Abstract
Background
Noninvasive monitoring of maximal inspiratory and expiratory flows (MIF and MEF, respectively) by electrical impedance tomography (EIT) might enable early recognition of changes in the mechanical properties of the respiratory system due to new conditions or in response to treatments. We aimed to validate EIT-based measures of MIF and MEF against spirometry in intubated hypoxemic patients during controlled ventilation and spontaneous breathing. Moreover, regional distribution of maximal airflows might interact with lung pathology and increase the risk of additional ventilation injury. Thus, we also aimed to describe the effects of mechanical ventilation settings on regional MIF and MEF.
Methods
We performed a new analysis of data from two prospective, randomized, crossover studies. We included intubated patients admitted to the intensive care unit with acute hypoxemic respiratory failure (AHRF) and acute respiratory distress syndrome (ARDS) undergoing pressure support ventilation (PSV, n = 10) and volume-controlled ventilation (VCV, n = 20). We measured MIF and MEF by spirometry and EIT during six different combinations of ventilation settings: higher vs. lower support during PSV and higher vs. lower positive end-expiratory pressure (PEEP) during both PSV and VCV. Regional airflows were assessed by EIT in dependent and non-dependent lung regions, too.
Results
MIF and MEF measured by EIT were tightly correlated with those measured by spirometry during all conditions (range of R2 0.629–0.776 and R2 0.606–0.772, respectively, p < 0.05 for all), with clinically acceptable limits of agreement. Higher PEEP significantly improved homogeneity in the regional distribution of MIF and MEF during volume-controlled ventilation, by increasing airflows in the dependent lung regions and lowering them in the non-dependent ones.
Conclusions
EIT provides accurate noninvasive monitoring of MIF and MEF. The present study also generates the hypothesis that EIT could guide PSV and PEEP settings aimed to increase homogeneity of distending and deflating regional airflows.
Similar content being viewed by others
Introduction
Electrical impedance tomography (EIT) is a noninvasive, bedside, radiation-free, dynamic lung imaging technique. EIT provides intrathoracic maps of lung impedance changes referenced to a baseline (i.e., the end-expiratory lung volume from previous breath) every 20–50 ms [1]. Intrathoracic impedance changes measured by EIT are linearly correlated with global and regional tidal volume, and the correlation is maintained at increasing positive end-expiratory pressure (PEEP) levels [2]. Thus, EIT yields noninvasive bedside continuous measure of regional lung volume changes during inspiration and expiration.
Inspiratory and expiratory airflows correspond to the velocity of lung volume changes over time. In intubated patients, they are traditionally measured through a spirometer applied to the ventilator circuit before the endotracheal tube or within the ventilator. Global maximal inspiratory and expiratory flows (MIF and MEF, respectively) measured by standard spirometry depend on the mechanical properties of the respiratory system (namely, lung compliance and airway resistance) [3]. Therefore, monitoring of MIF and MEF could be useful to guide ventilation settings (e.g., by selecting the positive pressure level associated with improved mechanics) and/or to evaluate the efficacy of pharmacologic treatments (e.g., increased MIF and/or MEF after bronchodilator drugs) [4]. However, spirometry only yields global measures of MIF and MEF, while heterogeneous distribution of altered lung mechanics is a hallmark of acute hypoxemic respiratory failure (AHRF) and acute respiratory distress syndrome (ARDS) [5]. Alveolar damage leads to collapse of lung units tightly bordering normal-, partial- and over-inflated units, potentially yielding imbalances in regional MIF and MEF values. Such imbalances can increase the risk of ventilator-induced lung injury (VILI) through multiple mechanisms [6], while settings obtaining more homogenous regional flows might reduce it. External classic spirometry sometimes leads to altered respiratory patterns and inaccurate measures, too [7]. Thus, a noninvasive bedside dynamic method to measure global and regional MIF and MEF values would be a valuable addition in understanding AHRF and ARDS patients’ pathophysiology and to guide personalized treatments.
In the present study, following preliminary data obtained in animal model [8], we aimed to validate in intubated AHRF and ARDS patients undergoing controlled ventilation and spontaneous breathing EIT-based measures of global MIF and MEF against standard spirometry. Moreover, we explored the effects of higher vs. lower PEEP and pressure support levels on regional flows; our hypothesis is that higher PEEP and lower pressure support could yield more homogenous distribution of regional MIF and MEF.
Materials and methods
Study population
We performed a new analysis of data collected during two prospective randomized crossover studies: in the first (pressure support ventilation (PSV) study) [9], ten intubated patients recovering from ARDS [10], lightly sedated (RASS − 2/0), undergoing PSV and admitted to the intensive care unit (ICU) of the university-affiliated San Gerardo Hospital, Monza, Italy, were enrolled; and in the second (volume-controlled ventilation (VCV) study) [11], twenty intubated, deeply sedated and paralyzed patients with AHRF (i.e., PaO2/FiO2 ≤ 300, PEEP ≥ 5 cmH2O, acute onset, no cardiac failure) or ARDS admitted to the same ICU were enrolled. The ethical committee of San Gerardo Hospital, Monza, Italy, approved the studies, and informed consent was obtained following local regulations. Additional details on the inclusion and exclusion criteria for the two studies are provided in an online data supplement (Additional file 1).
Demographic data collection
We collected sex, age, Simplified Acute Physiology Score II values, etiology, diagnosis and severity of ARDS, days on mechanical ventilation before study enrollment for each patient. In-hospital mortality was recorded, too.
EIT and ventilation monitoring
In each patient, EIT-dedicated belt, containing 16 equally spaced electrodes, was placed around the thorax at the fifth or sixth intercostal space and connected to a commercial EIT monitor (PulmoVista 500, Dräger Medical GmbH, Lübeck, Germany). During all study phases, EIT data were generated by application of small alternate electrical currents rotating around patient’s thorax, continuously recorded at 20 Hz and stored for offline analysis, as previously described [12]. Synchronized to EIT tracings, airway pressure and airflows from the mechanical ventilator were continuously recorded.
Interventions
More details on the two protocols can be found in the online data supplement (Additional file 1).
Briefly, in the PSV study, patients underwent the following crossover randomized steps, each lasting 20 min:
-
1.
Low support at clinical PEEP (PSVlow) vs. higher support at clinical PEEP (PSVhigh);
-
2.
Clinical support at low PEEP (PSV-PEEPlow) vs. clinical support at higher PEEP (PSV-PEEPhigh).
In the VCV study, instead, the following phases were performed in crossover randomized order, each lasting 20 min:
-
1.
Protective VCV at low PEEP (VCV-PEEPlow) vs. protective VCV at clinical PEEP + 5 cmH2O (VCV-PEEPhigh).
EIT and ventilation data
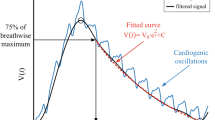
From offline analysis of the EIT tracings obtained during the last minutes of each phase (analysis of ten breaths), we measured global and regional (same-size dependent and non-dependent lung regions) noninvasive airflows waveform, as previously described [8]. Briefly, instantaneous global and regional inspiratory and expiratory airflows were measured as variations of global and regional impedance measured every 50 ms, multiplied by the tidal volume/tidal impedance ratio from the same study phase and divided by 50 ms. EIT airflow data were then transformed from mL/msec to L/min (Fig. 1), and the maximum EIT-derived global and regional MIF and MEF (MIFglob, MIFnon-dep and MIFdep; MEFglob, MEFnon-dep and MEFdep, respectively) were identified and the value averaged over 5–10 consecutive respiratory cycles.
Airflow waveforms measured by spirometer (red line) and electrical impedance tomography (EIT) (blue line) in two representative patients during pressure support ventilation (left) and volume-controlled ventilation (right). Note the correspondence between peak values by the two methods, with only modest underestimation by EIT
Regional index of flow homogeneity for both MIF and MEF was then calculated as the ratio between regional flow in the non-dependent and dependent regions (i.e. MIFnon-dep/dep and MEFnon-dep/dep). Values nearer to 1 unit indicate more homogenous distribution of regional airflows.
At the same time points of EIT data analysis, waveforms from the ventilator spirometer were analyzed to measure global MIF and MEF (MIFspiro and MEFspiro, respectively) and the value averaged over ten consecutive respiratory cycles. In one patient from the PSV study, technical issues with stored recordings prevented accurate measure of MIFspiro and MEFspiro.
Of note, in the present study, the terms MIF and MEF indicated the maximum inspiratory and expiratory flows measured under standardized settings in intubated patients undergoing PSV and VCV at different PEEP levels. In classic physiology, instead, MIF and MEF are measured during volitional maximum efforts. Indeed, during VCV, we did not perform additional volitional maneuvers for measuring MIF and MEF but rather compared airflows measured by EIT under standardized settings. Finally, expiratory flow is usually reported as negative value, but for the sake of clarity, in tables and results we expressed it as absolute values.
Finally, at the same time points, Global Inhomogeneity Index (GI) of the distribution of regional tidal volume was calculated as previously described [13].
Statistical analysis
Normal distribution was tested by the Shapiro–Wilk test. Data are presented as the mean ± standard deviation (SD) or median and interquartile range [IQR] for continuous variables, as appropriate. Absolute or relative frequencies (%) are used for categorical variables. Comparisons between two groups of normally distributed variables were performed by repeated-measure t test, while nonnormally distributed variables were compared by Wilcoxon signed rank test. Differences in categorized variables were assessed using the Chi-square test or the Fisher’s exact test, as appropriate. Association between MIF and MEF obtained by EIT and spirometry was assessed by linear regression. Agreement between measures of MIF and MEF assessed by EIT and spirometry was assessed by Bland–Altman plots. A level of p < 0.05 (two-tailed) was considered as statistically significant. Statistical analyses were performed by using Sigma-Plot 12.0 (Systat Software Inc., San Jose, CA, USA).
Results
Patients’ characteristics and mechanical ventilation settings
Patients’ characteristics are listed in Table 1: patients were relatively young and quite severe, with short delay between intubation and enrollment of this study (early AHRF and ARDS). Patients with ARDS on the day of the study were 5 in the PSV study vs. 8 in the VCV study (50% vs. 40%, p = 0.602) but PaO2/FiO2 and number of quadrants involved were more severe in the VCV study group (Table 1).
In the PSV study, lower support (PSVlow) was 3 ± 3 cmH2O while PSVhigh was 12 ± 3 cmH2O (p < 0.0001), both applied at clinical PEEP level of 7 ± 2 cmH2O. Tidal volume increased between the two phases (6.8 [5.2–8.2] mL/kg vs 8.2 [6.5–12.3] mL/kg, p = 0.005).
In the same study, lower PEEP (PSV-PEEPlow) level was 7 ± 2 cmH2O, while PSV-PEEPhigh was 12 ± 2 cmH2O (p < 0.0001), both implemented with clinical support of 8 ± 5 cmH2O. Tidal volume remained stable over these two phases (8.2 [6.7–10.2] mL/kg vs. 7.8 [6.4–10.7] mL/kg, p = 0.475).
Finally, in the VCV study, lower PEEP during the VCV-PEEPlow phase was 7 [7–8] cmH2O, while VCV-PEEPhigh was 12 [12–13] cmH2O (p < 0.001), both applied with protective tidal volume (7.0 [6.0–7.3] mL/kg vs. 6.8 [6.0–7.2] mL/kg; p = 0.94) and constant respiratory rate (18 [16–23] bpm).
Validation of EIT-based MIFglob vs. MIFspiro and MEFglob vs. MEFspiro
By pooling data from all six phases of both studies (n = 76 for each correlation), both MIFglob and MEFglob were tightly correlated with MIFspiro and MEFspiro (MIFglob = 0.8 MIFspiro + 2.0, R2 = 0.709 and p < 0.0001; MEFglob = 0.6 MEFspiro + 10.7, R2 = 0.611 and p < 0.0001) (Figs. 1 and 2) with clinically acceptable limits of agreement (mean bias for MIF = − 4.4 ± 4.7 L/min and limits of agreement − 13.6 to 4.8 L/min; mean bias for MEF = − 1.9 ± 5.1 L/min and limits of agreement − 11.9 to 8.1 L/min) (Fig. 2).
Regressions and Bland–Altman plots reporting specific results from each step of both studies (six conditions, 12 linear regressions and 12 Bland–Altman plots) can be found in the supplemental data (Additional file 1). Briefly, R2 values ranged between 0.606 and 0.776, all showing statistically significant correlations. Limits of agreement ranged between − 18.5 and 10.8 L/min, thus being clinically acceptable. Mean differences showed slightly lower values of MIFglob and MEFglob vs. spirometry data, except for differences between MEFglob and MEFspiro in the PSVlow and PSV-PEEPlow phases when a slight overestimation was observed.
Effects of higher vs. lower pressure support and PEEP on regional homogeneity of maximal airflows
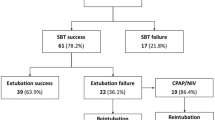
The effect of lower pressure support on the homogeneity of regional distribution of maximal inspiratory and expiratory airflows was not statically significant (Fig. 3), in comparison with higher support (Table 2).
Lower levels of pressure support improved homogeneity of regional maximal flow distribution both during inspiration and expiration in comparison with higher support (PSVlow vs. PSVhigh) (a); higher positive end-expiratory pressure level led to an improvement in maximal inspiratory and expiratory flows (MIF and MEF) homogeneity both during pressure support ventilation (PSV-PEEPhigh vs. PSV-PEEPlow) (b) and volume-controlled ventilation (VCV-PEEPhigh vs. VCV-PEEPlow); (c) dashed line represents perfect homogeneity
Application of higher PEEP improved maximal airflows homogeneity, albeit nonsignificantly, in the PSV study (Fig. 3), while the improvement was more consistent and highly significant in patients undergoing VCV. Higher PEEP during VCV increased airflows homogeneity by obtaining significantly higher MIF and MEF in the dependent lung regions and lowering them in the non-dependent ones.
GI index for regional tidal volume was significantly reduced only by higher levels of PEEP, both during PSV and VCV (Table 2). Interestingly, flow homogeneity was not correlated with the GI index (MIF homogeneity and GI, R2 = 0.018, p = 0.236; MEF homogeneity and GI: R2 = 0.017, p = 0.253).
By pooling data from all six phases of both studies (n = 80 for each correlation), regional MIF and MEF values were correlated with regional tidal volume (Vt) (Additional file 1: Figure S7), with R2 = 0.691 for MIFnon-dep vs. Vtnon-dep; R2 = 0.585 for MIFdep vs. Vtdep; R2 = 0.514 for MEFnon-dep vs. Vtnon-dep and R2 = 0.508 for MEFdep vs. Vtdep (p < 0.001 for all).
Discussion
Study main findings can be summarized as follows: EIT may represent an accurate method to continuously monitor global maximal inspiratory and expiratory flows at the bedside, both during assisted spontaneous breathing and controlled ventilation; regional homogeneity of maximal airflows distribution might be enhanced by higher PEEP during VCV.
In the present study, we compared measures of maximal inspiratory and expiratory flows obtained by standard spirometry integrated in the ICU ventilator vs. a noninvasive method based on EIT monitoring in intubated hypoxemic patients undergoing both assisted and controlled ventilation. Spirometry represents the current clinical standard to monitor MIF and MEF [14] but it has limitations, especially when applied to patients undergoing noninvasive ventilation via face mask for the risk of air leaks. Moreover, spirometry cannot be performed in patients undergoing support by high-flow nasal cannula [15] because it would interrupt treatment by sealing the nares and it would interfere with normal breathing pattern by using a mouthpiece. We showed tight correlations between the two methods and clinically acceptable limits of agreement. Our findings in hypoxemic patients are in line with those reported by Bodenstein et al. [8] in healthy and lung lavage pigs ventilated in pressure-controlled ventilation mode. Like data coming from animals, we also showed that EIT modestly underestimates airflows values. This might relate to the different site where the spirometer and the EIT measure airflows: the first lies within the ventilator while EIT conceptually performs spirometry within the lungs. Thus, the airflows measured by the spirometer and EIT might effectively differ, with EIT potentially assessing the physiology of the distal airways, where broncho-constriction/dilation takes place. We showed tight correlations between MIF and MEF measured by EIT vs. spirometry also during pressure support ventilation: this was not assessed in the animal study by Bodenstein et al. [8], and given the recent interest in promoting protective spontaneous breathing in hypoxemic patients [16], our data might have increased the clinical relevance of airflows monitoring by EIT. Considered altogether, our and previous data suggest that EIT might represent a valuable addition to advanced respiratory monitoring of hypoxemic patients, yielding bedside noninvasive continuous assessment of airflows. This might be particularly relevant to understand patients’ severity, guide noninvasive support and verify the effects of therapy. Indeed, airflows measured by EIT have already been previously reported in non-intubated patients with chronic obstructive pulmonary disease (COPD) [17, 18], asthma [4] and cystic fibrosis [19] to stratify the degree of lung disease and to assess the response to diagnostic tests or to bronchodilator therapies. Finally, preliminary results showed that, in spontaneously breathing patients supported by Nasal High Flow, noninvasive regional MIF and MEF measured by EIT might be of relevance to detect reduced respiratory effort and improved mechanics, potentially decreasing the risk of patient self-inflicted lung injury (P-SILI) [20]. However, in the absence of appropriate calibration, during Nasal High Flow, EIT-based measure of airflows could only be assessed as changes from a given baseline.
In addition to accurate measure of global MIF and MEF, we showed that EIT can detect changes in regional airflows induced by different ventilation settings. This was not explored in the previous study by Bodenstein et al. [8] in animals with lung injury. Inhomogeneity in the spatial distribution of lung damage is a hallmark of AHRF and ARDS, due to gravitational distribution of lung edema, local intensity of inflammation and occlusion of segmental bronchi by secretions [21]. Moreover, interaction between mechanical ventilation and lung heterogeneity has been hypothesized as a major determinant of ventilation-induced lung injury (VILI), even in the presence of protective recommended settings. To this end, the role of airflows in inducing VILI has been largely neglected [22]. In the present study, we described that, during VCV, higher level of PEEP yielded more homogenous maximal airflows distribution between non-dependent and dependent lung regions. During PSV, higher PEEP ameliorated homogeneity but by less significant extent, maybe because of small sample size or less severe population. Anyhow, these results might represent a new specific physiological benefit for the lungs of hypoxemic patients, for a few different reasons: increased MIF and MEF in the dorsal lung could indicate lower resistance due to stenting of airway closure [23, 24]; reduced MIF and MEF in the non-dependent lung could imply lower risks of regional cyclic inspiratory–expiratory hyper-stretch [25, 26]; and more balanced velocity of dependent and non-dependent airflows could reduce the cyclic stress of mid-lung structures at the interface between the two regions [27]. The mechanisms through which lower support and higher PEEP improved regional homogeneity of airflows distribution likely differed (enhanced contraction of the dependent region of the diaphragm vs. higher inflating pressure at end expiration) but both finally led to increased regional transpulmonary pressure in the dependent compressed lung [28,29,30]. We previously showed that higher PEEP and lower levels of PSV lead to more homogenous tidal volume distribution in the lungs [9, 11]. Although regional tidal volume and maximal flows were somehow correlated in our patients, previous studies showed that flows could have specific pathophysiologic significance on the risk of VILI, even in the presence of constant tidal volume [25, 31]. Moreover, modified ventilation settings might not yield the same effects on regional flows and volumes. For example, if PEEP is increased but it remains below the airway opening threshold, maximal inspiratory flow could increase due to the higher pressure gradient while regional tidal volume might be only minimally affected as it mostly depends from regional compliance. Our data might suggest that targeting more homogenous distribution of regional airflows could represent another sensitive method to titrate personalized ventilation settings which deserves further scrutiny.
Our study has relevant limitations. First, we performed a new analysis of data coming from two prospective randomized crossover physiological studies aimed at exploring the effects of pressure support on tidal volume distribution and at validating EIT-based measure of end-expiratory lung volume change against the helium dilution technique. Hence, power analysis was not specifically performed to explore differences in regional airflows during different ventilation settings. Low number of patients might also explain lack of statistical significance in some of the study comparisons. Second, patients’ population (i.e. patients with AHRF and ARDS) was enrolled based on a reasonable clinical definition but this might have introduced heterogeneity in terms of lung disease severity and regional lung mechanics. Third, EIT does not image the whole lung, while spirometry measures airflows coming from all lung regions. However, as tidal volume measured by EIT is validated against imaging methods covering the whole lung [30], the same correlation could be inferred for airflows. Fourth, we explored relatively narrow and low ranges of pressure support and PEEP, but these might represent more closely current clinical practice. Fifth, classically, MIF and MEF are volitional maneuvers, highly influenced by the cooperation of the patient. In the present study, instead, we assessed MIF and MEF under standardized settings of PSV and VCV to increase clinical significance for intubated and sedated ICU patients. Further studies should be performed to verify whether the presented correlations between EIT and spirometry remain valid in awake, non-intubated patients.
Conclusions
In intubated patients with AHRF and ARDS undergoing controlled ventilation and spontaneous breathing, maximal inspiratory and expiratory flows can be measured accurately by EIT. This is an exploratory study, and further studies need to be performed to validate airflows measured by EIT. Moreover, higher PEEP yields higher regional inspiratory and expiratory airflows in the dorsal lung probably through improvement in regional mechanics and eventually leads to more homogenous distribution of lung-distending and -deflating airflows in controlled models. EIT might represent a useful method for noninvasive assessment of global and regional airflows. The use of EIT as a dynamic tool to measure regional dynamic mechanical behavior and guide personalized treatments could be the object of future studies.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- AHRF:
-
acute hypoxemic respiratory failure
- ARDS:
-
acute respiratory distress syndrome
- EIT:
-
electrical impedance tomography
- ICU:
-
intensive care unit
- MEF:
-
maximal expiratory flow
- PEEP:
-
positive end-expiratory pressure
- MIF:
-
maximal inspiratory flow
- PSV:
-
pressure support ventilation
- SD:
-
standard deviation
- IQR:
-
interquartile range
- VCV:
-
volume-controlled ventilation
- VILI:
-
ventilation-induced lung injury
- GI index:
-
global inhomogeneity index
- P-SILI:
-
patients’ self-induced lung injury
References
Mauri T, Mercat A, Grasselli G. What’s new in electrical impedance tomography. Intensive Care Med. 2018;1:1. https://doi.org/10.1007/s00134-018-5398-z (Epub ahead of print).
Bikker IG, Leonhardt S, Bakker J, et al. Lung volume calculated from electrical impedance tomography in ICU patients at different PEEP levels. Intensive Care Med. 2009;35(8):1362–7.
Chen L, Del Sorbo L, Grieco DL, et al. Airway closure in acute respiratory distress syndrome: an underestimated and misinterpreted phenomenon. Am J Respir Crit Care Med. 2018;197(1):132–6.
Frerichs I, Zhao Z, Becher T, et al. Regional lung function determined by electrical impedance tomography during bronchodilator reversibility testing in patients with asthma. Physiol Meas. 2016;37(6):698–712.
Cressoni M, Cadringher P, Chiurazzi C, et al. Lung inhomogeneity in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2014;189(2):149–58.
Wolf GK, Gómez-Laberge C, Rettig JS, et al. Mechanical ventilation guided by electrical impedance tomography in experimental acute lung injury. Crit Care Med. 2013;41(5):1296–304.
Gilbert R, Auchincloss JH Jr, Brodsky J, et al. Changes in tidal volume, frequency, and ventilation induced by their measurement. J Appl Physiol. 1972;33(2):252–4.
Bodenstein M, Boehme S, Bierschock S, et al. Determination of respiratory gas flow by electrical impedance tomography in an animal model of mechanical ventilation. BMC Pulm Med. 2014;14:73.
Mauri T, Bellani G, Confalonieri A, et al. Topographic distribution of tidal ventilation in acute respiratory distress syndrome: effects of positive end-expiratory pressure and pressure support. Crit Care Med. 2013;41(7):1664–73.
The ARDS Definition Task Force. Acute respiratory distress syndrome. The Berlin definition. JAMA. 2012;307(23):2526–33.
Mauri T, Eronia N, Turrini C, et al. Bedside assessment of the effects of positive end-expiratory pressure on lung inflation and recruitment by the helium dilution technique and electrical impedance tomography. Intensive Care Med. 2016;42(10):1576–87.
Mauri T, Eronia N, Abbruzzese C, et al. Effects of sigh on regional lung strain and ventilation heterogeneity in acute respiratory failure patients undergoing assisted mechanical ventilation. Crit Care Med. 2015;43(9):1823–31.
Zhao Z, Möller K, Steinmann D, et al. Evaluation of an electrical impedance tomography-based Global Inhomogeneity Index for pulmonary ventilation distribution. Intensive Care Med. 2009;35(11):1900–6.
Miller MR, Hankinson J, Brusasco V, et al. ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38.
Mauri T, Alban L, Turrini C, et al. Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med. 2017;43(10):1453–63.
Mauri T, Cambiaghi B, Spinelli E, et al. Spontaneous breathing: a double-edged sword to handle with care. Ann Transl Med. 2017;5(14):292.
Vogt B, Pulletz S, Elke G, et al. Spatial and temporal heterogeneity of regional lung ventilation determined by electrical impedance tomography during pulmonary function testing. J Appl Physiol. 2012;113(7):1154–61.
Vogt B, Zhao Z, Zabel P, et al. Regional lung response to bronchodilator reversibility testing determined by electrical impedance tomography in chronic obstructive pulmonary disease. Am J Physiol Lung Cell Mol Physiol. 2016;311(1):L8–19.
Zhao Z, Muller-Lisse U, Frerichs I, et al. Regional airway obstruction in cystic fibrosis determined by electrical impedance tomography in comparison with high resolution CT. Physiol Meas. 2013;34(11):N107–14.
Mauri T, Turrini C, Eronia N, et al. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195(9):1207–15.
Gattinoni L, Tonetti T, Quintel M. Regional physiology of ARDS. Crit Care. 2017;21(Suppl 3):312.
Maeda Y, Fujino Y, Uchiyama A, et al. Effects of peak inspiratory flow on development of ventilator-induced lung injury in rabbits. Anesthesiology. 2004;101(3):722–8.
Costa EL, Borges JB, Melo A, et al. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35(6):1132–7.
Karagiannidis C, Waldmann AD, Róka PL, et al. Regional expiratory time constants in severe respiratory failure estimated by electrical impedance tomography: a feasibility study. Crit Care. 2018;22(1):221.
Protti A, Maraffi T, Milesi M, et al. Role of strain rate in the pathogenesis of ventilator-induced lung edema. Crit Care Med. 2016;44(9):e838–45.
Katira BH, Engelberts D, Otulakowski G, et al. Abrupt deflation after sustained inflation causes lung injury. Am J Respir Crit Care Med. 2018;198(9):1165–76.
Broche L, Perchiazzi G, Porra L, et al. Dynamic mechanical interactions between neighboring airspaces determine cyclic opening and closure in injured lung. Crit Care Med. 2017;45(4):687–94.
Mauri T, Yoshida T, Bellani G, et al. PLeUral pressure working Group (PLUG—Acute Respiratory Failure section of the European Society of Intensive Care Medicine) Esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med. 2016;42(9):1360–73.
Baedorf Kassis E, Loring SH, Talmor D. Mortality and pulmonary mechanics in relation to respiratory system and transpulmonary driving pressures in ARDS. Intensive Care Med. 2016;42(8):1206–13.
Frerichs I, Amato MB, van Kaam AH, TREND study group, et al. Chest electrical impedance tomography examination, data analysis, terminology, clinical use and recommendations: consensus statement of the TRanslational EIT developmeNt stuDy group. Thorax. 2017;72(1):83–93.
Borgmann S, Schmidt J, Goebel U, Haberstroh J, Guttmann J, Schumann S. Dorsal recruitment with flow-controlled expiration (FLEX): an experimental study in mechanically ventilated lung-healthy and lung-injured pigs. Crit Care. 2018;22:245.
Acknowledgements
None.
Funding
The present study was supported in part by institutional funding (Ricerca corrente 2018—“Rimozione extracorporeal di anidride carbonica (CO2) e modulazione della ventilazione spontanea in pazienti con insufficienza respiratoria acuta (sindrome da distress respiratorio, ARDS) e acuta su cronico (broncopneumopatia cronico ostruttiva, COPD)”) of the Department of Anesthesia, Critical Care and Emergency, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy.
Author information
Authors and Affiliations
Contributions
TM, ES and GG contributed to design the conception and design of the study. FDC, CT, ML, LA, MA, DT and YW participated in acquisition and analysis of data for the study. TM, ES and FDC drafted the work. All authors collaborated to interpret data and revise the work critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethical committee of San Gerardo Hospital, Monza, Italy, approved the studies, and informed consent was obtained following local regulations.
Consent for publication
Not applicable.
Competing interests
Dr Mauri received personal fees as speaker from Drager, outside the submitted work. Dr. Grasselli received funding for lectures from Getinge, Draeger Medical, Fisher & Paykel, Pfizerand and travel/accommodation/congress registration support from Biotest and Getinge. The remaining authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1.
Regressions and Bland–Altman plots reporting specific results from each step of both studies (six conditions, 12 linear regressions and 12 Bland–Altman plots).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mauri, T., Spinelli, E., Dalla Corte, F. et al. Noninvasive assessment of airflows by electrical impedance tomography in intubated hypoxemic patients: an exploratory study. Ann. Intensive Care 9, 83 (2019). https://doi.org/10.1186/s13613-019-0560-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-019-0560-5