Abstract
Background
Food intake augments CO2 production; however, minute ventilation is not augmented during exercise after food intake. Respiratory chemoreceptors respond to CO2 and influence respiration. We examined the effect of food intake on respiratory chemosensitivity to CO2 in young adults.
Methods
The hypercapnic ventilatory response was measured in eleven healthy individuals before and after food intake. To evaluate the respiratory chemoreflex response to CO2, minute ventilation was plotted against end-tidal PCO2 using data obtained with the rebreathing method.
Results
Sublingual temperature, CO2 output, minute ventilation, and end-tidal PCO2 were all significantly higher at baseline in the session after food intake than in the session before food intake. On the other hand, there was no significant difference in chemosensitivity to CO2 between the sessions before and after food intake (1.60 ± 0.62 vs. 1.53 ± 0.62 l min−1 mmHg−1).
Conclusions
Food intake does not influence respiratory chemosensitivity to CO2 in young adults, which is different from infants. This suggests that control of respiration differs between young adults and infants and that the elevated minute ventilation after food intake in young adults is not caused by a change in respiratory chemosensitivity.
Similar content being viewed by others
Background
It is well known that food intake influences several physiological parameters. For example, food intake increases metabolism and body temperature [1,2,3]. This is the so-called postprandial thermogenesis or thermic effect of food. We recently reported that food intake also influences the respiratory response at rest [1]—i.e., food intake increases minute ventilation (VE) in resting young individuals. In that study, we speculated that this elevation in VE was caused by an elevation in the H+ ion concentration related to increases in CO2 output (VCO2) and the plasma noradrenaline concentration [4], which can be induced by an increase in sympathetic nervous system activity [5]. Young adults in that study exercised at 50% of peak oxygen uptake 90 min after food intake, and the increase in metabolism elicited by the food intake was still present during the subsequent exercise. Interestingly, we found that although VCO2 and end-tidal PCO2 (PETCO2) were increased by food intake during exercise, VE was not [1]. On the other hand, when we previously compared the ventilatory responses during exercise with participants breathing CO2-enriched air or room air, we found that breathing CO2-enriched air elevated PCO2 and VE [6]. We have thus obtained differing results regarding the impact of CO2 on VE.
It has also been reported that respiratory chemosensitivity is subject to alteration by several factors. For example, it was reported that exercise (at 19%, 26%, and 34% of maximal oxygen uptake) increased respiratory chemosensitivity to CO2 relative to the resting state [7] and that a rise in body temperature of > 0.7 °C increased respiratory chemosensitivity to CO2 [8]. From these findings, it is plausible that respiratory chemosensitivity to CO2 is increased during exercise after food intake. However, our previous study [1] did not reveal higher VE during exercise after food intake. From that finding, we hypothesized that VE remains steady as a result of redundant compensatory mechanisms [1, 9]. On the other hand, Durand et al. [10] tested the effect of feeding on respiratory responses in the newborn infant and reported that feeding suppresses respiratory chemosensitivity to CO2. It is therefore possible that food intake suppresses respiratory chemosensitivity to CO2 in infants, though it remains unclear whether food intake changes respiratory chemosensitivity in adults. To address this issue, we compared respiratory chemosensitivity to CO2 measured before and after food intake in young adults.
Material and methods
Participants
Eleven healthy participants [four males and seven females, mean age = 21 ± 2 (SD) year; height = 169.0 ± 7.4 cm; weight = 59.7 ± 8.5 kg] participated in the study. None of the participants were smokers, and none were taking any medication. All of the female participants were studied within 10 days of menstruation, and none were taking oral contraceptives, which contain female hormones. The study was approved by the Research Ethics Committee of the University of Shizuoka and conformed to the provisions of the Declaration of Helsinki. Written informed consent was obtained from all participants.
Test meal
Test meals were designed for each participant. After estimating the basal metabolic rate for each subject using the equation of Ganpule et al. [11], we estimated the total energy expenditure by multiplying the estimated basal metabolic rate by the estimated average physical activity level [12]. For six of the participants, that factor was 1.75; for the remaining five, it was 2. The amounts of carbohydrate, protein, and fat in the meals were based on the Dietary Reference Intakes for the Japanese [13]. As a result, test meals contained 117.6 ± 17.4 g of carbohydrate, 30.9 ± 8.8 g of protein, and 20.2 ± 5.4 g of fat. The total energy content was 3332 ± 633 kJ.
Experimental design
The experiment was conducted in the morning, and the participants were all asked to abstain from strenuous exercise and not to consume any food or alcohol during the 12 h prior to the experiment. After each subject came to the laboratory, they voided urine, were weighed, and sat in a chair to rest for 30 min. During this period, a heart rate (HR) monitor (S810i, Polar, Finland) was attached. HR was recorded every 5 s during the experiment and was averaged over 30-s periods. Just before the measurements were begun, sublingual temperature (Tsl) data were collected via copper-constantan thermocouples, which were sampled every 1 s using a data logger system (WE7000, Yokogawa, Japan) and averaged over 30-s periods. A mass-flow sensor and a gas-sampling tube were then connected to the mask, after which respiratory chemosensitivity to CO2 was measured using a rebreathing method [14, 15]. Participants consumed test meals after the measurement. Tsl and respiratory chemosensitivity were then measured 90 min after eating using the same procedure. The experiments were carried out in an experimental laboratory maintained at 25 °C and 40–60% relative humidity.
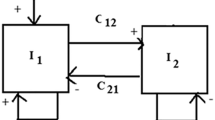
Rebreathing test
The participants wore a mask connected to a closed one-way circuit with a 6-l rubber bag containing the test gas (7% CO2, 43% O2, 50% N2). For the first 5 min with the stopcock open (“the one-way rebreathing circuit”), the participants breathed room air to measure control ventilation values. The stopcock was then closed, and rebreathing was begun. Rebreathing was terminated when the inspired CO2 fraction reached 9.2%. Rebreathing time ranged from 4 to 6 min in each participant. Respiratory parameters and gas concentrations were monitored breath-to-breath (AE-310S, Minato Medical Science, Japan). This test was performed twice with a 20-min recovery period between tests, and the mean values were evaluated for respiratory chemosensitivity, which was calculated as the slope of the regression line relating PETCO2 to VE. Because a ventilatory recruitment threshold was observed at around PETCO2 = 45 mmHg in several participants, regression analyses were conducted with data for PETCO2 > 50 mmHg. Previous studies showed that there is no significant difference in respiratory chemosensitivity to CO2 between steady-state and rebreathing methods when they are used under normal acid-base conditions [16, 17]. Therefore, the present results are comparable to results obtained using steady-state methods.
Statistical analysis
All values are reported as means ± SD. Paired t tests were used to compare the “before food intake” and “after food intake” sessions among the measured variables. Values of P < 0.05 were considered significant.
Results
Baseline Tsl, HR, oxygen uptake (VO2), VCO2, VE, respiratory frequency (fR), and PETCO2 were all significantly higher during the session after food intake (Table 1). The baseline respiratory exchange ratio, tidal volume (VT), and end-tidal PO2 did not significantly differ between sessions.
Figure 1 shows the respiratory chemosensitivity to CO2. There was no significant between-session difference in respiratory chemosensitivity to CO2 (1.60 ± 0.62 l min−1 mmHg−1 in the before food intake session vs. 1.53 ± 0.77 l min−1 mmHg−1 in the after food intake session, P = 0.59, effect size d = 0.13). However, six of the 11 participants showed higher chemosensitivity before food intake.
Conclusions
The present study showed that food intake leads to increases in Tsl, VO2, VCO2, VE, and PETCO2, which is consistent with earlier studies [1,2,3]. Moreover, the results suggest that the elevated VE is not caused by a change in respiratory chemosensitivity, and they support our earlier speculation that the elevation in VE is caused by increases in the H+ ion concentration and plasma noradrenaline concentration [1].
Our results showed that food intake did not influence respiratory chemosensitivity to CO2, which is in contrast to an earlier report [10]. It may be that this discrepancy reflects the difference in the type of food eaten by the participants. The infants who participated in the earlier study took in milk, while the young adults participating in the present study ate test meals containing rice, chicken, and other things. To test this idea, it will be necessary to examine the effect of different food types on respiration. Furthermore, food intake elicited an elevation in Tsl of only 0.3 °C in the present study. It is likely that no change in respiratory chemosensitivity can be explained by this small elevation in Tsl. Nonetheless, in infants, respiratory chemosensitivity to CO2 was changed by feeding, which suggests this change cannot be explained simply based on body temperature. To understand this discrepancy, it will be necessary to clarify the differences relating to respiration between young adults and infants.
González-Castillo et al. [18] compared the changes in gene expression that occur in the ventral respiratory column of the ventrolateral medulla, which is involved in determining respiratory rhythm and central chemoreception, between adult and neonatal rats. Their analysis confirmed the differential expression of 84 genes involved in the expression of neuronal ion (K+, Na+, and Ca2+) channels. Although it is not clear how these genes relate to respiratory chemosensitivity to CO2, it may be that the differences their expression relate to the different responses to CO2 in neonates and adults. Further study will be necessary to clarify the differences in respiratory control and to determine how respiratory chemosensitivity changes with aging.
In summary, our results suggest that food intake does not suppress respiratory chemosensitivity to CO2 in young adults, which is different from the situation in infants and suggests that respiratory chemosensitivity does not directly influence ventilatory responses after food intake. These observations do not support the hypothesis that blunted respiratory chemosensitivity to CO2 underlies the attenuation of the increase in VE during exercise after food intake. On the other hand, these results support the hypothesis that VE remains steady during exercise after food intake as a result of redundant mechanisms.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding authors on reasonable request.
Abbreviations
- f R :
-
Respiratory frequency
- HR:
-
Heart rate
- PETCO2 :
-
End-tidal PCO2
- T sl :
-
Sublingual temperature
- VCO2 :
-
CO2 output
- V E :
-
Minute ventilation
- VO2 :
-
Oxygen uptake
V T
Tidal volume
References
Hayashi K, Ito N, Ichikawa Y, Suzuki Y. Effect of food intake on the ventilatory response to increasing core temperature during exercise. Appl Physiol Nutr Metab. 2019;44(1):22–30.
Hill JO, DiGirolamo M, Heymsfield SB. Thermic effect of food after ingested versus tube delivered meals. Am J Physiol. 1985;248(3 Pt 1):E370–4.
Nielsen B. Does diet-induced thermogenesis change the preferred ambient temperature of humans? Eur J Appl Physiol Occup Physiol. 1987;56(4):474–8.
Heistad DD, Wheeler RC, Mark AL, Schmid PG, Abboud FM. Effects of adrenergic stimulation on ventilation in man. J Clin Invest. 1972;51(6):1469–75.
Berne C, Fagius J, Niklasson F. Sympathetic response to oral carbohydrate administration. J Clin Invest. 1989;84(5):1403–9.
Hayashi K, Honda Y, Miyakawa N, Fujii N, Ichinose M, Koga S, Kondo N, Nishiyasu T. Effect of CO2 on the ventilatory sensitivity to rising body temperature during exercise. J Appl Physiol. 2011;110(5):1334–41.
Weil JV, Byrne-Quinn E, Sodal IE, Kline JS, McCullough RE, Filley GF. Augmentation of chemosensitivity during mild exercise in normal man. J Appl Physiol. 1972;33(6):813–9.
Natalino MR, Zwillich CW, Weil JV. Effects of hyperthermia on hypoxic ventilatory response in normal man. J Lab Clin Med. 1977;89(3):564–72.
Ward SA. Ventilatory control. In: Control of Breathing During Exercise. San Rafael: Morgan & Claypool Life Sciences; 2014. p. 27–70.
Durand M, Leahy FN, Cates DB, Rigatto H, Chernick V. Effect of feeding on the chemical control of breathing in the newborn infant. Pediatr Res. 1981;15(12):1509–12.
Ganpule AA, Tanaka S, Ishikawa-Takata K, Tabata I. Interindividual variability in sleeping metabolic rate in Japanese subjects. Eur J Clin Nutr. 2007;61(11):1256–61.
Westerterp KR. Impacts of vigorous and non-vigorous activity on daily energy expenditure. Proc Nutr Soc. 2003;62(3):645–50.
Ministry of Health, Labour and Welfare. Dietary Reference Intakes for Japanese. 2014. http://www.mhlw.go.jp/stf/shingi/0000041824.html. Accessed 17 May 2019 [In Japanese]
Ogawa T, Hayashi K, Ichinose M, Nishiyasu T. Relationship between resting ventilatory chemosensitivity and maximal oxygen uptake in moderate hypobaric hypoxia. J Appl Physiol. 2007;103(4):1221–6.
Read DJ. A clinical method for assessing the ventilatory response to carbon dioxide. Australas Ann Med. 1967;16(1):20–32.
Clark TJ. The ventilatory response to CO2 in chronic airways obstruction measured by a rebreathing method. Clin Sci. 1968;34(3):559–68.
Linton RA, Poole-Wilson PA, Davies RJ, Cameron IR. A comparison of the ventilatory response to carbon dioxide by steady-state and rebreathing methods during metabolic acidosis and alkalosis. Clin Sci Mol Med. 1973;45(2):239–49.
González-Castillo C, Muñoz-Ortiz E, Guzmán-Brambila C, Rojas-Mayorquín AE, Beltran-Parrazal L, Ortuño-Sahagún D, Morgado-Valle C. Differential expression of ion channels in adults and neonatal rat ventral respiratory column. J Mol Neurosci. 2018;64(1):51–61.
Acknowledgements
We sincerely thank the volunteer subjects for participating in this study. We are also grateful to Y. Ichikawa (University of Shizuoka) for nutritional advice and providing test meals. We also greatly appreciate the help of Dr. William Goldman (English editing and critical comments).
Funding
This study was supported by a grant from the University of Shizuoka.
Author information
Authors and Affiliations
Contributions
KH and KS conceived and designed the research. KH, MS, and KS conducted experiments. KH and MS analyzed data. KH drafted the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee of the University of Shizuoka (#25–30). Written informed consent was obtained from all participants.
Consent for publication
All authors approved the final version of the manuscript and submission to the Journal of Physiological Anthropology.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hayashi, K., Suekuni, M. & Sugiyama, K. Effect of food intake on respiratory chemosensitivity to CO2 in young adults. J Physiol Anthropol 38, 8 (2019). https://doi.org/10.1186/s40101-019-0200-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40101-019-0200-7