Abstract
Background
The superiorities in proximal facet joint protection of robot-assisted (RA) pedicle screw placement and screw implantation via the cortical bone trajectory (CBT) have rarely been compared. Moreover, findings on the screw accuracy of both techniques are inconsistent. Therefore, we analyzed the screw accuracy and incidence of facet joint violation (FJV) of RA and CBT screw insertion in the same study and compared them with those of conventional pedicle screw (PS) insertion. The possible factors affecting screw accuracy and FJV were also analyzed.
Methods
A total of 166 patients with lumbar degenerative diseases requiring posterior L4-5 fusion were retrospectively included and divided into the RA, PS, and CBT groups from March 2019 to December 2021. The grades of intrapedicular accuracy and superior FJV were evaluated according to the Gertzbin–Robbins scale and the Babu scale based on postoperative CT. Univariable and multivariable analyses were conducted to assess the possible risk factors associated with intrapedicular accuracy and superior FJV.
Results
The rates of optimal screw insertion in the RA, PS, and CBT groups were 87.3%, 81.3%, and 76.5%, respectively. The difference between the RA and CBT groups was statistically significant (P = 0.004). Superior FJVs occurred in 28.2% of screws in RA, 45.0% in PS, and 21.6% in CBT. The RA and CBT groups had fewer superior FJVs than the PS group (P = 0.008 and P < 0.001, respectively), and no significant difference was observed between the RA and CBT groups (P = 0.267). Multivariable analysis revealed that the CBT technique was an independent risk factor for intrapedicular accuracy. Furthermore, older age, the conventional PS technique and a smaller facet angle were independently associated with the incidence of superior FJVs.
Conclusions
The RA and CBT techniques were associated with fewer proximal FJVs than the PS technique. The RA technique showed a higher rate of intrapedicular accuracy than the CBT technique. The CBT technique was independently associated with screw inaccuracy. Older age, conventional PS technique and coronal orientation of the facet join were independent risk factors for superior FJV.
Similar content being viewed by others
Background
Pedicle screw fixation facilitates stable three-column fixation and has become a standard technique for the treatment of various lumbar diseases [1, 2]. Although many studies have reported that the early results of spinal fusion were promising, the long-term clinical efficacy can be compromised because of adjacent segment disease (ASD). ASD has become the major cause of revision surgical procedures after lumbar fusion [3]. Recent studies have shown that cranial facet joint violation (FJV) is an important risk factor for ASD [4,5,6,7,8]. Injury to the superior facet joints during the placement of pedicle screws was associated with alterations in stability and the load-bearing capability of the adjacent segment [9,10,11], thus accelerating the degeneration of the joint and ultimately leading to ASD. The rates of FJV in different implantation techniques varies. Percutaneous pedicle screw placement was associated with significantly more cranial facet violations than traditional open surgery [12]. Two emerging techniques, robot-assisted (RA) screw placement and screw implantation via the cortical bone trajectory (CBT), have been gradually applied in clinical practice in recent years [13,14,15,16]. These two implantation techniques have shown remarkable superiority in proximal facet joint protection [17,18,19,20]. However, these two techniques have rarely been compared. Considering the special anatomical proximity of the pedicle, screw malposition can cause serious complications. Hence, screw accuracy is consistently regarded as one of the criteria for the measurement of the quality of each screw implantation technique. Both the RA and CBT screw implantation techniques are emerging minimally invasive techniques that can reduce paravertebral muscle dissection, but findings on the screw accuracy of both techniques are inconsistent [13, 21,22,23,24,25,26,27].
Therefore, we analyzed the screw accuracy and incidence of FJVs of RA and CBT screw insertion in the same study and compared them with those of conventional pedicle screw insertion.
Methods
Study design and patients
The study was approved by the hospital institutional review board. A consecutive series of lumbar fusions performed between March 2019 and December 2021 were retrospectively reviewed. Patients were selected using the following inclusion criteria: age between 20 and 80 years old; inclusion for single-level fusion of L4-5 due to lumbar degenerative disease associated with segmental instability, including huge disc herniation, lumbar spinal stenosis, and spondylolisthesis (grade I/II); ineffective results with conservative treatment for at least 6 months before surgery; and postoperative CT examination. The exclusion criteria were as follows: decompression without fusion; previous surgery on the lumbar spine; congenital malformations of the lumbar spine; and incomplete imaging data. All patients underwent surgery by the same team of experienced surgeons. The choice of insertion approach was based on a discussion between the surgeon and the patient and was related to inadequate reimbursement for use of RA in many cases.
Surgical techniques
RA pedicle screw placement
In the RA group, according to the intraoperative 3D fluoroscopic images of the surgical area, the surgeon planned screw trajectories on the robotic workstation (TINAVI, China). After the robotic arm moving to the planned path, the placement of 4 guide pins were completed through the guidance of robotic arm. The guide pins were fixed properly, then an interbody polyetheretherketone (PEEK) cage was placed under the tubular retractors. After decompression, adequate-sized cannulated screws were subsequently inserted.
Traditional PS placement
In the PS group, a midline incision was made, followed by exposure of the spine to the spinous processes, laminae, and facet joint to allow clear identification of the bony landmarks. The entry point and trajectory were confirmed fluoroscopically. Adequate-sized pedicle screws were subsequently inserted. After decompression, an interbody PEEK cage was placed, and the rods and screw caps were inserted.
CBT screw placement
Through a midline incision, subperiosteal dissection was performed down to the spinous processes, laminae, and facet joint. The entry point of the cortical screw was located at the center of the superior articular process and 1 mm inferior to the inferior border of the transverse process. The trajectory direction was 10° laterally in the axial plane and 25°–30° cranially in the sagittal plane. The entry point and trajectory were determined according to the C-arm perspective. The initial hole was made using a 2.0-mm high-speed burr drill. The hole was deepened to 35 mm by using a 2.5-mm hand drill and subsequently tapped to 4.5 mm. After PLIF, adequate-sized screws and rods were inserted.
Outcome measure
The following imaging indicators were measured based on the postoperative CT scans.
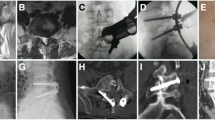
Intrapedicular accuracy
Screw accuracy was evaluated according to the Gertzbin and Robbins scale [28] (Fig. 1). Grade A (no cortical penetration); grade B (the distance of cortical penetration ≤ 2 mm); grade C (2 mm ≤ the distance of cortical penetration < 4 mm); grade D (4 mm ≤ the distance of cortical penetration < 6 mm); grade E (the distance of cortical penetration ≥ 6 mm). Grade A was regarded as the excellent position, grades A and B indicated clinically acceptable positions, while grades C, D, and E were considered clinically unacceptable positions.
Screw violation grade
The grade of proximal FJV was determined in accordance with the Babu scale [29] (Fig. 1) and was classified as grade 0 (screw not in facet), grade 1 (screw in lateral facet but not in facet articulation), grade 2 (penetration of facet articulation less than 1 mm), and grade 3 (penetration of facet articulation more than 1 mm or traveling within the facet articulation).
Other variables were also measured during assessment of the postoperative CT scan, such as the incision depth (defined as the distance between the L4 lamina and skin), superior facet angle (measured as described by Grobler et al. [30], Fig. 2) and the degree of L4 vertebral slippage. Radiographic data were independently measured by two spinal surgeons, who had professionally mastered the measurement methods for screw accuracy, detection of proximal FJV and related indicators. If divergences existed between the two evaluators, a third evaluator made the final decision. As secondary parameters, we recorded the surgical time from skin to skin (min), intraoperative blood loss (mL), postoperative drainage (mL), drop in hemoglobin after surgery (g/L), postoperative hospital stay (days), and perioperative complications (e.g. dural tear, wound infections, intraoperative revision caused by screw malposition and neurologic deficit). The preoperative diagnosis, age, sex, BMI, VAS score for back pain, and VAS score for leg pain were also noted for each patient.
Statistical analysis
Statistical analyses were performed using SPSS 25.0 software (IBM Corp., Armonk, New York, USA). Continuous variables were presented as the mean and standard deviation. Analysis of variance was carried out to compare variables among the three groups and the least significant difference (LSD) method was used for subsequent pairwise comparisons. P < 0.05 was considered statistically significant. The rank-sum test was used under the condition of heterogeneity of variance, and the post hoc Bonferroni correction for multiple comparisons was applied (significance level adjusted to 0.0167). Categorical variables were expressed as absolute (no.) and relative (%) frequencies, and the chi-square test was used for analysis. Interobserver reliabilities for screw accuracy and FJV assessment were measured with the weight kappa coefficient. The reliabilities were high (κ = 0.867 and 0.892, respectively), indicating that the measurements were reliable. The factors that affected the intrapedicular accuracy and proximal FJV were explored through univariable analysis in terms of sex, age, BMI, superior facet angle, implantation technique, vertebral slip more than 10%, and incision depth. Binary logistic regression with the enter method was used, and the final model maintained only the predictors with a significance level < 0.05 during the univariable analysis (if there were few influencing factors, the inclusion level was relaxed to 0.1). All findings were reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [31].
Results
Demographic data
CTs were unavailable in 14 patients (7.8%) due to refusal. A total of 166 patients were included in the present study, including 65 males and 101 females. Among them, 55 patients underwent RA screw insertion, 60 patients underwent PS screw insertion, and 51 patients underwent CBT screw insertion. No significant differences were observed in terms of sex, age, body mass index (BMI), preoperative diagnosis, or preoperative pain score (P > 0.05) (Table 1).
Perioperative data
The drop in hemoglobin after surgery and the incidence of adverse events were not significantly different among the three groups (P = 0.788, P = 0.313, Table 2). Compared to the other two groups, the RA group had a lower intraoperative blood loss, postoperative drainage, and postoperative hospital stay but had a longer surgical time. Meanwhile, the CBT group had a similar postoperative drainage and postoperative hospital stay but lower intraoperative blood loss and a longer surgical time than the PS group (Table 3).
Screw accuracy
The rates of optimal screw (Grade A) in the RA, PS, and CBT groups were 87.3%, 81.3%, and 76.5%, respectively (Table 4). Pairwise comparisons revealed that the difference between the RA and CBT groups was statistically significant (P = 0.004) (Table 5). In addition, the rates of clinically acceptable screw (Grade A + B) were 98.2%, 97.5%, and 94.1%, indicating no significant differences among the three techniques (P = 0.616, 0.028, 0.072) (Table 5).
Superior FJV
Superior FJVs occurred in 28.2% of screws in the RA group and 21.6% of screws in the CBT group. In the PS group, the rate reached 45%. The RA and CBT groups had fewer superior FJVs than the PS group (P = 0.008 and P < 0.001, respectively), and no significant difference was observed between the RA and CBT groups (P = 0.267) (Table 5).
Factors associated with intrapedicular accuracy and FJV
CBT screw technique, BMI and incision depth were included in the final logistic regression analysis model of intrapedicular accuracy (P < 0.1) (Table 6). The results demonstrated that the CBT screw technique was an independent risk factor for intrapedicular accuracy (odds ratio [OR] = 3.527, P = 0.007) (Table 7). Age, the conventional PS technique, superior facet angle and pedicle cortex penetration were associated with FJVs in the univariable analysis (P < 0.05, Table 8). Binary logistic regression analysis was conducted with these variables, and the following independent factors for FJV were identified: superior facet angle (OR = 0.931, P < 0.001), PS (OR = 3.508, P < 0.001), and age (OR = 1.039, P = 0.003) (Table 9).
Discussion
As lumbar fusion has become increasingly used in clinical practice, the incidence of ASD, one of the late complications of this procedure, has also increased gradually [7]. Superior FJV, as an important risk factor for ASD [6,7,8], has attracted increasing attention. Since screw malposition may cause serious complications [32], the safety and accuracy of screw placement are critical. Thus, different insertion techniques have been applied to increase intrapedicular accuracy and reduce the incidence of superior FJVs [13, 19, 24]. The RA and CBT techniques are novel screw placement methods that have been reported to be associated with a low incidence of FJVs [18, 19, 33, 34]. However, the FJV incidence of these two techniques has not been compared. In terms of screw accuracy, the literature reporting on these two techniques has not been consistent [21, 23, 25, 27]. Therefore, we analyzed the screw accuracy and FJV incidence of RA and CBT in the same study and compared them with those of conventional PS insertion.
Screw accuracy and risk factors
The combined results of the intrapedicular accuracy of RA screw placement in previously published literatures are not consistent. Kim et al. [24] found no remarkable difference between RA (Renaissance, Israel) and freehand pedicle screw insertion. By using the same robot navigation system, Molliqaj et al. [23] found that RA screw placement had higher accuracy than the freehand technique (93.4% vs. 88.9%), while Ringel et al. [21] found that RA screws were less accurate than conventional screws (85% vs. 93%), and most malpositioned RA screws were laterally deviated (SpineAssist, Israel). In the present study, we used the TiRobot system (TINAVI Medical Technologies, Beijing, China). TINAVI robot-assisted screw placement can remarkably improve the precision of screws [13, 35]. The results of the present study show that the RA screws had the highest accuracy (98.3% clinically acceptable screws), no grade D and E accuracies, no screw-related complications, and high surgical safety.
Few studies have focused on assessing the insertion accuracy for CBT screws. Thus, there is no specific accuracy criterion for CBT screws. However, some researchers have applied the evaluation methodology of traditional pedicle screws to CBT screws [25, 36]. Tan et al. [27] used 3D imaging and visualization software to study the safety of freehand CBT techniques and found that 78% of the screws had ideal and safety trajectories, while the remaining 22% were unsafe. Ishii et al. [25] studied the accuracy of freehand CBT screw insertion and found that 3.3% were unacceptable, while 2.2% required revision. Based on their experience in CBT screw placement with more than 20 human cadavers for biomechanical study, the operator in our study used bone anatomical landmarks combined with intraoperative fluoroscopy. The results showed 94.1% acceptable screw insertion for CBT, a 5.9% unacceptable screw rate, and a 7.9% perioperative complication rate with no serious complications that required reoperation. The screw accuracy of the CBT technique in our study was high but still lower than that of the other two techniques. Multivariable analyses revealed that the CBT screw technique is an independent risk factor for screw accuracy. Given that the CBT technique was developed in the last 10 years, it has been applied far less often than the conventional PS procedure. Additional experience and improvements in the technique could further increase the screw placement accuracy of this procedure.
Superior FJV and risk factors
The current study demonstrated that the RA and CBT techniques can reduce the incidence of FJVs, and no substantial difference was observed between these two groups. The lower rate of FJVs in RA screw placement can be explained by the mechanism of guidance. The TiRobot system used in this study can choose the entry point and trajectory of the screws during planning. When facet joint invasion is observed on the blueprint, we can move the entry point outside, increase the screw tilt angle, and effectively avoid an FJV. This phenomenon is difficult to actualize in conventional open surgery, because the outward migration of the entry point needs to overcome the resistance of the paravertebral soft tissues and requires wide muscle dissection. Similarly, the CBT screw technique can effectively reduce the FJV rate because the entry point of the CBT screw is near the pars articularis, which is far from the superior facet joint, and because of the downsizing of the screw diameter (4.5–5.5 mm), and this configuration can reduce the probability of joint damage.
With a high FJV rate, the conventional PS insertion technique was an independent risk factor for FJVs in our study. Chen et al. [37] and Chung et al. [38] studied the incidence of FJVs in several commonly used insertion methods for conventional PS and found that the lowest incidence of FJVs was achieved with the intersection technique, followed by the Weinstein technique and the mamillary process technique, whereas the Roy-Camille method had the highest incidence, reaching up to 100%. Considering that the Roy-Camille method requires removal of the tip of the superior articular process, the screw invades the joint when it is screwed into the tail touching the facet joint. However, patients with serious degeneration, unclear anatomical landmarks, and high soft tissue tenson are very common in clinical practice, and we are obliged to move inside the entry point, remove the tip of the superior articular process, and pass through the exposed spongy bone into the pedicle. Under these conditions, the RA and CBT techniques are recommended.
In addition, the present study revealed that a smaller facet angle and older age were significant risk factors independent of the surgical technique. Teles et al. [39] and Patel et al. [40] compared the incidence of FJVs between percutaneous and open screw placement and found that facet angle was an independent risk factor for FJVs. The morphology of the facet joint varies greatly among individuals. The direction of the facet joint from L1 to L5 gradually decreases from the sagittal position to the coronal position [41]. Under a smaller facet angle, the facet joint tends to the coronal position, making it more likely for the screw to invade the facet joint regardless of the technique of screw placement [19].
The effect of age on FJV has not been fully elucidated. Zeng et al. [42] and Patel et al. [40] found that age < 60 years was an independent risk factor for FJV during percutaneous and open screw placement. However, Matsukawa et al. [43] found that age > 70 years was a risk factor for FJV for CBT screws. Similar to the findings of Matsukawa et al., older age in the present study was an independent risk factor for the occurrence of FJVs. The occurrence of FJVs is multifactorial. Young patients have developed paravertebral muscle and high soft tissue tension, thus affecting screw implantation [40, 42]. Severe degeneration of the facet joint in elderly patients makes the choice of entry point difficult and increases the risk of FJVs [43]. During RA screw placement, the entry point is selected according to the planned path. The guide is tension-free, which greatly reduces the impact of the paravertebral soft tissue on the screw placement. The trajectory of CBT screws diverges, and the process of screw placement is less affected by the paravertebral muscles. Therefore, age is an independent risk factor for FJV. This phenomenon also reflects the advantages of the RA and CBT techniques for young patients with developed paravertebral muscle. Therefore, the use of an appropriate implantation technique according to the situation of the patient can reduce the occurrence of FJVs.
Perioperative data
The RA group had the lowest intraoperative blood loss, postoperative drainage, and postoperative hospital stay, but had the longest surgical time, which is consistent with previous studies [35, 36]. The long surgical time of RA screw placement is attributed to greater intraoperative preparation and the learning curve effect [13]. Lower intraoperative blood loss and a longer surgical time were observed in the CBT group compared with the PS group. Owing to the reduced muscle dissection and shorter incision length, the CBT screw technique can reduce intraoperative blood loss [37]. The longer surgical time is possibly due to the surgeon’s lack of familiarity with the technique [38]. The operation time can be further shortened owing to the potential time saved by the more limited exposure required for CBT screw placement.
The data of the 16 patients in the CBT group were used in our previous article [19], in which screw accuracy and FJV incidence between the CBT and PS placement techniques were compared. In the present study, we increased the number of patients and added the RA group. The superiority of the RA and CBT procedures in superior facet joint protection was compared, that never been reported in previous studies.
We recognize that our study has several limitations. First, although no significant difference was found in the general data of the three groups, a possible bias still existed because this was not a randomized control trial. Second, not all patients had postoperative CT scans (14 patients (7.8%) refused the CT scan because of concerns about radiation damage), which may have biased the results. Third, the clinical effects among the three insertion techniques were not reported in the current study, and the relationship between the different grades of violation and clinical outcomes needs further investigation in future work. Prospective trials with large sample sizes and high quality are also needed in the future.
Conclusions
The RA and CBT techniques were associated with fewer proximal FJVs than the PS technique. The RA technique showed a higher rate of intrapedicular accuracy than the CBT technique. The CBT technique was independently associated with screw inaccuracy. Older age, conventional PS technique and coronal orientation of the facet join were independent risk factors for superior FJV.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASD:
-
Adjacent segment degeneration
- BMI:
-
Body mass index
- CBT:
-
Cortical bone trajectory screw
- CT:
-
Computed tomography
- FJV:
-
Facet joint violation
- LCS:
-
Lumbar canal stenosis
- LDH:
-
Lumbar discal hernia
- MIS-TLIF:
-
Minimal invasive transforaminal lumbar interbody fusion
- PEEK:
-
Polyetheretherketone
- PS:
-
Pedicle screw
- RA:
-
Robot-assisted
- SPL:
-
Spondylolisthesis
- PLIF:
-
Posterior lumbar interbody fusion
- VAS:
-
Visual analogue scale/score
References
Vaccaro AR, Garfin SR. Pedicle-screw fixation in the lumbar spine. J Am Acad Orthop Surg. 1995;3(5):263–74.
Boden SD. Overview of the biology of lumbar spine fusion and principles for selecting a bone graft substitute. Spine (Phila Pa 1976). 2002;27(16 Suppl 1):S26–31.
Irmola TM, Häkkinen A, Järvenpää S, Marttinen I, Vihtonen K, Neva M. Reoperation rates following instrumented lumbar spine fusion. Spine. 2018;43(4):295–301.
Yang JY, Lee J, Song H. The impact of adjacent segment degeneration on the clinical outcome after lumbar spinal fusion. Spine (Philadelphia, Pa 1976). 2008;33(5):503–7.
Yugué I, Okada S, Masuda M, Ueta T, Maeda T, Shiba K. Risk factors for adjacent segment pathology requiring additional surgery after single-level spinal fusion: impact of pre-existing spinal stenosis demonstrated by preoperative myelography. Eur Spine J. 2016;25(5):1542–9.
Bagheri SR, Alimohammadi E, Zamani Froushani A, Abdi A. Adjacent segment disease after posterior lumbar instrumentation surgery for degenerative disease: incidence and risk factors. J Orthop Surg-Hong K. 2019;27(2):920543725.
Lau K, Samartzis D, To N, Harada GK, An HS, Wong A. Demographic, surgical, and radiographic risk factors for symptomatic adjacent segment disease after lumbar fusion: a systematic review and meta-analysis. J Bone Jt Surg Am. 2021;103(15):1438–50.
Oh HS, Seo HY. The relationship between adjacent segment pathology and facet joint violation by pedicle screw after posterior lumbar instrumentation surgery. J Clin Med. 2021. https://doi.org/10.3390/jcm10132911.
Wang H, Ma L, Yang D, Wang T, Liu S, Yang S, Ding W. Incidence and risk factors of adjacent segment disease following posterior decompression and instrumented fusion for degenerative lumbar disorders. Medicine. 2017;96(5): e6032.
Cardoso MJ, Dmitriev AE, Helgeson M, Lehman RA, Kuklo TR, Rosner MK. Does superior-segment facet violation or laminectomy destabilize the adjacent level in lumbar transpedicular fixation? An in vitro human cadaveric assessment. Spine (Phila Pa 1976). 2008;33(26):2868–73.
Y X, X L, Q Z, S K, H L, F D, Z S, B L, D H, Z L et al: Superior-segment bilateral facet violation in lumbar transpedicular fixation, Part III: a biomechanical study of severe violation. Spine. 2020.
Jones-Quaidoo SM, Djurasovic M, Owens RN, Carreon LY. Superior articulating facet violation: percutaneous versus open techniques. J Neurosurg Spine. 2013;18(6):593–7.
Han X, Tian W, Liu Y, Liu B, He D, Sun Y, Han X, Fan M, Zhao J, Xu Y, et al. Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomized controlled trial. J Neurosurg Spine. 2019;30(5):615–22.
Kantelhardt SR, Martinez R, Baerwinkel S, Burger R, Giese A, Rohde V. Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J. 2011;20(6):860–8.
Marengo N, Berjano P, Cofano F, Ajello M, Zenga F, Pilloni G, Penner F, Petrone S, Vay L, Ducati A, et al. Cortical bone trajectory screws for circumferential arthrodesis in lumbar degenerative spine: clinical and radiological outcomes of 101 cases. Eur Spine J. 2018;27(Suppl 2):213–21.
Sakaura H, Miwa T, Yamashita T, Kuroda Y, Ohwada T. Cortical bone trajectory screw fixation versus traditional pedicle screw fixation for 2-level posterior lumbar interbody fusion: comparison of surgical outcomes for 2-level degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2018;28(1):57–62.
Gao S, Lv Z, Fang H. Robot-assisted and conventional freehand pedicle screw placement: a systematic review and meta-analysis of randomized controlled trials. Eur Spine J. 2018;27(4):921–30.
Zhang Q, Xu YF, Tian W, Le XF, Liu B, Liu YJ, He D, Sun YQ, Yuan Q, Lang Z, et al. Comparison of superior-level facet joint violations between robot-assisted percutaneous pedicle screw placement and conventional open fluoroscopic-guided pedicle screw placement. Orthop Surg. 2019;11(5):850–6.
Zhang R, Zhou L, Zhang L, Zhang H, Ge P, Jia C, Zhang Y, Zhang J, Shen C. The rates and risk factors of intra-pedicular accuracy and proximal facet joint violation for single-level degenerative lumbar diseases. Spine. 2021;46(23):E1274–82.
Marengo N, Ajello M, Pecoraro MF, Pilloni G, Vercelli G, Cofano F, Zenga F, Ducati A, Garbossa D. Cortical bone trajectory screws in posterior lumbar interbody fusion: minimally invasive surgery for maximal muscle sparing—a prospective comparative study with the traditional open technique. Biomed Res Int. 2018;2018:1–7.
Ringel F, Stüer C, Reinke A, Preuss A, Behr M, Auer F, Stoffel M, Meyer B. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws. Spine. 2012;37(8):E496–501.
Marcus HJ, Cundy TP, Nandi D, Yang G, Darzi A. Robot-assisted and fluoroscopy-guided pedicle screw placement: a systematic review. Eur Spine J. 2014;23(2):291–7.
Molliqaj G, Schatlo B, Alaid A, Solomiichuk V, Rohde V, Schaller K, Tessitore E. Accuracy of robot-guided versus freehand fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery. Neurosurg Focus. 2017;42(5):E14.
Kim H, Jung W, Chang B, Lee C, Kang K, Yeom JS. A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery. Int J Med Robot Comput Assist Surg. 2017;13(3): e1779.
Ishii M, Ohnishi A, Yamagishi A, Ohwada T. Freehand screw insertion technique without image guidance for the cortical bone trajectory screw in posterior lumbar interbody fusion: what affects screw misplacement? J Neurosurg Spine. 2021;36:1–7. https://doi.org/10.3171/2021.2.SPINE202145.
Maruo K, Arizumi F, Kusuyama K, Kishima K, Tachibana T. Accuracy and safety of cortical bone trajectory screw placement by an inexperienced surgeon using 3D patient-specific guides for transforaminal lumbar interbody fusion. J Clin Neurosci. 2020;78:147–52.
Tan Z, McLachlin S, Whyne C, Finkelstein J. Validation of a freehand technique for cortical bone trajectory screws in the lumbar spine. J Neurosurg Spine. 2019;31(2):201–8.
Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976). 1990;15(1):11–4.
Babu R, Park JG, Mehta AI, Shan T, Grossi PM, Brown CR, Richardson WJ, Isaacs RE, Bagley CA, Kuchibhatla M, et al. Comparison of superior-level facet joint violations during open and percutaneous pedicle screw placement. Neurosurgery. 2012;71(5):962–70.
Grobler LJ, Robertson PA, Novotny JE, Pope MH. Etiology of spondylolisthesis. Assessment of the role played by lumbar facet joint morphology. Spine (Phila Pa 1976). 1993;18(1):80–91.
Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(5):31.
Katonis P, Christoforakis J, Kontakis G, Aligizakis AC, Papadopoulos C, Sapkas G, Hadjipavlou A. Complications and problems related to pedicle screw fixation of the spine. Clin Orthop Relat Res. 2003;411:86–94.
Zhou L, Zhang R, Li H, Shen C. Comparison of cranial facet joint violation rate and four other clinical indexes between robot-assisted and freehand pedicle screw placement in spine surgery: a meta-analysis. Spine (Philadelphia, Pa 1976). 2020;45(22):E1532–40.
Sakaura H, Ikegami D, Fujimori T, Sugiura T, Mukai Y, Hosono N, Fuji T. Early cephalad adjacent segment degeneration after posterior lumbar interbody fusion: a comparative study between cortical bone trajectory screw fixation and traditional trajectory screw fixation. J Neurosurg Spine. 2020;32(2):155–9.
Zhang Q, Han X, Xu Y, Liu Y, Liu B, He D, Sun Y, Tian W. Robot-assisted versus fluoroscopy-guided pedicle screw placement in transforaminal lumbar interbody fusion for lumbar degenerative disease. World Neurosurg. 2019;125:e429–34.
Ding H, Han B, Hai Y, Liu Y, Guan L, Pan A, Liu T. The feasibility of assessing the cortical bone trajectory screw placement accuracy using a traditional pedicle screw insertion evaluation system. Clin Spine Surg. 2021;34(2):E112–20.
Chen Z, Zhao J, Xu H, Liu A, Yuan J, Wang C. Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J. 2008;17(11):1476–80.
Chung KJ, Suh SW, Swapnil K, Yang JH, Song HR. Facet joint violation during pedicle screw insertion: a cadaveric study of the adult lumbosacral spine comparing the two pedicle screw insertion techniques. Int Orthop. 2007;31(5):653–6.
Teles AR, Paci M, Gutman G, Abduljabbar FH, Ouellet JA, Weber MH, Golan JD. Anatomical and technical factors associated with superior facet joint violation in lumbar fusion. J Neurosurg Spine. 2018;28(2):173.
Patel JY, Kundnani VG, Merchant ZI, Jain S, Kire N. Superior facet joint violations in single level minimally invasive and open transforaminal lumbar interbody fusion: a comparative study. Asian Spine J. 2020;14(1):25–32.
Tian W, Xu Y, Liu B, Liu Y, He D, Yuan Q, Lang Z, Lyu Y, Han X, Jin P. Lumbar spine superior-level facet joint violations: percutaneous versus open pedicle screw insertion using intraoperative 3-dimensional computer-assisted navigation. Chin Med J-Peking. 2014;127(22):3852–6.
Zeng Z, Jia L, Xu W, Yu Y, Hu X, Jia Y, Wang J, Cheng L. Analysis of risk factors for adjacent superior vertebral pedicle-induced facet joint violation during the minimally invasive surgery transforaminal lumbar interbody fusion: a retrospective study. Eur J Med Res. 2015. https://doi.org/10.1186/s40001-015-0174-9.
Matsukawa K, Kato T, Yato Y, Sasao H, Imabayashi H, Hosogane N, Asazuma T, Chiba K. Incidence and risk factors of adjacent cranial facet joint violation following pedicle screw insertion using cortical bone trajectory technique. Spine (Philadelphia, Pa 1976). 2016;41(14):E851–6.
Acknowledgements
Not applicable.
Funding
We received funding from The Clinical Research Project of the First Affiliated Hospital of Anhui Medical University (Grant Number LCYJ2021ZD002).
Author information
Authors and Affiliations
Contributions
H-QZ: Analysis and interpretation of data, drafting the article; C-CW: Data curation, analysis and interpretation of data; R-JZ: Revising it critically for important intellectual content; L-PZ: Acquisition of data (Software measurement); C-YJ: Acquisition of data (Software measurement); PG: Acquisition of data; C-LS: The conception and design of the study and final approval of the version to be submitted. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Institutional Review Boards of the First Affiliated Hospital of Anhui medical University and was performed in accordance with the Declaration of Helsinki and current ethical guidelines. Written informed consent was obtained from all the study participants.
Consent for publication
Not applicable.
Competing interests
The authors confirm that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, HQ., Wang, CC., Zhang, RJ. et al. Predictors of accurate intrapedicular screw placement in single-level lumbar (L4-5) fusion: robot-assisted pedicle screw, traditional pedicle screw, and cortical bone trajectory screw insertion. BMC Surg 22, 284 (2022). https://doi.org/10.1186/s12893-022-01733-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-022-01733-6