Abstract
Background
Ring chromosomes can be formed by terminal breaks of two arms of a chromosome and their rejoining, leading to a loss of genetic material. They may also be formed by telomere-telomere fusions with no deletion, resulting in the formation of a complete ring. Mosaic X-ring chromosomes are extremely rare and have highly variable phenotypes. Here, we report a case with a mosaic X-ring chromosome in a patient with Turner syndrome, and we illustrate the unreported complicated mechanism using chromosome analysis and fluorescence in situ hybridization (FISH).
Case presentation
A 10-year-old girl of short stature presenting Turner syndrome was admitted to our hospital. The patient’s clinical characteristics were subsequently documented. Genetic analysis showed a karyotype of mostly 45,X[140]/46,X,r(X)[60]. The X ring chromosome was cytogenetically characterized as 45,X/46,X,r(X)(p22.32q21.1), with a length of approximately 74 Mb.
Conclusions
Taken together, we report a rare case with a mosaic X ring chromosome in Turner syndrome and we believe this case expands our collective knowledge of mosaic structural chromosomal disorders and provides new insight into clinical management and genetic counseling for Turner syndrome.
Similar content being viewed by others
Background
Turner syndrome (TS) occurs in approximately 1/300 to 1/2500 of newborn girls [1]. Its main clinical presentations are short stature, ovarian hypoplasia, webbed neck, valgus, and low hairline [2,3,4]. TS is a chromosomal disease derived from a complete or partial deletion or structural abnormality of the X chromosome. In addition, some TS patients carry a small supernumerary marker chromosome (sSMC) whose origin, characteristics, and structure have not yet been identified using traditional chromosome banding technology. In TS, the sSMC usually presents in the form of chimerism, which has its own formation and origin characteristics [5].
TS with an X-ring chromosome-related phenotype can present with mental disorders, learning difficulties, autism spectrum disorders, craniofacial abnormalities, cardiovascular diseases, and skeletal issues, as well as the other presentations associated with Turner syndrome. In addition to the common characteristics of TS, the clinical presentation of these patients depends on the origin, size, gene replication time, genes affected by changes in replication number, degree of mosaicism, and X inactivation status of the sSMC [4]. In the present study, we report a rare case who had common clinical features of TS and annular X chromosome with mosaics and a breaking point confined to the region Xp22.32-q21.1 in the X chromosome.
Case presentation
A 10-year-old female was admitted to our hospital with a past medical history of short stature and moderate intellectual development. She was born to a 22-year-old G1P1 female at 40 weeks via vaginal delivery, with no special conditions during pregnancy. The patient’s birth weight was 2945 g and the patient’s length was 46 cm. The patient’s family history was unremarkable for immediate family members in terms of Turner syndrome. No other family members presented learning or developmental disabilities and short stature. The patient’s parents denied consanguinity. The proband was developmentally delayed. She was followed by developmental pediatrics and received physical therapy. The clinical features of these cases are summarized in Table 1.
Methods
A cytogenetic microarray experiment was performed using a cyto-HD array according to the manufacturers’ instructions (Affymetrix, Inc., Santa Clara, CA, USA). Data was analyzed using Chromosome Analysis Suite (ChAS) software (Affymetrix, Inc., Santa Clara, CA, USA). High-resolution chromosome analysis was performed according to standard protocols. Fluorescence in situ hybridization (FISH) was performed using a Spectrum Green-labeled probe for the pericentromeric region of chromosome X(SRY/DXZ1). A total of 25 metaphase and 200 interphase cells were visualized using a fluorescence microscope (Olympus BX53, Japan). Follicular-stimulating hormone (FSH) and luteinizing hormone (LH) were measured using a chemiluminescence assay according to the manufacturer’s instructions (Beckman AU680 Controller Area Network CAN, USA).
Results
The case was a 10-year-old girl who was diagnosed with TS in 2021. She had short stature and ovarian dysplasia was observed by ultrasound examination (Fig. 1).
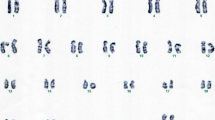
In this case, the level of FSH and LH measured was 82.9 and 17.86 mIU/ml, respectively (Table 1). Both FSH and LH were measured at higher levels than normal (3.82–10.54 mIU/ml for FSH and 1.85–12.19 mIU/ml for LH). Karyotyping revealed mosaicism for a ring X chromosome in two types of cells, with karyotypes 45,X and 46,X,r (X) (Fig. 2). The proportion of cells with 46,X,r(X) was 30%. The origin of the ring chromosome was next determined by FISH with a probe for the peri centromeric region of the X chromosome. The degree of mosaicism was further confirmed by scoring FISH signals from metaphase and interphase cells (Fig. 2).
Karyotype analysis. A, High resolution G-band karyotype (550–850 bands) of a cell showing 46 chromosomes, with an absent chromosome X (Left) and a small ring chromosome (Right). B, FISH with a specific centromeric X chromosome probe (DXZ1) showing two signals; one in the normal chromosome X and one in the small ring chromosome
According to ISCN 2020, the microarray karyotype could be written as arr[GRCh37] Xp22.33p22.32(168552_5051774) × 1, Xq21.1q28(80226215_155233098) × 1, Xp22.32q21.1(5905382_80163627) × 1–2. Cytogenetic microarray analysis revealed the exact locations of the breakage points on the arms of the X chromosome [45,X/46,X,r(X)(p22.32q21.1)] (Fig. 3). The length of the r(X) chromosome was found to be 74 Mb (Xp22.32 –Xq21.1), harboring 363 OMIM genes. The degree of mosaicism was determined from the cytogenetic microarray experiment by comparing the deviation in the probe intensity signals from baseline (Fig. 3).
Chromosome microarray analysis shows loss of Mosaic arr[GRCh37] Xp22.33p22.32(168552_5051774) × 1, Xq21.1q28(80226215_155233098) × 1, Xp22.32q21.1(5905382_80163627) × 1–2. The pink section represents the lost Mosaic. The ring X chromosome was about 74 Mb in size. The genomic location was chrX:5905382–80163627
Discussion
TS is a chromosomal disorder in females. Classic TS patients have the karyotype 45,X. Some other TS patients can present with mosaicism or have a structurally rearranged X karyotype [3]. Patients who carry a structurally abnormal X chromosome are a unique group, and they have provided opportunities to evaluate genotype/phenotype correlations in relation to X chromosome content and inactivation. Mosaicism karyotypes with structurally abnormal ring chromosomes are even rarer, accounting for only 5% of TS patients [2].
We here describe a 10 year old girl who had short stature and ovarian dysplasia. She was found to have a de novo mosaic 45,X/46,X, + r (p22.32q21.1) by cytogenetic analysis. The observed deletion of p22.32p22.33 [4.8 Mb] and Xq21.1-Xq28 was approximately 75 Mb in size, and harbored 605 genes. We found several similar cases associated with our case where a ring chromosome has been described previously. For example, the cases Xpter-Xp22.12 [21 MB] and Xq21.33-Xq28 [62 Mb] had more severe symptoms than our case, and these case’s deletion fragment contained 789 genes compared to our case, which only contained 605 [6]. This difference in symptom severity could be explained by the amount of X deletion and the number of genes contained in the deleted region. It was also possible that the difference in severity between the cases was due to differences in the degree of mosaicism for two cell lines 45, X and 46, Xr (X) (70:30 in ou case compared to 50:50 in the more sever case). However, it is difficult to ascertain the impact of mosaicism on clinical phenotype as level of mosaicism has been reported to go down with age due to the unstable nature of r (X) chromosomes.
Furthermore, we compared Xp deletions and clinical presentations in our case to those of previously reported cases that showed no evidence of ovarian dysgenesis with an Xp terminal deletion, Here, we report a rare case of TS with an X ring mosaicism karyotype of 45,X and 46,X, r(X)(p22.32q21.1). This case had an atypical phenotype. For example, her intellectual development did not lag behind her peers, and the patient’s breast development was Tanner stage 2. Other symptoms are described in Table 1. A case similar to ours (Xpter-Xp22.12 and Xpter-Xp22.31, respectively) had been reported in (Xp22.33-Xp22.12) without any sign of ovarian dysgenesis [7,8,9]. Therefore, we considered ovarian dysgenesis in our case might have been due to Xq deletion rather than Xp deletion.
Previous studies have found that ring X chromosomes, which are active, as defined by deficient XIST transcription, are present in females who have mental retardation and multiple congenital abnormalities [10, 11]. Small ring (X) chromosomes lacking the XIST gene have been associated with a severe phenotype that includes mental retardation, facial dysmorphism, and congenital abnormalities [10, 12]. It has been hypothesized that the loss of XIST results in functional disomy for the sequences contained in the ring. However, in our case, XIST was intact with the ring chromosome negating the role of XIST inactivation in the clinical phenotype of patients. Therefore, we believe that the results of ring X formation was most likely inactivation in our case.
Moreover, the loss of different genetic material leads to different clinical phenotypes in Turner syndrome, and the chromosomal karyotype and clinical phenotype are dependent. Short stature is the most common characteristic, and is caused by the perturbations of the SHOX gene on Xp22.3 [7, 8, 13]. The key region determining the development of female gonads is in Xq21-Xq27, and the disruption of these regions will lead to female ovarian dysplasia [14, 15]. Our case was consistent with the phenotype reported in previous studies. The clinical phenotype of our case was less severe than that of a classic 45X karyotype, which may be related to mosaicism of the ring X chromosome, but this is still as uncertain.
In summary, we describe the phenotype in terms of clinical symptoms, ultrasound diagnosis, and cytogenetics, of a girl with a rare genotype and TS. We discussed the similarities and differences between our case and other previously reported cases with similar genotypes. We used a combination of techniques and analysis of information from public gene databases (Decipher/Clingen/UCSC/Pubmed) to provide additional evidence to clarify the genotype-phenotypic associations of TS, which can facilitate further genetic counseling and enrich database information on TS.
Availability of data and materials
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.
References
Stochholm K, Juul S, Juel K, Naeraa RW, Gravholt CH. Prevalence, incidence, diagnostic delay, and mortality in Turner syndrome. J Clin Endocrinol Metab. 2006;91(10):3897–902.
Álvarez-Nava F, Soto M, Sanchez MA, Fernandez E, Lanes R. Molecular analysis in Turner syndrome. J Pediatr. 2003;142(3):336–40.
Gravholt CH, Viuff MH, Brun S, Stochholm K, Andersen NH. Turner syndrome: mechanisms and management. Nat Rev Endocrinol. 2019;15(10):601–14.
Morgan T. Turner syndrome: diagnosis and management. Am Fam Phys. 2007;76(3):405–10.
Chen J, Guo M, Luo M, Deng S, Tian Q. Clinical characteristics and management of Turner patients with a small supernumerary marker chromosome. Gynecol Endocrinol J Int Soc Gynecol Endocrinol. 2021;37(8):730–4.
Chauhan P, Jaiswal SK, Lakhotia AR, Rai AK. Molecular cytogenetic characterization of two Turner syndrome patients with mosaic ring X chromosome. J Assist Reprod Genet. 2016;33(9):1161–8.
Cho EH, Kim SY, Kim JK. A case of 9.7 Mb terminal Xp deletion including OA1 locus associated with contiguous gene syndrome. J Korean Med Sci. 2012;27(10):1273–7.
Zinn AR, Tonk VS, Chen Z, Flejter WL, Gardner HA, Guerra R, Kushner H, Schwartz S, Sybert VP, Van Dyke DL, Ross JL. Evidence for a Turner syndrome locus or loci at Xp112-p221. Am J Hum Genet. 1998;63(6):1757–66.
Lachlan KL, Youings S, Costa T, Jacobs PA, Thomas NS. A clinical and molecular study of 26 females with Xp deletions with special emphasis on inherited deletions. Hum Genet. 2006;118(5):640–51.
Migeon BR, Luo S, Stasiowski BA, Jani M, Axelman J, Van Dyke DL, Weiss L, Jacobs PA, Yang-Feng TL, Wiley JE. Deficient transcription of XIST from tiny ring X chromosomes in females with severe phenotypes. Proc Natl Acad Sci USA. 1993;90(24):12025–9.
Leppig KA, Sybert VP, Ross JL, Cunniff C, Trejo T, Raskind WH, Disteche CM. Phenotype and X inactivation in 45, X/46, X, r(X) cases. Am J Med Genet A. 2004;128A(3):276–84.
Turner C, Dennis NR, Skuse DH, Jacobs PA. Seven ring (X) chromosomes lacking the XIST locus, six with an unexpectedly mild phenotype. Hum Genet. 2000;106(1):93–100.
James RS, Coppin B, Dalton P, Dennis NR, Mitchell C, Sharp AJ, Skuse DH, Thomas NS, Jacobs PA. A study of females with deletions of the short arm of the X chromosome. Hum Genet. 1998;102(5):507–16.
Marozzi A, Manfredini E, Tibiletti MG, Furlan D, Villa N, Vegetti W, Crosignani PG, Ginelli E, Meneveri R, Dalpra L. Molecular definition of Xq common-deleted region in patients affected by premature ovarian failure. Hum Genet. 2000;107(4):304–11.
Sher ES, Addelston MB, Plotnick L, Urban MD, Berkovitz GD. Molecular investigation of two male subjects with short stature and a 45, X/46, X, ring(Y) karyotype. Horm Res. 1998;49(1):46–50.
Acknowledgements
We sincerely thank the patient for participation in the present study. We thank all the participants for their help and support, and especially for Zesen Zhu (Technical Support Center of Zhejiang Biosan Biochemical Technologies Co., Ltd.) for his support in genetic analysis. We thank LetPub (www.letpub.com) for linguistic assistance and pre-submission expert review.
Funding
This work was supported by a grant from the Natural Science Foundation of Hunan Province (2019JJ60080).
Author information
Authors and Affiliations
Contributions
H. Luo and Liu Ni recruited patients. Yi-Qiong Yang, Xiao-Min Zhang, Hongping Huang, and Sainan Tan performed experiments. Chen Ling, Li Liang, Ling Wang, Tang Dan, Shu-Xiang Zhou, and Chunliu Yang interpreted the data. H. Luo designed the study and reviewed all the data. H. Luo wrote the manuscript, and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Women and Children Healthcare Hospital of Zhu Zhou (No. 2017037). Written informed consent was obtained from the patient who participated in this study.
Consent for publication
Written informed consent was obtained for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Luo, H., Ni, L., Yang, YQ. et al. Characterization of a rare mosaic X-ring chromosome in a patient with Turner syndrome. Mol Cytogenet 15, 15 (2022). https://doi.org/10.1186/s13039-022-00593-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13039-022-00593-2