Abstract
Porcine reproductive and respiratory syndrome (PRRS) is an important swine disease that affects many swine industries worldwide. The disease can cause reproductive failure and respiratory problems in a swine population. As vaccination is an important tool to control the spread of PRRS virus (PRRSV), we employ a mathematical model to investigate the transmission dynamics of PRRSV and the effects of immunity information, as well as vaccination control strategies. We also explore optimal vaccination coverage and vaccination rate to minimize the number of infected swines and vaccination efforts. Our results suggest that: (i) higher vaccination coverage and vaccination rate together with prior knowledge about immunity may help reduce the prevalence of PRRSV, and (ii) longer maximum vaccination efforts are required when swines stay longer in a population and it takes them longer time to recover from PRRS infections.
Similar content being viewed by others
1 Introduction
Porcine reproductive and respiratory syndrome (PRRS) is an important disease responsible for reproductive and respiratory disorders in a swine population. The disease is caused by porcine reproductive and respiratory syndrome virus (PRRSV) which belongs to the Arterivirus genus [1]. The virus was first recognized in the USA in 1987, but PRRSV currently becomes endemic in the global swine industry [2]. Clinical symptoms include severe reproductive failure, pneumonia, decreased performance such as growth rate and numbers of progeny, and increased mortality [3]. Infections may last for several days due to the properties of PRRSV that induces prolonged viremia. Transmission primarily occurs via close contact between swines but airborne transmission and transmission through semen are possible [4]. Typically, PRRSV may cause epidemic outbreaks in virus-free areas or outbreaks after the introduction of a new strain in endemic regions.
Vaccination is an important method used for controlling the spread of PRRSV. There are at least two types of PRRSV vaccine commercially available: modified-live virus vaccine (MLV) and killed virus vaccine [5, 6]. MLV vaccines generally provide full protection against PRRSV strains that are homologous to the vaccine virus but may only provide partial cross-protection against heterologous strains [5]. The vaccines have been shown to effectively reduce disease occurrence, severity, mortality and poor growth in swines [7, 8]. They are usually available in endemic regions while killed vaccines that are less efficacious are generally used in non-endemic areas. Improving immune response to PRRSV vaccines is currently an important challenge.
Mathematical modeling has been used as an important tool to help understand the dynamics of infectious diseases among farm animals. However, mathematical models for describing the spread of PRRSV are not numerous [9,10,11,12,13]. Evans et al. [9] developed a stochastic model of a farrow-finish heard and found that the persistence of PRRSV increases according to increased herd size, increased contact between different age groups, and increased reintroduction of infectious swines. Jeong et al. [10] formulated a stochastic model to investigate control strategies. Their results suggest repeated mass immunization with herd closure or gilt acclimatization over single mass immunization for disease control within a farm. Arruda et al. [12] constructed a discrete event agent-based stochastic model to study the occurrence of PRRS outbreaks in swine herds when vaccines are implemented. Their results highlighted the importance of maintaining internal biosecurity practices as control strategies may not prevent the infection from spreading among the swine population. Suksamran et al. [13] used a two-step parameter-driven Bayesian approach to model the spatio-temporal dynamics of PRRS and demonstrated the importance of pig trade in PRRS transmission in the US. To the best of our knowledge, none of preceding studies have addressed the effects of optimal vaccination strategies and immunity information. In this study, we first investigate the transmission dynamics of PRRSV among a swine population by using a mathematical model, and explore the effects of vaccination strategies when two types of vaccination are taken into account, vaccination at births and vaccination from a susceptible pool. Then, we additionally introduce discrete-time vaccination and immunity information to study how immunity information influences the presence of infected swines. Moreover, when vaccination is continuously time-dependent, we explore optimal vaccination strategies and the effects of lifespan and recovery time.
2 Model formulation
To study the transmission dynamics of PRRSV and effects of certain parameters on the prevalence, we introduce a mathematical model by dividing a swine population into three categories: susceptible \((S)\), infectious \((I)\), and recovered \((R)\). A flow diagram of the model is illustrated in Fig. 1.
A flow diagram for describing the transmission dynamics of PRRSV among the swine population. In the diagram, S, I, and R represent susceptible, infected, and recovered swines. PRRSV is transmitted at rate β; swines are recovered at rate γ. PRRSV may cause a reproductive failure so that only the proportion r of swines successfully reproduces. Generally, births occur at rate b and swines die at rate μ. Swines are vaccinated at births with the vaccination coverage q and vaccinated at rate u from a susceptible pool
In the model, the growth rate is assumed to be logistic with a carrying capacity K owing to limitation of resources and man power [14,15,16]. For simplicity of the model and swines as prolific breeders, animal replacement is not included here. In the growth term, b represents a natural birth rate of swines. Due to the possibility of reproductive failures from PRRSV infection in infected swines, we assume that normal births occur in susceptible and recovered swines while in the infected swines, only the proportion r of them can successfully give births. If \(r=0\), it means that reproductive failure completely occurs in infected swines. At the other extreme, if \(r=1\), it means that PRRSV infection does not affect the swine reproduction. In the model, the swine population dies at a rate μ.
Here, we assume that transmission of PRRSV mainly occurs via close contacts while airborne and other transmission modes are negligible. It is assumed that virus transmission occurs at a rate β and swines recover from an infection with PRRSV at a rate γ. Note that since only homologous strains are considered in this work and swines are short-lived, swines are assumed to acquire life-long immunity.
In this proposed study, swines are vaccinated by MLV vaccines. There are two types of vaccination: vaccination at births and vaccination from a susceptible pool. We assume that a fraction q of the swine population is vaccinated at births while susceptible swines are successfully vaccinated at a rate u where \(1/u\) is the average time that susceptible swines remain susceptible before vaccination. For simplicity, vaccines are assumed to be 100% efficacious in the model.
From the aforementioned assumptions, transmission dynamics of PRRSV is described by the following model:
3 Analytic results
From model (1), the following inequality is obtained:
so that we have
Similarly, it can be shown that \(I\geq 0\), and \(R\geq 0\). Accordingly, solutions of system (1) with positive initial conditions remain non-negative for all time \(t\geq 0\). Let \(N(t)=S(t)+I(t)+R(t)\). Then
Hence,
Consequently, the feasible region is given by
3.1 Steady states
By setting the right-hand sides of (1) equal to zero, two steady states of the system are found: disease free and disease-present steady states.
-
1
The disease-free steady state is given by \(E^{0} = (S^{0},I ^{0},R^{0})\) with
$$ \begin{gathered} S^{0} = \biggl(1-\frac{\mu }{b} \biggr)K-R^{0}, \\ I^{0} = 0, \\ R^{0} = \frac{(q\mu +u) (1-\frac{\mu }{b} )K}{\mu +u}. \end{gathered} $$ -
2
The disease-present steady state is given by \(E^{*} = (S^{*},I ^{*},R^{*})\) where we have
$$\begin{aligned}& S^{*} = \frac{\mu +\gamma }{\beta }, \\& R^{*} = \frac{((\mu +u)-(1-q)\mu )(\mu +\gamma )}{(1-q)\mu \beta }+\frac{(( \mu +u)-(1-q)\mu )I^{*}}{(1-q)\mu \beta }, \end{aligned}$$and \(I^{*}\) satisfying
$$\begin{aligned} a_{0}\bigl(I^{*}\bigr)^{2}+a_{1} I^{*}+a_{2}=0 \end{aligned}$$with
$$\begin{aligned}& a_{0} = \frac{-b(\mu +\gamma )}{K\mu } \biggl(r-1+\frac{\mu +\gamma }{(1-q) \mu } \biggr), \\& \begin{aligned} a_{1} &= \biggl((1-q)b-\frac{b(\mu +u)(\mu +\gamma )}{K\mu \beta } \biggr) \biggl(r-1+ \frac{\mu +\gamma }{(1-q)\mu } \biggr)-\frac{b(\mu +u)( \mu +\gamma )^{2}}{K\beta \mu ^{2}(1-q)} \\ & \quad {} -(\mu +\gamma ), \end{aligned} \\& a_{2}= \biggl(\frac{b}{\mu }-1 \biggr) \biggl( \frac{(\mu +u)(\mu + \gamma )}{\beta } \biggr)-\frac{b(\mu +u)^{2}(\mu +\gamma )^{2}}{K\mu ^{2}\beta ^{2}(1-q)} . \end{aligned}$$
After some time, a system solution either approaches or moves away from a steady state. If it approaches the steady state, dynamical behaviors of the system will not change and remain at the steady state. Whether the system solution approaches the disease-free steady state or the disease-present steady state depends on stability conditions which can be determined via the basic reproduction number of system (1).
3.2 The basic reproduction number (\(R_{0}\))
The basic reproduction number \((R_{0})\) is a quantity that represents the number of infected swines after introducing an infected swine into a susceptible population. Consequently, PRRSV dies out from a swine population if \(R_{0}<1\) and persists if \(R_{0}>1\). Note that \(R_{0}\) can also be used to reflect the severity of an outbreak and the prevalence level. If \(R_{0}\) is large, it is more likely that an outbreak is severe and the disease prevalence is high [15]. The basic reproduction number can be calculated by the next-generation matrix method [17]. Let us rewrite system (1) in the following form:
where
and
Note that X is sorted so that the disease compartments come first in order, \(\mathcal{F}\) is a column matrix of the rate of appearance of new infections in each compartment, and \(\mathcal{V}\) is a column matrix of the transfer rate of individuals out of each compartment. Finding the Jacobian matrices of \(\mathcal{F}\) and \(\mathcal{V}\) at the disease-free steady state \(E^{0}\) gives
The Jacobian of \(\mathcal{V}\) at the disease-free steady state is given by
where \(m=(S^{0}+R^{0})/K\). Consequently, by partitioning the above Jacobian matrices in such a way that F and V are a non-negative matrices and a non-singular M matrix, we get
Therefore, \(R_{0}\) can be calculated as the spectral radius of \(FV^{-1}\) and it is given by
Based on the formula, \(R_{0}\) can be reduced by increasing vaccination coverage and vaccination rate.
3.3 Stability analysis
Theorem
The disease-free steady state is locally asymptotically stable if \(R_{0}<1\).
Proof
To prove this theorem, we use the Routh–Hurwitz criterion. First, we calculate the Jacobian matrix at the disease-free steady state
To find the eigenvalues of \(J(E^{0})\), set \(\det (J(E^{0})-\lambda I)=0\) to obtain the characteristic equation of the following form:
with
under the assumption that \(b>\mu \), or equivalently, that the birth rate exceeds the death rate. According to the Routh–Hurwitz criterion [18], the following three conditions must be satisfied:
-
1
\(m_{1}>0\),
-
2
\(m_{3}>0\),
-
3
\(m_{1}m_{2}>m_{3}\).
It is obvious that \(m_{1}>0\) if \(R_{0}<1\). This is also true for the second condition that \(m_{3}>0\). Let us now consider the last condition as follows:
It can be clearly seen that \(m_{1}m_{2}>m_{3}\) for \(R_{0}<1\). Consequently, based on the Routh–Hurwitz criterion, the disease-free steady state is locally asymptotically stable if and only if \(R_{0}<1\). Equivalently, PRRSV dies out if \(R_{0}<1\) and persists otherwise. □
4 Numerical results
In this section, numerical approaches are implemented to investigate the transmission dynamics of PRRSV among the swine population and the effects of a vaccination program on the prevalence of PRRSV. Figure 2(a) shows the presence of susceptible, infectious, and recovered swines according to time when parameters are set as values shown in Table 1. In Fig. 2(b), we demonstrate that PRRSV persists when \(R_{0}>1\) and dies out when \(R_{0}<1\).
To explore the effects of vaccination on the epidemic size and the endemic number, u and q are varied (\(0\leq q\leq 1\), \(0\leq u \leq 2\)) as shown in Fig. 3. It is obvious that increasing the vaccination coverage and the vaccination rate can help reduce the severity of an outbreak (see Fig. 3(a)–(b)) and the prevalence of \(PRRSV\) among the swine population (see Fig. 3(c)–(d)). Furthermore, by adjusting our numerical simulation, we are able to investigate discrete-time vaccination strategies which may be more realistic in the real world. We assume that swines are vaccinated at births at certain time points (semiannually, annually, and biennially) and then keep the model being time-continuous and vaccination-free during each time interval. Two scenarios of vaccination strategies are studied here: (A) when only susceptible swines are vaccinated and (B) when both susceptible and recovered swines are vaccinated. For the investigation of discrete-time vaccination, vaccination at births is only taken into account while vaccination from the susceptible pool is not considered. Hence, we assume that at the beginning of each time interval T, a proportion q of swines is vaccinated at births so that the initial conditions are reset at every time interval as follows:
where \(T_{n}\) is the nth time interval with \(T_{n}=nT\) for \(n=0,1,2,\ldots \) and \(x(T_{n},T_{n-1})\) with \(x=S,I,R\) represents a solution of x of (1) at the time \(T_{n}\) solved with the initial value at the time \(T_{n-1}\) as \(x(T_{n-1})\) and \(q=0\) for \(T_{n-1}< t< T_{n}\). It can be seen in Fig. 4(a)–(c) that the frequency of vaccination and the information about immunity affects the prevalence of PRRSV and the severity of subsequent outbreaks. The prevalence and the severity of subsequent outbreaks increase when swines are vaccinated less frequently and when vaccination is without information about immunity. In Fig. 4(d)–(e), the vaccination interval is set to be annual to investigate the effects of vaccination coverage and immunity information. The vaccination coverage is chosen to be \(q=0.7\) in Fig. 4(d) and \(q=0.3\) in Fig. 4(e). Our results in Fig. 4(a), (b), and (e) suggest that the prevalence of infected swines increases when the vaccine coverage is reduced and the number of infected swines dramatically increases, especially when the information about immunity is not known (see Fig. 4(e)).
The epidemic size and the endemic number: (a) the epidemic size when q varies and \(u=0,0.5,1,1.5, 2\); (b) the epidemic size when u varies and \(q=0,0.3,0.5,0.8,1\); (c) the endemic number when when q varies and \(u=0,0.5,1,1.5,2\); and (d) the endemic number when u varies and \(q=0,0.3,0.5,0.8,1\)
(a)–(c) The number of infectious swines according to time when vaccination occurs at the beginning of each time interval semiannually, annually, and biennially for \(q=0.5\), \(u=0\) for two vaccination scenarios, (A) and (B). In (d) and (e), vaccination occurs annually but the vaccination coverage is set to be 0.7 and 0.3, respectively
5 Optimal control results
To find optimal vaccination strategies to control the spread of PRRSV, both vaccination coverage and vaccination rate are now assumed to depend on time. The objective is to minimize the number of infected swines and control efforts. Hence, the objective functional is described by
The time domain is chosen to be 2 years in this study, \(t\in [0,T]=[0,2]\). The vaccination coverage ranges between 0 and 1 while the vaccination rate ranges from 0 to 2. Note that the optimal solution remains the same shape even though T changes. To obtain an adjoint problem for an optimal solution, we follow the same steps as appeared in [22] by creating the Hamiltonian as follows:
The optimality conditions are defined by:
Consequently, we obtain
The adjoint equations and transversality conditions for this optimal problem are:
where \(\lambda _{1}(2)=\lambda _{2}(2)=\lambda _{3}(2)=0\). Finally, we solve system (1) along with (2) to obtain the optimal results by the forward–backward sweep method with the time step of 0.002.
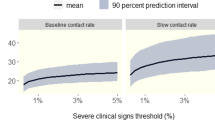
Our results in Fig. 5(a) suggest that vaccination at births and vaccination from the susceptible population should be at the maximum rates before reducing them at the end of the control interval. By estimating constant vaccination coverage and vaccination rate that have the same area under curves (AUCs) with optimal q and u, approximately 1.5 and 1.3, we obtain \(u\approx 0.663\) and \(q=0.762\) which gives \(R_{0}\approx 3\) with the rest of model parameters in Table 1. Consequently, we can compare our optimal results with the constant case by using the area under the curve \(I(t)\). For the optimal case, AUC is 10 while it is 14 for the constant one. Hence, our results suggest optimality of the solution or the smaller number of infected swines after applying the optimal vaccination strategy. Figure 5(b) and 5(e) demonstrate optimal vaccination controls when the death rate is varied and their corresponding optimal results. When the death rate is low, the average time that swines stay in a farm becomes longer and \(R_{0}\) becomes bigger for the constant case. The optimal controls suggest the longer effort to vaccinate swines at the maximum vaccination coverage and the maximum vaccination rate if swines spend time in a farm longer. When the recovery rate is varied, the lower rate suggests the longer time of being infectious and the higher \(R_{0}\) for the constant case. In Figs. 5(c) and 5(f), our optimal control results suggest a longer effort to vaccinate swines at the maximum vaccination coverage and the maximum vaccination rate if the recovery rate is low.
(a) & (d) Optimal vaccination coverage and vaccination rate and their optimal results; (b) & (e) Optimal vaccination coverage and vaccination rate and their optimal results when the death rate is varied \(\mu =1,2,3\); (c) & (f) Optimal vaccination and vaccination rate and their optimal results when the recovery rate is varied \(\gamma =365/28,365/56,365/84\)
6 Conclusion and discussion
In this study, a mathematical model is employed to help investigate the transmission dynamics of PRRSV among a swine population, factors that may affect the prevalence of PRRSV and the severity of outbreaks, and optimal vaccination strategies to minimize the number of infectious swines. Two vaccination scenarios are considered: vaccination at births and vaccination from a susceptible pool.
Based on the next-generation matrix method, the basic reproduction number \((R_{0})\) is calculated. If \(R_{0}<1\), the disease-free steady state is stable so that PRRSV dies out from the swine population. Local stability of the disease-free steady state is also demonstrated in the study. If \(R_{0}>1\), PRRSV persists in the swine population. The formula of \(R_{0}\) suggests that several factors may involve in determining the presence of PRRSV. For example, the higher transmission rate may result in a higher tendency of PRRSV to be prevalent in the swine population. It also suggests that PRRSV can be controlled by increasing vaccination coverage and vaccination rate.
To identify factors that affect the prevalence of PRRSV and the severity of outbreaks, we implement numerical techniques. Our findings suggest that increasing the vaccination coverage and the vaccination rate helps reduce the prevalence of PRRSV and severity of outbreaks. Our results also suggest that the prevalence and the severity of subsequent outbreaks increase if swines are vaccinated less frequently or information about immunity is absent. The worst vaccination scenario happens when vaccination resources and information are limited or equivalently both events occur. Moreover, our optimal results suggest that the effort of vaccinating swines should be maximized as long as possible when swines stay longer in the farm or it takes longer for them to recover from PRRS infections. These results also link to our calculated \(R_{0}\); if \(R_{0}\) is large, vaccination effort should be prolonged as much as possible.
Finally, we believe that this study may help gain a better understanding of transmission dynamics of PRRSV and suggest possible control strategies to help reduce infection cases.
References
Wang, X., Marthaler, D., Rovira, A., Rossow, S., Murtaugh, M.P.: Emergence of a virulent porcine reproductive and respiratory syndrome virus in vaccinated herds in the United States. Virus Res. 210, 34–41 (2015)
Keffaber, K.: Reproductive failure of unknown etiology. Am. Assoc. Swine Pract. Newslett. 1, 1–9 (1989)
Cho, J.G., Dee, S.A.: Porcine reproductive and respiratory syndrome virus. Theriogenology 66, 655–662 (2006)
Pileri, E., Mateu, E.: Review on the transmission porcine reproductive and respiratory syndrome virus between pigs and farms and impact on vaccination. Vet. Res. 47, 108 (2016)
Charerntantanakul, W.: Adjuvants for porcine reproductive and respiratory syndrome virus vaccines. Vet. Immunol. Immunopathol. 129, 1–13 (2009)
Zhou, L., Yang, H.: Porcine reproductive and respiratory syndrome in China. Virus Res. 154, 31–37 (2010)
Corzo, C.A., Mondaca, E., Wayne, S., Torremorell, M., Dee, S., Davies, P., Morrison, R.B.: Control and elimination of porcine reproductive and respiratory syndrome virus. Virus Res. 154, 185–192 (2010)
Díaz, I., Gimeno, M., Callén, A., Pujols, J., López, S., Charreyre, C., Joisel, F., Mateu, E.: Comparison of different vaccination schedules for sustaining the immune response against porcine reproductive and respiratory syndrome virus. Vet. J. 197, 438–444 (2013)
Evans, C.M., Medley, G.F., Creasey, S.J., Green, L.E.: A stochastic mathematical model of the within-herd transmission dynamics of porcine reproductive and respiratory syndrome virus (PRRSV): fade-out and persistence. Prev. Vet. Med. 93, 248–257 (2010)
Jeong, J., Aly, S.S., Cano, J.P., Polson, D., Kass, P.H., Perez, A.M.: Stochastic model of porcine reproductive and respiratory syndrome virus control strategies on a swine farm in the United States. Am. J. Vet. Res. 75, 260–267 (2014)
Haredasht, S.A., Polson, D., Main, R., Lee, K., Holtkamp, D., Martínez-López, B.: Modeling the spatio-temporal dynamics of porcine reproductive & respiratory syndrome cases at farm level using geographical distance and pig trade network matrices. BMC Vet. Res. 13, 163 (2017)
Arruda, A.G., Friendship, R., Carpenter, J., Greer, A., Poljak, Z.: Evaluation of control strategies for porcine reproductive and respiratory syndrome (PRRS) in swine breeding herds using a discrete event agent-based model. PLoS ONE 11, e0166596 (2017)
Suksamran, J., Lenbury, Y., Satiracoo, P., Rattanakul, C.: A model for porcine reproductive and respiratory syndrome with time-dependent infection rate: traveling wave solution. Adv. Differ. Equ. 2017, 215 (2017)
Gao, L.Q., Hethcote, H.W.: Disease transmission models with density-dependent demographics. J. Math. Biol. 30, 717–731 (1992)
Chamchod, F., Cantrell, R., Cosner, G., Hassan, A.N., Beier, J., Ruan, S.: A modeling approach to investigate epizootic outbreaks and enzootic maintenance of Rift Valley fever virus. Bull. Math. Biol. 76, 2052–2072 (2014)
Tkachenko, N., Weissmann, J.D., Petersen, W.P., Lake, G., Zollikofer, C.P.E., Callegari, S.: Individual-based modelling of population growth and diffusion in discrete time. PLoS ONE 12, e0176101 (2017)
van den Driessche, P., Watmough, J.: Reproduction numbers and sub-threshold endemic equilibria for compartmental models of disease transmission. Math. Biosci. 180, 29–48 (2002)
Edelstein-Keshet, L.: Mathematical Models in Biology. Random House, New York (2005)
Pepin, K.M., Davis, A.J., Cunningham, F.L., VerCauteren, K.C., Eckery, D.C.: Potential effects of incorporating fertility control into typical culling regimes in wild pig populations. PLoS ONE 12, e0183441 (2017)
Charpin, C., Mahé, S., Keranflec’h, A., Belloc, C., Cariolet, R., Potier, M.L., Rose, N.: Infectiousness of pigs infected by the porcine reproductive and respiratory syndrome virus (PRRSV) is time-dependent. Vet. Res. 43, 69 (2012)
Nodelijk, G., De Jong, M.C.M., Van Nes, A., Vernooy, J.C.M., Van Leengoed, L.A.M.G., Pol, J.M.A., Verheijden, J.H.M.: Introduction, persistence and fade-out of porcine reproductive and respiratory syndrome virus in a Dutch breeding herd: a mathematical analysis. Epidemiol. Infect. 124, 173–182 (2000)
Lenhart, S., Workman, J.T.: Optimal Control Applied to Biological Models. CRC Press, Boca Raton (2007)
Funding
PP would like to acknowledge the financial support from the Science Achievement Scholarship of Thailand. FC and CK were partially supported by the Centre of Excellence in Mathematics.
Author information
Authors and Affiliations
Contributions
PP and FC designed the study. PP developed the model, performed the analytic calculations and the numerical simulations, and interpreted the results. All wrote the manuscript, read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Phoo-ngurn, P., Kiataramkul, C. & Chamchod, F. Modeling the spread of porcine reproductive and respiratory syndrome virus (PRRSV) in a swine population: transmission dynamics, immunity information, and optimal control strategies. Adv Differ Equ 2019, 432 (2019). https://doi.org/10.1186/s13662-019-2351-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13662-019-2351-6