Abstract
Spinal cord injury (SCI) is a catastrophic injury to the central nervous system (CNS) that can lead to sensory and motor dysfunction, which seriously affects patients' quality of life and imposes a major economic burden on society. The pathological process of SCI is divided into primary and secondary injury, and secondary injury is a cascade of amplified responses triggered by the primary injury. Due to the complexity of the pathological mechanisms of SCI, there is no clear and effective treatment strategy in clinical practice. Exosomes, which are extracellular vesicles of endoplasmic origin with a diameter of 30–150 nm, play a critical role in intercellular communication and have become an ideal vehicle for drug delivery. A growing body of evidence suggests that exosomes have great potential for repairing SCI. In this review, we introduce exosome preparation, functions, and administration routes. In addition, we summarize the effect and mechanism by which various exosomes repair SCI and review the efficacy of exosomes in combination with other strategies to repair SCI. Finally, the challenges and prospects of the use of exosomes to repair SCI are described.
Similar content being viewed by others
Introduction
SCI is a catastrophic injury to the CNS that can lead to sensory and motor dysfunction and is characterized by a high rate of disability and mortality [1, 2]. Approximately 10.4–83 per 1 million people suffer from SCI each year worldwide. Furthermore, the morbidity and mortality rates are increasing each year. SCI still imposes significant costs on society and presents several challenges to the medical community [3]. After SCI, a series of pathophysiological changes occur at the lesion site, including inflammatory response and neuronal apoptosis, which are followed by the formation of cavities and scars, resulting in the inhibition of axonal regeneration [4]. Unfortunately, regeneration after SCI is extremely weak due to the low plasticity of the CNS and limited neuronal regeneration. Currently, there is no effective method to completely repair the function of the spinal cord after SCI [5].
Exosomes, which are extracellular vesicles of endoplasmic origin with a diameters of 30–150 nm, are secreted by cells [6]. Exosomes contains various biologically active molecules, including nucleic acids and proteins, which play a crucial role in intercellular communication [7, 8]. Importantly, exosomes show good stability, biocompatibility, biological barrier permeability, and low immunogenicity, which supports their use in the repair of tissue damage [9,10,11]. Furthermore, exosomes can carry new functional proteins through genetically engineered cells [12, 13]. In addition, exosomes can also be used as carriers of small molecules or nucleic acids to target drugs to specific types of cells or tissues [14,15,16]. Thus, exosomes are not only a potential tool for exploring the mechanism of SCI but may also be an important substance for repairing SCI in the future [17,18,19]. Consequently, in this article, we describe the preparation, functions, administration routes mechanism, and challenges of various exosomes in the treatment of SCI.
Preparation of exosomes
Isolation
Depending on the source and size of the exosomes, different techniques can be used to isolate exosomes from body fluids or cell cultures. To date, five exosome isolation techniques have been reported, including ultrahigh-speed centrifugation, size-based isolation, in situ polymer precipitation, immunoaffinity capture, and microfluidic derivations [20] (Fig. 1). Among these, ultrahigh-speed centrifugation is the most commonly used method of exosome isolation [21]. There are multiple techniques available to extract exosomes. However, these technologies have the drawbacks such as low extraction efficiency and poor purity. Therefore, there is an urgent need to further study the extraction techniques to optimize the large-scale production of exosomes for their clinical applications.
Identification
A variety of techniques have been used to better understand the composition of exosomes. Based on the morphological features, particle size, and surface markers of exosomes, methods for exosome identification include transmission electron microscopy, scanning electron microscopy, cryo-electron microscopy, atomic force microscopy, nanoparticle tracking analysis, dynamic light scattering, trypsin digestion, mass spectrometry, enzyme-linked immunosorbent assay (ELISA), and marker protein expression assays such as Western blot analysis and flow cytometry [22,23,24] (Fig. 1).
Functions of exosomes
Diagnostic role
The natural structure and unique functions of exosomes give them great potential as carriers of natural drugs or genes and high diagnostic potential in immunotherapy, vaccination trials, and regenerative medicine, but the development of efficient and reliable isolation methods is necessary to fully exploit their potential [25]. Exosomes hold promise as diagnostic biomarkers for cardiovascular disease, Parkinson's disease, other neurodegenerative diseases (e.g., Alzheimer's disease), and cancer [26]. In current clinical trials, the use of exosomes as diagnostic biomarkers is based on their role in intercellular communication and disease progression, as well as the loading of related cargoes such as miRNAs, various noncoding RNAs, mitochondrial RNAs, and surface proteins [27,28,29].
Therapeutic role
Exosome treatment strategies can be categorized as direct, indirect, or alternative therapies. Direct therapies refer to the use of exosomes as therapeutic agents. Direct therapies take advantage of the ability of exosomes to transfer proteins and nucleic acids between cells and use exosomes as drug carriers to treat disease or injury [26]. Indirect methods refer to the use of exosomes as biomarkers. Exosomes are present in the bloodstream and in all body fluids and exhibit high stability over a wide range of temperatures when isolated [30]. These properties reduce the cost of storage and transport and increase the clinical value of exosomes as biomarkers. Alternative approaches include the elimination of disease-promoting exosomes [31]. Exosomes can be used to stop disease progression by ablating the presence of exosomes that contain harmful disease-associated cargoes, such as viral miRNAs, proteins, and immunosuppressive factors, which promote tumorigenesis, tumour growth, tumour metastasis, and tumour drug resistance [31,32,33,34].
Prognostic role
Tumour-derived exosome cargo matches the genetic content of parental tumour cells [35]. Moreover, exosomes are stable in the bloodstream and protect their cargo from degradation [36]. Therefore, exosomes are increasingly recognized as novel biomarkers for the prognostic evaluation of patients with cancer. Exosomes components, such as the exosome membrane bound proteins New York esophageal squamous cell carcinoma 1 (NY-ESO-1), human alkaline phosphatase (PLAP), epidermal growth factor receptor (EGFR), antibody to apoptosis inducible factor 6 interacting protein (AlIX) and epithelial cell adhesion molecule (EpCAM), can be used as non-invasive prognostic biomarkers of lung cancer [37]. Serum exosomal miR-10b and miR-21 are independent prognostic factors of early disease-free survival in patients with hepatocellular liver cancer [38]. KRAS mutations in circulating exosomal DNA may serve as a prognostically relevant biomarker for patients with early-stage pancreatic cancer [39]. Detection of androgen receptor splice variant 7 (AR-V7) in plasma-derived exosomal RNA significantly predicts resistance to hormone therapy in patients with metastatic prostate cancer, making it a potentially prognostically relevant biomarker [40]. Plasma circulating exosomes carrying PSMA3 and lncPMSA3-AS1 in patients with multiple myeloma are significantly associated with progression-free survival and overall survival [41]. Numerous studies have shown that the prospect of using exosomes for prognostic assessment is intriguing, but their use as prognostic biomarkers of cancer still faces significant challenges. Therefore, further studies are urgently needed to identify reliable exosome biomarkers in large samples for clinical applications. Although exosomes have not been used for the prognostic evaluation of SCI, this may be a new research direction in the future.
Administration routes of exosomes
Intravenous injection
Intravenous injection of exosomes is a commonly used methods of tissue repair. Huang et al. demonstrated that intravenous injection of epidural adipose tissue-derived mesenchymal stromal cell-derived extracellular vesicles (MSCs-EVs) could improve the repair effect of SCI by inhibiting the activation of the NLRP3 inflammasome and reducing the expression of inflammatory factors [42]. Other researchers showed that intravenous injection of exosomes secreted by miR-29b-modified bone marrow mesenchymal stromal cells could repair SCI in rats [17]. Overall, intravenous injection is one of the most commonly used methods in experiments because there are no barriers to absorption or first-pass metabolism, and this route has the highest bioavailability among the various delivery methods, allowing long-term therapy.
Local injection
Local injection of gingival mesenchymal stromal cell-derived exosomes (GMSCs-Exos) significantly reduced periodontal bone resorption and the number of tartrate-resistant acid phosphatase (TRAP)-positive osteoclasts, and these effects were further enhanced by pretreating GMSCs with tumour necrosis factor α (TNF-α) [43]. Local injection of miR-6924-5p-rich exosomes derived from genetically modified scleraxis-overexpressing PDGFRα (+) BMMSCs significantly reduced osteoclast formation and then improved the healing strength of tendons and bone [44]. Local injections are difficult because multiple repeated administrations are required, although the drug concentration is high.
Intranasal injection
Neuroinflammation-induced migration of mesenchymal stromal cell-derived exosomes (MSCs-Exos) has been shown to have a high affinity for neurons in the lesion after intranasal administration. Intranasal administration of exosomes resulted in significant motor improvements, sensory recovery, and faster recovery of urinary reflexes. Functional recovery was associated with biological changes, such as decreased neuroinflammation, increased axonal regeneration, angiogenesis promotion, and improved electrophysiological signals [45]. Depression-like behaviour was ameliorated in mildly stressed mice after intranasal injection of a miR-139-5p antagonist, suggesting that increased levels of exosomal miR-139-5p may mediate the stress-induced depression-like behaviour in mice [46]. However, there have been few studies on the transnasal administration of exosomes, and many studies are needed to evaluate the efficacy.
Intravitreal injection
Intravitreal injection of exosomes is another important method for tissue repair and is mainly used to treat retinal disease. Mead et al. [47] have reported that intravitreal injection of BMSCs-Exos promoted the survival of retinal ganglion cells through miRNA-dependent mechanisms. Wang et al. [48] have demonstrated that intravitreal injection of an exosome-associated adeno-associated viral vector enhanced retinoschisin 1 gene transduction in the mouse retina. Moisseiev and colleagues [49] have found that intravitreal administration of MSCs-Exos protected against retinal ischaemia. Intravitreal injection of exosomes has rarely been reported in the literature, but it is a safe, reliable, and effective method of exosomes administration to treat ophthalmic disorders.
Overall, the routes of administration of exosomes include intravenous, local, and intranasal administration and intravitreal injection (Fig. 1). However, there have been few comparative studies on the advantages and disadvantages of these methods, which need to be further studied by researchers in the future.
Pathological mechanisms of SCI
Pathological process of SCI
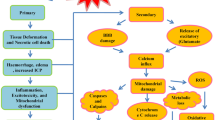
SCI is pathophysiologically divided into primary and secondary injuries [1]. Primary injury occurs when the spine is suddenly injured, resulting in fractures and vertebral displacements characterized by bone fragments and ruptures of the spinal cord ligaments, including destruction of the nerve parenchyma, axonal network destruction, haemorrhage, and disruption of glial membranes [50]. Secondary injury is a cascade of responses triggered by the primary injury, and it is a progressive disease characterized by increased production of proinflammatory cytokines, reactive oxygen species, oxidative damage, and excitatory amino acids (e.g., glutamate), loss of ion homeostasis, mitochondrial dysfunction, and cell death [51].
SCI can be temporally divided into the acute (< 48 h), subacute (48 h to 14 days), intermediate (14 days to 6 months), and chronic (> 6 months) phases [52]. Based on previous studies, we classified the factors that affect SCI recovery as the inflammatory microenvironment, neurotrophic factors in the microenvironment, and the regenerative microenvironment (Fig. 2).
Inflammatory microenvironment
Microglia play an important role in the activation and regulation of neuroinflammation after SCI. Microglia can be classified as M1 and M2 types based on their functional role in the inflammatory response, and M1 cells are considered proinflammatory, while M2 cells are considered anti-inflammatory [53,54,55]. Therefore, finding factors that promote the polarization of microglia towards the M2 phenotype is of great importance for SCI. Furthermore, activated microglia release proinflammatory cytokines, proteases, or other cytotoxic factors, which lead to secondary SCI [56]. Meanwhile, activated microglia may also play a beneficial role by inhibiting lesion expansion, clearing debris, producing anti-inflammatory factors, and attracting numerous immune cells to penetrate the damaged blood-spinal cord barrier (BSCB) [57,58,59].
Macrophages are derived from blood monocytes and form an innate immune defence together with microglia. David et al. reported that bone marrow-derived macrophages invade lesion centres, phagocytose apoptotic and necrotic cells, and remove tissue debris after SCI [56]. However, nuclear factor kappa β (NF-κβ), signal transducer and activators of transcription 1 (STAT1), and interferon regulatory factor 5 (IRF-5) promote macrophage differentiation into the M1 subtypes, which is proinflammatory. In addition, reactive oxygen species (ROS), reactive nitrogen species (RNS), and lipid peroxidation mediate M1 macrophage activation and the conversion from the M2 phenotype to the M1 phenotype [60, 61]. Furthermore, macrophages also release inflammatory cytokines that exacerbate secondary SCI [57, 59]. Therefore, macrophages are a double-edged sword in the repair of SCI.
Trophic factors in the microenvironment
Trophic factors mainly include brain-derived neurotrophic factor, glial cell line-derived neurotrophic factor, nerve growth factors, hepatocyte growth factor (HGF), insulin-like growth factor-1 (IGF-1), fibroblast growth factor and neurotrophic factor 3. Neurotrophic factors are crucial for the repair of SCI because promote axonal regeneration. Insufficient secretion of mature neurotrophic factors and increased expression of precursors after SCI can lead to apoptosis and necrosis in neurons and result in the collapse of growth cones, which are important factors that limiting nerve regeneration.
Regenerative microenvironment
Myelin sheath regeneration
The myelin sheath refers to a layer of membrane wrapped around the axons of nerve cells, which is composed of Schwann cells. The myelin sheath has the following functions: (1) to avoid interference between axons and surrounding tissues; (2) accelerate the transmission of action potentials through “skip conduction”; and (3) guide axon regeneration after axon damage. Thus, myelin regeneration is one of the important links in the recovery of neural function after SCI.
In the acute phase of SCI, the number of oligodendrocytes that die and the integrity of myelin are disrupted [62, 63]. In the subacute phase of SCI, oligodendrocyte progenitor cells (OPCs) are activated and begin to differentiate into new oligodendrocytes. In addition, some OPCs may differentiate into Schwann cells. Endothelial cells are activated, and some of these cells differentiate into oligodendrocytes. In the chronic phase of SCI, the new-born oligodendrocytes form myelin around the preserved or regenerated axons [2].
Axonal regeneration
In the acute phase of SCI, axonal degeneration is enhanced by oligodendrocyte death and myelin degradation [2]. In the subacute phase of SCI, axons are demyelinated and remodelled [64]. In the chronic phase of SCI, axonal necrosis occurs and then the number of axons decreases and reaches a minimum [65, 66].
Various harmful factors can influence axonal regeneration after SCI. First, microtubules become unstable, disorganized, and unevenly distributed, leading to an low supply of growth cones and impaired axonal contraction [67]. Second, mitochondrial dysfunction can lead to a lack of energy supply to neurons and vascular endothelial cells, ultimately hindering axonal regeneration [68]. Thus, axonal regeneration after SCI requires the restoration of mitochondrial function to ensure sufficient energy supply [69]. Li et al. [70] found that fgf13-induced microtubule stabilization enhanced mitochondrial axonal transport. Third, a membrane-associated protein belonging to the reticulin family, oligodendrocyte myelin glycoprotein, and myelin-associated glycoprotein have been identified as myelin-associated inhibitors that can collapse axon growth cones and inhibit neurite growth [71,72,73,74,75]. Therefore, it is crucial to conduct in-depth research on the relevant mechanisms that prevent axonal regeneration.
Scar formation
Scarring after SCI proceeds as follows: In the acute phase of SCI, astrocytes polarize towards the A1 and A2 phenotypes, and pericytes migrate from blood vessels towards the centre of the injury. In the subacute phase of SCI, the scar is formed by natural astrocytes, OPCs, and astrocytes derived from neural stem cells (NSCs). In addition, pericytes derived from fibroblasts close the scar. In the chronic phase of SCI, the scar is stabilized, limiting inflammation and inhibiting axonal regeneration [2].
Astrocytes and pericytes are the main cells involved in scar formation after SCI. Astrocytes are an integral part of the CNS and play an important role in normal neuronal development, synapse formation, neuronal circuit function, and action potential propagation [76,77,78]. Astrocytes have been classified as A1 and A2 subtypes. A1 astrocytes have upregulated the expression of complement cascade genes that disrupt synapses and damage the nervous system, while A2 astrocytes have upregulated the expression of several neurotrophic factors that may be neuroprotective [79]. Hara et al. [80] reported that type I collagen was highly expressed in the spinal cord during the scar-forming phase and induced astrocytic scar formation via the integrin–N-cadherin pathway. Moreover, pericytes have long projections that surround the vessel wall and are involved in regulating blood flow and the development, maturation, and remodelling of vessels [81,82,83]. Subsequently, scholars have shown that inhibiting fibrous scar formation caused by pericytes is beneficial for axonal regeneration [84,85,86]. In summary, in-depth research on scar formation after SCI related to astrocytes and pericytes is crucial for improving neurological function recovery after SCI.
Exosome-mediated repair of SCI
Neural stem cell-derived exosomes (NSCs-Exos)
NSCs can differentiate into neurons, oligodendrocytes, and astrocytes and have the ability to repair SCI [87,88,89]. However, NSC transplantation has many disadvantages that are difficult to overcome. First, it is difficult to pass the BSCB due to a large cell size; second, large cell size blocks distal blood vessels leading to local tumour formation, and third, exogenous NSCs have low survival rates in vivo. Therefore, these factors lead to limited repair of SCI by NSCs [90, 91]. Subsequently, NSCs-Exos, which are derived from NSCs, were attempted to be applied to the repair of SCI and showed encouraging results [92, 93]. Ma et al. claimed that NSCs-Exos promoted neural regeneration by regulating miR-219a-2-3p to repair the SCI [94]. Chen et al. reported that NSCs-Exos promoted neuronal morphology remodelling and improved nerve function in the lower limbs by regulating the PTEN/AKT pathway [95]. Zhong et al. [96] showed that NSCs-Exos were able to transfer vascular endothelial growth factor A (VEGF-A) into spinal microvascular endothelial cells and improve SCI repair through the proangiogenic effects of VEGF-A. Moreover, Zhang et al. [97] showed that NSCs-Exos suppressed neuronal cell apoptosis by activating autophagy via the miR-374-5p/STK-4 axis in SCI. Therefore, NSCs-Exos are a novel and promising substance for the repair of SCI.
Schwann cell-derived exosomes (SCs-Exos)
SCs are glial cells associated with peripheral nerves that repair injuries to peripheral and central nerves. SCs, which are an important component of the myelin sheaths, have been shown to play an active role in nerve repair [98, 99]. Nevertheless, the therapeutic efficacy of SC transplantation in promoting functional recovery after SCI is limited due to the poor survival rate of SCs after transplantation and the difficulty of overcoming the blood–brain barrier (BBB) [100, 101]. Then, SCs-Exos have been shown to facilitate axonal regeneration and inhibit inflammatory responses [102, 103]. Scholars found that SCs-Exos could promote angiogenesis through the upregulation of integrin-β1, inhibit neuronal apoptosis through the modulation of the EGFR/Akt/mTOR pathway, and affect the anti-inflammatory response through the modulation of the SOCS3/STAT3 pathway, which improved the recovery effect of motor function after SCI [104,105,106,107]. Thus, SCs-Exos are an alternative option for repairing SCI by promoting myelin regeneration.
Mesenchymal stromal cell-derived exosomes (MSCs-Exos)
MSCs are pluripotent stem cells that can be derived from various cells, such as bone marrow, adipose tissue, and umbilical cord. In particular, MSCs-Exos can maintain the integrity of the BSCB and promote angiogenesis, proliferation and antioxidant effects, as well as immunomodulatory, anti-inflammatory, and antiapoptotic effects [108]. MSCs-Exos, which are derived from MSCs, are enriched in important MSC substances [109]. Accordingly, various MSCs-Exos, such as HUCMSCs-Exos, BMSCs-Exos and engineered MSCs-Exos, promote nerve regeneration, facilitate angiogenesis, inhibit the inflammatory response, suppress oxidative stress, block apoptosis, and reduce glial scar formation, thus working to repair SCI [92, 110,111,112,113]. Furthermore, a multiple signalling pathways associated with SCI repair by MSCs-Exos have been described, including PTEN/AKT, PTEN-AKT-mTOR, TLR4/NF-κβ, TLR4/MyD88/NF-κβ, ROS/MAPK/NF-κβ/P65, TIMP2/MMP, miR-21/PTEN/PDCD4, and miR-329-3p/IGF1R axes [110, 114,115,116,117,118,119]. Indeed, one type of MSCs-Exos can repair SCI through multiple pathways; for example, engineered BMSCs-Exos can simultaneously inhibit neuronal apoptosis and promote vascularization (Fig. 3). Thus, MSCs-Exos may provide new insights for repairing SCI.
Astrocyte-derived exosomes (AS-Exos)
Astrocytes are the most common glial cells in the CNS and play a role in supporting the BBB, controlling ionic homeostasis, and regulating neuronal function in the CNS [120, 121]. Recently, scholars have found that AS-Exos play an important role in CNS injury. Under physiological conditions, AS-Exos contains proteins and miRNAs that promote neuronal survival and axonal growth [122, 123]. However, under pathological conditions, AS-Exos may promote neuronal apoptosis [124]. Long et al. [125] reported that AS-Exos could promote microglial polarization towards the M2 phenotype by inhibiting ERK and NF-κβ p65 phosphorylation, thereby attenuating neurological deficits due to traumatic brain injury (TBI). Zhang et al. [95] suggested that AS-Exos could activate the Nrf2 signalling pathway to inhibit neuronal oxidative stress and neuronal apoptosis, thus relieving TBI. Chen et al. [126] have found that AS-Exos carrying GJA1-20k can decrease Cx43 phosphorylation, protect mitochondrial function, and decrease the rate of neuronal apoptosis, thus promoting neuronal recovery. Studies have shown that AS-Exos could reduce cerebral ischaemia/reperfusion-induced neurological injury by targeting TLR7 to downregulate the NF-κβ/MAPK pathway [127]. Although studies have used AS-Exos to treat TBI, few have used them to treat SCI. However, both TBI and SCI are CNS injuries, and there are similarities in the injury mechanisms and treatment options. We believe that more and more research will be done in the future on AS-Exos-mediated repair of SCI and that AS-Exos are a very promising factors for repairing SCI.
Platelet-rich plasma-derived exosomes (PRP-Exos)
To date, few studies have focused on PRP-Exos for the repair of SCI, but numerous reports have focused on platelet-rich plasma extracellular vesicles (PRP-EVs) for the treatment of SCI [128]. PRP-Exos and PRP-EVs are PRP derivatives that are similar in their major components and differ only in diameter. Thus, in this section, we reviewed the role of PRP-EVs in repairing SCI. PRP-EVs are enriched with a variety of important biomolecules, including growth factors, cytokines, chemokines, lipids, and nucleic acids, which are able to influence coagulation, inflammatory response, and neovascularization; therefore, PRP-EVs have promising applications in the field of tissue repair and regeneration [129,130,131]. In recent years, many scholars have conducted preclinical studies of PRP-EVs used in myocardial ischaemia [132, 133], cerebral ischaemia [134], atherosclerosis [135, 136], vascular damage [137], haemorrhagic shock [138], wound healing [139, 140], acute lung injury [141], necrosis of the femoral head [142], and osteoarthritis [143]. However, there have been few studies related to PRP-EVs in the treatment of SCI. Therefore, this is a direction for future research. We believe that the study of PRP-Exos and PRP-EVs in SCI repair is in its early stage, and a large number of in-depth studies are still needed to evaluate their role in repairing SCI.
Macrophage-derived exosomes (M-Exos)
Macrophages are an important kind of immune cell and are classified into two subtypes: M1 and M2 [144]. M1 macrophages are able to secrete substances that promote the inflammatory response, which leads to the aggravation of SCI; however, M2 macrophages inhibit the inflammatory response and promote angiogenesis, which helps to repair SCI [145,146,147,148]. Therefore, the opposite roles of M1 and M2 macrophages in the SCI microenvironment have received increasing attention. Huang et al. [149] found that M2 macrophage-derived exosomes (M2-Exos) were able to activate the HIF-1/VEGF signalling pathway to promote neovascularization and thus play a role in repairing SCI. Peng et al. [150] noted that M2-Exos induced the transformation of M1 macrophages into M2 macrophages by regulating the miR-23a-3p/PTEN/PI3K/AKT signalling axis, thereby improving the local microenvironment after SCI. Moreover, Zhang et al. also reported that peripheral macrophage-derived exosomes (PM-Exos) promoted repair after SCI by inducing local polarization of anti-inflammatory microglia by inhibiting the PI3K/AKT/mTOR pathway [151]. Thus, M-Exos is critical in SCI repair.
Vascular endothelial cell-derived exosomes (VECs-Exos)
Ge et al. [152] found that VECs-Exos could enhance M2 microglia/macrophage polarization and improve functional recovery by delivering USP13 and concluded that VECs-Exos were promising agents for the repair of SCI. Unfortunately, there have been very few studies on the repair of SCI by VECs-Exos, and more and more insightful experimental research is necessary.
Induced pluripotent stem cell-derived exosomes (iPSCs-Exos)
Li et al. [153] reported that iPSCs-Exos carrying miR-199b-5p could treat SCI confirmed that miR-199b-5p induced macrophage polarization and SCI recovery by regulating the HGF and phosphoinositide 3-kinase (PI3K) signalling pathways and concluded that the miR-199b-5p-bearing iPSCs-Exos might become an effective method to treat SCI. At present, few studies have been conducted on the treatment of SCI by iPSCs-Exos, which need to be further studied in the future.
Microglia-derived exosomes (MG-Exos)
Microglia are a type of immune cell found in the CNS that protects neuronal cells. Li et al. [154] found that MG-Exos inhibited neuronal apoptosis and promoted axon growth by regulating the p53/p21/CDK1 signalling pathway, which had neuroprotective effects. In addition, Peng et al. [155] claimed that MG-Exos could improve spinal cord functional recovery after injury by inhibiting oxidative stress and promoting the survival and function of endothelial cells by activating the Keap1/Nrf2/HO-1 signalling pathway. Moreover, Huang et al. [156] found that the increase in miR-124-3p in MG-Exos following TBI could inhibit neuronal inflammation and contribute to neurite outgrowth after being transferred into neurons. Thus, MG-Exos are also an optional, promising and important substance for the treatment of SCI.
Regulatory T cell-derived exosomes (Treg-Exos)
Treg cells are present within all tissues and supress excessive immune activation to curb autoimmunity and maintain immune homeostasis [157]. Xiong and colleagues [158] found that Treg cell-derived exosomal miR-709 attenuated microglial pyroptosis and promoted motor function recovery after SCI. However, little is known about the exact mechanism by which Treg-Exos promotes the recovery of behavioural function after SCI in mice, which needs to be further explored in future studies.
Various exosomes and their functions in the treatment of SCI are summarized in Table 1.
Mechanisms by which exosomes repair SCI
Promote nerve regeneration
Neurons are the basic structural and functional units of the nervous system. SCI can result in neuronal damage [159]. Chen et al. [95] claimed that FTY720-loaded NSCs-Exos therapy could promote neuronal morphology by modulating the PTEN/AKT pathway and improve hindlimb motor function. SCs-Exos and MG-Exos have protect axons through the EGFR/Akt/mTOR and p53/p21/CDK1 pathways, respectively [106, 154]. Moreover, many researchers found that MSCs-Exos could inhibit neuronal cell death and promote axonal regeneration through various pathways, including the miR-5627-5p/FSP1, ERK1/2, and PTEN-AKT-mTOR pathways [118, 160,161,162]. Thus, promoting axonal regeneration is one of the ways to repair SCI (Fig. 4).
Promote angiogenesis
Vascularization facilitates nerve regeneration and promotes neurovascular unit recovery after SCI [163]. Yuan et al. [110] found that pericyte exocytosis could promote blood flow, improve vascular endothelial function, and protect the BSCB via the PTEN/AKT signalling pathway, which is beneficial for SCI recovery. Huang et al. [149] showed that M2 macrophage-derived exosomes could promote angiogenesis after SCI through activation of the HIF-1/VEGF pathway. Thus, angiogenesis and improvements in vascular endothelial function promoted by exosomes are one of the ways to repair the SCI (Fig. 4).
Anti-inflammatory effects
Microglia and macrophages can release cytokines and chemokines after SCI, leading to neuroinflammatory responses [164]. According to the previous studies, exosomes that exert anti-inflammatory effects can be categorized into multiple groups. First, exosomes such as HUCMSCs-Exos can inhibit microglia and macrophage activation through the BCL2/Bax and Wnt/β-catenin signalling pathways [165]. Second, exosomes such as SCs-Exos and M2-Exos inhibit M1 macrophages/microglia polarization and promote M2 polarization via the SOCS3/STAT3 and miR-23a-3p/PTEN/PI3K/AKT pathways [105, 150]. Third, exosomes such as BMSCs-Exos and MSCs-Exos induce differentiation of microglia or macrophages of the M1 subtype toward the M2 type by inhibiting the TLR4/MyD88/NF-κβ and promoting the PI3K/AKT pathways [54, 115]. Fourth, exosomes such as PM-Exos can activate autophagy in microglia and enhance anti-inflammatory effects by inhibiting the PI3K/AKT/mTOR pathway [151]. Thus, exosomes can inhibit neuroinflammatory responses through multiple signalling pathways to repair SCI (Fig. 4).
Antiapoptotic effects
Apoptosis is a type of programmed cell death that plays an important role in SCI, especially in secondary SCI. It occurs in glial cells, oligodendrocytes, neurons, and vascular endothelial cells and severely affects the recovery of neurologic function [166, 167]. Therefore, blocking apoptosis after SCI is essential and can improve the recovery effect of SCI. Various types of exosomes, such as NSCs-Exos, BMSCs-Exos or HUCMSCs-Exos, have been shown to have antiapoptotic effects after SCI through different signalling pathways, including the TLR4/MyD88/NF-κβ [115], PI3K/Akt [168], BCL2/Bax and Wnt/β-catenin [165], miR-21/PTEN/PDCD4 [119] and miR-16-5p/IGF-1 pathways [169]. Thus, the antiapoptotic effects of exosomes can repair SCI (Fig. 4).
Antioxidative stress effects
Lipid peroxidation is one of the characteristic features of secondary SCI, which is caused by significantly increased levels of ROS and RNS and eventually leads to cytokinesis, the destruction of proteins and nucleic acids, and apoptosis or necrosis [170, 171]. Thus, inhibiting oxidative stress is necessary for functional recovery after SCI. Numerous types of exosomes, such as MSCs-Exos or MG-Exos, have been confirmed to have antiapoptotic effects after SCI by regulating multiple signalling pathways, such as the miR-329-3p/IGF1R [172], Keap1/Nrf2/HO-1 [155] and miR-16-5p/IGF-1 pathways [169]. Thus, the antioxidative effect of exosomes can repair SCI (Fig. 4).
Exosomes combined with other methods to repair SCI
Exosomes combined with hydrogels
Although exosomes have been shown to have favourable effects on SCI, scholars have shown that intravenous injection of exosomes has serious drawbacks, including a short half-life and low targetability [173]. Therefore, exploring other types of medical biomaterials to improve the efficacy of exosomes is an urgent problem. Hydrogel is a polymer material with high water content and diverse physical properties. Hydrogels currently used for SCI repair include natural hydrogels such as alginate, agarose, collagen, fibronectin, gelatine, and extracellular matrix, and synthetic hydrogels such as polylactic acid, polylactic acid-glycolic acid, and polyethylene glycol [174]. Researchers showed that exosomes encapsulated by hydrogels offer multiple advantages, including slow rate release of exosomes, the maintenance of exosome bioactivity, and improved exosome targeting, which offer promising prospects for the medical use of exosomes [175]. Many scholars have proven that exosomes combined with hydrogels can provide better anti-inflammatory effects, inhibit glial scar formation, promote axonal regeneration, and promote neovascularization after local injection and long-term release, thus improving neurological function after SCI [174, 176,177,178,179] (Fig. 5). Thus, exosomes combined with hydrogels are a promising approach for the repair of SCI.
Exosomes carrying drugs
Successful delivery of therapeutic agents to target cells and tissues is limited by many factors, including the instability of therapeutic agents in vivo, the isolation of target tissues and the BSCB, and drug efflux systems, among which, the BSCB is one of the major obstacles to SCI repair [173]. However, exosomes show great potential for application as drug carriers due to their relatively small molecular structure, natural molecular transport properties, good biocompatibility, and ability to penetrate BSCB [173, 180]. As a result, researchers have modified exosomes to use them as therapeutic drug carriers. Recently, Zeng et al. [181] identified an azide-modified Ile-Lys-Val-Ala-Val peptide conjugated onto M2-Exos that provided strong evidence of SCI recovery, including inhibiting inflammation, promoting neuronal differentiation of NSCs, and targeting the injured site of the spinal cord after tail vein injection. In addition, Gao et al. [182] found that another combination agent in which berberine was attached to M2-Exos could repair SCI through anti-inflammatory and antiapoptotic effects and by inducing the polarization of M1-type macrophages to the M2 type. Moreover, Yue et al. [183] indicated that exosomes could enhance the solubility of resveratrol and enhance penetration of the drug through the BBB, thereby increasing its concentration in the CNS. Thus, as drug carriers, exosomes have many advantages. They maintain drug stability in the body, improve drug solubility, mediate drug targeting, and facilitate drug crossing of the BBB and BSCB (Fig. 5). Consequently, exosomes will be a promising drug delivery system for the repair of SCI.
Challenges in the use of exosomes to repair SCI
Low amounts
Currently, various methods of exosome acquisition are available. However, no standardized consensus on exosome extraction methods has been established. Accordingly, exosomes extracted by different methods showed significant differences in protein and RNA levels [184]. Furthermore, even if exosomes are extracted, they are present in very low amounts [185,186,187]. To date, ultracentrifugation is the most commonly used method of exosome isolation; however, the exosomes acquired by ultracentrifugation may contain other impurities, such as extracellular vesicles with diameters close to those of the exosomes [188] (Fig. 6).
Low targeting
Scholars attribute the low targeting of exosomes to the fact that intravenously injected exosomes accumulate in the kidneys, liver, and spleen and are rapidly eliminated through glomerular filtration, biliary excretion, and phagocytosis by the reticuloendothelial system, which ultimately leads to poor therapeutic efficacy [173, 189, 190] (Fig. 6).
Other challenges
Despite the favourable results of exosomes in preclinical studies of SCI, using exosomes to repair SCI in the clinic practice still faces challenges. First, clarifying the conditions for the safe storage, transport, and preservation of exosomes is fundamental to the development of exosome therapy. Second, clarifying the dose, frequency, duration, and method of administration of exosomes for SCI repair is an important measure to ensure therapeutic efficacy [180, 191] (Fig. 6).
Conclusion
SCI repair remains a challenge for the medical field. Exosomes derived from various cells are important intercellular communication substances that can mediate SCI repair by inhibiting inflammatory responses, promoting neurovascular regeneration, inhibiting scarring, resisting oxidative stress, and reducing cell apoptosis, which affect SCI repair by regulating multiple signalling pathways, including the PTEN-AKT/mTOR, EGFR/Akt/mTOR, p53/p21/CDK1, ERK1/2, HIF-1/VEGF, SOCS3/STAT3, TLR4/MyD88/NF-κβ, ROS/MAPK/NF-κβ P65, BCL2/Bax, Wnt/β-catenin, PI3K/AKT/mTOR, HGF, PTEN/PDCD4 and Keap1/Nrf2/HO-1 pathways. Moreover, engineered exosomes, exosome-carried drugs, and exosome-combined hydrogels are important ways to enhance the repair of SCI and are hot research topics. The use of exosomes for SCI repair also faces disadvantages such as low targeting and a short half-life, but we believe that the existing research results provide sufficient evidence for preclinical studies and the use of exosomes to treat SCI. In summary, exosomes are a promising therapeutic strategy for SCI.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- SCI:
-
Spinal cord injury
- CNS:
-
Central nervous system
- NSCs-Exos:
-
Neural stem cell-derived exosomes
- SCs-Exos:
-
Schwann cell-derived exosomes
- MSCs-Exos:
-
Mesenchymal stromal cell-derived exosomes
- AS-Exos:
-
Astrocyte-derived exosomes
- PRP-Exos:
-
Platelet-rich plasma-derived exosomes
- M-Exos:
-
Macrophage-derived exosomes
- VECs-Exos:
-
Vascular endothelial cell-derived exosomes
- iPSCs-Exos:
-
Induced pluripotent stem cell-derived exosomes
- MG-Exos:
-
Microglia-derived exosomes
- Treg-Exos:
-
Regulatory T cell-derived exosomes
- MSCs-EVs:
-
Mesenchymal stromal cell-derived extracellular vesicle
- BMSCs-Exos:
-
Bone marrow mesenchymal stromal cell-derived exosomes
- GMSCs-Exos:
-
Gingival tissue mesenchymal stromal cell-derived exosomes
- HUCMSCs-Exos:
-
Human umbilical cord mesenchymal stromal cell-derived exosomes
- TRAP:
-
Tartrate-resistant acid phosphatase
- TNF-α:
-
Tumour necrosis factor α
- BSCB:
-
Blood-spinal cord barrier
- NF-κβ:
-
Nuclear factor kappa β
- STAT1:
-
Signal transducer and activators of transcription 1
- IRF-5:
-
Interferon regulatory factor 5
- ROS:
-
Reactive oxygen species
- RNS:
-
Reactive nitrogen species
- HGF:
-
Hepatocyte growth factor
- IGF-1:
-
Insulin-like growth factor-1
- OPCs:
-
Oligodendrocyte progenitor cells
- CSPGs:
-
Chondroitin sulphate proteoglycans
- VEGF:
-
Vascular endothelial growth factor
- BBB:
-
Blood–brain barrier
- TBI:
-
Traumatic brain injury
- PRP-EVs:
-
Platelet-rich plasma extracellular vesicles
- HIF-1:
-
Hypoxia-inducible factor-1
- Ber:
-
Berberine
- ELISA:
-
Enzyme-linked immunosorbent assay
- NY-ESO-1:
-
New York esophageal squamous cell carcinoma 1
- PLAP:
-
Human alkaline phosphatase
- EGFR:
-
Epidermal growth factor receptor
- AlIX:
-
Antibody to apoptosis inducible factor 6 interacting protein
- EpCAM:
-
Epithelial cell adhesion molecule
- AR-V7:
-
Androgen receptor splice variant 7
References
Shen Y, Cai J. The importance of using exosome-loaded miRNA for the treatment of spinal cord injury. Mol Neurobiol. 2023;60(2):447–59.
Fan B, Wei Z, Feng S. Progression in translational research on spinal cord injury based on microenvironment imbalance. Bone Res. 2022;10(1):35.
Karsy M, Hawryluk G. Modern medical management of spinal cord injury. Curr Neurol Neurosci Rep. 2019;19(9):65.
Wertheim L, Edri R, Goldshmit Y, Kagan T, Noor N, Ruban A, Shapira A, Gat-Viks I, Assaf Y, Dvir T. Regenerating the injured spinal cord at the chronic phase by engineered iPSCs-derived 3D neuronal networks. Adv Sci (Weinh). 2022;9(11):e2105694.
Gong BS, Feng Q. Netrin-1: the new tumor markers in renal clear cell carcinoma. Asian Pac J Trop Med. 2015;8(6):489–93.
Pegtel DM, Gould SJ. Exosomes. Annu Rev Biochem. 2019;88:487–514.
Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367(6478):eaau6977.
Tkach M, Théry C. Communication by extracellular vesicles: where we are and where we need to go. Cell. 2016;164(6):1226–32.
Jiang XC, Zhang T, Gao JQ. The in vivo fate and targeting engineering of crossover vesicle-based gene delivery system. Adv Drug Deliv Rev. 2022;187:114324.
Yang LT, Patel KD, Rathnam C, Thangam R, Hou YN, Kang H, Lee KB. Harnessing the therapeutic potential of extracellular vesicles for biomedical applications using multifunctional magnetic nanomaterials. Small. 2022;18(13):2104783.
Hessvik NP, Llorente A. Current knowledge on exosome biogenesis and release. Cell Mol Life Sci. 2018;75(2):193–208.
Liang G, Kan S, Zhu Y, Feng S, Feng W, Gao S. Engineered exosome-mediated delivery of functionally active miR-26a and its enhanced suppression effect in HepG2 cells. Int J Nanomed. 2018;13:585–99.
Ye Y, Zhang X, Xie F, Xu B, Xie P, Yang T, Shi Q, Zhang CY, Zhang Y, Chen J, Jiang X, Li J. An engineered exosome for delivering sgRNA:Cas9 ribonucleoprotein complex and genome editing in recipient cells. Biomater Sci. 2020;8(10):2966–76.
Luan X, Sansanaphongpricha K, Myers I, Chen H, Yuan H, Sun D. Engineering exosomes as refined biological nanoplatforms for drug delivery. Acta Pharmacol Sin. 2017;38(6):754–63.
Antimisiaris SG, Mourtas S, Marazioti A. Exosomes and exosome-inspired vesicles for targeted drug delivery. Pharmaceutics. 2018;10(4):218.
Peng H, Ji W, Zhao R, Yang J, Lu Z, Li Y, Zhang X. Exosome: a significant nano-scale drug delivery carrier. J Mater Chem B. 2020;8(34):7591–608.
Yu T, Zhao C, Hou S, Zhou W, Wang B, Chen Y. Exosomes secreted from miRNA-29b-modified mesenchymal stem cells repaired spinal cord injury in rats. Braz J Med Biol Res. 2019;52(12):e8735.
Li C, Li X, Zhao B, Wang C. Exosomes derived from miR-544-modified mesenchymal stem cells promote recovery after spinal cord injury. Arch Physiol Biochem. 2020;126(4):369–75.
Jiang Z, Zhang J. Mesenchymal stem cell-derived exosomes containing miR-145-5p reduce inflammation in spinal cord injury by regulating the TLR4/NF-κB signaling pathway. Cell Cycle. 2021;20(10):993–1009.
Yang XX, Sun C, Wang L, Guo XL. New insight into isolation, identification techniques and medical applications of exosomes. J Control Release. 2019;308:119–29.
Chen C, Zhang Z, Gu X, Sheng X, Xiao L, Wang X. Exosomes: new regulators of reproductive development. Mater Today Bio. 2023;19:100608.
Lässer C, Eldh M, Lötvall J. Isolation and characterization of RNA-containing exosomes. J Vis Exp. 2012;59:e3037.
Zhao R, Zhao T, He Z, Cai R, Pang W. Composition, isolation, identification and function of adipose tissue-derived exosomes. Adipocyte. 2021;10(1):587–604.
Shao H, Im H, Castro CM, Breakefield X, Weissleder R, Lee H. New technologies for analysis of extracellular vesicles. Chem Rev. 2018;118(4):1917–50.
Li X, Corbett AL, Taatizadeh E, Tasnim N, Little JP, Garnis C, Daugaard M, Guns E, Hoorfar M, Li ITS. Challenges and opportunities in exosome research-perspectives from biology, engineering, and cancer therapy. APL Bioeng. 2019;3(1):011503.
Lai JJ, Chau ZL, Chen SY, Hill JJ, Korpany KV, Liang NW, Lin LH, Lin YH, Liu JK, Liu YC, Lunde R, Shen WT. Exosome processing and characterization approaches for research and technology development. Adv Sci (Weinh). 2022;9(15):e2103222.
Sina AA, Vaidyanathan R, Dey S, Carrascosa LG, Shiddiky MJ, Trau M. Real time and label free profiling of clinically relevant exosomes. Sci Rep. 2016;6:30460.
Sina AA, Vaidyanathan R, Wuethrich A, Carrascosa LG, Trau M. Label-free detection of exosomes using a surface plasmon resonance biosensor. Anal Bioanal Chem. 2019;411(7):1311–8.
Vaidyanathan R, Naghibosadat M, Rauf S, Korbie D, Carrascosa LG, Shiddiky MJ, Trau M. Detecting exosomes specifically: a multiplexed device based on alternating current electrohydrodynamic induced nanoshearing. Anal Chem. 2014;86(22):11125–32.
Zhou B, Xu K, Zheng X, Chen T, Wang J, Song Y, Shao Y, Zheng S. Application of exosomes as liquid biopsy in clinical diagnosis. Signal Transduct Target Ther. 2020;5(1):144.
Marleau AM, Chen CS, Joyce JA, Tullis RH. Exosome removal as a therapeutic adjuvant in cancer. J Transl Med. 2012;10:134.
Fu M, Gu J, Jiang P, Qian H, Xu W, Zhang X. Exosomes in gastric cancer: roles, mechanisms, and applications. Mol Cancer. 2019;18(1):41.
Hassanpour M, Rezaie J, Nouri M, Panahi Y. The role of extracellular vesicles in COVID-19 virus infection. Infect Genet Evol. 2020;85:104422.
Yang C, Robbins PD. The roles of tumor-derived exosomes in cancer pathogenesis. Clin Dev Immunol. 2011;2011:842849.
Tovar-Camargo OA, Toden S, Goel A. Exosomal microRNA biomarkers: emerging frontiers in colorectal and other human cancers. Expert Rev Mol Diagn. 2016;16(5):553–67.
Baassiri A, Nassar F, Mukherji D, Shamseddine A, Nasr R, Temraz S. Exosomal non coding RNA in LIQUID biopsies as a promising biomarker for colorectal cancer. Int J Mol Sci. 2020;21(4):1398.
Lobb RJ, van Amerongen R, Wiegmans A, Ham S, Larsen JE, Möller A. Exosomes derived from mesenchymal non-small cell lung cancer cells promote chemoresistance. Int J Cancer. 2017;141(3):614–20.
Tian XP, Wang CY, Jin XH, Li M, Wang FW, Huang WJ, Yun JP, Xu RH, Cai QQ, Xie D. Acidic microenvironment up-regulates exosomal miR-21 and miR-10b in early-stage hepatocellular carcinoma to promote cancer cell proliferation and metastasis. Theranostics. 2019;9(7):1965–79.
Allenson K, Castillo J, San Lucas FA, Scelo G, Kim DU, Bernard V, Davis G, Kumar T, Katz M, Overman MJ, Foretova L, Fabianova E, Holcatova I, Janout V, Meric-Bernstam F, Gascoyne P, Wistuba I, Varadhachary G, Brennan P, Hanash S, Li D, Maitra A, Alvarez H. High prevalence of mutant KRAS in circulating exosome-derived DNA from early-stage pancreatic cancer patients. Ann Oncol. 2017;28(4):741–7.
Del Re M, Biasco E, Crucitta S, Derosa L, Rofi E, Orlandini C, Miccoli M, Galli L, Falcone A, Jenster GW, van Schaik RH, Danesi R. The detection of androgen receptor splice variant 7 in plasma-derived exosomal RNA strongly predicts resistance to hormonal therapy in metastatic prostate cancer patients. Eur Urol. 2017;71(4):680–7.
Xu H, Han H, Song S, Yi N, Qian C, Qiu Y, Zhou W, Hong Y, Zhuang W, Li Z, Li B, Zhuang W. Exosome-transmitted PSMA3 and PSMA3-AS1 promote proteasome inhibitor resistance in multiple myeloma. Clin Cancer Res. 2019;25(6):1923–35.
Huang J-H, Fu C-H, Xu Y, Yin X-M, Cao Y, Lin F-Y. Extracellular vesicles derived from epidural fat-mesenchymal stem cells attenuate NLRP3 inflammasome activation and improve functional recovery after spinal cord injury. Neurochem Res. 2020;45(4):760–71.
Nakao Y, Fukuda T, Zhang Q, Sanui T, Shinjo T, Kou X, Chen C, Liu D, Watanabe Y, Hayashi C, Yamato H, Yotsumoto K, Tanaka U, Taketomi T, Uchiumi T, Le AD, Shi S, Nishimura F. Exosomes from TNF-α-treated human gingiva-derived MSCs enhance M2 macrophage polarization and inhibit periodontal bone loss. Acta Biomater. 2021;122:306–24.
Feng W, Jin Q, Ming-Yu Y, Yang H, Xu T, You-Xing S, Xu-Ting B, Wan C, Yun-Jiao W, Huan W, Ai-Ning Y, Yan L, Hong T, Pan H, Mi-Duo M, Gang H, Mei Z, Xia K, Kang-Lai T. MiR-6924-5p-rich exosomes derived from genetically modified Scleraxis-overexpressing PDGFRα(+) BMMSCs as novel nanotherapeutics for treating osteolysis during tendon-bone healing and improving healing strength. Biomaterials. 2021;279:121242.
Guo S, Perets N, Betzer O, Ben-Shaul S, Sheinin A, Michaelevski I, Popovtzer R, Offen D, Levenberg S. Intranasal delivery of mesenchymal stem cell derived exosomes loaded with phosphatase and tensin homolog siRNA repairs complete spinal cord injury. ACS Nano. 2019;13(9):10015–28.
Wei ZX, Xie GJ, Mao X, Zou XP, Liao YJ, Liu QS, Wang H, Cheng Y. Exosomes from patients with major depression cause depressive-like behaviors in mice with involvement of miR-139-5p-regulated neurogenesis. Neuropsychopharmacology. 2020;45(6):1050–8.
Mead B, Tomarev S. Bone marrow-derived mesenchymal stem cells-derived exosomes promote survival of retinal ganglion cells through miRNA-dependent mechanisms. Stem Cells Transl Med. 2017;6(4):1273–85.
Wang W, Liu J, Yang M, Qiu R, Li Y, Bian S, Hao B, Lei B. Intravitreal injection of an exosome-associated adeno-associated viral vector enhances retinoschisin 1 gene transduction in the mouse retina. Hum Gene Ther. 2021;32(13–14):707–16.
Moisseiev E, Anderson JD, Oltjen S, Goswami M, Zawadzki RJ, Nolta JA, Park SS. Protective effect of intravitreal administration of exosomes derived from mesenchymal stem cells on retinal ischemia. Curr Eye Res. 2017;42(10):1358–67.
Anjum A, Yazid MD, Fauzi Daud M, Idris J, Ng AMH, Selvi Naicker A, Ismail OHR, Athi Kumar RK, Lokanathan Y. Spinal cord injury: pathophysiology, multimolecular interactions, and underlying recovery mechanisms. Int J Mol Sci. 2020;21(20):7533.
Venkatesh K, Ghosh SK, Mullick M, Manivasagam G, Sen D. Spinal cord injury: pathophysiology, treatment strategies, associated challenges, and future implications. Cell Tissue Res. 2019;377(2):125–51.
Ahuja CS, Wilson JR, Nori S, Kotter MRN, Druschel C, Curt A, Fehlings MG. Traumatic spinal cord injury. Nat Rev Dis Primers. 2017;3:17018.
Jiang D, Gong F, Ge X, Lv C, Huang C, Feng S, Zhou Z, Rong Y, Wang J, Ji C, Chen J, Zhao W, Fan J, Liu W, Cai W. Neuron-derived exosomes-transmitted miR-124-3p protect traumatically injured spinal cord by suppressing the activation of neurotoxic microglia and astrocytes. J Nanobiotechnol. 2020;18(1):105.
Liu W, Rong Y, Wang J, Zhou Z, Ge X, Ji C, Jiang D, Gong F, Li L, Chen J, Zhao S, Kong F, Gu C, Fan J, Cai W. Exosome-shuttled miR-216a-5p from hypoxic preconditioned mesenchymal stem cells repair traumatic spinal cord injury by shifting microglial M1/M2 polarization. J Neuroinflamm. 2020;17(1):47.
Kigerl KA, Gensel JC, Ankeny DP, Alexander JK, Donnelly DJ, Popovich PG. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J Neurosci. 2009;29(43):13435–44.
David S, Kroner A. Repertoire of microglial and macrophage responses after spinal cord injury. Nat Rev Neurosci. 2011;12(7):388–99.
Hines DJ, Hines RM, Mulligan SJ, Macvicar BA. Microglia processes block the spread of damage in the brain and require functional chloride channels. Glia. 2009;57(15):1610–8.
Perrin FE, Lacroix S, Avilés-Trigueros M, David S. Involvement of monocyte chemoattractant protein-1, macrophage inflammatory protein-1alpha and interleukin-1beta in Wallerian degeneration. Brain. 2005;128(Pt 4):854–66.
Beck KD, Nguyen HX, Galvan MD, Salazar DL, Woodruff TM, Anderson AJ. Quantitative analysis of cellular inflammation after traumatic spinal cord injury: evidence for a multiphasic inflammatory response in the acute to chronic environment. Brain. 2010;133(Pt 2):433–47.
Conti A, Miscusi M, Cardali S, Germanò A, Suzuki H, Cuzzocrea S, Tomasello F. Nitric oxide in the injured spinal cord: synthases cross-talk, oxidative stress and inflammation. Brain Res Rev. 2007;54(1):205–18.
Bains M, Hall ED. Antioxidant therapies in traumatic brain and spinal cord injury. Biochim Biophys Acta. 2012;1822(5):675–84.
Fan H, Tang HB, Kang J, Shan L, Song H, Zhu K, Wang J, Ju G, Wang YZ. Involvement of endoplasmic reticulum stress in the necroptosis of microglia/macrophages after spinal cord injury. Neuroscience. 2015;311:362–73.
Fan H, Tang HB, Shan LQ, Liu SC, Huang DG, Chen X, Chen Z, Yang M, Yin XH, Yang H, Hao DJ. Quercetin prevents necroptosis of oligodendrocytes by inhibiting macrophages/microglia polarization to M1 phenotype after spinal cord injury in rats. J Neuroinflamm. 2019;16(1):206.
Alizadeh A, Dyck SM, Karimi-Abdolrezaee S. Traumatic spinal cord injury: an overview of pathophysiology, models and acute injury mechanisms. Front Neurol. 2019;10:282.
Tran AP, Warren PM, Silver J. The biology of regeneration failure and success after spinal cord injury. Physiol Rev. 2018;98(2):881–917.
Hassannejad Z, Yousefifard M, Azizi Y, Zadegan SA, Sajadi K, Sharif-Alhoseini M, Shakouri-Motlagh A, Mokhatab M, Rezvan M, Shokraneh F, Hosseini M, Vaccaro AR, Harrop JS, Rahimi-Movaghar V. Axonal degeneration and demyelination following traumatic spinal cord injury: a systematic review and meta-analysis. J Chem Neuroanat. 2019;97:9–22.
Ma L, Yu H, Gan S, Gong R, Mou K, Xue J, Sun S. p53-Mediated oligodendrocyte apoptosis initiates demyelination after compressed spinal cord injury by enhancing ER-mitochondria interaction and E2F1 expression. Neurosci Lett. 2017;644:55–61.
Cheng L, Cai B, Lu D, Zeng H. The role of mitochondrial energy metabolism in neuroprotection and axonal regeneration after spinal cord injury. Mitochondrion. 2023;69:57–63.
Sheng Z-H, Cai Q. Mitochondrial transport in neurons: impact on synaptic homeostasis and neurodegeneration. Nat Rev Neurosci. 2012;13(2):77–93.
Li J, Wang Q, Wang H, Wu Y, Yin J, Chen J, Zheng Z, Jiang T, Xie L, Wu F, Zhang H, Li X, Xu H, Xiao J. Lentivirus mediating FGF13 enhances axon regeneration after spinal cord injury by stabilizing microtubule and improving mitochondrial function. J Neurotrauma. 2017;35(3):548–59.
McKerracher L, David S, Jackson DL, Kottis V, Dunn RJ, Braun PE. Identification of myelin-associated glycoprotein as a major myelin-derived inhibitor of neurite growth. Neuron. 1994;13(4):805–11.
Mukhopadhyay G, Doherty P, Walsh FS, Crocker PR, Filbin MT. A novel role for myelin-associated glycoprotein as an inhibitor of axonal regeneration. Neuron. 1994;13(3):757–67.
Caroni P, Schwab ME. Two membrane protein fractions from rat central myelin with inhibitory properties for neurite growth and fibroblast spreading. J Cell Biol. 1988;106(4):1281–8.
Chen MS, Huber AB, van der Haar ME, Frank M, Schnell L, Spillmann AA, Christ F, Schwab ME. Nogo-A is a myelin-associated neurite outgrowth inhibitor and an antigen for monoclonal antibody IN-1. Nature. 2000;403(6768):434–9.
Kottis V, Thibault P, Mikol D, Xiao ZC, Zhang R, Dergham P, Braun PE. Oligodendrocyte-myelin glycoprotein (OMgp) is an inhibitor of neurite outgrowth. J Neurochem. 2002;82(6):1566–9.
Chung WS, Clarke LE, Wang GX, Stafford BK, Sher A, Chakraborty C, Joung J, Foo LC, Thompson A, Chen C, Smith SJ, Barres BA. Astrocytes mediate synapse elimination through MEGF10 and MERTK pathways. Nature. 2013;504(7480):394–400.
Allen NJ, Bennett ML, Foo LC, Wang GX, Chakraborty C, Smith SJ, Barres BA. Astrocyte glypicans 4 and 6 promote formation of excitatory synapses via GluA1 AMPA receptors. Nature. 2012;486(7403):410–4.
Kucukdereli H, Allen NJ, Lee AT, Feng A, Ozlu MI, Conatser LM, Chakraborty C, Workman G, Weaver M, Sage EH, Barres BA, Eroglu C. Control of excitatory CNS synaptogenesis by astrocyte-secreted proteins Hevin and SPARC. Proc Natl Acad Sci U S A. 2011;108(32):E440–9.
Bush TG, Puvanachandra N, Horner CH, Polito A, Ostenfeld T, Svendsen CN, Mucke L, Johnson MH, Sofroniew MV. Leukocyte infiltration, neuronal degeneration, and neurite outgrowth after ablation of scar-forming, reactive astrocytes in adult transgenic mice. Neuron. 1999;23(2):297–308.
Hara M, Kobayakawa K, Ohkawa Y, Kumamaru H, Yokota K, Saito T, Kijima K, Yoshizaki S, Harimaya K, Nakashima Y, Okada S. Interaction of reactive astrocytes with type I collagen induces astrocytic scar formation through the integrin-N-cadherin pathway after spinal cord injury. Nat Med. 2017;23(7):818–28.
Silver J, Miller JH. Regeneration beyond the glial scar. Nat Rev Neurosci. 2004;5(2):146–56.
Armulik A, Genové G, Betsholtz C. Pericytes: developmental, physiological, and pathological perspectives, problems, and promises. Dev Cell. 2011;21(2):193–215.
Hall CN, Reynell C, Gesslein B, Hamilton NB, Mishra A, Sutherland BA, O’Farrell FM, Buchan AM, Lauritzen M, Attwell D. Capillary pericytes regulate cerebral blood flow in health and disease. Nature. 2014;508(7494):55–60.
Anderson MA, Burda JE, Ren Y, Ao Y, O'Shea TM, Kawaguchi R, Coppola G, Khakh BS, Deming TJ, Sofroniew MV. Astrocyte scar formation aids central nervous system axon regeneration. Nature. 2016;532(7598):195–200.
Silver J. The glial scar is more than just astrocytes. Exp Neurol. 2016;286:147–9.
Dias DO, Kim H, Holl D, Werne Solnestam B, Lundeberg J, Carlén M, Göritz C, Frisén J. Reducing pericyte-derived scarring promotes recovery after spinal cord injury. Cell. 2018;173(1):153-65.e22.
Cheng Z, Zhu W, Cao K, Wu F, Li J, Wang G, Li H, Lu M, Ren Y, He X. Anti-inflammatory mechanism of neural stem cell transplantation in spinal cord injury. Int J Mol Sci. 2016;17(9):1380.
Kokaia Z, Lindvall O. Sensors of succinate: neural stem cell grafts fight neuroinflammation. Cell Stem Cell. 2018;22(3):283–5.
Peruzzotti-Jametti L, Bernstock JD, Vicario N, Costa ASH, Kwok CK, Leonardi T, Booty LM, Bicci I, Balzarotti B, Volpe G, Mallucci G, Manferrari G, Donegà M, Iraci N, Braga A, Hallenbeck JM, Murphy MP, Edenhofer F, Frezza C, Pluchino S. Macrophage-derived extracellular succinate licenses neural stem cells to suppress chronic neuroinflammation. Cell Stem Cell. 2018;22(3):355-68.e13.
Jeong JO, Han JW, Kim JM, Cho HJ, Park C, Lee N, Kim DW, Yoon YS. Malignant tumor formation after transplantation of short-term cultured bone marrow mesenchymal stem cells in experimental myocardial infarction and diabetic neuropathy. Circ Res. 2011;108(11):1340–7.
Wang X, Botchway BOA, Zhang Y, Yuan J, Liu X. Combinational treatment of bioscaffolds and extracellular vesicles in spinal cord injury. Front Mol Neurosci. 2019;12:81.
Liu W, Wang Y, Gong F, Rong Y, Luo Y, Tang P, Zhou Z, Zhou Z, Xu T, Jiang T, Yang S, Yin G, Chen J, Fan J, Cai W. Exosomes derived from bone mesenchymal stem cells repair traumatic spinal cord injury by suppressing the activation of A1 neurotoxic reactive astrocytes. J Neurotrauma. 2019;36(3):469–84.
Webb RL, Kaiser EE, Scoville SL, Thompson TA, Fatima S, Pandya C, Sriram K, Swetenburg RL, Vaibhav K, Arbab AS, Baban B, Dhandapani KM, Hess DC, Hoda MN, Stice SL. Human neural stem cell extracellular vesicles improve tissue and functional recovery in the murine thromboembolic stroke model. Transl Stroke Res. 2018;9(5):530–9.
Tan HL, Teow SY, Pushpamalar J. Application of metal nanoparticle hydrogel composites in tissue regeneration. Bioengineering (Basel). 2019;6(1):17.
Chen J, Zhang C, Li S, Li Z, Lai X, Xia Q. Exosomes derived from nerve stem cells loaded with FTY720 promote the recovery after spinal cord injury in rats by PTEN/AKT signal pathway. J Immunol Res. 2021;2021:8100298.
Zhong D, Cao Y, Li CJ, Li M, Rong ZJ, Jiang L, Guo Z, Lu HB, Hu JZ. Neural stem cell-derived exosomes facilitate spinal cord functional recovery after injury by promoting angiogenesis. Exp Biol Med (Maywood). 2020;245(1):54–65.
Zhang L, Han P. Neural stem cell-derived exosomes suppress neuronal cell apoptosis by activating autophagy via miR-374-5p/STK-4 axis in spinal cord injury. J Musculoskelet Neuronal Interact. 2022;22(3):411–21.
Jessen KR, Mirsky R, Lloyd AC. Schwann cells: development and role in nerve repair. Cold Spring Harb Perspect Biol. 2015;7(7):a020487.
Woodhoo A, Sahni V, Gilson J, Setzu A, Franklin RJ, Blakemore WF, Mirsky R, Jessen KR. Schwann cell precursors: a favourable cell for myelin repair in the central nervous system. Brain. 2007;130(Pt 8):2175–85.
Toft A, Tome M, Barnett SC, Riddell JS. A comparative study of glial and non-neural cell properties for transplant-mediated repair of the injured spinal cord. Glia. 2013;61(4):513–28.
Webber C, Zochodne D. The nerve regenerative microenvironment: early behavior and partnership of axons and Schwann cells. Exp Neurol. 2010;223(1):51–9.
Ching RC, Wiberg M, Kingham PJ. Schwann cell-like differentiated adipose stem cells promote neurite outgrowth via secreted exosomes and RNA transfer. Stem Cell Res Ther. 2018;9(1):266.
Wong FC, Ye L, Demir IE, Kahlert C. Schwann cell-derived exosomes: Janus-faced mediators of regeneration and disease. Glia. 2022;70(1):20–34.
Huang JH, Chen YN, He H, Fu CH, Xu ZY, Lin FY. Schwann cells-derived exosomes promote functional recovery after spinal cord injury by promoting angiogenesis. Front Cell Neurosci. 2022;16:1077071.
Ren J, Zhu B, Gu G, Zhang W, Li J, Wang H, Wang M, Song X, Wei Z, Feng S. Schwann cell-derived exosomes containing MFG-E8 modify macrophage/microglial polarization for attenuating inflammation via the SOCS3/STAT3 pathway after spinal cord injury. Cell Death Dis. 2023;14(1):70.
Pan D, Zhu S, Zhang W, Wei Z, Yang F, Guo Z, Ning G, Feng S. Autophagy induced by Schwann cell-derived exosomes promotes recovery after spinal cord injury in rats. Biotechnol Lett. 2022;44(1):129–42.
Pan D, Li Y, Yang F, Lv Z, Zhu S, Shao Y, Huang Y, Ning G, Feng S. Increasing toll-like receptor 2 on astrocytes induced by Schwann cell-derived exosomes promotes recovery by inhibiting CSPGs deposition after spinal cord injury. J Neuroinflamm. 2021;18(1):172.
Pashoutan Sarvar D, Shamsasenjan K, Akbarzadehlaleh P. Mesenchymal stem cell-derived exosomes: new opportunity in cell-free therapy. Adv Pharm Bull. 2016;6(3):293–9.
Guy R, Offen D. Promising opportunities for treating neurodegenerative diseases with mesenchymal stem cell-derived exosomes. Biomolecules. 2020;10(9):1320.
Yuan X, Wu Q, Wang P, Jing Y, Yao H, Tang Y, Li Z, Zhang H, Xiu R. Exosomes derived from pericytes improve microcirculation and protect blood-spinal cord barrier after spinal cord injury in mice. Front Neurosci. 2019;13:319.
Zhang C, Zhang C, Xu Y, Li C, Cao Y, Li P. Exosomes derived from human placenta-derived mesenchymal stem cells improve neurologic function by promoting angiogenesis after spinal cord injury. Neurosci Lett. 2020;739:135399.
Zhou W, Silva M, Feng C, Zhao S, Liu L, Li S, Zhong J, Zheng W. Exosomes derived from human placental mesenchymal stem cells enhanced the recovery of spinal cord injury by activating endogenous neurogenesis. Stem Cell Res Ther. 2021;12(1):174.
Sun G, Li G, Li D, Huang W, Zhang R, Zhang H, Duan Y, Wang B. hucMSC derived exosomes promote functional recovery in spinal cord injury mice via attenuating inflammation. Mater Sci Eng C Mater Biol Appl. 2018;89:194–204.
Wang L, Pei S, Han L, Guo B, Li Y, Duan R, Yao Y, Xue B, Chen X, Jia Y. Mesenchymal stem cell-derived exosomes reduce A1 astrocytes via downregulation of phosphorylated NFκB P65 subunit in spinal cord injury. Cell Physiol Biochem. 2018;50(4):1535–59.
Fan L, Dong J, He X, Zhang C, Zhang T. Bone marrow mesenchymal stem cells-derived exosomes reduce apoptosis and inflammatory response during spinal cord injury by inhibiting the TLR4/MyD88/NF-κB signaling pathway. Hum Exp Toxicol. 2021;40(10):1612–23.
Liu C, Hu F, Jiao G, Guo Y, Zhou P, Zhang Y, Zhang Z, Yi J, You Y, Li Z, Wang H, Zhang X. Dental pulp stem cell-derived exosomes suppress M1 macrophage polarization through the ROS-MAPK-NFκB P65 signaling pathway after spinal cord injury. J Nanobiotechnol. 2022;20(1):65.
Xin W, Qiang S, Jianing D, Jiaming L, Fangqi L, Bin C, Yuanyuan C, Guowang Z, Jianguang X, Xiaofeng L. Human bone marrow mesenchymal stem cell-derived exosomes attenuate blood-spinal cord barrier disruption via the TIMP2/MMP pathway after acute spinal cord injury. Mol Neurobiol. 2021;58(12):6490–504.
Chen Y, Tian Z, He L, Liu C, Wang N, Rong L, Liu B. Exosomes derived from miR-26a-modified MSCs promote axonal regeneration via the PTEN/AKT/mTOR pathway following spinal cord injury. Stem Cell Res Ther. 2021;12(1):224.
Kang J, Li Z, Zhi Z, Wang S, Xu G. MiR-21 derived from the exosomes of MSCs regulates the death and differentiation of neurons in patients with spinal cord injury. Gene Ther. 2019;26(12):491–503.
Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta Neuropathol. 2010;119(1):7–35.
Sofroniew MV. Astrocyte reactivity: subtypes, states, and functions in CNS innate immunity. Trends Immunol. 2020;41(9):758–70.
Taylor AR, Robinson MB, Gifondorwa DJ, Tytell M, Milligan CE. Regulation of heat shock protein 70 release in astrocytes: role of signaling kinases. Dev Neurobiol. 2007;67(13):1815–29.
Wang S, Cesca F, Loers G, Schweizer M, Buck F, Benfenati F, Schachner M, Kleene R. Synapsin I is an oligomannose-carrying glycoprotein, acts as an oligomannose-binding lectin, and promotes neurite outgrowth and neuronal survival when released via glia-derived exosomes. J Neurosci. 2011;31(20):7275–90.
Chaudhuri AD, Dastgheyb RM, Yoo SW, Trout A, Talbot CC Jr, Hao H, Witwer KW, Haughey NJ. TNFα and IL-1β modify the miRNA cargo of astrocyte shed extracellular vesicles to regulate neurotrophic signaling in neurons. Cell Death Dis. 2018;9(3):363.
Long X, Yao X, Jiang Q, Yang Y, He X, Tian W, Zhao K, Zhang H. Astrocyte-derived exosomes enriched with miR-873a-5p inhibit neuroinflammation via microglia phenotype modulation after traumatic brain injury. J Neuroinflamm. 2020;17(1):89.
Chen W, Zheng P, Hong T, Wang Y, Liu N, He B, Zou S, Ren D, Duan J, Zhao L, Feng J. Astrocytes-derived exosomes induce neuronal recovery after traumatic brain injury via delivering gap junction alpha 1–20 k. J Tissue Eng Regen Med. 2020;14(3):412–23.
Wu W, Liu J, Yang C, Xu Z, Huang J, Lin J. Astrocyte-derived exosome-transported microRNA-34c is neuroprotective against cerebral ischemia/reperfusion injury via TLR7 and the NF-κB/MAPK pathways. Brain Res Bull. 2020;163:84–94.
Vajen T, Mause SF, Koenen RR. Microvesicles from platelets: novel drivers of vascular inflammation. Thromb Haemost. 2015;114(2):228–36.
Melki I, Tessandier N, Zufferey A, Boilard E. Platelet microvesicles in health and disease. Platelets. 2017;28(3):214–21.
Johnson J, Wu YW, Blyth C, Lichtfuss G, Goubran H, Burnouf T. Prospective therapeutic applications of platelet extracellular vesicles. Trends Biotechnol. 2021;39(6):598–612.
Boilard E. Extracellular vesicles and their content in bioactive lipid mediators: more than a sack of microRNA. J Lipid Res. 2018;59(11):2037–46.
Brill A, Dashevsky O, Rivo J, Gozal Y, Varon D. Platelet-derived microparticles induce angiogenesis and stimulate post-ischemic revascularization. Cardiovasc Res. 2005;67(1):30–8.
Li Q, Song Y, Wang Q, Chen J, Gao J, Tan H, Li S, Wu Y, Yang H, Huang H, Yu Y, Li Y, Zhang N, Huang Z, Pang Z, Qian J, Ge J. Engineering extracellular vesicles with platelet membranes fusion enhanced targeted therapeutic angiogenesis in a mouse model of myocardial ischemia reperfusion. Theranostics. 2021;11(8):3916–31.
Hayon Y, Dashevsky O, Shai E, Brill A, Varon D, Leker RR. Platelet microparticles induce angiogenesis and neurogenesis after cerebral ischemia. Curr Neurovasc Res. 2012;9(3):185–92.
Ma Q, Fan Q, Han X, Dong Z, Xu J, Bai J, Tao W, Sun D, Wang C. Platelet-derived extracellular vesicles to target plaque inflammation for effective anti-atherosclerotic therapy. J Control Release. 2021;329:445–53.
Yao Y, Sun W, Sun Q, Jing B, Liu S, Liu X, Shen G, Chen R, Wang H. Platelet-derived exosomal microRNA-25-3p inhibits coronary vascular endothelial cell inflammation through adam10 via the NF-κB signaling pathway in ApoE(−/−) mice. Front Immunol. 2019;10:2205.
Mause SF, Ritzel E, Liehn EA, Hristov M, Bidzhekov K, Müller-Newen G, Soehnlein O, Weber C. Platelet microparticles enhance the vasoregenerative potential of angiogenic early outgrowth cells after vascular injury. Circulation. 2010;122(5):495–506.
Lopez E, Srivastava AK, Burchfield J, Wang YW, Cardenas JC, Togarrati PP, Miyazawa B, Gonzalez E, Holcomb JB, Pati S, Wade CE. Platelet-derived- extracellular vesicles promote hemostasis and prevent the development of hemorrhagic shock. Sci Rep. 2019;9(1):17676.
Guo SC, Tao SC, Yin WJ, Qi X, Yuan T, Zhang CQ. Exosomes derived from platelet-rich plasma promote the re-epithelization of chronic cutaneous wounds via activation of YAP in a diabetic rat model. Theranostics. 2017;7(1):81–96.
Xu N, Wang L, Guan J, Tang C, He N, Zhang W, Fu S. Wound healing effects of a Curcuma zedoaria polysaccharide with platelet-rich plasma exosomes assembled on chitosan/silk hydrogel sponge in a diabetic rat model. Int J Biol Macromol. 2018;117:102–7.
Ma Q, Fan Q, Xu J, Bai J, Han X, Dong Z, Zhou X, Liu Z, Gu Z, Wang C. Calming cytokine storm in pneumonia by targeted delivery of TPCA-1 using platelet-derived extracellular vesicles. Matter. 2020;3(1):287–301.
Tao SC, Yuan T, Rui BY, Zhu ZZ, Guo SC, Zhang CQ. Exosomes derived from human platelet-rich plasma prevent apoptosis induced by glucocorticoid-associated endoplasmic reticulum stress in rat osteonecrosis of the femoral head via the Akt/Bad/Bcl-2 signal pathway. Theranostics. 2017;7(3):733–50.
Liu X, Wang L, Ma C, Wang G, Zhang Y, Sun S. Exosomes derived from platelet-rich plasma present a novel potential in alleviating knee osteoarthritis by promoting proliferation and inhibiting apoptosis of chondrocyte via Wnt/β-catenin signaling pathway. J Orthop Surg Res. 2019;14(1):470.
Zhang X-M, Chen D-G, Li SC, Zhu B, Li Z-J. Embryonic origin and subclonal evolution of tumor-associated macrophages imply preventive care for cancer. Cells. 2021;10(4):903.
Gensel JC, Zhang B. Macrophage activation and its role in repair and pathology after spinal cord injury. Brain Res. 2015;1619:1–11.
Kong X, Gao J. Macrophage polarization: a key event in the secondary phase of acute spinal cord injury. J Cell Mol Med. 2017;21(5):941–54.
Zajac E, Schweighofer B, Kupriyanova TA, Juncker-Jensen A, Minder P, Quigley JP, Deryugina EI. Angiogenic capacity of M1- and M2-polarized macrophages is determined by the levels of TIMP-1 complexed with their secreted proMMP-9. Blood. 2013;122(25):4054–67.
Jetten N, Verbruggen S, Gijbels MJ, Post MJ, De Winther MP, Donners MM. Anti-inflammatory M2, but not pro-inflammatory M1 macrophages promote angiogenesis in vivo. Angiogenesis. 2014;17(1):109–18.
Huang JH, He H, Chen YN, Liu Z, Romani MD, Xu ZY, Xu Y, Lin FY. Exosomes derived from M2 macrophages improve angiogenesis and functional recovery after spinal cord injury through HIF-1α/VEGF axis. Brain Sci. 2022;12(10):1322.
Peng P, Yu H, Xing C, Tao B, Li C, Huang J, Ning G, Zhang B, Feng S. Exosomes-mediated phenotypic switch of macrophages in the immune microenvironment after spinal cord injury. Biomed Pharmacother. 2021;144:112311.
Zhang B, Lin F, Dong J, Liu J, Ding Z, Xu J. Peripheral macrophage-derived exosomes promote repair after spinal cord injury by inducing local anti-inflammatory type microglial polarization via increasing autophagy. Int J Biol Sci. 2021;17(5):1339–52.
Ge X, Zhou Z, Yang S, Ye W, Wang Z, Wang J, Xiao C, Cui M, Zhou J, Zhu Y, Wang R, Gao Y, Wang H, Tang P, Zhou X, Wang C, Cai W. Exosomal USP13 derived from microvascular endothelial cells regulates immune microenvironment and improves functional recovery after spinal cord injury by stabilizing IκBα. Cell Biosci. 2023;13(1):55.
Li J, Jing Y, Bai F, Wu Y, Wang L, Yan Y, Jia Y, Yu Y, Jia B, Ali F. Induced pluripotent stem cells as natural biofactories for exosomes carrying miR-199b-5p in the treatment of spinal cord injury. Front Pharmacol. 2022;13:1078761.
Li C, Qin T, Liu Y, Wen H, Zhao J, Luo Z, Peng W, Lu H, Duan C, Cao Y, Hu J. Microglia-derived exosomal microRNA-151-3p enhances functional healing after spinal cord injury by attenuating neuronal apoptosis via regulating the p53/p21/CDK1 signaling pathway. Front Cell Dev Biol. 2021;9:783017.
Peng W, Wan L, Luo Z, Xie Y, Liu Y, Huang T, Lu H, Hu J. Microglia-derived exosomes improve spinal cord functional recovery after injury via inhibiting oxidative stress and promoting the survival and function of endothelia cells. Oxid Med Cell Longev. 2021;2021:1695087.
Huang S, Ge X, Yu J, Han Z, Yin Z, Li Y, Chen F, Wang H, Zhang J, Lei P. Increased miR-124-3p in microglial exosomes following traumatic brain injury inhibits neuronal inflammation and contributes to neurite outgrowth via their transfer into neurons. Faseb J. 2018;32(1):512–28.
Huppert LA, Green MD, Kim L, Chow C, Leyfman Y, Daud AI, Lee JC. Tissue-specific Tregs in cancer metastasis: opportunities for precision immunotherapy. Cell Mol Immunol. 2022;19(1):33–45.
Xiong W, Li C, Kong G, Zeng Q, Wang S, Yin G, Gu J, Fan J. Treg cell-derived exosomes miR-709 attenuates microglia pyroptosis and promotes motor function recovery after spinal cord injury. J Nanobiotechnol. 2022;20(1):529.
Park E, Velumian AA, Fehlings MG. The role of excitotoxicity in secondary mechanisms of spinal cord injury: a review with an emphasis on the implications for white matter degeneration. J Neurotrauma. 2004;21(6):754–74.
Shao C, Chen Y, Yang T, Zhao H, Li D. Mesenchymal stem cell derived exosomes suppress neuronal cell ferroptosis via lncGm36569/miR-5627-5p/FSP1 axis in acute spinal cord injury. Stem Cell Rev Rep. 2022;18(3):1127–42.
Yuan B, Pan S, Dong YQ, Zhang WW, He XD. Effect of exosomes derived from mir-126-modified mesenchymal stem cells on the repair process of spinal cord injury in rats. Eur Rev Med Pharmacol Sci. 2020;24(2):483–90.
Li D, Zhang P, Yao X, Li H, Shen H, Li X, Wu J, Lu X. Exosomes derived from miR-133b-modified mesenchymal stem cells promote recovery after spinal cord injury. Front Neurosci. 2018;12:845.
Li S, Dinh HTP, Matsuyama Y, Sato K, Yamagishi S. Molecular mechanisms in the vascular and nervous systems following traumatic spinal cord injury. Life (Basel). 2022;13(1):9.
Yates AG, Anthony DC, Ruitenberg MJ, Couch Y. Systemic immune response to traumatic CNS injuries-are extracellular vesicles the missing link? Front Immunol. 2019;10:2723.
Kang J, Guo Y. Human umbilical cord mesenchymal stem cells derived exosomes promote neurological function recovery in a rat spinal cord injury model. Neurochem Res. 2022;47(6):1532–40.
Beattie MS, Farooqui AA, Bresnahan JC. Review of current evidence for apoptosis after spinal cord injury. J Neurotrauma. 2000;17(10):915–25.
Kuzhandaivel A, Nistri A, Mazzone GL, Mladinic M. Molecular mechanisms underlying cell death in spinal networks in relation to locomotor activity after acute injury in vitro. Front Cell Neurosci. 2011;5:9.
Zhang A, Bai Z, Yi W, Hu Z, Hao J. Overexpression of miR-338-5p in exosomes derived from mesenchymal stromal cells provides neuroprotective effects by the Cnr1/Rap1/Akt pathway after spinal cord injury in rats. Neurosci Lett. 2021;761:136124.
Tian F, Yang J, Xia R. Exosomes secreted from circZFHX3-modified mesenchymal stem cells repaired spinal cord injury through mir-16-5p/IGF-1 in mice. Neurochem Res. 2022;47(7):2076–89.
Dong Y, Yong VW. Oxidized phospholipids as novel mediators of neurodegeneration. Trends Neurosci. 2022;45(6):419–29.
Kumar S, Theis T, Tschang M, Nagaraj V, Berthiaume F. Reactive oxygen species and pressure ulcer formation after traumatic injury to spinal cord and brain. Antioxidants (Basel). 2021;10(7):1013.
Liu J, Lin M, Qiao F, Zhang C. Exosomes derived from lncRNA TCTN2-modified mesenchymal stem cells improve spinal cord injury by miR-329-3p/IGF1R axis. J Mol Neurosci. 2022;72(3):482–95.
Feng J, Zhang Y, Zhu Z, Gu C, Waqas A, Chen L. Emerging exosomes and exosomal MiRNAs in spinal cord injury. Front Cell Dev Biol. 2021;9:703989.
Fan L, Liu C, Chen X, Zheng L, Zou Y, Wen H, Guan P, Lu F, Luo Y, Tan G, Yu P, Chen D, Deng C, Sun Y, Zhou L, Ning C. Exosomes-loaded electroconductive hydrogel synergistically promotes tissue repair after spinal cord injury via immunoregulation and enhancement of myelinated axon growth. Adv Sci (Weinh). 2022;9(13):e2105586.
Mol EA, Lei Z, Roefs MT, Bakker MH, Goumans MJ, Doevendans PA, Dankers PYW, Vader P, Sluijter JPG. Injectable supramolecular ureidopyrimidinone hydrogels provide sustained release of extracellular vesicle therapeutics. Adv Healthc Mater. 2019;8(20):e1900847.
Li L, Zhang Y, Mu J, Chen J, Zhang C, Cao H, Gao J. Transplantation of human mesenchymal stem-cell-derived exosomes immobilized in an adhesive hydrogel for effective treatment of spinal cord injury. Nano Lett. 2020;20(6):4298–305.
Wang C, Wang M, Xia K, Wang J, Cheng F, Shi K, Ying L, Yu C, Xu H, Xiao S, Liang C, Li F, Lei B, Chen Q. A bioactive injectable self-healing anti-inflammatory hydrogel with ultralong extracellular vesicles release synergistically enhances motor functional recovery of spinal cord injury. Bioact Mater. 2021;6(8):2523–34.
Mu J, Li L, Wu J, Huang T, Zhang Y, Cao J, Ma T, Chen J, Zhang C, Zhang X, Lu T, Kong X, Sun J, Gao J. Hypoxia-stimulated mesenchymal stem cell-derived exosomes loaded by adhesive hydrogel for effective angiogenic treatment of spinal cord injury. Biomater Sci. 2022;10(7):1803–11.
Mu J, Wu J, Cao J, Ma T, Li L, Feng S, Gao J. Rapid and effective treatment of traumatic spinal cord injury using stem cell derived exosomes. Asian J Pharm Sci. 2021;16(6):806–15.
Liu WZ, Ma ZJ, Li JR, Kang XW. Mesenchymal stem cell-derived exosomes: therapeutic opportunities and challenges for spinal cord injury. Stem Cell Res Ther. 2021;12(1):102.
Zeng J, Gu C, Sun Y, Chen X. Engineering of M2 macrophages-derived exosomes via click chemistry for spinal cord injury repair. Adv Healthc Mater. 2023;12:2203391.
Gao ZS, Zhang CJ, Xia N, Tian H, Li DY, Lin JQ, Mei XF, Wu C. Berberine-loaded M2 macrophage-derived exosomes for spinal cord injury therapy. Acta Biomater. 2021;126:211–23.
Fan Y, Li Y, Huang S, Xu H, Li H, Liu B. Resveratrol-primed exosomes strongly promote the recovery of motor function in SCI rats by activating autophagy and inhibiting apoptosis via the PI3K signaling pathway. Neurosci Lett. 2020;736:135262.
Zhang J, Li S, Li L, Li M, Guo C, Yao J, Mi S. Exosome and exosomal microRNA: trafficking, sorting, and function. Genom Proteom Bioinform. 2015;13(1):17–24.
Samanta S, Rajasingh S, Drosos N, Zhou Z, Dawn B, Rajasingh J. Exosomes: new molecular targets of diseases. Acta Pharmacol Sin. 2018;39(4):501–13.
Yamashita T, Takahashi Y, Takakura Y. Possibility of exosome-based therapeutics and challenges in production of exosomes eligible for therapeutic application. Biol Pharm Bull. 2018;41(6):835–42.
Charoenviriyakul C, Takahashi Y, Morishita M, Matsumoto A, Nishikawa M, Takakura Y. Cell type-specific and common characteristics of exosomes derived from mouse cell lines: yield, physicochemical properties, and pharmacokinetics. Eur J Pharm Sci. 2017;96:316–22.
Li P, Kaslan M, Lee SH, Yao J, Gao Z. Progress in exosome isolation techniques. Theranostics. 2017;7(3):789–804.
Barile L, Vassalli G. Exosomes: therapy delivery tools and biomarkers of diseases. Pharmacol Ther. 2017;174:63–78.
Gutierrez-Millan C, Calvo Díaz C, Lanao JM, Colino CI. Advances in exosomes-based drug delivery systems. Macromol Biosci. 2021;21(1):e2000269.
Schepici G, Silvestro S, Mazzon E. Regenerative effects of exosomes-derived MSCs: an overview on spinal cord injury experimental studies. Biomedicines. 2023;11(1):201.
Sheng X, Zhao J, Li M, Xu Y, Zhou Y, Xu J, He R, Lu H, Wu T, Duan C, Cao Y, Hu J. Bone marrow mesenchymal stem cell-derived exosomes accelerate functional recovery after spinal cord injury by promoting the phagocytosis of macrophages to clean myelin debris. Front Cell Dev Biol. 2021;9:772205.
Li S, Liao X, He Y, Chen R, Zheng WV, Tang M, Guo X, Chen J, Hu S, Sun J. Exosomes derived from NGF-overexpressing bone marrow mesenchymal stem cell sheet promote spinal cord injury repair in a mouse model. Neurochem Int. 2022;157:105339.
Chang Q, Hao Y, Wang Y, Zhou Y, Zhuo H, Zhao G. Bone marrow mesenchymal stem cell-derived exosomal microRNA-125a promotes M2 macrophage polarization in spinal cord injury by downregulating IRF5. Brain Res Bull. 2021;170:199–210.
Zhang M, Wang L, Huang S, He X. Exosomes with high level of miR-181c from bone marrow-derived mesenchymal stem cells inhibit inflammation and apoptosis to alleviate spinal cord injury. J Mol Histol. 2021;52(2):301–11.
Luo Y, Xu T, Liu W, Rong Y, Wang J, Fan J, Yin G, Cai W. Exosomes derived from GIT1-overexpressing bone marrow mesenchymal stem cells promote traumatic spinal cord injury recovery in a rat model. Int J Neurosci. 2021;131(2):170–82.
He X, Zhang J, Guo Y, Yang X, Huang Y, Hao D. Exosomal miR-9-5p derived from BMSCs alleviates apoptosis, inflammation and endoplasmic reticulum stress in spinal cord injury by regulating the HDAC5/FGF2 axis. Mol Immunol. 2022;145:97–108.
Luo Z, Peng W, Xu Y, Xie Y, Liu Y, Lu H, Cao Y, Hu J. Exosomal OTULIN from M2 macrophages promotes the recovery of spinal cord injuries via stimulating Wnt/β-catenin pathway-mediated vascular regeneration. Acta Biomater. 2021;136:519–32.
Acknowledgements
We thank Zhijia Ma and Ran Meng for identifying relevant literature in the manuscript and for editing the manuscript.
Funding
This research was supported by Jilin Provincial Science and Technology Department Project (YDZJ202301ZYTS032), Qinhuangdao Science & Technology Bureau (201902A119), Jilin Province Health Science and Technology Capability Enhancement Project (2023JC012) and Jilin University Bethune Plan Project.
Author information
Authors and Affiliations
Contributions
TY and JHJ wrote portions of the initial draft of this paper and modified the initial draft. LLY and YZ contributed to the figures editing. JHJ and MFW designed the work, edited the initial draft of this paper and made final changes to the final version before submission. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, T., Yang, LL., Zhou, Y. et al. Exosome-mediated repair of spinal cord injury: a promising therapeutic strategy. Stem Cell Res Ther 15, 6 (2024). https://doi.org/10.1186/s13287-023-03614-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-023-03614-y