Abstract
Background
Salivary gland (SG) hypofunction (objectively reduced saliva flow rate) and xerostomia (subjective sensation of dry mouth) are common and burdensome side effects of radiotherapy to the head and neck region. Currently, only sparse symptomatic treatment is available to ease the discomfort of xerostomia. The objective of this study is to assess the effect of mesenchymal stem cell (MSC) therapy on SG function after radiation-induced injury.
Methods
This systematic review will include animal intervention studies assessing efficacy and safety of MSCs in treating radiation-induced SG hypofunction. The primary outcome is the effect of MSC administration on salivary flow rates (SFR), by comparing treated groups to control groups when available. Secondary outcomes are morphological and immunohistochemical effects as well as safety of MSC treatment. Electronic searches in MEDLINE (PubMed) and Embase databases will be constructed and validated according to the peer review of electronic search strategies (PRESS) and assessed by two independent researchers. Data from eligible studies will be extracted, pooled, and analyzed using random-effects models. Risk of bias will be evaluated with the Systematic Review Centre for Laboratory animal Experimentation (SYRCLE) risk of bias tool.
Discussion
Thus far, critical appraisal of MSC therapy as an effective treatment for SG hypofunction caused solely by radiation injury has not been conducted. A summary of the existing literature on preclinical studies concerning this issue can provide valuable information about effectiveness, mode of action, and safety, allowing further optimization of preclinical and clinical trials.
Systematic review registration
PROSPERO CRD42021227336
Similar content being viewed by others
Background
Impaired salivary gland (SG) function and xerostomia (subjective sensation of dry mouth) are very common long-term side effects of radiation to the head and neck region [1]. Radiation therapy plays a key role in the curative treatment of most head and neck cancers, either independently or in adjunction to other treatment modalities, such as surgery and chemotherapy [2]. Although the emergent intensity-modulated radiation therapy (IMRT) allows a more precise delivery to target tumor tissue while to some extent sparing surrounding tissues, the SGs are often included in the radiation portal, leading to degeneration with long-term loss of function [3, 4]. In addition to the subjective sensation of dry mouth, decreased salivation predisposes to speech and swallowing problems, infections and tooth loss, and consequently poor quality of life. Only sparse symptomatic treatment is available yet, and no current regimens are aimed at restoring SG function [1, 5,6,7].
Accumulating literature on animal studies suggests that mesenchymal stromal/stem cell (MSC) transplantation therapy can restore radiation-injured SGs and hence can be a potentially curative treatment for SG hypofunction [8, 9]. Moreover, MSC therapy was shown to enhance the unstimulated salivary flow rate (SFR) in human participants in a randomized control phase I/II trial [10].
MSCs are multipotent adult cells capable of differentiating into all mesodermal lineages (i.e., osteoblasts, adipocytes, chondrocytes) in vitro. They have been isolated from numerous connective tissues and have been shown to enhance regeneration through their angiogenic, anti-inflammatory, and immune-modulatory properties [11,12,13].
Recent systematic reviews have addressed the potential value of MSCs as an effective treatment for SG hypofunction and xerostomia [8, 9, 14]. However, critical appraisal of its use in SG hypofunction caused solely by radiation damage has yet to be conducted. It is therefore of great importance to review preclinical studies on this issue in order to optimize further clinical trials and to favor its prospective implication in the curative treatment of radiation-induced SG hypofunction [15].
Research questions
-
1.
What impact does MSC therapy have on restoration of SG function after radiation-induced injury and hypofunction in animal models?
-
2.
Is MSC therapy safe in terms of adverse events?
Objectives
The main objective of the present study is to assess the effect of MSC therapy on restoring SG function after radiation-induced injury. By reviewing the literature on animal studies, we will examine if MSC therapy promotes changes in SFR as well as on SG morphology and in saliva composition. Furthermore, safety of the intervention will be analyzed by observing adverse events.
Methods
Protocol and registration
The systematic review protocol was developed by a research team of clinical and preclinical research scientists, experts in knowledge synthesis and translation, one expert in literature search, and experts in data management. It was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) [16]. A summary of the protocol is listed at PROSPERO. The final protocol is reported using the PRISMA guidelines (Additional file 1).
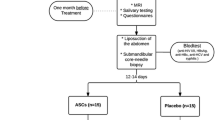
Types of studies
This review will include animal intervention studies evaluating the efficacy and safety of MSC therapy for radiation-induced SG hypofunction. All studies addressing the above will be included, and it will be noted whether the studies were controlled, uncontrolled, randomized, and/or blinded. Human studies will be excluded in the systematic review; however, they will be mentioned/described in the introduction and/or discussion of the final manuscript to bring some background on the clinical implementation of MSC therapy for SG hypofunction. As far as we know, a single clinical trial was conducted on this topic [10].
Types of animal models
We will include preclinical in vivo models of experimentally induced radiation damage of the major SGs that represent pathophysiological features of human SG hypofunction and xerostomia. No restrictions regarding induction of radiation damage (e.g., frequency, duration, power) will be applied. Eligible animal models include healthy mammals of both sexes and all ages. It will be noted if the models include the use of immunosuppressive drugs. In vitro studies will be excluded.
Types of interventions
The assessed intervention will be MSC administration to animals exhibiting radiation-induced SG hypofunction, including intra-glandular MSC implantation, intravenous and/or intramuscular injections, and others. Studies with repeated dosing interventions will be included. MSCs may be autologous, allogeneic, syngeneic, or xenogeneic and derived from any organ or tissue (e.g., bone marrow, adipose tissue). It will be noted if MSCs have been preconditioned in any way, or if they have been labelled either genetically or by surface labelling. MSC secretome, exosomes, and treatment with parts of MSCs are also included. The time period between induction of radiation damage and MSC administration in included studies will be reported but will not be a restriction with regard to inclusion and exclusion of relevant studies. However, MSC administration must be subsequent to induction of radiation damage.
Types of control comparisons
MSC-treated populations will be compared to untreated, vehicle-treated, or sham controls with experimentally induced radiation damage of the major SGs. Baseline controls are accepted and will be included in the (narrative) analysis. It will be noted if studies reported clearly defined controls.
Types of outcome measures
Primary outcomes
The primary outcome is change in SG function measured by SFR subsequent to MSC administration.
Secondary outcomes
Defined a priori secondary outcomes are changes in SG morphology (e.g., weight, atrophy), SG histology including immunohistochemical appearance (e.g., cytoprotection, apoptosis, vascularity), changes in the composition of saliva (e.g., proteins, RNAs, inorganic ions), and circulating immune cells, SG paracrine effects, mode of action, and safety in terms of objective adverse events (e.g., animal mortality, morbidity, impaired physical activity, signs of pain or distress such as grimacing, flinching, writhing ) of MSC therapy.
Timing of outcome assessment
Outcomes will be assessed post-intervention. All time points will be extracted at data extraction and compared in the narrative synthesis. Only the final point will be kept for meta-analysis. If possible, subgroup analysis will be performed to compare the exposure and treatment patterns (e.g., frequency, time to treatment).
Electronic search strategies for identification of studies
Electronic search strategies were developed by the research group in collaboration with a medical information specialist. PubMed® and Embase® will be searched using Medical Subject Headings (MeSH), Emtrees, and text words relating to mesenchymal stem cells, salivary gland hypofunction, salivary gland damage, salivary gland dysfunction, radiation-induced salivary gland damage, or xerostomia. Search strings for the two databases were created, as shown below. Syntax and subject headings were adapted according to the database being searched. Search strategies will be validated using the peer review of electronic search strategies (PRESS) template by another member of the review team [17]. No restriction on publication date, publication type, or language will be applied. Apart from searching these databases, we will manually seek for further relevant articles by verifying reference lists of included papers.
Search string for PubMed
(((((("Stem Cells"[Mesh] OR "Stromal Cells"[Mesh] OR "Stem Cell Transplantation"[Mesh] OR Stem Cell*[Text Word] OR stromal cell*[Text Word] OR mesenchymal [Text Word] OR ASC*[Text Word] OR ADSC*[Text Word] OR MSC*[Text Word] OR BMSC*[Text Word] OR "cell therapy"[Text Word])) OR (("secretome"[Text Word] OR "exosome"[Text Word]))))) AND (((saliva*[Text Word] OR "Salivation"[Mesh] OR "Xerostomia"[Mesh] OR xerostomia [Text Word] OR hyposalivation [Text Word] OR "dry mouth"[Text Word] OR salivary gland*[Text Word] OR "salivary hypofunction"[Text Word] OR "intraglandular"[Text Word])) OR ((submandibular*[Text Word] OR parotid [Text Word])))) AND ("Radiotherapy"[Mesh] OR radiotherap*[Text Word] OR radiation*[Text Word] OR radio-induced [Text Word] OR irradiation*[Text Word] OR postradiation*[Text Word] OR chemoradiotherap*[Text Word] OR "Radiation Injuries"[Mesh] OR "Radiation"[Mesh])
Search string for Embase
1. (stem cell/ or adipose derived stem cell/ or adult stem cell/ or exp mesenchymal stem cell/ or mononuclear stem cell/ or multipotent stem cell/)
2.stroma cell/
3. stem cell transplantation/ or allogeneic stem cell transplantation/ or autologous stem cell transplantation/ or mesenchymal stem cell transplantation/
4. (Stem Cell* or stromal cell* or mesenchymal or ASC* or ADSC* or MSC* or BMSC* or "cell therapy").mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]
5. 1 or 2 or 3 or 4
6. saliva/
7.
hyposalivation/
8.
xerostomia.mp. or exp xerostomia/
9.
salivation.mp. or exp salivation disorder/ or salivation/
10.
dry mouth.mp.
11.
salivary gland.mp. or salivary gland/
12.
(xerostomia or hyposalivation or "dry mouth" or salivary gland* or "salivary hypofunction" or "intraglandular" or saliva).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]
13.
salivation.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]
14.
11 or 12 or 13
15.
exp radiation/ or exp intensity modulated radiation therapy/ or exp radiation injury repair/ or radiation.mp. or exp radiation exposure/ or exp ionizing radiation/ or exp radiation injury/
16.
(radiotherap* or radiation* or radio-induced or irradiation* or postradiation* or chemoradiotherap*).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]
17.
15 or 16
18.
5 and 14 and 17
19.
limit 18 to updaterange="oemezd (20200429195810-20200429195810]"
20.
("exosome" or "secretome").mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]
21.
4 or 20
22.
(submandibular* or parotid).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]
23.
6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 22
24.
17 and 21 and 23
Searching other resources
Three reviewers (PMJ, AFC, CH) will manually seek for further relevant articles by verifying reference lists of included papers as well as reviews that are excluded but identified during screening.
Data collection and analysis
The online software Covidence© (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org) will be used for importing citations from literature searches, screening of abstracts and titles, screening of full texts, and extracting data. Duplicates will be removed using EndNote™. All analyses will be conducted in the statistical software R©.
Selection of studies and data extraction
Three researchers (AFC, CH, PMJ) will independently screen titles and abstracts, after which full-text articles meeting the inclusion criteria will be identified and reviewed. Inclusion criteria are as follows: animal intervention studies including mammals of both sexes and all ages, exposure of SGs to ionizing radiation, and MSC therapy of all administration routes and outcomes mentioned in “Types of outcome measures.” In vitro studies, treatments other than MSCs, MSC secretome and exosomes, and SG damage due to causes other than ionizing radiotherapy and nonrelevant outcomes will be excluded. Disagreements will be solved by consensus, and if no agreement can be reached, another reviewer (BF or CDL) will be consulted. Reasons for exclusion of potentially eligible studies will be recorded and presented in accordance with the PRISMA-P guidelines developed for proper reporting of clinical systematic reviews.
Study level characteristics will be extracted independently by two researchers: study characteristics (e.g., design), study population (e.g., species, race, sex, gene modifications), type of SG injury induction (e.g., radiation injury, radiation dose, timing of injury induction with regard to intervention), type of anesthesia, intervention, and comparison (e.g., MSC dose and administration route, number of treatments), preclinical endpoints (e.g., SFR, adverse events), and timing of endpoint measurement and follow-up time and deaths. Data will be extracted from text, tables, and graphs. Graphs data will be extracted using the digital ruler WebPlotdigitizer©. Discrepancies will be resolved by consensus or by a third member of the review team. Data extraction forms will be prepared a priori, and a calibration exercise will pilot five studies to refine the forms and ensure inter-rater consistency using Cohen’s kappa coefficient [18]. Inter-rater reliability for ordered (nonbinary or categorical outcomes) will be evaluated using appropriate methods (Pearson correlation for continuous data and Spearman correlation for ranked data).”
Foreign articles in Swedish, Danish, Norwegian, German, and French will be extracted by knowledgeable co-authors and collaborators. If an article in another language than the one mentioned is included, we will extract data as best as possible using Google translate. In the event where this could not be done, the article would be excluded from data analysis in post hoc. Data to be extracted are either continuous (e.g., SFR (ml/min)) or dichotomous (e.g., adverse events). In case of missing data, authors will be contacted by e-mail twice; if we receive no answer after the second e-mail, the authors will be considered unreachable.
Assessment of risk of bias in included studies
The methodological quality will be assessed independently by two researchers using the SYRCLE (Systematic Review Center for Laboratory animal Experimentation) risk of bias tool [19]. This includes assessment of domains related to selection bias, performance bias, detection bias, attrition bias, and reporting bias. For each included study, each domain will be scored as low, high, or unclear risk of bias. To address the effect of risk of bias and small study size, we will perform sensitivity analysis where we will remove high risk of bias studies and/or small study to the meta-analysis. A meta-analysis will be performed if there are at least two included studies. However, we will then emphasize that the results most likely are due to a low number of studies if that is the case and hence need critical appraisal. Discrepancies will be resolved by consensus or by a third member of the review team.
Description of reporting
The latest Animal Research: Reporting of In Vivo Experiments (ARRIVE) guidelines will be used to evaluate the quality of reporting in preclinical studies. The ARRIVE guidelines were developed by the National Centre for the Replacement, Refinement, and Reduction of Animals in Research (NC3Rs) to improve the transparent and comprehensive reporting of research methods and results for in vivo animal experiments [20].
Data analysis
A descriptive summary will be conducted for all outcomes. To evaluate the efficacy of MSCs in treating radiation-induced SG hypofunction, a random-effects meta-analysis adjusted to Hedge’s g will be conducted on SFR. We consider meta-analysis as feasible with a minimum of two studies. If possible, subgroup analyses will be conducted on studies using complete MSCs and studies using MSC secretome or exosomes. Subgroup analysis will also be considered on other heterogeneity factors such as species, strain, sex, age, radiation characteristics (dose, duration, frequency), MSC administration route, frequency of treatment, and time between radiation and treatment. To perform this analysis, we require at least two studies in different categories. If there are multiple time points, only the last one will be included in the meta-analysis. If all studies included in the quantitative synthesis report similar outcome measures for SFR, the pooled effect estimate will be quantified with a weighted mean difference with 95% confidence intervals (95% CI). If not, a standardized mean difference with 95% CIs will be used. To evaluate safety of the treatment, a random-effects meta-analysis will be conducted on adverse events. The pooled estimate will be quantified with risk ratios with 95% CIs. Heterogeneity of the study results will be investigated using Cochrane Q-test and quantified with I2 values.
Discussion
Regenerative stem cell therapy is considered a prospective curative treatment for SG hypofunction and xerostomia. A large number of irradiated head and neck cancer patients worldwide are suffering from the harsh and long-lasting side effect of SG hypofunction and xerostomia, hence the importance of reaching a curative treatment.
Previous systematic reviews on preclinical trials have shown promising effects of MSC therapy on SG hypofunction [8, 9, 14]. However, these reviews have included SG hypofunction as a consequence of various causes, and therefore, different pathophysiological patterns could be expected. The effect of MSC therapy on SG hypofunction caused solely by radiation injury has not been evaluated.
Early phases of clinical trials on MSC treatment on radiation-induced SG hypofunction have recently been accomplished [10]. Progression of clinical research on the issue warrants further examination of efficacy and safety in animal models, supposedly improving methodology and standardizing procedures in order to manage radiation-induced SG hypofunction and xerostomia in a clinical setting.
Availability of data and materials
Not applicable
Abbreviations
- MSC:
-
Mesenchymal stem cell
- SG:
-
Salivary gland
- SFR:
-
Salivary flow rate
- PRESS:
-
Peer review of electronic search strategies
- SYRCLE:
-
SYstematic Review Center for Laboratory animal Experimentation
- PRISMA-P:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocol
- ARRIVE:
-
Animal Research: Reporting of In Vivo Experiments
- CI:
-
Confidence interval
References
Jensen SB, Vissink A, Limesand KH, Reyland ME. Salivary gland hypofunction and xerostomia in head and neck radiation patients. J Natl Cancer Inst Monogr. 2019;2019(53):95–106.
Marur S, Forastiere AA. Head and neck squamous cell carcinoma: update on epidemiology, diagnosis, and treatment. Mayo Clin Proc. 2016;91(3):386–96.
Vissink A, van Luijk P, Langendijk JA, Coppes RP. Current ideas to reduce or salvage radiation damage to salivary glands. Oral Dis. 2015;21(1):e1–10.
Nutting CM, Morden JP, Harrington KJ, Urbano TG, Bhide SA, Clark C, et al. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol. 2011;12(2):127–36.
Kakoei S, Haghdoost A-A, Rad M, Mohammadalizadeh S, Pourdamghan N, Nakhaei M, et al. Xerostomia after radiotherapy and its effect on quality of life in head and neck cancer patients. Arch Iran Med. 2012;15(4):214–8.
Liu X-K, Zeng Z-Y, Hong M-H, Zhang A-L, Cui N-J, Chen F-J. Clinical analysis of xerostomia in patients with nasopharyngeal carcinoma after radiation therapy. Ai Zheng Aizheng Chin J Cancer. 2004;23(5):593–6.
Memtsa P-T, Tolia M, Tzitzikas I, Bizakis J, Pistevou-Gombaki K, Charalambidou M, et al. Assessment of xerostomia and its impact on quality of life in head and neck cancer patients undergoing radiation therapy. Mol Clin Oncol. 2017;6(5):789–93.
Coppes RP, Stokman MA. Stem cells and the repair of radiation-induced salivary gland damage. Oral Dis. 2011;17(2):143–53.
Jensen DH, Oliveri RS, Trojahn Kølle S-F, Fischer-Nielsen A, Specht L, Bardow A, et al. Mesenchymal stem cell therapy for salivary gland dysfunction and xerostomia: a systematic review of preclinical studies. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(3):335–342.e1.
Grønhøj C, Jensen DH, Vester-Glowinski P, Jensen SB, Bardow A, Oliveri RS, et al. Safety and efficacy of mesenchymal stem cells for radiation-induced xerostomia: a randomized, placebo-controlled phase 1/2 trial (MESRIX). Int J Radiat Oncol Biol Phys. 2018;101(3):581–92.
El Agha E, Kramann R, Schneider RK, Li X, Seeger W, Humphreys BD, et al. Mesenchymal stem cells in fibrotic disease. Cell Stem Cell. 2017;21(2):166–77.
Galipeau J, Krampera M, Barrett J, Dazzi F, Deans RJ, DeBruijn J, et al. International Society for Cellular Therapy perspective on immune functional assays for mesenchymal stromal cells as potency release criterion for advanced phase clinical trials. Cytotherapy. 2016;18(2):151–9.
Ozdemir T, Fowler EW, Hao Y, Ravikrishnan A, Harrington DA, Witt RL, et al. Biomaterials-based strategies for salivary gland tissue regeneration. Biomater Sci. 2016;4(4):592–604.
Mavragani CP, Nezos A, Moutsopoulos HM. New advances in the classification, pathogenesis and treatment of Sjogren’s syndrome. Curr Opin Rheumatol. 2013;25(5):623–9.
Hooijmans CR, de Vries RBM, Ritskes-Hoitinga M, Rovers MM, Leeflang MM, IntHout J, et al. Facilitating healthcare decisions by assessing the certainty in the evidence from preclinical animal studies. PLOS One. 2018;13(1):e0187271.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Medica. 2012;22(3):276–82.
Hooijmans CR, Rovers MM, de Vries RB, Leenaars M, Ritskes-Hoitinga M, Langendam MW. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014;14(1):43.
NP du S, Hurst V, Ahluwalia A, Alam S, Avey MT, Baker M, et al. The ARRIVE guidelines 2.0: updated guidelines for reporting animal research. PLOS Biol. 2020;18(7):e3000410.
Acknowledgements
The corresponding author Charlotte Duch Lynggaard would like to thank Candys Foundation for funding.
Funding
The corresponding author Charlotte Duch Lynggaard is funded by the nonprofit organization Candys Foundation.
Author information
Authors and Affiliations
Contributions
The main design of the protocol was constructed by PMJ, CDL, JM, and CvB; however, all authors contributed to improvement and editing. PMJ and CDL were responsible for the drafting of the manuscript. SR developed the search strategy. RTL developed the data analysis strategy. SBJ, BF,CH, BSK, AFN, and CvB provided critical revisions for important intellectual content. JM had important methodological inputs and were responsible for risk of bias assessment strategy. All authors have reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) 2015 checklist: recommended items to address in a systematic review protocol.
Additional file 2.
A. Search string for PubMed. B. Search string for EMBASE.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jansson, P.M., Lynggaard, C.D., Carlander, A.F. et al. Mesenchymal stromal/stem cell therapy for radiation-induced salivary gland hypofunction in animal models: a protocol for a systematic review and meta-analysis. Syst Rev 11, 72 (2022). https://doi.org/10.1186/s13643-022-01943-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-022-01943-2