recommended range, but we still accepted such results due to at least two out of three fit indices comply with the cut-off criteria [82]. However, significant changes in CFI and TLI values were observed across part-time job subgroups for strict invariance (baseline: ΔCFI = -0.015, ΔTLI = -0.011; follow-up: ΔCFI = -0.039, ΔTLI = -0.030), the highest supporting scalar invariance. Complete MI results are shown in Supplementary 1: Table S2 and Supplementary 2 reports a more detailed description.
Longitudinal measurement invariance
With regards to LCFA, results showed that all fit indices fitted the range, and all models were acceptable (CFI and TLI ≥ 0.900, RMSEA ≤ 0.100, SRMR ≤ 0.080; ΔCFI and ΔTLI ≤ 0.010, ΔRMSEA ≤ 0.015, ΔSRMR ≤ 0.030) (Table 4).
Convergent and discriminant validity
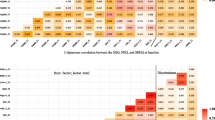
Results of the correlation analysis are reported in Fig. 1. The left side of the black line represents inter–factor and factor–total correlations, whereas the right side of the black line represents convergent and discriminant validity. The inter–factor and factor–total correlations ranged from 0.463 to 0.917, representing moderate to high correlations.
-
(i)
A strong correlation was shown between scores on the SCI-SC and RU_SATED-C scale (|r|≥ 0.500) that fell within the hypothesized range, supporting for satisfactory convergent validity.
-
(ii)
A moderate correlation was shown between scores on the SCI-SC and PHQ-4-C (0.300 ≤ |r| < 0.500) that fell within the hypothesized range, supporting for satisfactory discriminant validity.
Inter–factor and factor–total, convergent and discriminant validity between the SCI-SC, RU_SATED-C scale and PHQ-4-C (N = 343)
Notes: The color gradient indicates the correlation strength. Red indicates positive correlation and purple indicates negative correlation
Abbreviations: SCI Sleep Condition Indicator, SC simplified Chinese, SF Short Form, DIS Daytime Impact Subscale, SPS Sleep Pattern Subscale, RU_SATED Regularity, Satisfaction, Alertness, Timing, Efficiency, Duration, PHQ‑4 Patient Health Questionnaire‑4, GAD‑2 Generalized Anxiety Disorder‑2, PHQ‑2 Patient Health Questionnaire‑2, T1 Time 1, T2 Time 2
Internal consistency and test–retest reliability
Table 5 shows internal consistency results of the SCI-SC and its subscales. For two time points, both values indicated excellent internal consistency (Cronbach’s alpha and McDonald’s omega > 0.700). Supplementary 1: Table S3 displays the reliability results of other two measures.
Meanwhile, ICC values spanned two-time points higher than 0.700, and SEM values ranged from 1.178 to 2.656, indicating excellent test–retest reliability (Table 5).
Discussion
This study provided a novel perspective on the measurement properties of the SCI-SC in a sample of healthcare students that has a comparable distribution of gender and age to general Chinese healthcare students [88]. As far as we are aware, it is the first to provide LMI evidence of the SCI. The findings demonstrated an appropriate two-factor model, multi-group and longitudinal MI, reasonable convergent and discriminant validity, good internal consistency, and adequate test–retest reliability in healthcare students. In general, the SCI-SC is a reliable screening tool for appraising insomnia symptoms among healthcare students.
Structural validity
CFA results within Chinese healthcare students demonstrated the most excellent fit indices in the two-factor model, replicating finding from the simplified Chinese version among community residents [27]. The finding is consistent with most languages: the original English [19], traditional Chinese [11], French [22], Persian [25], Indonesian [28] and Turkish [29]. However, it is worth noting that the Swedish version produced unidimensionality outcome among university students [24], attributed to the classical test theory (CTT) being sample- and culture-dependent [89]. Therefore, further assessment of factor structure of the SCI-SC in different samples is called for to further strengthen its applicability across cultures and samples.
Measurement invariance
When testing groups with diverse backgrounds, evaluating MI is the prerequisite for meaningful comparisons across subgroups [90]. The four invariance models, configural, metric, scalar, and strict invariance, respectively, assume equality of factor structure, factor loadings, item intercepts, and item residual across groups and two time points [78]. Strict invariance was supported across gender, age, home location, physical exercise, and stress-coping strategy, suggesting that the SCI-SC was a reliable instrument to measure insomnia among different demographic characteristics in healthcare students. More specially, given confirming configural, metric, and scalar invariance, the current study findings supported reference comparisons of the measured structure, unstandardized regression coefficients, and regression coefficients and means of the latent structures of the SCI-SC in healthcare students [79]. While some researchers have questioned the impracticality of any MI level above scalar invariance [79], strict invariance is necessary to test for differences in factor structure or latent means [80]. Strict invariance was not reached between subgroups of part-time job. It is in line with some comparable literature; for instance, a study among nursing students revealed that students who have part-time jobs were at risk for sleep disorders [91]. The study determined sufficient LMI that the SCI-SC could capably measure a certain construct similarly across time. Naturally, as the study is the first to test LMI of the SCI, further studies on LCFA are desirable.
Convergent and discriminant validity
A strong correlation was observed between the SCI-SC and RU_SATED-C scale, supporting our hypothesis that the SCI-SC had adequate convergent validity among healthcare students. The RU-SATED-C scale assesses global sleep health and contains components such as satisfaction with sleep and sleep efficiency that are closely related to insomnia, and as such, the high correlation evidence between these two scales may be attributed to their shared focus on the same aspect of sleep. Furthermore, regarding discriminant validity, a moderate correlation was found between the SCI-SC evaluating insomnia and the PHQ-4-C assessing anxiety and depression, providing sufficient evidence to support capability of the SCI-SC to differentiate between theoretically different structures [58, 92]. Additionally, the finding aligns with other surveys on the correlation of insomnia with anxiety and depression [93,94,95,96]. An international longitudinal study has revealed that post-pandemic insomnia symptoms produced the highest level of anxiety and depression [97]. As more insomnia symptoms may lead to increased mental health issues, it is important to accurately assess insomnia among healthcare students.
In the insomnia research field, the PSQI and ISI are widely used due to their good psychometric properties and easy of use [47]. However, the PSQI was designed to evaluate general sleep disturbances, not specifically for insomnia [17, 98]. The ISI was developed not based on the updated DSM-5 and lacks an assessment of duration [18, 99]. The SCI is based on the updated DSM-5 insomnia criteria, following the latest developments in the understanding of the psychopathology of insomnia and incorporating published research diagnostic criteria and recommended quantitative parameters for sleep disturbance [19]. Strong relationships between the SCI and commonly-used scales have been validated in various languages: English [19], Italian [21], traditional Chinese [11], French [22], Swedish [24], and Indonesian [28]. In contrast, there is a gap in the testing of the SCI-SC against commonly-used scales, underscoring the imperative for future research to evaluate its relationship with scales like the PSQI and ISI.
Internal consistency and test–retest reliability
The study illustrated the strong inter–factor and factor–total correlations, excellent internal consistency, and stable test–retest reliability of the SCI-SC among healthcare students. This effectiveness as a screening tool for insomnia symptoms was consistent with a previous report among Chinese community residents [19, 27]. Due to criticism of Cronbach’s alpha from some scholars [100], this study also used McDonald’s omega to corroborate internal consistency. Our findings suggested high inter-item relatedness and have evidence to support the high degree of interrelatedness among items [83]. Our ICC and SEM analyses supported robustness of test-retest reliability.
Strengths and limitations
Some strengths are worth mentioning. First, we did not merely validate reliability and validity of the SCI-SC but also explore detailed MI across multiple groups. Second, this study conducted repeated measurements over two time points, rare in studies of the SCI. Last, this study is valuable for application among healthcare students and an addition to LMI of the SCI.
Some limitations deserve comment. Although adequate convergent and discriminant validity have been reported by establishing the correlation of the SCI-SC with the RU_SATED-C scale and dissociation from the PHQ-4-C, there was a lack of comparison with commonly-used scales, e.g., the PSQI and ISI. Moreover, convenience sampling method in only healthcare students and a single university site may all lead to a reduction in generalizability and selection bias, narrowing the extensiveness of conclusions.
Future directions
Results supported the two-factor solution was preferred model, with high item interrelatedness and temporal stability, as well as satisfactory convergent and discriminant validity. Meaningful comparisons can be performed across groups (gender, age, home location, physical exercise, and stress-coping strategy) and over time among healthcare students, but comparisons need to be made with caution with varying part-time job situations. The SCI-SC, as an easy-to-use instrument for early screening of insomnia, could aid in clinical settings to monitor sleep among healthcare students of heightened risks. Accurately measuring insomnia using suitable tools is essential to save resources as well as early diagnosis and treatment of insomnia in healthcare students.
Subsequent studies should be appropriately considered in three ways while assessing or applying the SCI-SC: (i) an exploration with objective measures of sleep such as polysomnography, actigraphy, and smart mattresses; (ii) a validation of the SCI-SC with a more general population; (iii) a future exploration with multi-approaches, for instance, item response theory (IRT) and network analysis.
Conclusion
This study demonstrated promising measurement properties of the SCI-SC in healthcare students as the first assessment of LMI and test–retest reliability. Through adaptation and validation, a wealth of valid and reliable evidence was found for use of the SCI-SC in screening insomnia symptoms. The SCI-SC, with good psychometric properties, is instrumental in establishing DSM-5-based insomnia diagnosis and treatment in healthcare students.
Availability of data and materials
The datasets analyzed during the current study are not publicly available due to the personal health information of participants needing to be protected but are available (de-identified data) from the corresponding author on reasonable request.
Abbreviations
- CFA:
-
confirmatory factor analysis
- CFI:
-
comparative fit index
- COSMIN:
-
COnsensus-based Standards for the selection of health Measurement INstruments
- DI:
-
Daytime Impact
- DIS:
-
Daytime Impact Subscale
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- GAD-2:
-
Generalized Anxiety Disorder-2
- ICC:
-
intraclass correlation coefficient
- LCFA:
-
longitudinal confirmatory factor analysis
- LMI:
-
longitudinal measurement invariance
- MI:
-
measurement invariance
- PHQ-2:
-
Patient Health Questionnaire-2
- PHQ-4:
-
Patient Health Questionnaire-4
- Q-SV:
-
sociodemographic variables questionnaire
- RU_SATED:
-
Regularity, Satisfaction, Alertness, Timing, Efficiency, Duration
- RMSEA:
-
root means square error of approximation
- SCI:
-
Sleep Condition Indicator
- SP:
-
Sleep Pattern
- SPS:
-
Sleep Pattern Subscale
- SRMR:
-
standardized root mean square residual
- TLI:
-
Tucker–Lewis index
References
Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–94. https://doi.org/10.1378/chest.14-0970.
Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379(9821):1129–41. https://doi.org/10.1016/s0140-6736(11)60750-2.
Rosenberg RP. Prevalence, impact, and burden of insomnia and discussing it with patients. J Clin Psychiatry. 2021;82(2):ei20008br1c. https://doi.org/10.4088/JCP.EI20008BR1C.
Bernert RA, Joiner TE Jr, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28(9):1135–41. https://doi.org/10.1093/sleep/28.9.1135.
Kapoor A, Perlis ML, Bastien C, Williams N, Hale L, Branas C, Barrett M, Killgore WD, Wills CC, Grandner MA. Associations between insomnia and anxiety symptoms: which elements of insomnia are associated with which elements of anxiety? Sleep. 2020;43(Supplement_1):A411–2. https://doi.org/10.1093/sleep/zsaa056.1103.
Perlis ML, Giles DE, Buysse DJ, Tu X, Kupfer DJ. Self-reported sleep disturbance as a prodromal symptom in recurrent depression. J Affect Disord. 1997;42(2–3):209–12. https://doi.org/10.1016/s0165-0327(96)01411-5.
Ishak WW, Bagot K, Thomas S, Magakian N, Bedwani D, Larson D, Brownstein A, Zaky C. Quality of life in patients suffering from insomnia. Innov Clin Neurosci. 2012;9(10):13–26.
Molnar F, Frank C, Chun S, Lee EK. Insomnia in older adults: approaching a clinical challenge systematically. Can Fam Physician. 2021;67(1):25–6. https://doi.org/10.46747/cfp.670125.
Roth T, Drake C. Defining insomnia: the role of quantitative criteria. Sleep. 2006;29(4):424–5. https://doi.org/10.1093/sleep/29.4.424.
McCrae CS, Rowe MA, Tierney CG, Dautovich ND, Definis AL, McNamara JPH. Sleep complaints, subjective and objective sleep patterns, health, psychological adjustment, and daytime functioning in community-dwelling older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60(4):182–9. https://doi.org/10.1093/geronb/60.4.P182.
Wong ML, Lau KNT, Espie CA, Luik AI, Kyle SD, Lau EYY. Psychometric properties of the Sleep Condition Indicator and Insomnia Severity Index in the evaluation of insomnia disorder. Sleep Med. 2017;33:76–81. https://doi.org/10.1016/j.sleep.2016.05.019.
Meng R, Kato T, Mastrotheodoros S, Dong L, Fong DYT, Wang F, Cao M, Liu X, Yao C, Cao J, et al. Adaptation and validation of the Chinese version of the Sleep Quality Questionnaire. Qual Life Res. 2023;32(2):569–82. https://doi.org/10.1007/s11136-022-03241-9.
Zhu Y, Jiang C, Yang Y, Dzierzewski JM, Spruyt K, Zhang B, Huang M, Ge H, Rong Y, Ola BA, et al. Depression and anxiety mediate the association between sleep quality and self-rated health in healthcare students. Behav Sci. 2023;13(2):82. https://doi.org/10.3390/bs13020082.
Zhu Y, Meng R, Jiang C, Yang N, Huang M, Wang X, Zou W, Lou C, Xiao R, Lu J, et al. Sleep quality and subjective well-being in healthcare students: examining the role of anxiety and depression. Front Public Health. 2023;11:1281571. https://doi.org/10.3389/fpubh.2023.1281571.
Huang M, Ma H, Spruyt K, Dzierzewski JM, Jiang C, He J, Yang N, Ying Y, Ola BA, Meng R. Assessing psychometric properties and measurement invariance of the Sleep Quality Questionnaire among healthcare students. BMC Psychol. 2023;12(1):41. https://doi.org/10.1186/s40359-023-01276-2.
Yang N, Ma H, Huang M, Lau EYY, Fong DYT, Wang M, Wang P, Xu S, Xu J, Jiang C, et al. Measurement properties and optimal cutoff point of the WHO-5 among Chinese healthcare students. Psychol Res Behav Manag. 2023;16:5141–58. https://doi.org/10.2147/prbm.S437219.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4.
Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. https://doi.org/10.1016/s1389-9457(00)00065-4.
Espie CA, Kyle SD, Hames P, Gardani M, Fleming L, Cape J. The Sleep Condition Indicator: a clinical screening tool to evaluate insomnia disorder. BMJ Open. 2014;4(3):e004183. https://doi.org/10.1136/bmjopen-2013-004183.
Voinescu BI, Szentágotai A. Categorical and dimensional assessment of insomnia in the general population. J Cogn Behav Psychother. 2013;13(1a):197–209.
Palagini L, Ragno G, Caccavale L, Gronchi A, Terzaghi M, Mauri M, Kyle S, Espie CA, Manni R. Italian validation of the Sleep Condition Indicator: a clinical screening tool to evaluate insomnia disorder according to DSM-5 criteria. Int J Psychophysiol. 2015;98(3 Pt 1):435–40. https://doi.org/10.1016/j.ijpsycho.2015.08.008.
Bayard S, Lebrun C, Maudarbocus KH, Schellaert V, Joffre A, Ferrante E, Le Louedec M, Cournoulat A, Gely-Nargeot M-C, Luik AI. Validation of a French version of the Sleep Condition Indicator: a clinical screening tool for insomnia disorder according to DSM-5 criteria. J Sleep Res. 2017;26(6):702–8. https://doi.org/10.1111/jsr.12556.
Gim W, Kim M. Development of a meditation application as an assistance tool for meditation-based interventions. J Korean Contents Assoc. 2018;18(9):441–53. https://doi.org/10.5392/JKCA.2018.18.09.441.
Hellström A, Hagell P, Broström A, Ulander M, Luik AI, Espie CA, Årestedt K. A classical test theory evaluation of the Sleep Condition Indicator accounting for the ordinal nature of item response data. PLoS ONE. 2019;14(3):e0213533. https://doi.org/10.1371/journal.pone.0213533.
Ranjkesh F, Nasiri M, Sharif Nia SH, Goudarzian AH, Hosseinigolafshani SZ. Validation of the Persian version of the Sleep Condition Indicator in pregnant women. Iran J Epidemiol. 2019;14(4):366–74.
Khaled SM, Petcu C, Al-Thani MA, Al-Hamadi AMHA, Daher-Nashif S, Zolezzi M, Woodruff P. Prevalence and associated factors of DSM-5 insomnia disorder in the general population of Qatar. BMC Psychiatry. 2021;21(1):84. https://doi.org/10.1186/s12888-020-03035-8.
Meng R, Lau EYY, Spruyt K, Miller CB, Dong L. Assessing measurement properties of a simplified Chinese version of Sleep Condition Indicator (SCI-SC) in community residents. Behav Sci. 2022;12(11):433. https://doi.org/10.3390/bs12110433.
Hasan F, Vidyanti AN, Tsai PS, Wu D, Lee HC, Yuliana LT, Romadlon DS, Marta OFD, Chiu HY. Psychometric properties of Indonesian version of Sleep Condition Indicator for screening poststroke insomnia. Sleep Breath. 2023;27(5):2013–20. https://doi.org/10.1007/s11325-023-02797-1.
Uygur H, Ahmed O, Uygur OF, Miller CB, Hursitoglu O, Bahar A, Demiroz D, Drake CL. Validity and reliability of the Turkish version of the Sleep Condition Indicator: a clinical screening instrument based on the DSM-5 criteria for insomnia. Nat Sci Sleep. 2024;16:63–74. https://doi.org/10.2147/nss.S433656.
Medeiros ALD, Mendes DBF, Lima PF, Araujo JF. The relationships between sleep-wake cycle and academic performance in medical students. Biol Rhythm Res. 2001;32(2):263–70. https://doi.org/10.1076/brhm.32.2.263.1359.
Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, Turin TC. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med. 2015;11(1):69–74. https://doi.org/10.5664/jcsm.4370.
Li L, Wang YY, Wang SB, Zhang L, Li L, Xu DD, Ng CH, Ungvari GS, Cui X, Liu ZM, et al. Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res. 2018;27(3):e12648. https://doi.org/10.1111/jsr.12648.
Perotta B, Arantes-Costa FM, Enns SC, Figueiro-Filho EA, Paro H, Santos IS, Lorenzi-Filho G, Martins MA, Tempski PZ. Sleepiness, sleep deprivation, quality of life, mental symptoms and perception of academic environment in medical students. BMC Med Educ. 2021;21(1):111. https://doi.org/10.1186/s12909-021-02544-8.
Zhang M, Qin L, Zhang D, Tao M, Han K, Chi C, Zhang Z, Tao X, Liu H. Prevalence and factors associated with insomnia among medical students in China during the COVID-19 pandemic: characterization and associated factors. BMC Psychiatry. 2023;23(1):140. https://doi.org/10.1186/s12888-023-04556-8.
Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10(5):323–37. https://doi.org/10.1016/j.smrv.2005.11.001.
Kayaba M, Matsushita T, Enomoto M, Kanai C, Katayama N, Inoue Y, Sasai-Sakuma T. Impact of sleep problems on daytime function in school life: a cross-sectional study involving Japanese university students. BMC Public Health. 2020;20(1):371. https://doi.org/10.1186/s12889-020-08483-1.
Anthoine E, Moret L, Regnault A, Sébille V, Hardouin J-B. Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. Health Qual Life Outcomes. 2014;12:176. https://doi.org/10.1186/s12955-014-0176-2.
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. 2018;6:149. https://doi.org/10.3389/fpubh.2018.00149.
Deyo RA, Diehr P, Patrick DL. Reproducibility and responsiveness of health status measures statistics and strategies for evaluation. Control Clin Trials. 1991;12(4 Suppl):142S–58S. https://doi.org/10.1016/s0197-2456(05)80019-4.
McKechnie D, Fisher MJ. Considerations when examining the psychometric properties of measurement instruments used in health. Aust J Adv Nurs. 2022;39(2):36–47. https://doi.org/10.37464/2020.392.481.
Streiner DL, Norman GR, Cairney J. Health Measurement Scales: a practical guide to their development and use. New York: Oxford University Press; 2014.
Toledano-Toledano F, Rodríguez-Rey R, Moral de La Rubia J, Luna D. A sociodemographic variables questionnaire (Q-SV) for research on family caregivers of children with chronic disease. BMC Psychol. 2019;7(1):85. https://doi.org/10.1186/s40359-019-0350-8.
Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17. https://doi.org/10.5665/sleep.3298.
Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–21. https://doi.org/10.1176/appi.psy.50.6.613.
World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. https://doi.org/10.1001/jama.2013.281053.
Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–83. https://doi.org/10.1037//0022-3514.56.2.267.
Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29(9):1155–73. https://doi.org/10.1093/sleep/29.9.1155.
Meng R, Dong L, Dzierzewski JM, Mastrotheodoros S, Cao M, Yu B, Wang J, Gong B, Li J, Spruyt K. The RU_SATED as a measure of sleep health: cross-cultural adaptation and validation in Chinese healthcare students. BMC Psychol. 2023;11(1):200. https://doi.org/10.1186/s40359-023-01203-5.
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–44. https://doi.org/10.1001/jama.282.18.1737.
Patient Health Queastionnaire (PHQ) Screeners. https://www.phqscreeners.com. Assessed 29 Aug 2019.
Fong TCT, Ho RTH, Yip PSF. Psychometric properties of the Patient Health Questionnaire-4 among Hong Kong young adults in 2021: associations with meaning in life and suicidal ideation. Front Psychiatry. 2023;14:1138755. https://doi.org/10.3389/fpsyt.2023.1138755.
Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48(2):1–36. https://doi.org/10.18637/jss.v048.i02.
Meade AW, Johnson EC, Braddy PW. Power and sensitivity of alternative fit indices in tests of measurement invariance. J Appl Psychol. 2008;93(3):568–92. https://doi.org/10.1037/0021-9010.93.3.568.
Irr: various coefficients of interrater reliability and agreement. https://CRAN.R-project.org/package=irr. Accessed 30 Jan 2023.
Svetina D, Rutkowski L, Rutkowski D. Multiple-group invariance with categorical outcomes using updated guidelines: an illustration using Mplus and the lavaan/semTools packages. Struct Equ Modeling. 2020;27(1):111–30. https://doi.org/10.1080/10705511.2019.1602776.
Mokkink LB, de Vet HCW, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, Terwee CB. COSMIN Risk of Bias checklist for systematic reviews of Patient-Reported Outcome Measures. Qual Life Res. 2018;27(5):1171–9. https://doi.org/10.1007/s11136-017-1765-4.
Bennett DA. How can I deal with missing data in my study? Aust N Z J Public Health. 2001;25(5):464–9.
DeVon HA, Block ME, Moyle-Wright P, Ernst DM, Hayden SJ, Lazzara DJ, Savoy SM, Kostas-Polston E. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007;39(2):155–64. https://doi.org/10.1111/j.1547-5069.2007.00161.x.
Li C-H. Confirmatory factor analysis with ordinal data: comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods. 2016;48(3):936–49. https://doi.org/10.3758/s13428-015-0619-7.
Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. https://doi.org/10.1080/10705519909540118.
Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociol Methods Res. 1992;21(2):230–58. https://doi.org/10.1177/0049124192021002005.
Steiger JH. Structual model evaluation and modification - an interval estimation approach. Multivariate Behav Res. 1990;25(2):173–80. https://doi.org/10.1207/s15327906mbr2502_4.
Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis: Pearson new international edition. 7th ed. London: Pearson Higher Education; 2014.
Finch H. Measurement invariance. In: Michalos AC, editor. Encyclopedia of quality of life and well-being research. Dordrecht: Springer Netherlands; 2014. p. 3909–12.
Theorell-Haglöw J, Miller CB, Bartlett DJ, Yee BJ, Openshaw HD, Grunstein RR. Gender differences in obstructive sleep apnoea, insomnia and restless legs syndrome in adults - What do we know? A clinical update. Sleep Med Rev. 2018;38:28–38. https://doi.org/10.1016/j.smrv.2017.03.003.
Brewster GS, Riegel B, Gehrman PR. Insomnia in the older adult. Sleep Med Clin. 2022;17(2):233–9. https://doi.org/10.1016/j.jsmc.2022.03.004.
Billings ME, Hale L, Johnson DA. Physical and social environment relationship with sleep health and disorders. Chest. 2020;157(5):1304–12. https://doi.org/10.1016/j.chest.2019.12.002.
Friedrich A, Schlarb AA. Let’s talk about sleep: a systematic review of psychological interventions to improve sleep in college students. J Sleep Res. 2018;27(1):4–22. https://doi.org/10.1111/jsr.12568.
Kim BS, Jeon HJ, Hong JP, Bae JN, Lee JY, Chang SM, Lee YM, Son J, Cho MJ. DSM-IV psychiatric comorbidity according to symptoms of insomnia: a nationwide sample of Korean adults. Soc Psychiatry Psychiatr Epidemiol. 2012;47(12):2019–33. https://doi.org/10.1007/s00127-012-0502-0.
Li D, Li X. Independent and combined associations between physical activity and sedentary time with sleep quality among Chinese college students. Int J Environ Res Public Health. 2022;19(11):6697. https://doi.org/10.3390/ijerph19116697.
Moreno Reyes P, Muñoz Gutiérrez C, Pizarro Mena R, Jiménez Torres S. Effects of physical exercise on sleep quality, insomnia, and daytime sleepiness in the elderly. A literature review. Rev Esp Geriatr Gerontol. 2020;55(1):42–9. https://doi.org/10.1016/j.regg.2019.07.003.
Rubio-Arias JÁ, Marín-Cascales E, Ramos-Campo DJ, Hernandez AV, Pérez-López FR. Effect of exercise on sleep quality and insomnia in middle-aged women: a systematic review and meta-analysis of randomized controlled trials. Maturitas. 2017;100:49–56. https://doi.org/10.1016/j.maturitas.2017.04.003.
Pengpid S, Peltzer K, Kassean HK, Tsala Tsala JP, Sychareun V, Müller-Riemenschneider F. Physical inactivity and associated factors among university students in 23 low-, middle- and high-income countries. Int J Public Health. 2015;60(5):539–49. https://doi.org/10.1007/s00038-015-0680-0.
Gardani M, Bradford DRR, Russell K, Allan S, Beattie L, Ellis JG, Akram U. A systematic review and meta-analysis of poor sleep, insomnia symptoms and stress in undergraduate students. Sleep Med Rev. 2022;61:101565. https://doi.org/10.1016/j.smrv.2021.101565.
Hamadi HY, Zakari NMA, Jibreel E, Al Nami FN, Smida JAS, Ben Haddad HH. Stress and coping strategies among nursing students in clinical practice during COVID-19. Nurs Rep. 2021;11(3):629–39. https://doi.org/10.3390/nursrep11030060.
Liu X, Ping S, Gao W. Changes in undergraduate students’ psychological well-being as they experience university life. Int J Environ Res Public Health. 2019;16(16):2864. https://doi.org/10.3390/ijerph16162864.
Morgan IG, Wu PC, Ostrin LA, Tideman JWL, Yam JC, Lan W, Baraas RC, He X, Sankaridurg P, Saw SM, et al. IMI risk factors for myopia. Invest Ophthalmol Vis Sci. 2021;62(5):3. https://doi.org/10.1167/iovs.62.5.3.
Millsap RE. Statistical approaches to measurement invariance. New York: Routledge; 2012.
Wells CS. Assessing measurement invariance for applied research. Cambridge: Cambridge University Press; 2021.
Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90. https://doi.org/10.1016/j.dr.2016.06.004.
Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Modeling. 2007;14(3):464–504. https://doi.org/10.1080/10705510701301834.
Nelemans SA, Meeus WHJ, Branje SJT, Van Leeuwen K, Colpin H, Verschueren K, Goossens L. Social Anxiety Scale for Adolescents (SAS-A) short form: longitudinal measurement invariance in two community samples of youth. Assessment. 2019;26(2):235–48. https://doi.org/10.1177/1073191116685808.
Prinsen CAC, Vohra S, Rose MR, Boers M, Tugwell P, Clarke M, Williamson PR, Terwee CB. How to select outcome measurement instruments for outcomes included in a “Core Outcome Set” - a practical guideline. Trials. 2016;17(1):449. https://doi.org/10.1186/s13063-016-1555-2.
Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, Terwee CB. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–57. https://doi.org/10.1007/s11136-018-1798-3.
Crutzen R, Peters GY. Scale quality: alpha is an inadequate estimate and factor-analytic evidence is needed first of all. Health Psychol Rev. 2017;11(3):242–7. https://doi.org/10.1080/17437199.2015.1124240.
Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–40. https://doi.org/10.1519/15184.1.
Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol Methods. 1996;1(1):16–29. https://doi.org/10.1037/1082-989X.1.1.16.
Wu D, Rockett IRH, Yang T, Feng X, Jiang S, Yu L. Deliberate self-harm among Chinese medical students: a population-based study. J Affect Disord. 2016;202:137–44. https://doi.org/10.1016/j.jad.2016.05.030.
Lewis V. Health measurement scales: a practical guide to their development and use, 5th edition. Aust N Z J Public Health. 2016;40(3):294–5. https://doi.org/10.1111/1753-6405.12484.
Han K, Colarelli SM, Weed NC. Methodological and statistical advances in the consideration of cultural diversity in assessment: a critical review of group classification and measurement invariance testing. Psychol Assess. 2019;31(12):1481–96. https://doi.org/10.1037/pas0000731.
Manyeneng LG, Pilusa ML, Mogotlane MS. Health and safety risks affecting part-time nursing students. Health SA. 2021;26:1404. https://doi.org/10.4102/hsag.v26i0.1404.
Bard HA, O’Driscoll C, Miller CB, Henry AL, Cape J, Espie CA. Insomnia, depression, and anxiety symptoms interact and individually impact functioning: a network and relative importance analysis in the context of insomnia. Sleep Med. 2023;101:505–14. https://doi.org/10.1016/j.sleep.2022.12.005.
Jiang C, Ma H, Luo Y, Fong DYT, Umucu E, Zheng H, Zhang Q, Liu X, Liu X, Spruyt K, et al. Validation of the Chinese version of the Perceived Stress Scale-10 integrating exploratory graph analysis and confirmatory factor analysis. Gen Hosp Psychiatry. 2023;84:194–202. https://doi.org/10.1016/j.genhosppsych.2023.07.008.
Jiang C, Mastrotheodoros S, Zhu Y, Yang Y, Hallit S, Zhao B, Fan Y, Huang M, Chen C, Ma H, et al. The Chinese version of the Perceived Stress Questionnaire-13: psychometric properties and measurement invariance for medical students. Psychol Res Behav Manag. 2023;16:71–83. https://doi.org/10.2147/prbm.S385510.
Jiang C, Zhu Y, Luo Y, Tan C-S, Mastrotheodoros S, Costa P, Chen L, Guo L, Ma H, Meng R. Validation of the Chinese version of the Rosenberg Self-Esteem Scale: evidence from a three-wave longitudinal study. BMC Psychol. 2023;11(1):345. https://doi.org/10.1186/s40359-023-01293-1.
Guo WP, Min Q, Gu WW, Yu L, Xiao X, Yi WB, Li HL, Huang B, Li JL, Dai YJ, et al. Prevalence of mental health problems in frontline healthcare workers after the first outbreak of COVID-19 in China: a cross-sectional study. Health Qual Life Outcomes. 2021;19(1):103. https://doi.org/10.1186/s12955-021-01743-7.
Meaklim H, Junge MF, Varma P, Finck WA, Jackson ML. Pre-existing and post-pandemic insomnia symptoms are associated with high levels of stress, anxiety, and depression globally during the COVID-19 pandemic. J Clin Sleep Med. 2021;17(10):2085–97. https://doi.org/10.5664/jcsm.9354.
Morin CM. Insomnia: psychological assessment and management. New York: Guilford; 1993.
Edinger JD, Bonnet MH, Bootzin RR, Doghramji K, Dorsey CM, Espie CA, Jamieson AO, McCall WV, Morin CM, Stepanski EJ. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27(8):1567–96. https://doi.org/10.1093/sleep/27.8.1567.
Viladrich C, Angulo-Brunet A, Doval E. A journey around alpha and omega to estimate internal consistency reliability. An Psicol. 2017;33(3):755–82. https://doi.org/10.6018/analesps.33.3.268401.
Acknowledgements
The authors thank the study respondents and research assistants for their time. The authors appreciate the handling editor and three reviewers for their constructive insights and ideas.
Funding
This study was supported by the Medical Research Fund of Zhejiang Province, Grant No. 2023RC073, the Research Initiation Fund of Hangzhou Normal University, Grant No. RWSK20201003, and the National Undergraduate Training Program for Innovation and Entrepreneurship, Grant No. 202410346040.
Author information
Authors and Affiliations
Contributions
RM: Conceptualization, Data Curation, Funding Acquisition, Investigation, Methodology, Project Administration, Resources, Software, Supervision, Validation, Writing - Original Draft, Writing - Review & Editing. YY: Validation, Writing - Original Draft, Writing - Review & Editing. YL, CBM, KS, and EYYL: Methodology, Validation, Writing - Review & Editing. MH: Formal Analysis, Validation, Visualization, Writing - Review & Editing. YX, YJ, LF, WC, JY, NY, JX, CJ, and LL: Validation, Writing - Review & Editing. HM: Resources, Validation, Writing - Review & Editing. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Institutional Review Board of the School of Public Health, Hangzhou Normal University, China (Reference No. 20210014), and adhered to the ethical standards in accordance with the Declaration of Helsinki. All healthcare students freely consented to answer the questionnaires and offered their informed consent before the survey. This study was conducted with full respect and protection of privacy.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Meng, R., Ying, Y., Luo, Y. et al. A longitudinal examination of the measurement properties and invariance of the Sleep Condition Indicator in Chinese healthcare students. BMC Psychiatry 24, 518 (2024). https://doi.org/10.1186/s12888-024-05844-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05844-7