Abstract
Background
Mesenchymal stromal/stem cells (MSCs) have been suggested for salivary gland (SG) restoration following radio-induced salivary gland damage. This study aimed to determine the safety and effectiveness of MSC therapy on radio-induced SG damage and hypofunction in preclinical in vivo studies.
Methods
PubMed and EMBASE were systematically searched for preclinical in vivo interventional studies evaluating efficacy and safety of MSC treatment following radio-induced salivary gland damage published before 10th of January 2022. The primary endpoint was salivary flow rate (SFR) evaluated in a meta-analysis. The study protocol was published and registered on PROSPERO (www.crd.ac.uk/prospero), registration number CRD42021227336.
Results
A total of 16 preclinical in vivo studies were included for qualitative analysis (858 experimental animals) and 13 in the meta-analysis (404 experimental animals). MSCs originated from bone marrow (four studies), adipose tissue (10 studies) and salivary gland tissue (two studies) and were administered intravenously (three studies), intra-glandularly (11 studies) or subcutaneously (one study). No serious adverse events were reported. The overall effect on SFR was significantly increased with a standardized mean difference (SMD) of 6.99 (95% CI: 2.55–11.42). Studies reported improvements in acinar tissue, vascular areas and paracrine factors.
Conclusion
In conclusion, this systematic review and meta-analysis showed a significant effect of MSC therapy for restoring SG functioning and regenerating SG tissue following radiotherapy in preclinical in vivo studies without serious adverse events. MSC therapy holds significant therapeutic potential in the treatment of radio-induced xerostomia, but comprehensive, randomized, clinical trials in humans are required to ascertain their efficacy in a clinical setting.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most patients with head and neck cancer (HNC) are treated with radiotherapy [1]. Salivary gland (SG) hypofunction and xerostomia, the subjective feeling of dry mouth, are common and long-term side effects following radiotherapy in the head and neck area [2]. Despite the emergence of intensity-modulated radiation-therapy (IMRT), that to some extent spare the surrounding tissue due to a more precise delivery to target tissue, the SG are often damaged [3, 4]. Radio-induced SG damage is dose-dependent and leads to gland degeneration and progressive decline in saliva production, followed by complications such as xerostomia, problems with speech and swallowing, oral infections and dental caries thus reducing quality of life. Currently, only symptomatic treatments are available, and there is a lack of regenerative and restorative therapeutic options [2, 5,6,7].
Mesenchymal stromal/stem cells (MSCs) are multipotent adult progenitor cells that in vitro can differentiate into mesodermal lineages with abilities for tissue regeneration and which can be isolated from numerous connective tissues, e.g. bone marrow (MSCs[M]) and adipose tissue (MSCs[AT]) [8,9,10]. Aside from being easily accessible, MSCs encompass various advantages such as proliferative and differentiating capacities; but also, immunomodulatory, and trophic properties such as anti-inflammatory, anti-fibrotic, anti-apoptotic, angiogenetic and immunosuppressive effects [11,12,13]. Thus, MSCs have a therapeutic and disease-modifying potential to repair and/or restore radio-induced SG damage. Recent preclinical in vivo studies have focused on mesenchymal stem cell (MSC) transplantation to repair radiation damaged SGs as a potentially curative treatment for SG hypofunction [14, 15]. Also, MSC therapy have shown to improve salivary flow rate (SFR) in humans [16,17,18,19].
Nevertheless, while MSC therapy shows potential as a treatment option for radio-induced SG damage, existing studies have been limited in size, characterized by high heterogeneity in relation to MSC origin, and only a few have been conducted in both preclinical in vivo models and humans. The use of MSCs therapy for radio-induced SG hypofunction alone has not yet been evaluated in a systematic review and meta-analysis. The aim of this study was therefore to review the safety and effectiveness of MSC therapy for restoring SG function after radiation-induced damage in preclinical in vivo studies. This is of great importance to optimize clinical trials and to assess the prospective implication in the curative treatment of SG hypofunction caused by radiotherapy.
Method
The study adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement and the study protocol was published and registered on PROSPERO (www.crd.ac.uk/prospero), registration number CRD42021227336 [20].
We considered preclinical in vivo models that assessed MSC therapy following experimentally induced radiation injury of major SGs. Inclusion criteria were: (1) preclinical in vivo intervention studies of both sexes and all ages (2) exposure of SGs to ionizing radiation (3) MSC therapy of all administration routes. There were no restrictions regarding induction of radiation damage, but MSCs administration should be after induction of radiation injury. MSC secretome, exosomes, and treatment with parts of MSCs were also included. In vitro models, treatments other than MSCs, SG damage other than ionizing radiation and non-relevant outcome were excluded. Human studies were not included in the formal analysis but described and included the discussion. The primary outcome was efficacy measured by SFR and secondary outcomes was SG morphology, SG histology, changes in saliva composition, circulating immune cells, SG paracrine effects, mode of action and safety in terms of objective adverse events as previously described [20].
Systematic Search
In January 2022 two authors (ALFC, CH) systematically searched PubMed and Embase for preclinical in vivo interventional studies assessing the efficacy and safety of MSC therapy for radiation-induced SG hypofunction. The search was performed using Medical Subject Headings (MeSH), Emtrees and text words relating to MSCs, SG hypofunction, SG damage, SG dysfunction, radiation-induced SG damage or xerostomia. The specific search string for PubMed and Embase was previously described [20]. The search of databases reference lists was evaluated for additional relevant studies.
Data Extraction
Two authors (ALFC, CH) independently screened all articles for eligibility and disagreement was solved by consensus or by discussion with a third reviewer (BM or CDL). The following information was extracted from each study: (1) article information (author, publication year), (2) details on preclinical in vivo model (species, sex, sample size, age), (3) study design (controlled, uncontrolled, randomized and/or blinded), (4) irradiation details (dose, Gy, quality assurance and days from irradiation to MSC therapy), 6) MSC therapy (type, concentration, administration route, follow-up time), 7) statistical analysis, 8) outcomes (functional and molecular outcomes).
Quality Assessment and Risk of Bias
We assessed the quality of reporting in the included studies according to the latest Animal Research: reporting of in vivo Experiments (ARRIVE) guidelines [21]. One point was given for evidence of each quality criterion. The methodological quality was assessed using the SYRCLE (Systematic review Center for Laboratory Animal Experimentation) risk of bias tool in domains related to selection bias, performance bias, detection bias, attrition bias and reporting bias [22].
Data Analysis
A descriptive summary of all outcomes was performed. The efficacy of MSC therapy was evaluated by a random effect meta-analysis adjusted to Hedge’s g on SFR. If there were multiple time points, only the last one was included in the meta-analysis. A standardized mean difference (SMD) with 95% confidence intervals (CIs) was used to evaluate the effect on SFR. The SMD was calculated by dividing the difference in mean outcome between the groups with the standard deviation of outcome among participants as per recommendation by the Cochrane Handbook [23]. Heterogeneity of the study results was investigated using the Cochrane Q test and quantified with I² values. Subgroup analyses were performed for species, strain, sex, administration route, age in weeks, radiation duration, frequency of treatment, radiation dose and time between radiation to MSC treatment. Sub analysis on frequency of radiation was not performed since radiation was administered as a single treatment in all studies.
Results
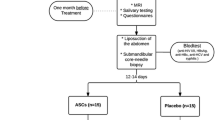
Sixteen preclinical studies published between 2011 and 2019 met the inclusion criteria, see Fig. 1 [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. One human study [19] (n = 30, intervention group n = 15) were identified. All preclinical in vivo studies were included in the quantitative (858 experimental animals) and 13 (404 experimental animals) were also included in the qualitative analyses, see Fig. 1.
Description of the Preclinical in vivo Models
All studies investigated the safety and efficacy of MSC-based therapy for xerostomia and SG hypofunction following radiation in the head and neck area. A total of 858 animals were included of which 341 received intervention with MSC therapy. Ten studies included mice, two studies rats and one study miniature pigs. The irradiation dose varied from 10 to 25 Gy, and all were administered as a single dose. See Table 1.
MSCs were originating from bone marrow (4 studies) [24, 27, 36, 37], adipose tissue (10 studies) [25, 28,29,30,31,32,33, 35, 38, 39], and salivary gland tissue (2 studies) [26, 34] and were administered intravenously (3 studies) [28, 31, 39], intra-glandularly (11 studies) [24,25,26,27, 29, 32,33,34,35,36, 38] or subcutaneously (1 study) [30]. One study did not specify administration route [37]. One study used secretomes originating from adipose tissue [39]. The mean follow-up time was 12 weeks after MSC treatment, ranging from 7 days to 24 weeks. See Table 1.
Safety of MSC
All included preclinical in vivo studies described the MSC-based cell therapy as safe with no reported serious adverse events [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39].
The Effect of MSCs on Efficacy, Salivary Flow Rate
13 studies included SFR as primary functional outcome [24,25,26,27,28,29, 31,32,33,34,35, 38, 39]. Eleven studies found a significant increase in SFR after intervention with MSCs compared to other groups (placebo/sham or IR only) [24,25,26,27,28,29, 32,33,34,35, 38], with an overall effect of SMD 6.99 (95% CI: 2.55–11.42), ranging from 1.68 (95% CI: 0.63–2.74) [31] to 25.41(95% CI: 15.22–35.59) [33]. Heterogeneity was X2 = 177.37 (p < .001) and I2 = 93% (95% CI [90–95%]). See Fig. 2.
Subgroup analyses investigating the effect of species, strain, sex, administration route, age in weeks, radiation duration, frequency of treatment, radiation dose and time between radiation to MSC treatment revealed significant differences regarding strain (p < .001) and administration route (p = .01). The most prominent differences were observed in the strains NOD.SCID-PrckSCID (SMD 22.92, 95% CI: 18.99–26.86) and Wistar (SMD 25.41, 95% CI: 15.22–35.59) compared to C57BL/6 (SMD 2.90, 95% CI: 0.08–5.52), CH3 (SMD 4.99, 95% CI: 1.58–8.39) and Spraque-Dawley (SMD 2.49, 05% CI: 1.81–3.18), while the effect following intraglandular injection was greater than following intravenously injection (SMD 8.59, 95% CI: 2.94–14.24 versus 2.12, 95% CI: 1.20–3.05, respectively). There was no significant effect of species, sex, age in weeks, radiation dose, frequency of treatment or time from radiation to first treatment. Effect of duration of radiation was not possible to assess due to insufficient data. See Supplementary Results.
The Effect of MSCs on Salivary Gland Regeneration and Apoptosis
Seven studies reported improvements in acinar tissue [25,26,27, 29, 31, 32, 35] with more acinar cells [25, 29, 32, 35] and more compact acinar structure [26]. Also, several studies reported less inflammation and fibrosis [25, 28, 30, 33, 35, 36] and increased amylase [27, 28, 31,32,33,34, 37,38,39]. Li et al. and Wang et al. reported intact cellular ultra-microstructure with healthy cell membrane and almost undamaged cytoplasmic organelles [31, 38]. They also found significantly higher proliferative activity, but this was not found by others [27, 28]. Shin et al. found greater expression of SG epithelial cell markers (KRT7 and KRT18) and upregulated structure-related genes (SMR3A, AMY2A5, PRB1, AMY1, CLDN22, PRPMP, AMY1A and AQP5) [35]. Similarly, Choi et al. found higher expressions of AQP5, alfa-SMA and CD31 [33]. Mulyani et al. found increased expression of SDF1-CXCR4 and Bcl-2 genes [37]. Nine studies reported reduction in apoptotic cells [26,27,28,29,30,31,32,33, 38], though Wang et al. did not specify the results [32].
Lim et al. observed anti-alfa-amylase signaling in transplanted MSC(M) suggesting a transdifferentiation into SG epithelial cells [27], but this was not found by Kojima et al. [25].
The Effect of MSCs on Vascular Areas
Several studies reported an increase in vascular areas [25, 27, 29,30,31]. Furthermore, Kojima et al. localized MSCs in vessel endothelial cells post transplantation five- and ten-weeks post transplantation [25]. Wang et al. also found improvements in vascular areas, but only for the intervention group receiving both MSCs and platelet-rich-fibrin (PRF) [38].
The Paracrine Effects of MSCs
Five studies reported on the paracrine effect of MSC treatment [25, 29, 33,34,35]: Xiong et el. found increased mRNA levels VEGF, HGF and COX-2 [29]; Shin et al. found higher expression of the paracrine factors BDNF, GDNF, EGF, IGF1 and NGF [34]; Shin et al. found greater expression of the growth factor FGF10 [35]; Kojima et al., found increased expressions of HGF, VEGF, COX-2 and MMP-2 [25] and Choi et al., found increased levels of EGF [33].
Homing of Systemically Transplanted MSCs
Both Li et al. and Lim et al. found that systematically transplanted MSCs could be identified in the salivary glands post transplantation [28, 31]. An et al. also administered the therapy intravenously but did not report on homing to the SG post transplantation [39].
Platelet-Rich Fibrin in Addition to MSCs
Two studies also investigated MSC + PRF [30, 38]. Chen et al. found the MSC + PRF group had significantly improvement on soft tissue defects [30], while Wang et al. found that MSC + PRF had increased levels of acinar cells, amylase, microvessels and proliferative activity and reduced levels of apoptotic cells [38].
The Effect of MSCs on Efficacy and Safety in Human Studies
One human study investigated the intervention of intraglandular autologous MSCs(AT) in a randomized, placebo-controlled phase I/II study (n = 30) [19]. The study found MSC treatment to be safe and reported a significant increased UWS (50% after four months, p = .003) including improvements in patient-reported outcomes in the group receiving MSCs. Also, a significant increase in serous gland tissue, improvements in saliva composition, and a decrease in connective were observed. See Supplementary Results.
Risk of Bias and Quality Assessment
The preclinical in vivo studies were assessed using SYRCLEs risk of bias assessment tool with nine questions to determine potential biases [22]. All studies involved a risk of bias, especially regarding selection bias as none of the studies reported how the randomization of intervention/control groups was performed [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. Also, all studies revealed a high risk of performance bias, since none of the included studies used random housing or blinding of interventions/investigators [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. All studies, except Mulyani et al., had a low risk of bias concerning attrition bias and reporting bias. Seven studies had a low risk of detection bias since they reported blinding of the outcome assessment [27, 28, 32, 33]: (1) histological examination [26, 35] (2) immunohistochemical evaluation [27, 31, 32, 37] (3) evaluation of apoptotic cells [26, 27, 32, 37, 38] (4) evaluation of cytoprotective effects (AQP5, CD31, alfa-SMA, c-Kit) [38]. Nine studies did not report blinding [24,25,26, 29,30,31, 34, 35, 37]. See Fig. 3.
The quality of the included studies was assessed using the ARRIVE guidelines [21]. Highest score given was 9 [27, 28, 32, 33, 36, 38] and lowest score given was 5 [26]. Most studies revealed high quality with ≥ 8 points [25, 27,28,29, 31,32,33,34,35,36, 38, 39], but 4 studies had a total score of ≤ 7 [24, 26, 30, 37]. All studies except Jeong et al. reported sufficiently regarding study design and sample size [24, 25, 27,28,29,30,31,32,33,34,35,36,37,38]. All studies reported sufficiently on outcome measures and results and all studies were randomized, though none reported on the randomization method used and none reported how they included/excluded animals [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. One study failed to report sufficiently on statistical method [24], one on experimental animals [30] and two studies failed to report sufficiently on experimental procedures [26, 37]. See Supplementary Results.
Discussion
In this systematic review and meta-analysis, MSC therapy demonstrated a significant effect on SG function following radiation-induced gland damage in preclinical in vivo studies. The treatment proved to be safe, with no reported adverse reactions.
We found that MSC therapy had a significant impact on the SG functioning with a significant increase in the SFR. However, there was a high heterogeneity among included studies with differences in MSC origin, species, strains, age, radiation dose, administration route of MSC therapy, frequency of treatment and time between radiation and first treatment. The impact on SFR was significantly associated with strain and administration route. The most pronounced effect on SFR was observed when MSCs were administered intraglandular compared to systemic transplantation. Whether the effect of MSC therapy varies by strain is difficult to conclude, as only one study included Wistar [26], and one study NOD.SCID-PrckSCID [24], which both exhibited the most significant effect.
All studies but one, by Lin et al., reported elements of SG remodeling properties such as: increased density of acinar cells, more compact acinar structure, increased levels of amylase, decreased inflammation and fibrosis. If MSC therapy induces a higher proliferative activity remains uncertain. While Shin et al. reported such an effect, it was not confirmed by other studies [26, 27]. As possible modes of action, upregulation in epithelial markers (KRT7 and KRT18) and structure-related genes (SMR3A, AMY2A5, PRB1, AMY1, CLDN22, PRPMP, AMY1A, AQP5, AQP5, alfa-SMA and CD31) was identified [33, 35], while another study by Mulyani et al. found upregulation in genes encoding for proteins involved in cell migration, survival and differentiation (SDF1-CXCR4 and Bcl-2) [37].
This study also indicates that increased blood vessel regeneration and paracrine functioning participate in the tissue repair and restoration of gland damage. Several studies reported an increase in vascular areas [24, 26, 28,29,30, 32]. A wide range of growth factors (VEGF, HGF, COX-2, BDNF, GDNF, EGF, IGF1, NGF, FGF10 and MMP-2) contributing to various aspects of regeneration including angiogenesis, neural regeneration and cellular proliferation were identified – ultimately supporting the repair of damaged glandular tissues.
The severity of radio-induced salivary gland damage is influenced by several factors, with radiation mean dose being a critical one [40]. The delivery of radiotherapy was greatly standardized and administered as a single dose in all the included studies, which does not resemble the clinical radiotherapy regimens for head and neck cancer which are patient-specific and often fractionated across several weeks. This is important to keep in mind, when translating the findings from this systematic review to a clinical setting. Prolonged exposure to radiation leads to cumulative damage, but unfortunately, we could not further investigate the relation between radiation duration and effect of MSC therapy due to insufficient data. The time from radiotherapy to administration of MSC might also be important, since especially the decreased levels of apoptotic cells found in several studies [26,27,28, 38], indicates that MSC therapy could be protective in the acute phase of radiotherapy. The timing of MSC administration varied across the studies from 0 days [28, 29, 31,32,33, 36, 39] to 12 weeks [25] post radiotherapy, but we observed no impact of the time from radiation to the initial MSC treatment.
Two studies that investigated the effect of intravenously administered MSC therapy also reported on homing to the SGs post transplantation, both identifying MSCs in the SGs [28, 31]. However, large-scale studies are required to further investigate the migration and homing following systemic transplantation.
PRF is a platelet-rich regenerative therapy containing a variety of growth factors and is known to promote cell proliferation [41]. Two studies investigated if additional PRF treatment improved SG function [30, 38]. Chen et al. found the MSC + PRF group had significantly improvement on soft tissue defects, but the groups were small, n = 5 [30]. Wang et al. found that interventions with MSC, PRF or MSC + PRF improved SFR, gland and body weight, but MSC + PRF performed better regarding the regenerative outcomes [38].
In addition, the preclinical in vivo studies included in the meta-analysis, we identified one human, phase I/II, randomized, placebo-controlled clinical trial. The study found no serious adverse events and a significant effect on unstimulated SFR four months post MSC(AT) therapy in the treated group [19]. This is also supported by a recent study by Lynggaard et al. [16]. However, the long-term effects of intraglandular MSC therapy in humans remain divergent [18, 42].
As a possible mode of action, Lynggaard et al. also investigated the regenerative effects of intraglandular allogeneic MSC(AT) therapy on the salivary proteome [43]. They observed an increase in proteins associated with tissue regeneration post transplantation, yet the salivary proteome did not return to a healthy state when compared to healthy controls [43].
This review is limited by the heterogeneity of methodologies and limited long-term data, hindering definite conclusions. The included studies varied in relation to included species, strains, origin of MSCs, delivering methods, radiation and follow-up regimen and study design. Prospects lie in optimizing challenges related to standardization of MSC therapy such as delivery methods, origin, and refining dosage protocols. Also, the radiotherapy regimens in the preclinical in vivo models were standardized and did not mirror those used in head and neck cancer patients. This lack of resemblance could potentially influence the effectiveness of MSC therapy in a clinical setting.
In conclusion, this systematic review and meta-analysis showed a significant effect of MSC therapy for restoring SG functioning and regenerating SG tissue following radiotherapy in preclinical in vivo studies. No serious adverse events were identified and intraglandular transplantation performed better effect than systemic transplantation. MSC therapy holds significant therapeutic potential in the treatment of radio-induced xerostomia and hypofunction, but comprehensive, randomized, clinical trials in humans are required to ascertain their efficacy in a clinical setting.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Marur, S., & Forastiere, A. A. (2016). Head and Neck squamous cell carcinoma: Update on Epidemiology, diagnosis, and treatment. Mayo Clinic Proceedings, 91, 386–396. https://doi.org/10.1016/j.mayocp.2015.12.017.
Jensen, S. B., Vissink, A., Limesand, K. H., & Reyland, M. E. Salivary gland hypofunction and Xerostomia in Head and Neck Radiation patients. Journal of the National Cancer Institute. Monographs 2019;2019. https://doi.org/10.1093/jncimonographs/lgz016.
Vissink, A., van Luijk, P., Langendijk, J. A., & Coppes, R. P. (2015). Current ideas to reduce or salvage radiation damage to salivary glands. Oral Diseases, 21, e1–10. https://doi.org/10.1111/odi.12222.
Nutting, C. M., Morden, J. P., Harrington, K. J., Urbano, T. G., Bhide, S. A., Clark, C., et al. (2011). Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): A phase 3 multicentre randomised controlled trial. The Lancet Oncology, 12, 127–136. https://doi.org/10.1016/S1470-2045(10)70290-4.
Kakoei, S., Haghdoost, A. A., Rad, M., Mohammadalizadeh, S., Pourdamghan, N., Nakhaei, M., et al. (2012). Xerostomia after radiotherapy and its effect on quality of life in head and neck cancer patients. Archives of Iranian Medicine, 15, 214–218.
Memtsa, P. T., Tolia, M., Tzitzikas, I., Bizakis, J., Pistevou-Gombaki, K., Charalambidou, M., et al. (2017). Assessment of xerostomia and its impact on quality of life in head and neck cancer patients undergoing radiation therapy. Mol Clin Oncol, 6, 789–793. https://doi.org/10.3892/mco.2017.1200.
Liu, X. K., Zeng, Z. Y., Hong, M. H., Zhang, A. L., Cui, N. J., & Chen, F. J. (2004). [Clinical analysis of xerostomia in patients with nasopharyngeal carcinoma after radiation therapy]. Ai Zheng, 23, 593–596.
El Agha, E., Kramann, R., Schneider, R. K., Li, X., Seeger, W., Humphreys, B. D., et al. (2017). Mesenchymal stem cells in Fibrotic Disease. Cell Stem Cell, 21, 166–177. https://doi.org/10.1016/j.stem.2017.07.011.
Ozdemir, T., Fowler, E. W., Hao, Y., Ravikrishnan, A., Harrington, D. A., Witt, R. L., et al. (2016). Biomaterials-based strategies for salivary gland tissue regeneration. Biomater Sci, 4, 592–604. https://doi.org/10.1039/c5bm00358j.
Galipeau, J., Krampera, M., Barrett, J., Dazzi, F., Deans, R. J., DeBruijn, J., et al. (2015). International Society for Cellular Therapy perspective on immune functional assays for mesenchymal stromal cells as potency release criterion for advanced phase clinical trials. Cytotherapy, 18, 151–159. https://doi.org/10.1016/j.jcyt.2015.11.008.
Singer, N. G., & Caplan, A. I. (2011). Mesenchymal stem cells: Mechanisms of inflammation. Annu Rev Pathol Mech Dis, 6, 457–478. https://doi.org/10.1146/annurev-pathol-011110-130230.
Caplan, A. I., & Dennis, J. E. (2006). Mesenchymal stem cells as trophic mediators. Journal of Cellular Biochemistry, 98, 1076–1084. https://doi.org/10.1002/jcb.20886.
Caplan, A. I., & Correa, D. (2011). The MSC: An injury drugstore. Cell Stem Cell, 9, 11–15. https://doi.org/10.1016/j.stem.2011.06.008.
Coppes, R. P., & Stokman, M. A. (2011). Stem cells and the repair of radiation-induced salivary gland damage. Oral Diseases, 17, 143–153. https://doi.org/10.1111/j.1601-0825.2010.01723.x.
Jensen, D. H., Oliveri, R. S., Trojahn Kølle, S. F., Fischer-Nielsen, A., Specht, L., Bardow, A., et al. (2014). Mesenchymal stem cell therapy for salivary gland dysfunction and xerostomia: A systematic review of preclinical studies. Oral Surg Oral Med Oral Pathol Oral Radiol, 117, 335–342e1. https://doi.org/10.1016/j.oooo.2013.11.496.
Lynggaard, C. D., Grønhøj, C., Christensen, R., Fischer-Nielsen, A., Melchiors, J., Specht, L., et al. (2022). Intraglandular off-the-Shelf allogeneic mesenchymal stem cell treatment in patients with Radiation-Induced Xerostomia: A Safety Study (MESRIX-II). Stem Cells Transl Med, 11, 478–489. https://doi.org/10.1093/stcltm/szac011.
Blitzer, G. C., Glazer, T., Burr, A., Gustafson, S., Ganz, O., Meyers, R., et al. (2023). Marrow-derived autologous stromal cells for the restoration of salivary hypofunction (MARSH): A pilot, first-in-human study of interferon gamma-stimulated marrow mesenchymal stromal cells for treatment of radiation-induced xerostomia. Cytotherapy, 25, 1139–1144. https://doi.org/10.1016/j.jcyt.2023.07.009.
Lynggaard, C. D., Grønhøj, C., Jensen, S. B., Christensen, R., Specht, L., Andersen, E., et al. (2022). Long-term safety of treatment with autologous mesenchymal stem cells in patients with Radiation-Induced Xerostomia: Primary results of the MESRIX Phase I/II Randomized Trial. Clinical Cancer Research, 28, 2890–2897. https://doi.org/10.1158/1078-0432.CCR-21-4520.
Grønhøj, C., Jensen, D. H., Vester-Glowinski, P., Jensen, S. B., Bardow, A., Oliveri, R. S., et al. (2018). Safety and efficacy of mesenchymal stem cells for Radiation-Induced Xerostomia: A randomized, placebo-controlled phase 1/2 trial (MESRIX). International Journal of Radiation Oncology Biology Physics, 101, 581–592. https://doi.org/10.1016/j.ijrobp.2018.02.034.
Jansson, P. M., Lynggaard, C. D., Carlander, A. F., Jensen, S. B., Follin, B., Hoeeg, C., et al. (2022). Mesenchymal stromal/stem cell therapy for radiation-induced salivary gland hypofunction in animal models: A protocol for a systematic review and meta-analysis. Syst Rev, 11, 72. https://doi.org/10.1186/s13643-022-01943-2.
Percie du Sert, N., Hurst, V., Ahluwalia, A., Alam, S., Avey, M. T., Baker, M., et al. (2020). The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. Plos Biology, 18, e3000410. https://doi.org/10.1371/journal.pbio.3000410.
Hooijmans, C. R., Rovers, M. M., de Vries, R. B. M., Leenaars, M., Ritskes-Hoitinga, M., & Langendam, M. W. (2014). SYRCLE’s risk of bias tool for animal studies. Bmc Medical Research Methodology, 14, 43. https://doi.org/10.1186/1471-2288-14-43.
https://handbook-5-1.cochrane.org/chapter_9/9_2_3_2_the_standardized_mean_difference.htm. (n.d).
Lin, C. Y., Chang, F. H., Chen, C. Y., Huang, C. Y., Hu, F. C., Huang, W. K., et al. (2011). Cell therapy for salivary gland regeneration. Journal of Dental Research, 90, 341–346. https://doi.org/10.1177/0022034510386374.
Kojima, T., Kanemaru, S. I., Hirano, S., Tateya, I., Ohno, S., Nakamura, T., et al. (2011). Regeneration of radiation damaged salivary glands with adipose-derived stromal cells. The Laryngoscope, 121, 1864–1869. https://doi.org/10.1002/lary.22080.
Jeong, J., Baek, H., Kim, Y. J., Choi, Y., Lee, H., Lee, E., et al. (2013). Human salivary gland stem cells ameliorate hyposalivation of radiation-damaged rat salivary glands. Experimental & Molecular Medicine, 45, e58. https://doi.org/10.1038/emm.2013.121.
Lim, J. Y., Yi, T., Choi, J. S., Jang, Y. H., Lee, S., Kim, H. J., et al. (2013). Intraglandular transplantation of bone marrow-derived clonal mesenchymal stem cells for amelioration of post-irradiation salivary gland damage. Oral Oncology, 49, 136–143. https://doi.org/10.1016/j.oraloncology.2012.08.010.
Lim, J. Y., Ra, J. C., Shin, I. S., Jang, Y. H., An, H. Y., Choi, J. S., et al. (2013). Systemic transplantation of human adipose tissue-derived mesenchymal stem cells for the regeneration of irradiation-induced salivary gland damage. PLoS One, 8, e71167. https://doi.org/10.1371/journal.pone.0071167.
Xiong, X., Shi, X., & Chen, F. (2014). Human adipose tissuederived stem cells alleviate radiationinduced xerostomia. International Journal of Molecular Medicine, 34, 749–755. https://doi.org/10.3892/ijmm.2014.1837.
Chen, Y., Niu, Z., Xue, Y., Yuan, F., Fu, Y., & Bai, N. (2014). Improvement in the repair of defects in maxillofacial soft tissue in irradiated minipigs by a mixture of adipose-derived stem cells and platelet-rich fibrin. British Journal of Oral and Maxillofacial Surgery, 52, 740–745. https://doi.org/10.1016/j.bjoms.2014.06.006.
Li, Z., Wang, Y., Xing, H., Wang, Z., Hu, H., An, R., et al. (2015). Protective efficacy of intravenous transplantation of adipose-derived stem cells for the prevention of radiation-induced salivary gland damage. Archives of Oral Biology, 60, 1488–1496. https://doi.org/10.1016/j.archoralbio.2015.07.016.
Wang, Z., Ju, Z., He, L., Li, Z., Liu, Y., & Liu, B. (2017). Intraglandular transplantation of adipose-derived stem cells for the Alleviation of Irradiation-Induced parotid gland damage in Miniature pigs. Journal of Oral and Maxillofacial Surgery, 75, 1784–1790. https://doi.org/10.1016/j.joms.2016.08.001.
Choi, J. S., An, H. Y., Shin, H. S., Kim, Y. M., & Lim, J. Y. (2018). Enhanced tissue remodelling efficacy of adipose-derived mesenchymal stem cells using injectable matrices in radiation-damaged salivary gland model. Journal of Tissue Engineering and Regenerative Medicine, 12, e695–706. https://doi.org/10.1002/term.2352.
Shin, H. S., Lee, S., Hong, H. J., Lim, Y. C., Koh, W. G., & Lim, J. Y. (2018). Stem cell properties of human clonal salivary gland stem cells are enhanced by three-dimensional priming culture in nanofibrous microwells. Stem Cell Research & Therapy, 9, 74. https://doi.org/10.1186/s13287-018-0829-x.
Shin, H. S., Lee, S., Kim, Y. M., & Lim, J. Y. (2018). Hypoxia-activated adipose mesenchymal stem cells prevents Irradiation-Induced Salivary Hypofunction by enhanced paracrine effect through fibroblast growth factor 10. Stem Cells, 36, 1020–1032. https://doi.org/10.1002/stem.2818.
Elsaadany, B., Zakaria, M., & Mousa, M. R. (2019). Transplantation of bone marrow-derived mesenchymal stem cells preserve the salivary glands structure after Head and Neck Radiation in rats. Open Access Maced J Med Sci, 7, 1588–1592. https://doi.org/10.3889/oamjms.2019.350.
Mulyani, S. W. M., Astuti, E. R., Wahyuni, O. R., Ernawati, D. S., & Ramadhani, N. F. (2019). Xerostomia Therapy due to Ionized Radiation using preconditioned bone marrow-derived mesenchymal stem cells. Eur J Dent, 13, 238–242. https://doi.org/10.1055/s-0039-1694697.
Wang, Z., Xing, H., Hu, H., Dai, T., Wang, Y., Li, Z., et al. (2016). Intraglandular transplantation of adipose-derived stem cells combined with platelet-rich fibrin extract for the treatment of irradiation-induced salivary gland damage. Exp Ther Med, 15, 795–805. https://doi.org/10.3892/etm.2017.5497.
A, H. Y., C, H. S. S. J. S., & K, H. J. (2015). Adipose mesenchymal stem cell secretome modulated in hypoxia for remodeling of radiation-induced salivary gland damage. PLoS One, 10, e0141862. https://doi.org/10.1371/journal.pone.0141862.
Eisbruch, A., Ten Haken, R. K., Kim, H. M., Marsh, L. H., & Ship, J. A. (1999). Dose, volume, and function relationships in parotid salivary glands following conformal and intensity-modulated irradiation of head and neck cancer. International Journal of Radiation Oncology Biology Physics, 45, 577–587. https://doi.org/10.1016/s0360-3016(99)00247-3.
Dohan, D. M., Choukroun, J., Diss, A., Dohan, S. L., Dohan, A. J. J., Mouhyi, J., et al. (2006). Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics, 101, e37–44. https://doi.org/10.1016/j.tripleo.2005.07.008.
Kronberg Jakobsen, K., Duch Lynggard, C., Paaske, N., Fenger Carlander, A. L., Kastrup, J., Hauge Werner, A., et al. (2023). Long-term outcome following treatment with allogeneic mesenchymal stem/Stromal cells for Radiation-Induced Hyposalivation and Xerostomia. Stem Cells Transl Med.
Lynggaard, C. D., Jersie-Christensen, R., Juhl, M., Jensen, S. B., Grønhøj, C., Melchiors, J., et al. (2022). Intraglandular mesenchymal stem cell treatment induces changes in the salivary proteome of irradiated patients. Communications Medicine, 2, 160. https://doi.org/10.1038/s43856-022-00223-3.
Acknowledgements
We thank Julia Menon from the Preclinical Trials.eu, The Netherlands and Siri Beier Jensen from the Department of Dentistry and Oral Health, Aarhus University, Denmark for their careful and meticulous assistance in designing the study protocol
Funding
ALFC is support by the private fund Candys Foundation (reference: 2020 − 352–14024-1).
Open access funding provided by National Hospital
Author information
Authors and Affiliations
Contributions
ALFC: investigation, data curation, writing original draft preparation, visualization AG: data curation, review and editing CDL: Conceptualization, methodology, review and editing PMJ: review and editing BF: investigation, review and editing CH: investigation, review and editing BSK: review and editing RTL: formal analysis, review and editing CG: conceptualization, methodology, review and editing KKJ: conceptualization, review and editing AFN: review and editing CVB: Conceptualization, methodology, review and editing.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
C.D. Lynggaard, C. Grønhøj, and C. von Buchwald are co-inventors on a patent application PCT/EP2020/053878; the patent is owned by Rigshospitalet, Copenhagen University Hospital and the University of Copenhagen.
Role of the Funding Source
The funder had no role in study design, in the collection, analysis or interpretation of data, in the writing of the report or in the decision to submit this article for publication. The sole responsibility for the content of this article rests with the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Carlander, AL.F., Gundestrup, A.K., Jansson, P.M. et al. Mesenchymal Stromal/Stem Cell Therapy Improves Salivary Flow Rate in Radiation-Induced Salivary Gland Hypofunction in Preclinical in vivo Models: A Systematic Review and Meta-Analysis. Stem Cell Rev and Rep 20, 1078–1092 (2024). https://doi.org/10.1007/s12015-024-10700-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-024-10700-y