Abstract
Background
It remains unclear whether conservative oxygen therapy (COT) or liberal oxygen therapy (LOT) is more beneficial to the clinical outcomes of intensive care unit (ICU) patients. We systematically reviewed the efficacy and safety of conservative versus liberal oxygen therapy for ICU patients.
Methods
We systematically searched PubMed, Embase, Web of Science, Scopus, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, MedRxiv, and BioRxiv for reports on randomized controlled trials (RCTs) that compared the effects of COT versus LOT on the clinical outcomes of ICU patients published in English before April 2024. The primary outcome was the mortality rate, secondary outcomes included ICU and hospital length of stay, days free from mechanical ventilation support (MVF), vasopressor-free time (VFT), and adverse events.
Results
In all, 13 RCTs involving 10,632 patients were included in analyses. Meta-analysis showed COT did not reduce mortality at 30-day (risk ratio [RR] = 1.01, 95% confidence interval [CI] 0.94 to 1.09, I2 = 42%, P = 0.78), 90-day (RR = 1.01, 95% CI 0.95 to 1.08, I2 = 9%, P = 0.69), or longest follow-up (RR = 1.00, 95% CI 0.95 to 1.06, I2 = 22%, P = 0.95) compared to LOT in ICU patients. In subgroup analyses, no significant difference was observed between the two groups in terms of the different ICU, baseline P/F, and actual PaO2. In addition, COT did not affect ICU length of stay, hospital length of stay, or VFT, it only affected MVF days.
Conclusions
COT did not reduce all-cause mortality in ICU patients. Further RCTs are urgently needed to confirm the impact of COT strategy on specific populations.
Similar content being viewed by others
Introduction
Oxygen is essential for human survival and plays a crucial role in a wide range of physiological processes [1]. Oxygen therapy is among the most common interventions in critical illnesses [2]. However, excessive oxygenation can enhance the production of reactive oxygen species, which can lead to oxidative damage to cellular components, including DNA, lipids, and proteins, ultimately resulting in cell death, producing inflammation that damages lung tissue further [3,4,5]. Although previous studies in volunteers and experimental models have investigated the detrimental effects of hyperoxia [6, 7], overuse of oxygen remains prevalent in intensive care unit (ICU) particularly among patients with hypoxemic respiratory failure [8,9,10].
Therefore, conservative oxygen therapy (COT) has been proposed in recent years to prevent excessive oxygen exposure to patients. In 2016, a single-center, open-label randomized controlled trial (RCT) indicated that a conservative protocol resulted in lower ICU mortality [11]. Two years later, the IOTA systematic review and meta-analysis suggested that a LOT strategy above a peripheral oxygen saturation (SpO2) range of 94–96% is associated with increased mortality; this result supported the conservative administration of oxygen therapy in acutely ill patients [12]. However, such findings were not supported by subsequent studies, which yielded conflicting results with a similar setup [13,14,15,16,17,18,19,20,21,22,23,24]. Despite recommendations for oxygenation targets [25, 26], the clinical efficacy of oxygenation strategies in critically ill patients remains uncertain.
As new trial data have been published recently [27, 28], we present an updated this review of this topic. In addition, due to the heterogeneity of patient characteristics in relation to different types of ICU, baseline oxygenation, and actual target oxygenation, it is difficult to interpret the results of these systematic reviews using pairwise meta-analysis [12,13,14,15,16,17,18,19,20,21,22,23,24]. It is essential to evaluate the target oxygenation and distinguish subpopulations who are likely to benefit from different oxygenation strategies.Accordingly, we focus on data from mixed ICUs vs. medical ICUs, different baseline P/Fratios (P/F), and actual target arterial partial pressure of oxygen (PaO2), and conduct a systematic review and meta-analysis of the RCTs. Specifically, we compared COT versus LOT in those subpopulations, to explore the optimal oxygenation targets in ICU patients.
Materials and methods
We designed and and wrote this report the study according to the Preferred Reporting Items for Systematic Reviews and Meta Analysis Protocols checklist (PRISMA-P) [29] (the checklist is presented in Additional file 1: S6) and the principles of the Cochrane Handbook including the Methodological Expectations of Cochrane Intervention Reviews standards [30, 31]. We used GRADEpro GDT to assess the certainty of the results [32, 33]. Trial sequential analysis (TSA) [34, 35] was performed by using TSA version 0.9.5.10 to further investigate the effects of COT and LOT, which was achieved by defining the required information size, using the O’Brien-Fleming boundaries to adjust the thresholds for statistical significance each time a trial was included, and introducing the threshold for futility. Our protocol of this systematic review was pre-registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42023434202).
Search strategy
Two authors (XYL and WT) independently searched PubMed, Embase, Web of Science, Scopus, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, MedRxiv, and BioRxiv before April 2024, focusing on adult ICU patients subjected to two different oxygenation strategies. The details of the search strategy are summarized in additional files to this report (Additional file 1: Search strategy). We searched RCTs in English for which full texts were available. All of the references listed in the included studies were reviewed, and the relevant studies were manually searched.
Inclusion and exclusion criteria
Eligible studies were those that met the following criteria: (1) the enrolled adult patients were admitted to an ICU; (2) patients were randomly assigned to a COT group or a LOT group; (3) oxygenation targets between the two groups were realized by PaO2, arterial oxygen saturation (SaO2), or SpO2 rather than constant fraction of inspired oxygen (FiO2), we did not determine a priori thresholds of oxygenation for the two groups to ensure inclusion of all relevant trials; and (4) mortality was included as a primary or secondary outcome. Exclusion criteria were as follows: (1) the patients did not meet screening criteria; (2) only included patients at risk for ischemia or hypoxic encephalopathy (including traumatic brain injury, stroke, myocardial infarction, and cardiac arrest) or who underwent surgery (including trauma and coronary artery bypass surgery) were included; and (3) the publication was not in English; was a conference reports, commentary, and reviews; and/or represented a redundant publication from a single study.
Outcomes and definition
The primary outcome of interest was 30 (including 28)-day mortality, 90-day mortality, and the longest follow-up mortality in each study.We performed sensitivity analyses according to the two different ICUs (mixed/medical). A mixed ICU was defined as a unit that included both medical and surgical patients, whereas a medical ICU was one that included medical patients. We also performed a subgroup analysis from different baseline P/F at enrollment (mild to moderate hypoxemia, P/F ≥ 150 mmHg; moderate to severe hypoxemia, P/F < 150 mmHg), and the actual PaO2 ( PaO2 in the COT group ≥ 80 mmHg, < 80 mmHg). The secondary outcomes were ICU length of stay, hospital length of stay, days free from mechanical ventilation support (MVF), vasopressor-free time (VFT), and adverse events.
Data extraction and quality assessment
Two investigators (XYL and WT) independently extracted and recorded the desired information from the included studies based on the Cochrane recommendations [28], consisting of the first author, year of publication, setting, country, sample size, intervention protocols, demographic and illness characteristics of patients, and study outcomes. Authors were contacted in cases of missing data or if the reporting format was not suitable for the meta-analysis (e.g., included the data of surgical patients and medical patients). Datas were extracted using the software (GetDataW) when presented in a figure in the trial, or in part from secondary analysis of other studies. Continuous datas were extracted as sample size and mean (standard deviation, SD) or median (inter quartile range, IQR) provided in the studies, with the conversion of medians to estimated mean (SD). Any discrepancies that arose were resolved by the involvement of a third author (BD or HJH).
To evaluate the quality of the eligible RCTs, we used the risk of bias tool recommended by the Cochrane Collaboration [29]. The potential sources of bias were rated according to the following items: sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other sources of bias. Besides, the quality of evidence was assessed according to the GRADE (Grading of Recommendations Assessment, Development and Evaluation) guidelines on the basis of study limitations, imprecision, inconsistency, indirectness and publication bias for the targeted outcomes [33]. Publication bias was evaluated by visually inspecting funnel plots.
Statistical analysis
Meta-analysis and forest plots were performed using the Cochrane systematic review software Review Manager (RevMan; version 5.4.1; The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark). Dichotomous outcomes are expressed as RRs with 95% CIs, while continuous outcomes are expressed as weighted MDs and 95% CIs, mean (SD) were estimated from median IQRs for further comparison. Heterogeneity was tested using I2 statistics. A fixed-effect model was applied when I2 < 50%, indicating insignificant heterogeneity, whereas a random-effects model was chosen for cases of significant heterogeneity (I2 > 50%). P < 0.05 was considered statistically significant. A relative risk reduction (RRR) of 20%, a type I error level of 5%, and a type II error level of 10% were used in TSA.
Results
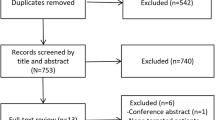
Study selection
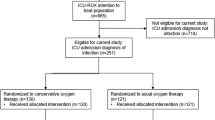
Following the search strategy, 21,367 records were imported for screening, and 11,712 records were screened by titles and abstracts after removal of duplicates or other reasons. Of these, 10,942 studies were excluded for either not being RCTs or not including adult patients. Furthermore, 68 reports could not be retrieved for evaluation. The remaining 702 studies underwent full-text assessment, of which 689 were excluded for the following reasons: inaccurate intervention, undesirable patient population, or presenting no outcomes of interest. Thus, 13 eligible RCTs [11, 27, 28, 36,37,38,39,40,41,42,43,44,45] were ultimately involved in the meta-analysis as depicted in Fig. 1. Two post-hoc subgroup analyses [46, 47] of the HOT-ICU trial [39] were also included for subgroup analyses.
Study description and quality assessment
The main characteristics of the 13 RCTs and 2 post-hoc subgroup analyses are summarized in Table 1, and further demographic details are shown in Additional file 1: Tables S1 and S2. All RCTs were performed in ICU; 9 were conducted in mixed ICU settings [11, 27, 36,37,38,39, 41,42,43] and 6 were conducted in medical ICU settings [28, 40, 44,45,46,47]. The mean baseline P/F varied among the included studies, being ≥ 150 mmHg in 8 studies [11, 27, 36, 38, 40, 42,43,44] and < 150 mmHg in 6 studies [28, 39, 41, 45,46,47]. The mean actual PaO2 levels in both COT and LOT group also varied among the included studies. In the COT group, it ranged from 61 to 87 mmHg, being ≥ 80 mmHg in 5 studies [11, 37, 38, 42, 43], and < 80 mmHg in 10 studies [27, 28, 36, 39,40,41, 44,45,46,47]. In the LOT group, it ranged from 76 to 115 mmHg in 15 studies [11, 27, 28, 36,37,38,39,40,41,42,43,44,45,46,47]. Regarding the difference in mortality, the rate was 5% lower in the COT group than in the LOT group in 3 studies [11, 37, 42], within 5% between the two groups in 8 studies [27, 28, 36, 38, 39, 43, 44, 46] and 5% higher in the COT group than in the LOT group in 4 studies [40, 41, 45, 47].
The results of quality assessment of the included studies are shown in Figure S1 (Additional file 1: Fig. S1). No selection bias was found in 13 studies, but high performance bias was found due to their unblinded designs. Symmetrical funnel plots of mortality rate showed no significant publication bias (Additional file 1: Fig. S2).
Outcomes
All 13 RCTs [11, 27, 28, 36,37,38,39,40,41,42,43,44,45] (10,632 patients) reported mortality outcomes: 4 reported 30-day mortality [11, 37, 44, 45]; 5 reported both 30- and 90-day [27, 38, 40,41,42] (and 180-day [38]) mortality; and 4 reported 90-day mortality [28, 36, 39, 43]. The mortality at the longest follow-up in the COT and LOT groups was 37.04% (1927 of 5202 patients) and 37.51% (1655 of 4412 patients), respectively, with no significant differences between the two groups (Fig. 2A). The results of the TSA was shown in Fig. 2B. The cumulative Z curve crossed the futility boundary but not crossed the conventional boundary, and 85.89% (9,614 of 11,194 patients) of the required information size was accrued. The results indicated that, when compared with LOT, COT did not reduce the relative risk of the longest follow-up mortality by 20% among ICU patients. The certainty of the evidence was very low (GRADE, Additional file 1: Fig. S3). Also, no significant differences were observed in the analysis of 30-day mortality [11, 27, 37, 38, 40,41,42, 44, 45] or 90-day mortality [27, 28, 36, 38,39,40,41,42,43] between the two groups (Additional file 1: Fig. S4, S5).
In subgroup analyses, there were no significant differences in mortality at any analyzed time point (30-day, 90-day, longest follow-up) between the two groups in terms of ICU admission type, different baseline P/F, or different actual PaO2 (Fig. 3; Additional file 1: Fig. S6, 7). Further details of the TSA results were shown in Additional file 1: Fig. S8–10.
No differences were found in terms of the ICU length of stay [11, 27, 36, 40, 42, 43, 45], length of hospital stay, [11, 27, 36, 40], or VFT days [36, 38, 42, 44] between the COT and LOT group, but MVF days [11, 27, 28, 36, 38, 42,43,44] was significant longer in the LOT group than in the COT group (Additional file 1: Fig. S11–13). The certainty of the evidence was low to very low (Additional file 1: Fig. S3).
Adverse events were reported in 7 RCTs [27, 28, 38, 39, 42,43,44], including organ failure, shock, infection, ICU-acquired weakness, seizure, and delirium (Additional file 1: Table S3). The incidence of adverse events was significantly lower in the COT group than in the LOT group. The results of TSA indicated that the improvement of COT could be considered conclusive with the available evidence (Additional file 1: Fig. S14). However, the certainty of the evidence was low (Additional file 1: Fig. S3). In the subgroup analyses, the incidence of adverse events in the COT group was significantly lower among the patients who enrolled in mixed ICU settings and with baseline P/F ≥ 150 mmHg. However, no differences were found between the two oxygenation strategies for patients enrolled in medical ICU settings and with baseline P/F < 150 mmHg (Fig. 4, Additional file 1: Fig. S13).
Discussion
In this systemic review and meta-analysis, we found that COT did not reduce the mortality rate relative to the LOT group in ICU patients; this was also true in terms of the different ICUs, baseline P/F, and actual PaO2 in the subgroup analyses. Some studies showed a slight trend of higher mortality in the COT group with actual PaO2 < 80 mmHg and in medical ICU settings. COT did not affect ICU length of stay, hospital length of stay, or VFT, only MVF days. The incidence of adverse events was significantly lower in the COT group (among patients enrolled in mixed ICU settings and with baseline P/F ratio ≥ 150 mmHg) than in the LOT group, but no differences were found between the two oxygenation strategies for patients enrolled in medical ICU settings and with baseline P/F < 150 mmHg.
Our review has several strengths. First, we included studies only involving ICU patients, and new high-quality RCTs were included [27, 28]. Second, we performed TSA with adjusted CIs in order to control for risk of random errors due to multiple outcomes, sparse data, and repetitive testing on accumulated data, to evaluate the benefits and harms of COT versus LOT in critically ill patients. We also contacted relevant trial authors if additional information was required. Third, to explore the robustness of our results and the influence of hypoxemia severity, ICU population and actual oxygenation on our primary outcome, we have performed the subgroup analyses according to ICU population, baseline oxygenation, and actual PaO2.
In this review, COT did not reduce mortality of ICU patients. In recent meta-analyses summarized in Additional file 1: Table S5 [12,13,14,15,16,17,18,19,20,21,22,23,24, 48], only two earlier reviews found that COT may result in a lower mortality rate. An IOTA meta-analysis [12] was conducted in both ICUs and ordinary care settings, considering all types of diseases, and it suggested that a LOT strategy above an SpO2 range of 94–96% was associated with increased mortality, but subgroup analyses revealed no significant differences in critical care patients. Another meta-analysis that included ICU patients in only four RCTs found that COT resulted in significantly lower mortality rate [48]. However, such findings have not been supported by any subsequent meta-analyses published after 2019 [13, 24]. Our systematic review including more RCTs further confirms these results. However, because blinding of participants and/or personnel is not possible, the the certainty of the evidence was low. Still, the TSA indicated that over 80% of the required information size was accrued, and evidence was able to assess the benefit or harm between the two groups.
No differences of mortality were found between two oxygenation strategies for patients enrolled in medical and mixed ICU settings. Compared to the previous meta-analyses [13, 24], we included more studies in the subgroup analysis. However, the TSA indicated that in most subgroups, the samples did not reach the required information size. We noticed that there was a difference in mortality of up to 5% between the two groups in some studies (Table 1). Interestingly, studies showing a trend of higher mortality in the COT group were mostly conducted in medical ICU settings [40, 41, 45, 47], and the main diagnoses of the included patients were medical diseases, mainly respiratory diseases (Additional file 1: Table S1). On the contrary, studies showing a trend of lower mortality in the COT group were all in mixed ICU settings [11, 37, 42]. We summarized the comorbidities of patients located in medical and mixed ICU and found that the incidence of cardiovascular, respiratory, and digestive diseases was significantly higher in medical ICU patients than that in mixed ICUs (Additional file 1: Table S4). It is reasonable to assume that the patients in medical ICUs may have had more severe gas-exchange impairments and refractory hypoxemia, requiring more oxygen. It may also be worth noting that the COT strategy avoids hyperoxemia but exposes patients to a higher risk of hypoxia, especially in these patients with more comorbidities [26]. Clinical trials comparing different oxygenation groups for these specific patient groups are needed; if possible, such studies should also incorporate stratification of important baseline risk factors (e.g., comorbidities).
In most including RCTs, SpO2 has been the primary parameter defining the target oxygenation range, but discrepancies sometimes exist between the targeted goals and the actual levels. Actually, PaO2 is superior to defining oxygenation target levels precisely and minimizing overlap between two groups [49]. Zhao et al. [17] performed a systematic review according to oxygenation goals, and found that different oxygenation goals do not lead to different mortalities in mechanically ventilated critical ill patients. Further, we performed the subgroup analysis based on the actual PaO2, and no differences of mortality were found between COT and LOT. However, we noticed a trend that (Table 1), the COT group with lower actual PaO2 (< 80 mmHg) may have a higher mortality rate than that of LOT group in some studies [40, 41, 45, 47]; while the COT group with higher PaO2 (≥ 80 mmHg) may have lower mortality in some studies [11, 37, 42], and the actual PaO2 was basically equal to the LOT group in some other studies (Table 1). As the normal range for PaO2 at sea level in healthy individuals is 80 to 100 mmHg [50], the COT strategy may not represent permissive hypoxia, which has not been well studied in adults. The observed degree of difference in mortality may have clinical significance, and thus more careful oxygen titration with “permissive hypoxia” should be considered in these patients until more robust evidence is available.
COT was not associated with any advantages in terms of ICU length of stay, hospital length of stay, or VFT compared to LOT, only MVF days. We believe that many factors contributed to these results, such as the primary diseases of patients admitted to different ICUs, the severity of baseline disease, and the treatment effects.
We also found that the incidence of adverse events in LOT was significantly higher among patients enrolled in mixed ICU settings and with a baseline P/F ≥ 150 mmHg than in COT. This is consistent with previous conclusions that higher oxygenation targets are associated with more adverse events [10]. However, no differences were found between the two oxygenation strategies for patients enrolled in medical ICU settings and with baseline P/F < 150 mmHg. This may also be due to the fact that these patients have more severe exchange impairments and refractory hypoxemia, where the adverse events are offset by the benefits of corrected hypoxia from oxygen therapy. However, due to the different definitions and the inadequate blinding of adverse events, more robust data are needed for a more compelling conclusion. We should also pay close attention to the microcirculation, long-term neurological function and others complications; new technological approaches, such as biomarkers, can be also considered in the future research.
There may be some implications for practice and future research. Given the presence of confounding factors in many existing RCTs, it remains of paramount importance to continue to conduct clinical trials, ideally comparing groups with a clinically relevant contrast between specific patient groups, such as according to the type and severity of disease of patients in the respiratory ICU; machine learning methods using data from these trials could also be utilized to build models for individual patients [51]. Meanwhile, the oxygenation strategies in all trials were grouped by PaO2, SpO2, or FiO2, all of which required manual adjustment during titration. New techniques, such as automated oxygen titration may better identify the suitable oxygenation target for a specific population in the future research [52]. Finally, adverse events are important signals for clinical practice guidelines; it may be necessary to take adverse events as primary or secondary outcomes, more robust data is needed for a compelling conclusion.
Some limitations of our review should be mentioned. First, the definitions of COT and LOT were not quite concordant among the studies assessed and the actual oxygenetions were also very different. Second, clinical heterogeneity among studies is a common concern. Third, inadequate blinding is often associated with performance bias. Finally, TSA indicated that the information size was insufficient for most outcomes, especially in most subgroups.
Conclusion
In conclusion, this systematic review and meta-analysis found that COT did not reduce all-cause mortality at 30-day, 90-day or longest follow-up of ICU patients. There was a trend, but without a statistical difference, showing that patients in the COT group with lower PaO2 had an increased mortality rate in medical ICU settings; further studies are needed to confirm our findings. COT was associated with a lower incidence of adverse events among patients enrolled in mixed ICU settings and with baseline P/F ≥ 150 mmHg; however, no differences were found between the two oxygenation strategies for patients enrolled in medical ICU settings and with baseline P/F < 150 mmHg.
Availability of data and materials
Not applicable.
Abbreviations
- COT:
-
Conservative oxygen therapy
- LOT:
-
Liberal oxygen therapy
- ICU:
-
Intensive care unit
- RCT:
-
Randomized controlled trial
- MVF:
-
Days free from mechanical ventilation support
- VFT:
-
Vasopressor-free time
- FiO2 :
-
Fraction of inspired oxygen
- PaO2 :
-
Arterial partial pressure of oxygen
- SaO2 :
-
Arterial oxygen saturation
- SpO2 :
-
Peripheral oxygen saturation
- P/F:
-
PaO2/FiO2 ratios
- RR:
-
Risk ratios
- CIs:
-
95% Confidence intervals
- MDs:
-
Mean differences
- SD:
-
Standard deviation
- IQRs:
-
Interquartile ranges
- TSA:
-
Trial sequential analysis
- RRR:
-
Relative risk reduction
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
References
West JB. Joseph Priestley, oxygen, and the enlightenment. Am J Physiol Lung Cell Mol Physiol. 2014;306(2):L111-119.
Helmerhorst HJ, Schultz MJ, van der Voort PH, de Jonge E, van Westerloo DJ. Bench-to-bedside review: the effects of hyperoxia during critical illness. Crit Care. 2015;19(1):284.
Crapo JD. Morphologic changes in pulmonary oxygen toxicity. Annu Rev Physiol. 1986;48:721–31.
Kallet RH, Matthay MA. Hyperoxic acute lung injury. Respir Care. 2013;58(1):123–41.
Singer M, Young PJ, Laffey JG, Asfar P, Taccone FS, et al. Dangers of hyperoxia. Crit Care. 2021;25(1):440.
Sackner MA, Landa J, Hirsch J, Zapata A. Pulmonary effects of oxygen breathing. A 6-hour study in normal men. Ann Intern Med. 1975;82(1):40–3.
Amarelle L, Quintela L, Hurtado J, Malacrida L. Hyperoxia and lungs: what we have learned from animal models. Front Med (Lausanne). 2021;8: 606678.
Itagaki T, Nakano Y, Okuda N, Izawa M, Onodera M, et al. Hyperoxemia in mechanically ventilated, critically ill subjects: incidence and related factors. Respir Care. 2015;60(3):335–40.
de Graaff AE, Dongelmans DA, Binnekade JM, de Jonge E. Clinicians’ response to hyperoxia in ventilated patients in a Dutch ICU depends on the level of FiO2. Intensive Care Med. 2011;37(1):46–51.
Eastwood G, Bellomo R, Bailey M, Taori G, Pilcher D, et al. Arterial oxygen tension and mortality in mechanically ventilated patients. Intensive Care Med. 2012;38(1):91–8.
Girardis M, Busani S, Damiani E, Donati A, Rinaldi L, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit: the oxygen-ICU randomized clinical trial. JAMA. 2016;316(15):1583–9.
Chu DK, Kim LH, Young PJ, Zamiri N, Almenawer SA, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391(10131):1693–705.
Barbateskovic M, Schjørring OL, Russo Krauss S, Jakobsen JC, Meyhoff CS, et al. Higher versus lower fraction of inspired oxygen or targets of arterial oxygenation for adults admitted to the intensive care unit. Cochrane Database Syst Rev. 2019;2019(11):CD012631.
Barbateskovic M, Schjørring OL, Krauss SR, Meyhoff CS, Jakobsen JC, et al. Higher vs lower oxygenation strategies in acutely ill adults: a systematic review with meta-analysis and trial sequential analysis. Chest. 2021;159(1):154–73.
Li L, Zhang Y, Wang P, Chong W, Hai Y, et al. Conservative versus liberal oxygen therapy for acutely ill medical patients: a systematic review and meta-analysis. Int J Nurs Stud. 2021;118: 103924.
Ni YN, Wang T, Liang BM, Liang ZA. The effect of conservative oxygen therapy in reducing mortality in critical care patients: a meta-analysis and trial sequential analysis. Front Med (Lausanne). 2021;8: 738418.
Zhao X, Xiao H, Dai F, Brodie D, Meng L. Classification and effectiveness of different oxygenation goals in mechanically ventilated critically ill patients: network meta-analysis of randomised controlled trials. Eur Respir J. 2021;58(3):2002928.
Chen XL, Zhang BL, Meng C, Huang HB, Du B. Conservative oxygen therapy for critically ill patients: a meta-analysis of randomized controlled trials. J Intensive Care. 2021;9(1):47.
Dong WH, Yan WQ, Chen Z. Effect of liberal or conservative oxygen therapy on the prognosis for mechanically ventilated intensive care unit patients: a meta-analysis. Sao Paulo Med J. 2022;140(3):463–73.
van der Wal LI, Grim CCA, Schultz MJ, de Jonge E, et al. Corrigendum to “Higher versus lower oxygenation strategies in the general intensive care unit population: a systematic review, meta-analysis and meta-regression of randomized controlled trials” [Journal of Critical Care, volume 72(2022) 154151]. J Crit Care. 2023;74: 154245.
Cumpstey AF, Oldman AH, Martin DS, Smith A, Grocott MPW. Oxygen targets during mechanical ventilation in the ICU: a systematic review and meta-analysis. Crit Care Explor. 2022;4(4): e0652.
Li X, Liu D, Liu C, Mao Z, Liu Y, et al. Conservative versus liberal oxygen therapy in relation to all-cause mortality among patients in the intensive care unit: a systematic review of randomized controlled trials with meta-analysis and trial sequential analysis. Med Intensiva (Engl Ed). 2023;47(2):73–83.
Crescioli E, Krejberg KU, Klitgaard TL, Nielsen FM, Barbateskovic M, et al. Long-term effects of lower versus higher oxygenation levels in adult ICU patients: a systematic review. Acta Anaesthesiol Scand. 2022;66(8):910–22.
Klitgaard TL, Schjørring OL, Nielsen FM, Meyhoff CS, Perner A, et al. Higher versus lower fractions of inspired oxygen or targets of arterial oxygenation for adults admitted to the intensive care unit. Cochrane Database Syst Rev. 2023;9(9):CD012631.
Siemieniuk RAC, Chu DK, Kim LH, Güell-Rous MR, Alhazzani W, et al. Oxygen therapy for acutely ill medical patients: a clinical practice guideline. BMJ. 2018;363: k4169.
O’Driscoll BR, Howard LS, Earis J, Mak V. BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax. 2017;72(Suppl 1):ii1–90.
van der Wal LI, Grim CCA, Del Prado MR, van Westerloo DJ, Boerma EC, et al. Conservative versus liberal oxygenation targets in intensive care unit patients (ICONIC): a randomized clinical trial. Am J Respir Crit Care Med. 2023;208(7):770–9.
Nielsen FM, Klitgaard TL, Siegemund M, Laake JH, Thormar KM, HOT-COVID Trial Group, et al. Lower vs higher oxygenation target and days alive without life support in COVID-19: The HOT-COVID randomized clinical trial. JAMA. 2024. https://doi.org/10.1001/jama.2024.2934.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, eds. Cochrane Handbook for Systematic Reviews of Interventions version 6.2. Cochrane; 2021. www.training.cochrane.org/handbook. Accessed on Feb 2021.
Higgins JPTLT, Chandler J, Tovey D, Thomas J, Flemyng E, Churchill R. Methodological expectations of cochrane intervention reviews. Cochrane. 2021. https://community.cochrane.org/sites/default/files/uploads/MECIR-February-2021.pdf. Accessed Oct 2020.
GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. www.gradepro.org. Accessed 25 Mar 2019.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, GRADE Working Group, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Mascha EJ. Alpha, beta, meta: guidelines for assessing power and type I error in meta-analyses. Anesth Analg. 2015;121(6):1430–3.
TSA 2011 [Computer program]Trial sequential analysis. Version 0.9 Beta. Copenhagen: Copenhagen Trial Unit. 2011. www.ctu.dk/tsa/downloads.aspx.
Panwar R, Hardie M, Bellomo R, Barrot L, Eastwood GM, et al. Conservative versus liberal oxygenation targets for mechanically ventilated patients. A pilot multicenter randomized controlled trial. Am J Respir Crit Care Med. 2016;193(1):43–51.
Yang X, Shang Y, Yuan S. Low versus high pulse oxygen saturation directed oxygen therapy in critically ill patients: a randomized controlled pilot study. J Thorac Dis. 2019;11(10):4234–40.
ICU-ROX Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group, Mackle D, Bellomo R, Bailey M, Beasley R, Deane A, et al. ICU-ROX Investigators the Australian and New Zealand Intensive Care Society Clinical Trials Group. Conservative oxygen therapy during mechanical ventilation in the ICU. N Engl J Med. 2020;382(11):989–98.
Schjørring OL, Klitgaard TL, Perner A, Wetterslev J, Lange T, et al. Lower or higher oxygenation targets for acute hypoxemic respiratory failure. N Engl J Med. 2021;384(14):1301–11.
Martin DS, McNeil M, Brew-Graves C, Filipe H, O’Driscoll R, et al. A feasibility randomised controlled trial of targeted oxygen therapy in mechanically ventilated critically ill patients. J Intensive Care Soc. 2021;22(4):280–7.
Barrot L, Asfar P, Mauny F, Montini F, Badie J, et al. Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med. 2020;382(11):999–1008.
Asfar P, Schortgen F, Boisramé-Helms J, Charpentier J, Guérot E, et al. Hyperoxia and hypertonic saline in patients with septic shock (HYPERS2S): a two-by-two factorial, multicentre, randomised, clinical trial. Lancet Respir Med. 2017;5(3):180–90.
Gelissen H, de Grooth HJ, Smulders Y, Wils EJ, de Ruijter W, et al. Effect of low-normal vs high-normal oxygenation targets on organ dysfunction in critically ill patients: a randomized clinical trial. JAMA. 2021;326(10):940–8.
Semler MW, Casey JD, Lloyd BD, Hastings PG, Hays MA, et al. Oxygen-saturation targets for critically ill adults receiving mechanical ventilation. N Engl J Med. 2022;387(19):1759–69.
Nafae RM, Shouman W, Abdelmoneam SH, Shehata SM. Conservative versus conventional oxygen therapy in type I acute respiratory failure patients in respiratory intensive care unit. Zagazig University. Monaldi Arch Chest Dis. 2023. https://doi.org/10.4081/monaldi.2023.2536.
Rasmussen BS, Klitgaard TL, Perner A, Brand BA, Hildebrandt T, et al. Oxygenation targets in ICU patients with COVID-19: a post hoc subgroup analyses of the HOT-ICU trial. Acta Anaesthesiol Scand. 2022;66(1):76–84.
Klitgaard TL, Schjørring OL, Severinsen MT, Perner A, Rasmussen BS. Lower versus higher oxygenation targets in ICU patients with haematological malignancy—insights from the HOT-ICU trial. BJA Open. 2022;4: 100090.
Hirase T, Ruff ES, Ratnani I, Surani SR. Impact of conservative versus conventional oxygenation on outcomes of patients in intensive care units: a systematic review and meta-analysis. Cureus. 2019;11(9): e5662.
Schjørring OL, Rasmussen BS. The paramount parameter: arterial oxygen tension versus arterial oxygen saturation as target in trials on oxygenation in intensive care. Crit Care. 2018;22(1):324.
Kratz A, Ferraro M, Sluss PM, Lewandrowski KB. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Laboratory reference values. N Engl J Med. 2004;351(15):1548–63.
DeMasi SC, Self WH, Semler MW. Oxygen targets and the future of critical care clinical research. Am J Respir Crit Care Med. 2023;208(7):746–8.
Roca O, Caritg O, Santafé M, Ramos FJ, Pacheco A, et al. Closed-loop oxygen control improves oxygen therapy in acute hypoxemic respiratory failure patients under high flow nasal oxygen: a randomized cross-over study (the HILOOP study). Crit Care. 2022;26(1):108.
Acknowledgements
The authors are grateful for all the participants in this study. We also would like to thank some authors for their data during the preparation of this updated systematic review.
Funding
This meta-analysis was funded by the China Postdoctoral Science Foundation (Certificate number: 2023M733905).
Author information
Authors and Affiliations
Contributions
WT is the guarantor of the manuscript and takes responsibility for the content (including data and analysis). Study design, literature search –XYL/BD/HJH/WT. Data collection/interpretation/analysis –XYL/BD/HJH/WT/HWZ/WW/JK. Manuscript writing/revisions–XYL/BD/HJH/WT/HWZ/WW/JK. Drafting of figures–XYL/BD/HJH/WT.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Search strategy.
Table S1. Demographic details of the included studies. Table S2. Primary diagnosis or comorbidities of the included studies. Table S3. Comorbidities of the included studies in medical ICU and Mixed ICU. Table S4. Adverse events of the included studies. Figure S1. Assessment on the risk of bias for the included RCTs. Figure S2. Funnel plot of mortality at the longest follow-up for the included studies. Figure S3. The GRADE assessment of the certainty of the evidence. Figure S4. Mortality at 30 days and TSA of the the included studies. Figure S5. Mortality at 90 days and TSA of the the included studies. Figure S6. Subgroup analysis of 30-day mortality for the included studies. Figure S7. Subgroup analysis of 90-day mortality for the included studies. Figure S8. TSA of 30-day mortality (subgroup analysis) for the included studies. Figure S9. TSA of 90-day mortality (subgroup analysis) for the included studies. Figure S10. TSA of mortality at the longest follow-up (subgroup analysis) for the included studies. Figure S11. Secondary outcomes for the included studies. Figure S12. Funnel plot of secondary outcomes for the included studies. Figure S13. TSA of secondary outcomes for the included studies. Figure S14. TSA of adverse evevts for the included studies. Figure S15. TSA of adverse evevts (subgroup analysis) for the included studies. Table S5. Meta-analysis of different oxygenation targets in recent years. Table S6. PRISMA2020 checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Xy., Dai, B., Hou, Hj. et al. Conservative versus liberal oxygen therapy for intensive care unit patients: meta-analysis of randomized controlled trials. Ann. Intensive Care 14, 68 (2024). https://doi.org/10.1186/s13613-024-01300-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-024-01300-7