Abstract
Background
Altered axial biomechanics of the knee are recognized as a risk factor for non-contact anterior cruciate ligament (ACL) injury. However, the relationship of knee and segmental torsion to non-contact ACL and combined anterolateral ligament (ALL) injury is unclear. This study aims to determine the relationship of knee and segmental torsion to non-contact ACL injury and to explore their relationship with ALL injuries.
Methods
We divided 122 patients with arthroscopically confirmed non-contact ACL injuries into an ACL injury group (isolated ACL injury, 63 patients) and an ACL + ALL injury group (ACL combined with ALL injury,59 patients). Additionally, 90 normal patients with similar age, gender and body mass index (BMI) were matched as a control group. The tibial tubercle-trochlear groove (TT-TG) distance, distal femoral torsion (DFT), posterior femoral condylar torsion (PFCT) and proximal tibial torsion (PTT) were measured using magnetic resonance imaging (MRI). We assessed the differences between the groups using an independent samples t test and utilized receiver operating characteristic (ROC) curves to determine the cut-off value for the increased risk of ACL injury.
Results
In patients with ACL injury, the measurements of the TT-TG (11.8 ± 3.1 mm), DFT (7.7° ± 3.5°) and PFCT (3.6° ± 1.3°) were significantly higher compared to the control group (9.1 ± 2.4 mm, 6.3° ± 2.7° and 2.8° ± 1.3°, respectively; P < 0.05), but the PTT did not differ between the two groups. The TT-TG, DFT and PFCT were not significantly larger in patients combined with ALL injury. ROC curve analysis revealed ACL injury is associated with TT-TG, DFT and PFCT.
Conclusions
Knee torsional alignment is associated with ACL injury, predominantly in the distal femur rather than the proximal tibia. However, its correlation with ALL injury remains unclear. These findings may help identify patients at high risk for non-contact ACL injury and inform the development of targeted prevention and treatment strategies.
Similar content being viewed by others
Introduction
Non-contact anterior cruciate ligament (ACL) injury accounts for more than half of all ACL injuries [1]. This type of injury primarily results by the mechanism of pivot shift, whereby ACL injury occurs when the tibia is valgus and internally rotated relative to the femur during knee motion resulting in greater stresses on the ACL [2]. To prevent non-contact ACL injury, several studies have investigated possible risk factors such as body mass index (BMI), neuromuscular defects, hormone levels, joint laxity and sex [3,4,5,6,7]. Moreover, several morphological characteristics of the bones can affect the biomechanics of the knee and increase the risk of ACL injury [8,9,10,11].
In recent years, many studies have demonstrated that altered biomechanics in the transverse plane is the core of the mechanism of ACL injury, and abnormal torsion changes the rotational stresses and increases the risk of ACL injury [12,13,14]. Alpay et al. identified femoral anteversion leading to abnormal torsion of the infratrochanteric femur as a risk factor for ACL injury [14]. The tibial tubercle to trochlear groove (TT-TG) distance, an indicator of knee torsion, is an essential factor in non-contact ACL injury, and a larger TT-TG increases tibial internal rotation, exposing the ACL to greater tension, thus increasing the risk of injury [15,16,17]. Non-contact ACL injury is usually due to a pivot-shift mechanism resulting from the combined action of the femur and tibia [2]. Therefore, distal femoral torsion (DFT), posterior femoral condylar torsion (PFCT), and proximal tibial torsion (PTT) may cause non-contact ACL injuries.
The anterolateral ligament (ALL) plays an essential role in the rotational stability of the knee, and its injury results in greater rotational stress on the knee, which is usually accompanied by a more severe knee injury [18, 19]. However, whether knee torsion is correlated with ACL combined ALL injuries is unclear. Therefore, understanding the torsion of various knee components may provide new insights into the mechanism of non-contact ACL injury.
The objective of this study is to measure the TT-TG, DFT, PFCT and PTT using magnetic resonance imaging (MRI) to explore the association between knee torsion and non-contact ACL injury using segmental analysis and to explore their relationship with combined ALL injury.
Material and methods
This study was approved by the Ethics Committee of The First Affiliated Hospital of Chongqing Medical University (IRB, NO. 2019-345). Retrospective data were collected from 603 patients diagnosed with ACL injury at our centre between 2015 and 2022. The requirement for informed consent was waived because this was a retrospective imaging study.
Patient selection
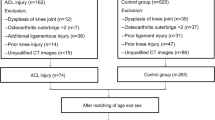
After the screening, 122 patients with non-contact ACL injury were included in the experimental group, which was divided into the ACL injury group comprising patients with isolated ACL injury (41 men, 22 women) and the ACL + ALL injury group consisting of patients with ACL + ALL injury (40 men and 19 women), based on the presence of combined ALL injury. Furthermore, 90 normal patients (60 men, 30 women), who had undergone knee MRI at our hospital, were included as the control group matched by sex and BMI. The inclusion criteria were:1. patients aged 18–50 years; 2. availability of complete preoperative radiographs, MRI and medical records; 3. ACL injuries were defined based on arthroscopy. The exclusion criteria were:1. patients with contact ACL injury; 2. patients with partial ACL injuries; 3. surgical history of the injured knee; 4. patients with joint or multiple ligament injuries, such as the posterior cruciate ligament, medial and lateral collateral ligament, and other injuries; 5. patients with Kellgren–Lawrence grades > 2; 6. patients with obvious valgus deformities; 7. general joint laxity. A detailed flowchart illustrating patient selection is presented in Fig. 1.
Data collection
Patients' demographics were reviewed from the medical reports. Coronal, sagittal and axial images of MRI were independently evaluated by two orthopaedic surgeons. For ALL status assessment, T2-weighted coronal plane images were utilized. ALL injury was defined as discontinuity of ALL fibres or with periligamentous oedema, or proximal or distal detachment, with or without Segond fracture [18, 20] (Fig. 2).
All MRI data were downloaded, and all parameters were measured using Radiant DICOM Viewer (Medixant, Poland). TT-TG, DFT, PFCT and PTT measurements were based on previously published methods for axial MRI assessment. Specifically, the TT-TG distance was defined as the distance between the most anterior part of the tibial trochanter and the middle of the trochlear groove; the DFT was defined as the angle between the posterior cortical line above the gastrocnemius insertion of the distal femur and the posterior condylar line; the PFCT was defined as the angle between the line passing through the medial sulcus/apex of the lateral epicondyle and the line passing through the posterior condylar axis on the same slice and the PTT was defined as the angle between the line that joins the posterior border of the tibial plateaus at the level of the tibial insertion of the posterior cruciate ligament and the line that joins the posterior border of the tibia at the level of the tibial tubercle (Fig. 3) [16, 21,22,23]. The software provided measurements in mm and degrees with two decimal points. We eventually reported to one decimal point. Two sports medicine-specialised orthopaedic surgeons (DHW and HKF) measured all variables, and ultimately the mean of the two physicians' measurements was reported.
Measurements of TT-TG, DFT, PFCT and PTT. a, Slice above the gastrocnemius insertion of the distal femur. b, Slice of the gastrocnemius insertion of the distal femur. c, Slice of the proximal tibia. d, Slice of the level of the tibial tuberosity. A The TT-TG distance is the superposition of slices b and d. The TT-TG distance is defined as the distance measured on MRI between the most anterior part of the tibial trochanter and the middle of the trochlear groove. B The DFT is the superposition of slices a and b. The DFT is defined as the angle between the posterior cortical line of the distal femur and the posterior condylar line. C PFCT is defined as the angle between the line passing through the medial sulcus/apex of lateral epicondyle and the line passing through the posterior condylar axis on the slice b. D The PTT is the superposition of slices c and d. The PTT is defined as the angle between the line that joins the posterior border of the tibial plateaus at the level of the tibial insertion of the posterior cruciate ligament and the line that joins the posterior border of the tibia at the level of the tibial tubercle. TT-TG, tibial tubercle to trochlear groove. DFT, distal femoral torsion. PFCT, posterior femoral condylar torsion. PTT, proximal tibial torsion
Statistical analysis
Statistical analyses were performed with the SPSS software 23.0 (IBM, New York, USA). Measured data including age, BMI, TT-TG, DFT, PFCT and PTT of the study subjects were assessed by the Shapiro–Wilk test to conform to normal distribution and were shown as mean ± standard deviation, and the independent samples t test was used for comparisons between groups. Count data (sex and injury side) were described as rates, and the Chi-square test was used for comparisons between groups. The area under the curve (AUC) and 95% confidence intervals (CIs) for TT-TG, DFT, PFCT and PTT were plotted using receiver operating characteristic (ROC) curves, and using the Youden index, we determined the cut-off value with the greatest sensitivity and specificity. Subsequently, odds ratios (OR) were calculated to evaluate whether TT-TG, DFT, PFCT and PTT were risk factors for ACL injury. A statistically significant difference was defined as P < 0.05. With a power of 80%, α level of 0.05 and 95% confidence level, the number of subjects needed was calculated as 25 per group.
Results
Table 1 presents the patients’ demographic characteristics. There were no significant differences between all groups regarding age, sex, side of injury or BMI. TT-TG, DFT and PFCT were significantly higher in patients with ACL injury than in controls. However, PTT did not show any significant difference between ACL-injured patients and controls (n.s.). Subgroup analyses also revealed that TT-TG, DFT and PFCT were significantly increased in ACL-injured and ACL + ALL-injured patients compared with controls (P < 0.05). Patients in the ACL + ALL injury group had mildly increased TT-TG, DFT and PFCT compared with the ACL injury group, but the differences were not significant (n.s.) (Table 2). In all patients with ACL injury, women had significantly increased DFT and PTT and significantly decreased TT-TG than men. Similarly, in the study population, DFT, PFCT and PTT were significantly increased in women, while TT-TG was significantly lower compared to men (Fig. 4).
Differences in TT-TG, DFT, PFCT and PTT between study and control groups in different genders. ns., no significant difference, *p < 0.05, **p < 0.01, ***p < 0.001. TT-TG, tibial tubercle to trochlear groove. DFT, distal femoral torsion. PFCT, posterior femoral condylar torsion. PTT, proximal tibial torsion
ROC curve analysis showed that in all patients, the AUC value of TT-TG was 0.749 (95% CI 0.684–0.814), and the cut-off value of TT-TG was 11.0 mm (Youden index 0.45), which had a sensitivity of 58% and specificity of 87% for predicting an increased risk of ACL injury (OR 9.05; 95% CI 4.47–18.34). The AUC value of DFT was 0.629 (95% CI 0.554–0.704), and the cut-off value of DFT was 7.9° (Youden index of 0.30), which had a sensitivity of 49% and specificity of 81% for predicting an increased risk of ACL injury (OR 4.16; 95% CI 2.20–7.85). The AUC value of the PFCT was 0.655 (95% CI 0.581–0.729), and the cut-off value of the PFCT was 3.5° (Youden index of 0.31), which had a sensitivity of 52% and specificity of 79% for predicting an increased risk of ACL injury (OR 3.99; 95% CI 2.15–7.40). The AUC value for the PTT was 0.536 and had no predictive value (Fig. 5).
Discussion
The most important finding of this study was that knee torsional alignment, expressed as TT-TG, was higher in patients with ACL injury than in controls and that it occurred predominantly in the distal femur. No difference in PTT was observed between patients with ACL injuries and controls. It was demonstrated in our study that the primary cause of knee torsion in patients with ACL injury is increased femoral torsion, rather than PTT. However, the relationship between increased knee torsion and combined ALL injury remains unclear.
Knee torsion is a potential axial misalignment which is an anatomical factor leading to altered axial biomechanics, which exhibits differences in various populations as well as in different diseases [17, 24, 25]. For ACL injury, previous biomechanical experiments have shown that for a given quadriceps force, the greater the angle of torsion, the greater the tibial shear, subjecting the ACL to greater stress [26]. Therefore, it is necessary to explore the outliers in patients with non-contact ACL injury and to determine the contributing components of each segment, to provide a theoretical basis for better prevention of non-contact ACL injury.
TT-TG has been previously used to evaluate patellofemoral instability, and subsequent studies have revealed that the TT-TG distance is significantly greater in patients with non-contact ACL injury than in normal knees and correlates with knee torsion, which is considered a similar axial measurement parameter [15, 17, 27]. Usually, a larger TT-TG indicates greater external rotation of the tibia relative to the femur and greater stress on the ACL. The pivot-shift mechanism is the primary cause of non-contact ACL injury, with anterior tibial translation, internal rotation of the tibia and backward movement of the lateral femoral condyle. Therefore, the greater the TT-TG distance, the more internal rotation of the tibia, leading to increased shear forces over the tibia, keeping the ACL under greater tension and increasing the risk of ACL injury. Conversely, when the ACL is injured, the mechanism limiting tibial internal rotation is lost; thus, internal rotation is increased in the tibia relative to the femur, resulting in a decrease in TT-TG [28]. Simultaneously, the ALL acts as a second stabilising mechanism for the ACL, controlling anterolateral rotation with the ACL [29]. The tibia is further internally rotated relative to the femur when the ALL is injured. Our study revealed an increase in TT-TG in ACL injury patients compared to controls; nevertheless, a greater difference in TT-TG may have been observed in patients before ACL injury. Polat et al. revealed an increase in TT-TG in patients with ACL + ALL injury compared with patients with only ACL injury [28]. No differences were observed between ACL injury and combined ALL injury; however, TT-TG before ACL injury may be different.
The correlation between femoral torsion and increased hip anteversion in ACL injuries has been discussed extensively. Alpay et al. revealed that femoral anteversion leading to increased infratrochanteric femoral torsion was a risk factor for non-contact ACL injury [14]. In addition, the distal femoral morphology is associated with an increased risk of ACL injury, with an increased depth of the posterior femoral condyle causing alterations in gait and mechanics between the tibiofemoral joints, leading to ACL injury [9, 30]. Increased internal rotation of the DFT and PFCT, as we noticed, was risk factors for ACL injury. Cadaveric experiments by Bretin et al. revealed that increased internal rotation of the distal femur led to mechanical axis valgus [31]. Valgus of the knee and internal rotation of the femur lead to a pivotal shift and consequent ACL injury. Biomechanical experiments by Omar et al. suggested that internal rotation of the distal femur may lead to a more posterior resting position of the tibia, thereby increasing the magnitude of the pivot shift [32]. These cadaveric and biomechanical experiments provide a theoretical basis for increased distal femoral and posterior condylar torsions.
Previous studies have revealed that internal tibial rotation is a risk factor for ACL injury [33, 34]. When ACL injury occurs, internal rotation of the knee further increases laxity occurrence. However, our results revealed no apparent correlation between PTT and ACL injuries. Winkler et al. discovered that external tibial rotation, an infratubercular deformity occurring predominantly in the distal tibia, was not significantly correlated with PTT [21]. Thus, knee torsion in patients with ACL injury occurs predominantly on the femoral side.
A relationship between increased knee torsion and combined ALL injury was not demonstrated by our findings. TT-TG, DFT and PFCT tended to be higher in patients with ACL + ALL injury than in those with isolated ACL injury; however, the difference was not significant. Further studies on the mechanism of ALL injury are required to clarify the role of knee torsion. The ALL with the ACL theoretically controls anterolateral rotation; thus, increased knee torsion will lead to greater knee rotational stress and aggravate the degree of knee injury [29]. Based on our findings, the relationship between knee torsion and combined ALL injuries remains unclear.
In the study population, DFT, PFCT and PTT were significantly greater and TT-TG significantly decreased in women compared to men. Similar to previous studies, DFT was significantly higher in women than in men. PFCT was significantly higher in patients with lower extremity valgus than in those with neutral or varus [35]. This finding is also consistent with a higher risk of non-contact ACL injury in women and patients with lower extremity valgus [1]. The mechanisms by which differences in knee morphology contribute to an increased risk of ACL injuries are multifaceted. Our findings suggest that knee torsion associated with ACL injury occurs predominantly in the distal femur rather than the proximal tibia, which contributes to a better understanding of the causes of ACL injury. Future kinematic research should clarify the mechanisms of ACL injury by these factors to provide more precise prevention and treatment.
This study has some limitations. Firstly, not all patients underwent contralateral MRI; therefore, assessing anatomical risk factors in the contralateral healthy knee was impossible. Secondly, several torsional indicators have been measured previously mainly using computed tomography, which may differ from our results. However, MRI is more widely used in ACL injuries and has a higher reliability, making our results more valuable [36]. Finally, because our study was retrospective and may have some selection bias, the correlation between knee torsion and the risk of ACL injury and exploring the underlying mechanisms need to be further validated by prospective studies with large sample sizes in the future. The results of this study allow for the identification of people at high risk for non-contact ACL injury in MRI and help physicians target prevention and treatment strategies.
Conclusions
Knee torsional alignment is associated with ACL injury, predominantly in the distal femur rather than in the proximal tibia; however, its relationship with combined ALL injuries is unclear. This helps clinicians identify patients at risk of non-contact ACL injury and inform them of prevention strategies.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ALL:
-
Anterolateral ligament
- BMI:
-
Body mass index
- MRI:
-
Magnetic resonance imaging
- TT-TG:
-
Tibial tubercle-trochlear groove
- DFT:
-
Distal femoral torsion
- PFCT:
-
Posterior femoral condylar torsion
- PTT:
-
Proximal tibial torsion
- ROC:
-
Receiver operating characteristic
- Cis:
-
Confidence intervals
- AUC:
-
Area under the curve
- OR:
-
Odds ratios
References
Chia L, De Oliveira SD, Whalan M, McKay MJ, Sullivan J, Fuller CW, Pappas E. Non-contact anterior cruciate ligament injury epidemiology in team-ball sports: a systematic review with meta-analysis by sex, age, sport, participation level, and exposure type. Sports Med (Auckland, NZ). 2022;52(10):2447–67.
Boden BP, Sheehan FT. Mechanism of non-contact ACL injury: OREF Clinical Research Award 2021. J Orthop Res: Off Publ Orthop Res Soc. 2022;40(3):531–40.
Wojtys EM, Huston LJ, Boynton MD, Spindler KP, Lindenfeld TN. The effect of the menstrual cycle on anterior cruciate ligament injuries in women as determined by hormone levels. Am J Sports Med. 2002;30(2):182–8.
Ramesh R, Von Arx O, Azzopardi T, Schranz PJ. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br. 2005;87(6):800–3.
Huang YL, Jung J, Mulligan CMS, Oh J, Norcross MF. A majority of anterior cruciate ligament injuries can be prevented by injury prevention programs: a systematic review of randomized controlled trials and cluster-randomized controlled trials with meta-analysis. Am J Sports Med. 2020;48(6):1505–15.
Dauty M, Crenn V, Louguet B, Grondin J, Menu P, Fouasson-Chailloux A. Anatomical and neuromuscular factors associated to non-contact anterior cruciate ligament injury. J Clin Med. 2022;11(5).
Bingzheng Z, Xinzhuo Z, Zhuo J, Xing Y, Bin L, Lunhao B. The effects of sex hormones during the menstrual cycle on knee kinematics. Front Bioeng Biotechnol. 2023;11:1209652.
Li K, Li J, Zheng X, Marot V, Murgier J, Cavaignac E, Huang W. Increased lateral meniscal slope is associated with greater incidence of lateral bone contusions in noncontact ACL injury. Knee Surg Sports Traumatol Arthroscopy: Off J ESSKA. 2020;28(6):2000–8.
Li K, Zheng X, Li J, Seeley RA, Marot V, Murgier J, Liang X, Huang W, Cavaignac E. Increased lateral femoral condyle ratio is associated with greater risk of ALC injury in non-contact anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2020;29(9):3077–84.
Jha V, Azam MQ, Jain P, Bali SA. Does femoral intercondylar notch volume differ in anterior cruciate ligament-injured adult patients compared to the uninjured? A meta-analysis. Clin Orthop Surg. 2022;14(1):76–89.
Hong CK, Lin YJ, Cheng TA, Chang CH, Hsu KL, Kuan FC, Su WR. Adult patients with ACL tears have greater tibial internal rotation in MRI compared to adolescent patients. J Orthop Surg Res. 2022;17(1):17.
Shin CS, Chaudhari AM, Andriacchi TP. Valgus plus internal rotation moments increase anterior cruciate ligament strain more than either alone. Med Sci Sports Exerc. 2011;43(8):1484–91.
Dai B, Garrett WE, Gross MT, Padua DA, Queen RM, Yu B. The effect of performance demands on lower extremity biomechanics during landing and cutting tasks. J Sport Health Sci. 2019;8(3):228–34.
Alpay Y, Ezici A, Kurk MB, Ozyalvac ON, Akpinar E, Bayhan AI. Increased femoral anteversion related to infratrochanteric femoral torsion is associated with ACL rupture. Knee Surg Sports Traumatol Arthroscopy: Off J ESSKA. 2020;28(8):2567–71.
Barahona M, Guzmán M, Barrientos C, Zamorano Á, Palet M, Hinzpeter J. The distance between Tibial tubercle and trochlear groove correlates with knee articular torsion. J Knee Surg. 2021;34(9):918–23.
Shen X, Xiao J, Yang Y, Liu T, Chen S, Gao Z, Zuo J. Multivariable analysis of anatomic risk factors for anterior cruciate ligament injury in active individuals. Arch Orthop Trauma Surg. 2019;139(9):1277–85.
Paul RW, Johnson EE, Hall A, Clements A, Bishop ME, Ciccotti MG, Cohen SB, Erickson BJ. Comparison of post-operative outcomes following anterior cruciate ligament reconstruction between patients with vs. without elevated tibial tubercle-trochlear groove (TT-TG) distance. Knee Surg Sports Traumatol Arthroscopy: Off J ESSKA. 2023;31(6):2446–53.
Helito CP, Helito PVP, Leao RV, Demange MK, Bordalo-Rodrigues M. Anterolateral ligament abnormalities are associated with peripheral ligament and osseous injuries in acute ruptures of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthroscopy: Off J ESSKA. 2017;25(4):1140–8.
Helito PVP, Helito CP, Rodrigues MB. Anterolateral ligament MRI of the knee in ACL injuries: MRI abnormalities association with instability. Eur Radiol. 2023;33(2):1456–64.
Balendra G, Willinger L, Pai V, Mitchell A, Lee J, Jones M, Williams A. Anterolateral complex injuries occur in the majority of “isolated” anterior cruciate ligament ruptures. Knee Surg Sports Traumatol Arthroscopy: Off J ESSKA. 2022;30(1):176–83.
Winkler PW, Lutz PM, Rupp MC, Imhoff FB, Izadpanah K, Imhoff AB, Feucht MJ. Increased external tibial torsion is an infratuberositary deformity and is not correlated with a lateralized position of the tibial tuberosity. Knee Surg Sports Traumatol Arthroscopy: Off J ESSKA. 2021;29(5):1678–85.
Seitlinger G, Moroder P, Scheurecker G, Hofmann S, Grelsamer RP. The contribution of different femur segments to overall femoral torsion. Am J Sports Med. 2016;44(7):1796–800.
Fan C, Niu Y, Wei M, Kong L, Wang F. Study on the correlation between the severity of patellofemoral arthritis and the morphology of the distal femur. BMC Musculoskelet Disord. 2023;24(1):90.
Kaiser P, Loth F, Attal R, Kummann M, Schuster P, Riechelmann F, Schlumberger M. Static patella tilt and axial engagement in knee extension are mainly influenced by knee torsion, the tibial tubercle-trochlear groove distance (TTTG), and trochlear dysplasia but not by femoral or tibial torsion. Knee Surg Sports Traumatol Arthroscopy: Off J ESSKA. 2020;28(3):952–9.
Mathon P, Micicoi G, Seil R, Kacaoglu B, Cerciello S, Ahmad F, LiArno S, Teitge R, Ollivier M. Healthy middle-aged Asian and Caucasian populations present with large intra- and inter-individual variations of lower limb torsion. Knee Surg Sports Traumatol Arthroscopy: Off J ESSKA. 2021;29(4):1083–9.
Nunley RM, Wright D, Renner JB, Yu B, Garrett WE. Gender comparison of patellar tendon tibial shaft angle with weight bearing. Res Sports Med. 2003;11(3):173–85.
Saper MG, Popovich JM Jr, Fajardo R, Hess S, Pascotto JL, Shingles M. The relationship between tibial tubercle-trochlear groove distance and noncontact anterior cruciate ligament injuries in adolescents and young adults. Arthroscopy: J Arthroscopic Relat Surg: Off Publ Arthroscopy Assoc N Am Int Arthroscopy Assoc. 2016;32(1):63–8.
Polat AE, Polat B, Gürpınar T, Sarı E, Çarkçı E, Erler K. Tibial tubercle-trochlear groove (TT-TG) distance is a reliable measurement of increased rotational laxity in the knee with an anterior cruciate ligament injury. Knee. 2020;27(5):1601–7.
Kang KT, Koh YG, Park KM, Choi CH, Jung M, Cho H, Kim SH. Effects of the anterolateral ligament and anterior cruciate ligament on knee joint mechanics: a biomechanical study using computational modeling. Orthop J Sports Med. 2022;10(4):23259671221084970.
He M, Li J. Increased lateral femoral condyle ratio measured by MRI is associated with higher risk of noncontact anterior cruciate ligament injury. BMC Musculoskelet Disord. 2022;23(1):190.
Bretin P, O’Loughlin PF, Suero EM, Kendoff D, Ostermeier S, Hüfner T, Krettek C, Citak M. Influence of femoral malrotation on knee joint alignment and intra-articular contract pressures. Arch Orthop Trauma Surg. 2011;131(8):1115–20.
Omar M, Al Saiegh Y, Liodakis E, Stuebig T, Guenther D, Steimer D, Hawi N, Krettek C, Suero EM. Effect of femoral antetorsion on tibiofemoral translation and rotation in the anterior cruciate ligament deficient knee. J Knee Surg. 2019;32(10):960–5.
Mitchell BC, Siow MY, Bastrom T, Bomar JD, Pennock AT, Parvaresh K, Edmonds EW. coronal lateral collateral ligament sign: a novel magnetic resonance imaging sign for identifying anterior cruciate ligament-deficient knees in adolescents and summarizing the extent of anterior tibial translation and femorotibial internal rotation. Am J Sports Med. 2021;49(4):928–34.
Hodel S, Torrez C, Flury A, Fritz B, Steinwachs MR, Vlachopoulos L, Fucentese SF. Tibial internal rotation in combined anterior cruciate ligament and high-grade anterolateral ligament injury and its influence on ACL length. BMC Musculoskelet Disord. 2022;23(1):262.
van der Wal WA, Meijer DT, Hoogeslag RAG, LaPrade RF. Meniscal Tears, Posterolateral and Posteromedial Corner Injuries, Increased Coronal Plane, and Increased Sagittal Plane Tibial Slope All Influence Anterior Cruciate Ligament-Related Knee Kinematics and Increase Forces on the Native and Reconstructed Anterior Cruciate Ligament: A Systematic Review of Cadaveric Studies. Arthroscopy: J Arthroscopic Relat Surg: Off Publ Arthroscopy Assoc N Am Int Arthroscopy Assoc. 2022;38(5):1664-1688.e1661.
Parikh S, Noyes FR. Patellofemoral disorders: role of computed tomography and magnetic resonance imaging in defining abnormal rotational lower limb alignment. Sports health. 2011;3(2):158–69.
Acknowledgements
None
Funding
This study was supported by National Natural Science Foundation of China (NO.81902293); Chongqing Science and Health Joint Medical Research Program (2022DBXM002); Key Project of Technical Innovation and Application Development in Chongqing (CSTB202ITIAD-KPX0069).
Author information
Authors and Affiliations
Contributions
DHW, HKF, LLH, XL, WH and KL contributed to the study conception and design. DHW and HKF performed material preparation, data collection and analysis. The first draft of the manuscript was written by DHW, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The First Affiliated Hospital of Chongqing Medical University (IRB approval number:2019–345) approved this study. The requirement for informed consent was waived because this was a retrospective imaging study.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, D., Fan, H., Hu, L. et al. Increased knee torsional misalignment associated with femoral torsion is related to non-contact anterior cruciate ligament injury: a case–control study. J Orthop Surg Res 19, 124 (2024). https://doi.org/10.1186/s13018-024-04609-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04609-y