Abstract
Purposes
This study aimed to investigate whether the morphology of the superior articular processes of L5 vertebra affected the accuracy of pedicle screw placement by reviewing 299 patients who had undergone L5 pedicle screw fixation over the past 12 months and measuring relevant parameters.
Methods
We retrospectively analyzed patients who underwent L5 vertebra fixation at our spine surgery department from October 20, 2020 to October 20, 2021. Patients with spondylolisthesis, spondylolysis, and scoliosis were excluded. Parameters associated with the superior articular process were analyzed, including Mammillary process-Spinal canal Distance (MCD), Inter-Facet Distance (IFD), Inter-Pedicle Distance (IPD), Zygapophysial Joints Angle (ZJA), Superior Articular Width, and Lateral Recess Transverse Diameter. The L5 vertebral body was reconstructed by Mimics 21.0, and the simulated L5 screws were inserted at multiple entry points to measure the Maximum Safe Transverse Angle (STAmax).
Results
A total of 299 patients who underwent L5 vertebra fixation with 556 pedicle screws were analyzed. An MCD < 6 mm was associated with a significant increase in screw placement failure rate and decrease in ZJA. The MCD was positively correlated with IFD. No significant change in IPD was observed. Mimics software analysis showed that the STAmax decreased with a decrease of MCD. When WBV < 6 mm, 93% of the trans-mammillary vertical line was located within 50% of the pedicle.
Conclusions
The superior articular process tended to narrow the spinal canal and exhibit a steep and a “cloverleaf” morphology when the MCD was < 6 mm. This morphology increased the risk of operator mis-judgement resulting in screw placement failure. Assessment of the relationship between the trans-mammillary vertical line and the pedicle represents a simple method to predict abnormal morphology of the superior articular process before surgery.
Similar content being viewed by others
Introduction
Pedicle screw fixation is essential for maintaining spinal stability in spinal surgery. Breach or perforation of the pedicle cortex is a widely acknowledged complication of screw placement, with an incidence rate between 6.5 and 13% [1,2,3,4]. Perforation of the medial and inferior wall of the pedicle cortex is more likely to lead to nerve stimulation, leading to postoperative nerve pain [5]. Most patients with postoperative pain due to screw placement failure need reoperation. Even if pedicle perforation does not result in neurological symptoms, pedicle wall damage reduces the biomechanical strength of pedicle screw fixation and accelerates the progression of degeneration of adjacent segments of the lumbar discs [6,7,8].
Common entry reference markers for pedicle screw placement include the mammillary process, accessory process, and lateral margin of zygapophysial joints. The commonly used methods of pin entry points include the Roy-Camille [9], Magerl [10], Weinstein [11], and “^”-shaped crest techniques. The “^”-shaped crest put forward by Professor Xin-ru Du is a crest structure where the pars interarticularis converges at the accessory process, which appears almost constantly in L1–L4, but only in 81% of L5 vertebra.
It is well-established that the accuracy of screw placement in L5 is not very ideal. Indeed, L5 is the segment with the highest lumbar screw placement failure rate with free-hand screw placement or X-ray navigation only [12]. The pedicle morphology of the L5 vertebral body varies significantly at different stages of physical development [13]. Moreover, L5 vertebral body exhibit the largest standard deviation of both vertebral width and pedicle parameters [14]. It is widely believed that the rate of screw placement failure is significantly increased if the spinal canal at L5 exhibits a “clover” shape. The “clover leaf” spinal canal remains poorly understood, warranting further studies.
In this study, the risk factors of screw placement failure were analyzed by reviewing patients who underwent L5 pedicle screw fixation in our center over the past 12 months, measuring the L5 vertebral body parameters, and analyzing the corresponding screw placement accuracy rates.
Materials and methods
We retrospectively analyzed patients in our spine surgery department who underwent L5 vertebrae fixation from 2020.10 to 2021.10. Patients who underwent lumbar multi-slice spiral computed tomography (CT) before and after surgery for lumbar disc herniation and lumbar spinal stenosis were included. To reduce the confounding effect of abnormal vertebral structure or rotation on screw placement, our exclusion criteria included 1. Lumbar spondylolisthesis; 2. Spondylolysis of L5 vertebral body; 3. Scoliosis (upper endplate L4–upper endplate S1 cobb Angle > 10°; or L5 upper endplate with horizontal angle > 5°); 4. L5 vertebral rotation (Nash-Moe Grade greater than or equal to grade 2 [15]); 5. Lumbosacral transitional vertebra. 6. Severe facet joint arthritis (Fujiwara Grade greater than or equal to grade 3 [16]).
A dual-source spiral 64-slice CT scanner (General Electric Company, USA) was used with the patients in the supine position.
During the analysis, we found that an increased screw placement failure rate paralleled a decrease in MCD. Therefore, we divided the patients into four groups, according to the mean and standard deviation of the MCD, A (MCD < 6 mm), B (6 mm < MCD < 8 mm), C (8 mm < MAC < 10 mm), and D (MCD > 10 mm) groups for measurement and analysis.
The Amiot grading system was used to evaluate the accuracy of pedicle screw placement, including levels 0–4: ideal position, 0–2 mm, 2–4 mm, 4–6 mm, and > 6 mm [17].
Three reference lines parallel to the upper endplate were drawn from the axial CT scans across the midline of the upper disc, across the superior margin of the pedicle, and across the inner edge of the pedicle. Measurement of the ZJA in plane b was performed in accordance with a previously published study by Boden et al. [18]. The SAW and IFD were measured in plane c, and the MCD and IPD were measured in plane d. Meanwhile, the LRTD was measured by the horizontal distance from the medial edge of the superior articular process to the medial edge of the corresponding pedicle (Fig. 1).
A Three axial sections parallel to the upper endplate: b. Through the midline of the disc; c. through the upper edge of the pedicle; d. through the medial margin of the pedicle. B ZJA was measured by the angle between the spinous process axis and the medial edge of the bilateral superior articular process. C IFD was measured by the distance between the inner edge of the bilateral superior articular process; SAW was measured by the length between the inner and outer edges of the superior articular process. D. MCD was measured by the vertical distance between the mammillary process and the inner edge of lateral pedicle; IPD was measured by the distance between the inner edges of bilateral pedicles; LRTD was measured by the distance between the superior articular process and the inner edge of the pedicle
The CT images were converted into 3D images of L5 vertebral bodies by Materialize interactive medical image control system version 21.0 (Mimics, Leuven, Flanders, Belgium). A 6.5-mm-diameter cylinder was used to simulate pedicle screws. The Magerl, Roy-Camille, and “^”-shaped crest techniques were used for the entry points, and the simulated screws were tangent to the medial pedicle wall. The STAmax was the angle between the pedicle screw and the line through the spinous process perpendicular to the posterior edge of the vertebral body (Fig. 2).
All statistical analyses were performed using SPSS 21.0 statistical software (SPSS, Chicago, IL, USA). An independent t-test was used to determine differences in pedicle parameters after stratifying by gender (male or female) and laterality (left or right). Analysis of variance (ANOVA) was used to examine the significance of differences in all pedicle parameters and demographics (age, height, weight, and BMI) between the A-D groups. The minimum significant difference was used for all comparisons between groups. Pearson correlation was used to examine the relationship between pedicle parameters and MCD. The chi-square test was used to compare categorical variables. A P-value < 0.05 was statistically significant.
Results
A total of 299 patients (141 men and 158 women) with a mean age of 57.9 ± 12.87 years (32–83 years) underwent L5 vertebra fixation with 556 pedicle screws from October 20, 2020, to October 20, 2021 (Table 1). The pedicle screws were classified as grade 0 (n = 469, 84.4%), grade 1 (n = 38, 6.8%), grade 2 (n = 32, 5.7%), grade 3 (n = 5, 0.9%), and grade 4 (n = 12, 2.2%). The failure rates of screw placement in groups A to D were 65.7%, 9.0%, 11.2% and 2.2%, respectively (Table 2).
Parameters in group A (with minimum MCD) and group D (with maximum MCD) were significantly different from other groups. The smallest ZJA and IFD were observed in group A (17.8 ± 1.4 mm and 33° ± 5.9°, respectively). The largest bilateral LRTD (6.6 ± 1.6 and 6.3 ± 1.4) and smallest SAW (14.8 ± 1.5 mm and 14.4 ± 1.3 mm) were also found in group A. The l-SAW was significant difference between group A and other groups, with not a significant difference on r-SAW (Table 3).
There was no significant correlation between MCD and IPD, while a positive correlation was found between MCD and IFD. Pearson’s correlation analysis showed that IFD positively correlated with MCD (r = 0.6976, P = 0.0001) (Fig. 3).
A smaller MCD was predominantly found in women. The proportion of female patients in group A was 72.2%. Further measurements showed that not only SAW was smaller than men in group A, but IFD was also smaller than men (Table 4).
As MCD decreases, STAmax decreases. The STAmax of group A was only 3.68° by the Magerl technique. The STAmax was about 15–16° for groups B and C and 25°for group D (Table 5).
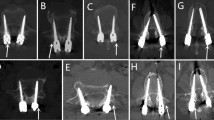
Interestingly, during the measurement process, we found a simple preoperative evaluation method. In preoperative horizontal or vertical CT cross sections, when a vertical line passing through the mammillary process was medial to the midpoint of the pedicle, it indicated that the superior articular process was too close to each other. This phenomenon was found in 93% of cases in Group A and 5% in the other groups (Fig. 4).
Discussions
Navigation technology has developed rapidly in recent years. Current evidence suggests that the accuracy of robotic screws placement or intraoperative CT navigation is higher than free-hand or intraoperative X-ray navigation [19]. However, this navigation equipment is expensive, and most spinal surgeons still place pedicle screws free-hand or with intraoperative X-ray. The accuracy of free-hand screw placement is not ideal, especially for L5. An increasing body of evidence suggests that during placement of L5 segment, it should be directed outwards and upwards [5, 20]. Measurement and analysis of CT images suggest that the entry points for L5 have a tendency to be inward, requiring either the “^”-shaped crest or Magerl technique.
At present, the commonly used screw placement entry points use the superior articular process and transverse process as the reference. However, the transverse process of the lower lumbar spine is deep and sometimes blocked by the iliac crest and pulled by the erector spine muscle; accordingly, it is difficult to fully expose the root of the transverse process during surgery. Therefore, the morphology of the superior articular process and its position relative to the spinal canal directly affect the accuracy of pedicle screw placement. When the superior articular process faces inward, the insertion point is also inward relative to the spinal canal. In this case, screw placement at an angle of 10–15° can cause the screw to penetrate the inner wall of the pedicle (Fig. 5). Importantly, we found that when the MCD was less than 6 mm, the screw placement failure rate increased significantly. Evaluation of the preoperative CT showed that the STAmax of screw placement was only 1–7°. For these patients, the angle of insertion should be abducted if the screws are placed at commonly used entry points.
In fact, such cases are not uncommon. More than 10% of the 299 patients (n = 36) presented with a low MCD, which may be attributed to selection bias caused by the smaller ZJA [21].
All 299 patients included in this study were patients with lumbar disc herniation or lumbar spinal stenosis. Although patients with severe facet arthritis were excluded at the time of inclusion, changes in facet joint morphology could affect the final measurements [22, 23]. The ZJA at L5 is generally about 45° and does not exhibit significant heterogeneity across different populations. The reported average ZJA in Indian [24], Chinese [25], and French [26] populations is 48.32°, 47.7°, and 44.4°, respectively. In the present study, the average ZJA of L5 (n = 598) was 46.3°, consistent with the literature. However, the ZJA in group A decreased significantly to 33.7°. Morphologically, this type of facet joint is more similar to the superior facet of L4. When the L5 superior facet became more sagittal than horizontal, it increased susceptibility to degenerative lumbar diseases, including lumbar disc herniation and degenerative lumbar spondylolisthesis [22, 27]. Excessively small vertebral bodies and steep facet joints were associated with lumbar instability, while excessively steep facet joints could accelerate the rate of disc degeneration [28].
Moreover, we found that the small distance between superior articular processes of L5 was associated with a small MCD. A study by Santiago et al. where the sagittal diameters of lumbar vertebrae and articular processes of 39 healthy Spaniards were measured showed the distance between L5 superior articular processes was 22.2 mm ± 0.40 mm [29]. Consistently, Oguz et al. measured the lumbar vertebrae of 24 healthy Turks, and the distance between L5 superior articular processes was 21.7 mm ± 2.8 mm [30]. In this study, the inter-facet distance in group A was only 17.8 mm ± 1.4 mm, indicating that the superior articular processes of group A are closer to each other than in other groups. In addition, the SAW was also smaller in group A compared with BCD, although this reduction was not statistically significant on one side. Compared with the normal superior articular process, the superior joint of group A exhibited a steeper and sharper variation. The steep superior articular process tended to narrow the spinal canal compared to the gentle superior articular process. The L5 spinal canal of this type of superior articular process typically exhibits a “clover” shape, with the superior articular process extending inward (Fig. 6).
IPD is also a factor that affects the relative position of the entry point. However, the IPD in group A was only 28.3 ± 2.2 mm and did not increase significantly. Meanwhile, the overall mean IPD was 28.4 mm ± 2.3 mm, which was not significantly different from the reported average transverse diameter in Chinese (29.61 mm ± 0.63 mm) and Indian (28.02 mm ± 0.37 mm) populations in the literature [31].
Mitra, Datir, and Hou et al. observed a sequential outward migration of the central entry point of the lumbar pedicle from L1–L4 [14, 32]. At L5, the entry point is located lateral to the lateral boundary of the facet joint. However, if the angle of the superior facet of L5 is small with no “abduction,” the usual Magerl entry point is inward-facing. In some medical centers, to avoid this kind of situation, the root of the transverse process is adopted for screw insertion, which is more lateral than Margel entry point, with an accuracy rate of > 98% [33]. However, a more external entry point means more muscle dissection, bleeding, and longer surgical time. Although screw placement failure was avoided in a small number of patients, the cost-effectiveness of this approach needs further study. Based on the current Magerl or “^”-shaped crest insertion methods, preoperative estimation of excessive orientation of the L5 superior articular process is a cost-effective method. When the MCD is less than 6 mm, the internal angle of screw placement should be reduced, and vertical entry into the vertebral body may be required.
Conclusions
We report a distinct superior articular process of the L5 vertebral body characterized by MCD < 6 mm, decreased IFD, SAW, and ZJA. In this type of vertebral body, the superior articular process is closer to the spinal canal when used as the reference for the traditional insertion point, increasing the risk of spinal canal invasion during pedicle screw placement. Preoperative evaluation of the superior articular process on CT images is vital to avoid screw perforation into the spinal canal.
References
Castro WHM, Halm H, Jerosch J, et al. Accuracy of pedicle screw placement in lumbar vertebrae. Spine (Phila Pa 1976). 1996;21:1320–4. https://doi.org/10.1097/00007632-199606010-00008.
Wood MJ, McMillen J. The surgical learning curve and accuracy of minimally invasive lumbar pedicle screw placement using CT based computer-assisted navigation plus continuous electromyography monitoring: a retrospective review of 627 screws in 150 patients. Int J Spine Surg. 2014. https://doi.org/10.14444/1027.
Kuo KL, Su YF, Wu CH, et al. Assessing the intraoperative accuracy of pedicle screw placement by using a bone-mounted miniature robot system through secondary registration. Plos One. 2016;11:e0153235. https://doi.org/10.1371/journal.pone.0153235.
Etemadifar M, Jamalaldini M. Evaluating accuracy of free-hand pedicle screw insertion in adolescent idiopathic scoliosis using postoperative multi-slice computed tomography scan. Adv Biomed Res. 2017;6:19. https://doi.org/10.4103/2277-9175.201331.
Attar A, Ugur HC, Uz A, et al. Lumbar pedicle: surgical anatomic evaluation and relationships. Eur Spine J. 2001;10:10–5. https://doi.org/10.1007/s005860000198.
Pihlajämaki H, Myllynen P, Böstman O. Complications of transpedicular lumbosacral fixation for non-traumatic disorders. J Bone Jt Surg. 1997;79:183–9. https://doi.org/10.1302/0301-620x.79b2.7224.
Jutte PC, Castelein RM. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J. 2002;11:594–8. https://doi.org/10.1007/s00586-002-0469-8.
Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine (Phila Pa 1976). 1993;18:2231–8. https://doi.org/10.1097/00007632-199311000-00015 (discussion 2238-9).
Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;203:7.
Magerl FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res. 1984;189:125–41.
Weinstein JN, Spratt KF, Spengler D, et al. Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976). 1988;13:1012–8. https://doi.org/10.1097/00007632-198809000-00008.
Waschke A, Walter J, Duenisch P, et al. CT-navigation versus fluoroscopy-guided placement of pedicle screws at the thoracolumbar spine: single center experience of 4500 screws. Eur Spine J. 2013;22:654–60. https://doi.org/10.1007/s00586-012-2509-3.
Senaran H, Yazici M, Karcaaltincaba M, et al. Lumbar pedicle morphology in the immature spine: a three-dimensional study using spiral computed tomography. Spine (Phila Pa 1976). 2002;27:2472–6. https://doi.org/10.1097/00007632-200211150-00010.
Hou S, Hu R, Shi Y. Pedicle morphology of the lower thoracic and lumbar spine in a Chinese population. Spine (Phila Pa 1976). 1993;18:1850–5. https://doi.org/10.1097/00007632-199310000-00021.
Drerup B. Principles of measurement of vertebral rotation from frontal projections of the pedicles. J Biomech. 1984;17:923–35. https://doi.org/10.1016/0021-9290(84)90005-8.
Fujiwara A, Tamai K, Yamato M, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J. 1999;8:396–401. https://doi.org/10.1007/s005860050193.
Amiot LP, Lang K, Putzier M, et al. Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine (Phila Pa 1976). 2000;25:606–14. https://doi.org/10.1097/00007632-200003010-00012.
Boden SD, Riew KD, Yamaguchi K, et al. Orientation of the lumbar facet joints: association with degenerative disc disease. J Bone Jt Surg. 1996;78:403–11. https://doi.org/10.2106/00004623-199603000-00012.
Aoude AA, Fortin M, Figueiredo R, et al. Methods to determine pedicle screw placement accuracy in spine surgery: a systematic review. Eur Spine J. 2015;24:990–1004. https://doi.org/10.1007/s00586-015-3853-x.
Ebraheim NA, Xu R, Darwich M, Yeasting RA. Anatomic relations between the lumbar pedicle and the adjacent neural structures. Spine (Phila Pa 1976). 1997;22:2338–41. https://doi.org/10.1097/00007632-199710150-00003.
Weinberg DS, Xie KK, Liu RW, et al. Increased pelvic incidence is associated with a more coronal facet orientation in the lower lumbar spine: a cadaveric study of 599 lumbar spines. Spine (Phila Pa 1976). 2016;41:E1138–45. https://doi.org/10.1097/BRS.0000000000001577.
Liu Z, Duan Y, Rong X, et al. Variation of facet joint orientation and tropism in lumbar degenerative spondylolisthesis and disc herniation at L4–L5: A systematic review and meta-analysis. Clin Neurol Neurosurg. 2017;161:41–7. https://doi.org/10.1016/j.clineuro.2017.08.005.
Choi HJ, Park JY, Chin DK, et al. Anatomical parameters of fifth lumbar vertebra in L5–S1 spondylolytic spondylolisthesis from a surgical point of view. Eur Spine J. 2014;23:1896–902. https://doi.org/10.1007/s00586-013-3111-z.
Mohanty SP, Pai Kanhangad M, Kamath S, Kamath A. Morphometric study of the orientation of lumbar zygapophyseal joints in a South Indian population. Orthop Surg (Hong Kong). 2017;25:2309499017739483. https://doi.org/10.1177/2309499017739483.
Dai LY. Orientation and tropism of lumbar facet joints in degenerative spondylolisthesis. Int Orthop. 2001;25:40–2. https://doi.org/10.1007/s002640000201.
Schuller S, Charles YP, Steib JP. Sagittal spinopelvic alignment and body mass index in patients with degenerative spondylolisthesis. Eur Spine J. 2011;20:713–9. https://doi.org/10.1007/s00586-010-1640-2.
Naeem K, Nathani KR, Barakzai MD, et al. Modifications in lumbar facet joint are associated with spondylolisthesis in the degenerative spine diseases: a comparative analysis. Acta Neurochir. 2021;163:863–71. https://doi.org/10.1007/s00701-020-04657-3.
Jiang X, Chen D, Li Z, Lou Y. Correlation between lumbar spine facet joint orientation and intervertebral disk degeneration: a positional MRI analysis. Neurol Surg Cent Eur Neurosurg. 2019;80:255–61. https://doi.org/10.1055/s-0039-1683450.
Santiago FR, Milena GL, Herrera RO, et al. Morphometry of the lower lumbar vertebrae in patients with and without low back pain. Eur Spine J. 2001;10:228–33. https://doi.org/10.1007/s005860100267.
Oğuz H, Akkuş S, Tarhan S, et al. Measurement of spinal canal diameters in young subjects with lumbosacral transitional vertebra. Eur Spine J. 2002;11:115–8. https://doi.org/10.1007/s005860100323.
Wang TM, Shih C. Morphometric variations of the lumbar vertebrae between Chinese and Indian adults. Acta Anat (Basel). 1992;144:23–9. https://doi.org/10.1159/000147280.
Mitra SR, Datir SP, Jadhav SO. Morphometric study of the lumbar pedicle in the indian population as related to pedicular screw fixation. Spine (Phila Pa 1976). 2002;27:453–9. https://doi.org/10.1097/00007632-200203010-00004.
Parker SL, McGirt MJ, Farber SH, et al. Accuracy of free-hand pedicle screws in the thoracic and lumbar spine: analysis of 6816 consecutive screws. Neurosurgery. 2011;68:170–8. https://doi.org/10.1227/NEU.0b013e3181fdfaf4 (discussion 178).
Acknowledgements
The authors would like to thank all the patients of the Foshan Fosun Changcheng Hospital for allowing to publish the paper and to use their images taken during hospital admission.
Funding
The manuscript submitted does not contain information about medical device(s)/drug(s). No funds were received in support of this work.
Author information
Authors and Affiliations
Contributions
XL and PL wrote the main manuscript text; HL and BC prepared figure and GC revised the article. All authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Reviewing the CT images of 299 patients will not violate the rights of the patients. After the discussion by the institutional review board, consent forms were not required. The study was approved by institutional review board of Foshan Fosun Chancheng Hospital (No. KY2022005).
Competing interests
The author’s declared that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, XG., Liang, PJ., Liu, HH. et al. A superior articular process morphology of 5th lumbar vertebra prone to screws placement failure: an anatomical study of 299 patients. J Orthop Surg Res 17, 505 (2022). https://doi.org/10.1186/s13018-022-03403-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-03403-y