Abstract
Compulsivity is considered a transdiagnostic dimension in obsessive–compulsive and related disorders, characterized by heterogeneous cognitive and behavioral phenotypes associated with abnormalities in cortico-striatal-thalamic-cortical circuitry. The present study investigated the structural morphology of white and gray matter in rats selected for low- (LD) and high- (HD) compulsive drinking behavior on a schedule-induced polydipsia (SIP) task. Regional brain morphology was assessed using ex-vivo high-resolution magnetic resonance imaging (MRI). Voxel-based morphometry of segmented MRI images revealed larger white matter volumes in anterior commissure and corpus callosum of HD rats compared with LD rats. HD rats also showed significantly larger regional volumes of dorsolateral orbitofrontal cortex, striatum, amygdala, hippocampus, midbrain, sub-thalamic nucleus, and cerebellum. By contrast, the medial prefrontal cortex was significantly smaller in HD rats compared with LD rats with no significant group differences in whole brain, ventricular, or cerebrospinal fluid volumes. These findings show that limbic cortico-basal ganglia structures implicated in impulse control disorders are distinct in rats that are vulnerable to develop compulsive behavior. Such abnormalities may be relevant to the etiology of compulsive disorders in humans.
Similar content being viewed by others
Compulsions are repetitive, stereotyped thoughts and behaviors designed to reduce harm and are performed according to rigid rules [1]. Compulsive behaviors are driven by repetitive urges and typically involve the experience of limited voluntary control over these urges [2]. Compulsions are not only a central symptom of obsessive–compulsive disorder (OCD), the paradigmatic example of compulsivity [3], but are also present in other neuropsychopathological conditions such as schizophrenia, autism spectrum disorder (ASD), attention-deficit hyperactivity disorder (ADHD), and addiction [4,5,6]. Obsessive Compulsive and Related Disorders (OCRDs) [4] includes body dysmorphic, hoarding, hair-pulling, skin picking and olfactory reference disorders and hypochondriasis, all sharing compulsions as a cardinal characteristic [7].
Regarding compulsive symptomatology, there are different and heterogeneous cognitive and behavioral phenotypes, related to response inhibition, cognitive flexibility, planning (and goal-directed behavior), working memory, and error monitoring [6]. Behavioral and cognitive variability may be caused by distinct aberrant brain circuits centered on the ‘‘cortico-striatal loop’’ system [8, 9]. Magnetic Resonance Imaging (MRI) studies have demonstrated increased connectivity between Prefrontal Cortex (PFC) and striatum in OCD [10,11,12]. Thus, several studies reveal a dorsolateral Prefrontal Cortex (dlPFC)—striatum hypoactivity and a compensatory activation of Anterior Cingulate Cortex and ventrolateral Prefrontal Cortex (vlPFC) in non-medicated OCD [13] and first-degree OCD relatives [14]. Moreover, OCD patients show ventromedial Prefrontal Cortex (vmPFC) hypoactivity during a recall memory task [15] or during symptom provocation [16] and a lack of a safety signal computed by this structure [17]. There is also a relationship between the OFC and the striatum in OCD patients confirmed by meta-analyses of a variety of neuroimaging studies [18]. Moreover, there exists a hyperactivity of the lateral OFC in OCD patients during symptom provocation normalized over the course of behavioral therapy [19]. Finally, this frontostriatal dysregulation present in OCD patients is normalized by Deep Brain Stimulation (DBS) in the ventral striatum and transcranial magnetic stimulation in the mPFC [10, 20].
However, inhibitory control deficit seems to be driven by different brain areas and its aberrant connectivity with the cortico-striatal system. For instance, inputs to the striatum are relayed from midbrain neurons in Ventral Tegmental Area (VTA) and Substantia Nigra (SN) [21,22,23]. Plasticity mechanisms in these areas are implicated in habit formation [24] and in a multitude of pathological conditions, including OCD, ADHD, Parkinson disease, Huntington disease, Tourette syndrome, and schizophrenia [25]. Hippocampus and amygdala are postulated to play a central role in the neurobiology of OCD through mediation of cognitive and affective processes. Volumetric abnormalities in hippocampus [26,27,28,29,30], its subregions [31,32,33], and amygdala [34,35,36,37] are reported in disorders with compulsive symptomatology. Furthermore, neuromodulation intervention of OCD points to several areas that may also be involved in the expression of compulsive symptoms: Presupplementary Motor Area (PSMA) and Supplementary Motor Area (SMA) are the most promising brain regions for Transcranial Direct Current Stimulation (tDCS) [38,39,40,41,42] and Subthalamic Nucleus (STN) seems to be an effective target for DBS [43,44,45]. Finally, increasing evidence reveals the cerebellum as an important structure of fronto-striatal circuit [46,47,48,49], highlighting its important role in higher-order cognitive functions [50, 51]. Clinical studies have found that the connectivity between cerebellum and PFC is lower, while connectivity with basal ganglia is stronger in OCD patients [14] suggesting less top-down control over the PFC on the lower regions.
Schedule-induced polydipsia (SIP) procedure is characterized by the development of an adjunctive behavior of excessive drinking in food-deprived animals exposed to intermittent food-reinforcement schedules [52, 53]. Translationally, psychogenic polydipsia is a similar phenomenon characterized by compulsive non-regulatory fluid consumption present in > 20% of chronic psychiatric patients, that has been linked compulsive spectrum disorders [54,55,56,57]. As drinking behavior on SIP is an excessive, persistent, and maladaptive behavior, SIP is one of the most well-established preclinical models for the study of neuropsychopathological disorders presenting compulsive behavior such as OCD, schizophrenia and alcohol abuse [58,59,60,61,62]. Thus, SIP seems to meet the criteria as a valid model of compulsive behavior [60]. Moreover, different studies have demonstrated relevant individual differences in SIP acquisition [63,64,65]. Indeed, two populations can be selected according to their SIP acquisition: High Drinker (HD) rats, considered as compulsive, versus Low Drinker (LD) rats, considered as non-compulsive [60]. SIP preclinical model allows us to identify a compulsive vulnerable population to study the brain correlates underlying compulsive spectrum disorders due to their transdiagnostic profile [60, 66].
The aim of the present study was to investigate the morphology of brain differences in white and gray matter structures in the compulsive phenotype of rats selected by SIP using high-resolution magnetic resonance imaging, in order to clarify the neuroanatomical substrates related to OCRDs.
Methods and materials
Animals
Twenty-four male Wistar rats from Envigo (Barcelona, Spain) were used in the present study. The animals were housed in social groups of four per cage, kept in a temperature-controlled environment at 22 °C, and with a 12:12 h light–dark cycle. Water and food were freely available and environmental enrichment was provided throughout the experiment. After 10 days for habituation animals through controlled feeding were gradually reduced to 85% of their free-feeding body weight. All procedures were conducted in accordance with the Spanish Royal Decree 53/2013 and the European Community Directive (2010/63/EU) for animal research. The present study was also approved by the Animal Research Committee from the University of Almería and complied with the ARRIVE guidelines (Additional file 1).
SIP procedure
Animals were tested in 8 standard operant chambers (32 × 25 × 34 cm) (MED Associates, St. Albans, VT, USA) equipped with a bottle of water, pellet dispenser and ambient light. Animals were exposed to a food pellet presentation using a fixed time 60 s (FT-60 s) schedule during 60 min sessions with free access to a bottle of tap water. Following the protocol described in [60] and after the 20 daily sessions, rats were divided into low drinkers (LD) and high drinkers (HD), depending on whether their water consumption (average of the last 5 sessions) was above or below the median of the group. Amount of water consumed (milliliters), total number of licks in the bottle, and total number of magazine entries were registered [67] (Additional file 1).
Cerebral MRI volumetric assessment
Immediately after the last SIP session and the separation into HD and LD rats, animals were perfused with 4% PFA, and the whole skull was stored in PFA prior to high-resolution ex-vivo analyses in the University of Cambridge. Brains were scanned intact inside the cranium using MRI at 9.4 Tesla using a Bruker BioSpec 94/20 system with the manufacturer-provided 4-channel rat brain array coil with an 86 mm birdcage transmit/receive coil [68]. (Parameters in Additional file 1).
Cerebral MR image processing
The user bias-free automatic pipe-line for image processing included the following steps: Images were treated for bias field correction using the ITK implementation of the N4 algorithm in python [69]. Segmentation of the brain and removal of signal from skull and external tissues was achieved by Brain extraction using the rBET software [70]. A normalization algorithm was implemented in Python to normalize signal intensities from different scans. Finally, each individual brain image was co-registered to a common space using the SIGMA rat brain atlas for reference [71]. For this task we used ANTs, the ANTsX ecosystem for quantitative biological and medical imaging [72]. Segmented regions of interest (ROIs) of the brain atlas were used to calculate volumes and signal intensities for those regions for each individual brain (Additional file 1).
Data analysis
SIP acquisition was analyzed using a two-way repeated-measures analysis of variance (ANOVA), with “group” (LD and HD) as between-subject factor and “sessions” (20 sessions) as the within-subject factor. The differences between groups in the volume of the different cerebral areas were studied using Student’s t-test (T-test). When appropriate, post hoc analyses were performed using Bonferroni correction. Statistical significance was established at p < 0.05. Effect size was reported when appropriate. All analyses were performed using Statistica® software (version 8.0) and all figures were made using GraphPad Prism 8 (Additional file 1).
Results
Screening for compulsivity on the schedule-induced polydipsia task
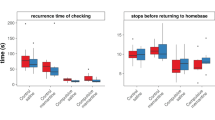
The mean water intake, total licks and total magazine entries in LD and HD over 20 SIP sessions are shown in Fig. 1. Concerning the water intake, repeated measures ANOVA revealed significant differences according to the interaction between the SIP acquisition sessions and LD vs HD (interaction SIP session × group effect: F(19,418) = 14,89, p < 0.001; η2p = 0.4). Repeated measures ANOVA and η2p also showed a significant interaction in total number of licks (interaction SIP session × group effect: F(19, 418) = 5.94, p < 0.001; η2p = 0.21). Post hoc analysis indicated that SIP induced different rates in drinking behavior across the 20 sessions in both groups. In water intake, the LD and HD groups differed in session 5 (p < 0.001; d = 1.65) and the HD group increased their water consumption in session 5 (p < 0.001; d = 2.01) compared to session 1. Similar differences between LD and HD were found in total number of licks: the LD and HD group differed in session 5 (p < 0.01; d = 1.68) and the HD group increased their number of licks in session 5 (p < 0.001; d = 2.18) compared to session 1. There were no significant differences between LD and HD animals in the total magazine entries on SIP (SIP session interaction × group effect: F(19, 418) = 1.23, p = 0.23). Please, note that the effect showed on SIP between HD and LD groups might not be due to a difference in motivation or reward processing, as both groups did not show differences in magazine entries. Therefore, these differences are associated to the performance of excessive and persistent drinking behavior, measured by water consumed and licking behavior on SIP (For a review see [60, 73, 74].
Schedule-Induced Polydipsia. The mean (± SEM) water intake (A), total number of licks (B), and magazine entries (C) in FT-60 s across 20 sessions of Schedule-Induced Polydipsia (SIP) in High drinker (HD, n = 12) and Low drinker (LD, n = 12) rats. *p < 0 .05 indicates significant differences between HD and LD rats from that session onward. #p < 0 .05 indicates significant differences from that session onward compared with session 1 in the same group
Cerebral MRI volumetric assessment
The following subsections show the significant brain volumetric differences in percentage (in relation to total brain volume) between HD and LD rats assessed by MRI and their relationship with SIP. The results are organized into: (1) general measures (whole brain volume, WM, GM, and CSF); (2) WM areas; (3) GM cortical areas; and (4) GM subcortical areas from anterior to posterior according to the Paxinos and Watson [75] brain atlas. In supplementary information: brain volumetric results in mm3 and no significant differences in Additional file 1: Table S1, and correlations between SIP variables and volumetric measures are presented in Additional file 1: Table S2 and S3.
Whole brain gray matter, white matter, and cerebrospinal fluid
The percentage of volume of whole brain, gray matter (GM), white matter (WM), and cerebrospinal fluid (CSF) are shown in Fig. 2. No significant differences between groups were observed in whole brain volume (Fig. 2A; total volume in mm3: df = 22; T-test = 1.19; p = 0.24), GM (Fig. 2B; df = 22; T-test = − 0.93; p = 0.36) or CSF (Fig. 2C; df = 22; T-test = − 1.11; p = 0.28). However, T-test analysis revealed an increased percentage of WM volume in HD animals compared to LD animals (Fig. 2D.; df = 22; T-test = − 2.66; p < 0.05; d = 1.09).
White matter structures
Volume in percentage of WM areas with statistical differences are shown in Fig. 3. T-test analysis revealed that HD animals showed an increased volume in the Corpus Callosum (CC) (Fig. 3B; df = 22; T-test = − 2.95; p < 0.05; d = 1.4) and Anterior Commissure (AC) (Fig. 3C; df = 22; T-test = − 3.1; p < 0.01; d = 1.38) compared to LD animals.
Volumetric MRI data of selected brain white matter structures. (Left). Statistical differences between groups in corpus callosum (CC), and Anterior Commissure (AC). (Right) One sagittal plane (top left), one transverse plane (top right), one coronal plane (bottom right) and a 3D rendered representation (bottom left) of the selected regions of interest analyzed including CC in cyan and AC in red. Data are expressed as the means ± SEM. *p < 0.05; **p < 0.01 indicate significant differences between LD and HD rats. (note: for some 2D views is not possible to visualize all ROIs in a single plain)
Gray matter structures: cortical areas
Volume in percentage of GM cortical areas with statistical differences between groups are shown in Fig. 4. T-test analysis revealed that HD animals showed an increased volume of motor cortex (Fig. 4C; df = 22; T-test = − 2.72; p < 0.05; d = 1) and dlOFC (Fig. 4E; df = 22; T-test = − 2.19; p < 0.05; d = 0.85) compared to LD animals. However, compulsive HD presented a decreased volume of mPFC compared to LD rats (Fig. 4A; df = 22; T-test = 2.54; p < 0.05; d = 1,13).
Volumetric MRI data of selected prefrontal brain grain matter structures. (Left). Statistical differences between groups in A, B medial prefrontral cortex (mPF), C, D Motor Cortex (MC), and E dorsolateral orbitofrontal cortex (dlOFC). (Right) One sagittal plane (top left), one transverse plane (top right), one coronal plane (bottom right) and a 3D rendered representation (bottom left) of the selected regions of interest analyzed including mPFC in magenta, MC in cyan and dlOFC in green. Data are expressed as the means ± SEM. *p < 0.05; **p < 0.01 indicate significant differences between LD and HD rats. (note: for some 2D views is not possible to visualize all ROIs in a single plain)
Water consumed (ml) during the last 5 sessions on SIP correlated with volume of motor cortex (Fig. 4D; r = 0.5; p < 0.05). Moreover, licking behavior during the last 5 sessions on SIP correlated with volume of Motor Cortex (r = 0.57; p < 0.01) and mPFC (Fig. 4B; r = − 0.47; p < 0.05).
Gray matter structures: subcortical anterior areas
Volume in percentage of GM subcortical anterior areas with statistical differences between groups are shown in Fig. 5. T-test analysis revealed that HD animals showed an increased volume in striatum (Fig. 5A; df = 22; T-test = − 2.44; p < 0.05; d = 1.26), and Preoptic Area (POA) (Fig. 5C; df = 22; T-test = − 2.59; p < 0.05; d = 1.17) compared LD rats.
Volumetric MRI data of selected brain gray matter structures. (Left) Statistical differences between groups in A, B) Striatum (ST), and C, D Preoptic area (POA). (Right) One sagittal plane (top left), one transverse plane (top right), one coronal plane (bottom right) and a 3D rendered representation (bottom left) of the selected regions of interest analyzed including Striatum in green and POA in purple. Data are expressed as the means ± SEM. *p < 0.05 indicates significant differences between LD and HD rats
Moreover, water consumed (ml) during the last 5 sessions on SIP correlated with volume of Striatum (Fig. 5B; r = 0.43; p < 0.05) and POA (Fig. 5D; r = 0.51; p < 0.01).
Gray matter structures: subcortical medial areas
Volume in percentage of GM subcortical medial areas with statistical differences between groups are shown in Fig. 6. T-test analysis revealed that HD animals showed increased volume in amygdala (Fig. 6A; df = 22; T-test = − 3.21; p < 0.01; d = 1.54), dentate gyrus (DG) (Fig. 6C; df = 22; T-test = − 2.72; p < 0.05; d = 1.5) and STN (Fig. 6D; df = 22; T-test = − 2.18; p < 0.05; d = 0.91).
Volumetric MRI data of subcortical medial gray matter structures. (Left) Statistical differences between groups in A, B Amygdala, C Dentate gyrus (DG), and D Subthalamic nucleus (STN). (Right) One sagittal plane (top left), one transverse plane (top right), one coronal plane (bottom right) and a 3D rendered representation (bottom left) of the selected regions of interest analyzed including: Amygdala in yellows, DG in cyan and STN in purple. Data are expressed as the means ± SEM. *p < 0.05; **p < 0.01 indicate significant differences between LD and HD rats. (for some 2D views is not possible to visualize all ROIs in a single plain)
Water consumed (ml) during the last 5 sessions on SIP correlated with volume of Amygdala (Fig. 6B; r = 0.47; p < 0.05).
Gray matter structures: subcortical posterior areas
Volume in percentage of GM subcortical posterior areas with statistical differences between groups are shown in Fig. 8. T-test analysis revealed that HD animals showed increased volume in periaqueductal gray (PAG) (Fig. 7A; df = 22; T-test = − 3.2; p < 0.01; d = 2.22), midbrain (Fig. 7C; df = 22; T-test = − 2.46; p < 0.05; d = 0.85) and parasubiculum (PaS) (Fig. 7D; df = 22; T-test = − 2.68; p < 0.05; d = 1.13).
Volumetric MRI data of subcortical posterior gray matter structures. (Left) Statistical differences between groups in A, B Periaqueductal gray matter (PAG), C midbrain, and D parasubiculum (PaS). (Right) One sagittal plane (top left), one transverse plane (top right), one coronal plane (bottom right) and a 3D rendered representation (bottom left) of the selected regions of interest analyzed including: PAG is in green, midbrain in yellow and PaS in purple. Data are expressed as the means ± SEM. *p < 0.05; **p < 0.01 indicate significant differences between LD and HD rats. (note: for some 2D views is not possible to visualize all ROIs in a single plain)
Water consumed (ml) during the last 5 sessions on SIP correlated with volume of PAG (Fig. 7B; r = 0.66; p < 0.001). Moreover, licking behavior during the last 5 sessions on SIP correlated with volume of PAG (r = 0.62; p < 0.001).
Cerebellum
Volume in percentage of cerebellum is shown in Fig. 8. T-test analysis revealed that HD animals showed increased volume in Cerebellum compared to LD animals (Fig. 8B; df = 22; T-test = − 2.37; p < 0.05; d = 0.99).
Volumetric MRI data of Cerebellum. (Left) Statistical differences between groups. (Right) One sagittal plane (top left), one transverse plane (top right), one coronal plane (bottom right) and a 3D rendered representation (bottom left) of the selected regions of interest analyzed including: Gray matter in green and white matter tracks in purple. Data are expressed as the means ± SEM. *p < 0.05; **p < 0.01 indicate significant differences between LD and HD rats
Discussion
The present study explored the possible alterations of the morphology in different brain areas on a compulsive phenotype of rats selected by SIP. The neuroimaging assessment has considered the whole-brain, the cortico-striatal-thalamic-cortical pathway, as well as the associated neurocircuitry that involves the limbic and the cerebellar network. Voxel-based morphometry revealed that compulsive HD rats showed a significantly increased volume of white matter structures (CC and AC), cortical structures (motor cortex and dl OFC), subcortical structures (striatum, amygdala, DG, STN, PAG, and midbrain) and cerebellum relative to LD animals. However, HD rats showed a decreased volume of mPFC compared to LD rats. No differences were observed between HD and LD groups either in the whole brain or in cerebrospinal fluid (CSF) volume. These results highlight and extend the knowledge about brain morphological alterations in the compulsive phenotype, which may underlie the behavioral inhibition deficits observed.
Compulsivity and structural brain assessment: white matter structures
Compulsive HD rats showed an increased general WM volume and its related structures, such as CC and AC compared to LD rats. Different preclinical studies on inhibitory control deficit have also revealed WM alterations. An abnormal increase of WM maturation was observed in an adolescent model of compulsive checking behavior [76], in selectively bred ASD/ADHD-like behavior rats [77], and in animals with repetitive traumatic brain injury (TBI) that showed impulsivity [78]. In line with our result, some studies have shown an increase in CC in an adolescent model of compulsive checking behavior [76], in selectively bred ASD/ADHD-like behavior rats [77], and in a female rat model of Fragile X syndrome characterized by autistic behaviors [79]. Moreover, OCD-like behavior mice exhibited increased c-fos expression in the AC ([80]. In contrast, in a previous study in our laboratory we found that HD rats selected by SIP showed reduced myelin basic protein (MBP) in the CC [61], as well as in a preclinical model of ASD [81, 82].
In line with our current findings, abnormal WM and myelin development have been proposed that may underlie several neuropsychiatric disorders [83]. Clinical studies using MRI observed increased WM in patients with OCD [84] and ASD [85,86,87], and WM volume was positively correlated with the severity of ritualistic/compulsive behaviors in adults and adolescents with anorexia nervosa [88]. However, the relationship between CC and AC and compulsive symptomatology is unclear. An increased CC volume has been linked to doubt-checking subclinical OC symptoms in healthy children [89], in ASD [90] and in pediatric OCD patients [91]. Moreover, the stereotaxic coordinates for DBS treatment for OCD are close to the AC [92]. However, a decreased volume of CC has also been associated with pediatric OCD [93], adult OCD [94], and ASD children [95].
Compulsivity and structural brain assessment: cortico-striatal circuit
The neurocircuitry traditionally involved in habit learning and compulsive behaviors includes the striatum and its connections with frontal cortex regions [24, 96,97,98].
HD compulsive animals showed increased volume of striatum and dlOFC, but reduced volume of mPFC compared to LD rats. In accordance to our findings, a previous study showed that SIP acquisition in rats induced structural plasticity changes by an increase in dendritic spine density in dorsolateral striatum compared to control rats exposed to a mass feeding condition [99]. Moreover, previous studies on SIP have revealed an alteration in the OFC, such as increased c-fos activity in the lOFC in rats with SIP acquisition [58] and in high compulsive rats selected by SIP [100]. Although our result in mPFC contrasts with previous data in our laboratory, where no differences were observed in the PrL cortex and IL cortex volume between HD and LD rats [101], different studies have shown a reduction in mPFC volume in RHA animals characterized by impulsive and compulsive behaviors [102], and in a model of ADHD, the juvenile SHRs rats [103].
In clinical studies, comparable structural abnormalities in these brain areas have been reported. Neuroimaging studies showed increased GM volumes of striatum and its subregions in OCD [104, 105] and in ASD [106, 107]. Striatum volume also showed a positive association with compulsivity scores in subclinical adolescent population [108] and with the severity of restricted and repetitive behaviors in ASD [109]. Moreover, clinical studies in OCD patients have also shown an increased volume of OFC [104]. Finally, in accordance with our findings, some clinical studies have also reported a reduction of mPFC in inhibitory control disorders such as in subjects with online game addiction [110] and in individuals with heavy drinking profile [111]. Indeed, symptom improvement in OCD patients by the cognitive-behavioral therapy correlated with larger volume within the right mPFC [112].
Compulsivity and structural brain assessment: cortico-striatal-thalamic-cortical circuit
In the assessment of the brain neurocircuitry implicated in compulsive behaviors, many authors also consider an extended network that involves other midbrain, thalamic and cortical areas [113].
In this sense, HD animals also presented an increased volume of motor cortex, STN and midbrain. As far as we know, motor cortex volume has not been fully studied in animal models of inhibitory control deficit. However, the different subregions of the motor cortex might have an encompassing role with the cortico-striatal network in a motor inhibition task [114] and in learning of simple sequences [115]. Moreover, when drug seeking is well established, it is under the dominant control of the dorsolateral striatum, which receives its major cortical afferents from the motor cortex [116]. Regarding the role of STN on compulsive behavior, stimulation or inactivation of STN have revealed to ameliorate the inhibitory control deficit in animal models of OCD [117, 118], of compulsive heroin taking [119], and of risk-preferring [120]. Finally, data similar to ours have been found in areas that compose the midbrain, such as increased volume of VTA in models of stress as maternally deprived animals [121], and correlation between maintained drug use despite negative consequences with PAG volume in a rat model of cocaine addiction [122].
Related to clinical studies, OCD patients had greater activation of the SMA during high- vs low-conflict trials in the multi-source interference Task [123] and a disruption in higher-order motor networks has been found in compulsive behavior such as skin-picking symptoms [124]. Moreover, in the clinical context, the bilateral DBS in the STN is a recommended treatment for refractory OCD [125]. Finally, an increase of midbrain [126] have been shown in OCD patients.
Compulsivity and structural brain assessment: the role of limbic and cerebellar areas
Moreover, other relevant brain structures of the limbic network associated with compulsivity are hippocampus and amygdala. The present study found increased volume of the DG of the hippocampus and amygdala in HD rats compared to LD rats. Our data in DG contrasts with previous findings in our lab, where HD group had a reduced dorsal hippocampus volume compared to LD group measured by stereology [101]. However, a classical study showed that hippocampal lesions were followed by a rapid and stable SIP acquisition [127]. Regarding increased amygdala, similar data was found in HD animals [101] and in the high-avoidance Hatano rats [128] that showed increased BLA volume.
Clinical studies have linked hippocampal and amygdalar abnormalities to compulsive symptomatology. An increased volume of hippocampus have been found in OCD patients [33, 104] and in internet GD patients, where the hippocampus volume correlated with symptom severity [129]. Moreover, the association between different subregions of amygdala and compulsive trait have been found in OCD [130, 131], in a sub-clinical population [34], in subjects with compulsive sexual behavior [36] and in individuals with internet GD [129].
In the present experiment, HD animals showed an increase in the volume of cerebellum, which is in line with different cerebellar alterations found in animal models of ASD/ADHD-like behaviors [77] of autism [132], of addiction [133], and in animals with repetitive jumping behavior [134].
In clinical studies, according with our results, a higher volume of different areas of cerebellum was found in ASD [106, 135, 136] and in OCD patients [104, 137,138,139]. Interestingly, cerebellar volume correlated with OC symptom severity in OCD patient [105] and with emotional dysregulation severity in ADHD patients [140].
In summary, our findings reveal a collection of morphological abnormalities implicated in the compulsive phenotype selected by SIP, that suggest a brain network that includes the traditional cortico-striatal-thalamic-cortical circuit and other less studied brain areas of the limbic, and cerebellar circuit, which expand the knowledge about brain areas that might be implicated in inhibitory control. The increased volume of several areas observed might not be attributable to a possible water increment in the brain, because no significant differences were found in the whole brain, ventricles, or CSF volume between groups. Possibly, specific and dissociable circuits within the compulsivity brain network might be associated with different dysfunctions, highlighting the heterogeneity of the plausible endophenotypes of OCD [141].
However, our study presents certain limitations. The volumetric assessment of the brain areas is a powerful analysis tool to identify abnormalities in the morphological functioning of neurocircuits, but the current study is unable to determine the underlying mechanisms of the morphological differences observed. Presumably, the volumetric changes found suggest a possible aberrant plasticity in these brain areas linked to compulsive behavior. In this regard, it is known that variations in the volume of particular brain regions may reflect microscopic alterations including changes in synaptogenesis, dendritic arborization, number of neurites, and neuronal and glial genesis, that might in turn, influence behavioral responses [142,143,144]. Moreover, we have observed morphologic changes in large areas that includes a great diversity in their functional specialization according to each of its substructures. Further understanding of these alterations is necessary for future experiments, which must also be provided with female rats. Another limitation of our study is the discrepancy between the findings in preclinical studies, which might be attributable to the wide variety of models used. This reinforces the translational validity of the neuroimaging studies, since in the clinical literature, this lack of concordance is also found, which might be due to heterogeneity within neurodevelopmental disorders, comorbidity, age onset and effect of psychopharmacology treatments.
The development of compulsive drinking by SIP exposure might induce microstructural abnormalities in the cortico-striatal-thalamic-cortical circuit as well as in limbic and cerebellar areas in HD compulsive rats. These results suggest that SIP might potentially have a time-dependent role in modulating the brain plasticity, specifically in high compulsive vulnerable rats, the HD group selected by SIP. This hypothesis is in consonance with previous data in our laboratory where a brain volumetric assessment did not reveal significant differences between HD and LD rats in basal conditions, but the re-exposure to SIP induced significant changes only in HD animals [101]. Finally, this pattern is also found in the clinical literature, when the potential brain differences in compulsive patients become evident during the exposition to the problem situation [15, 16, 19], supporting SIP as a valid and translational model for the study of compulsivity.
Conclusions
The present MRI study reveals a collection of morphological abnormalities and suggests the implication of frontostriatal circuit and its modulators, which might have different functions linked to compulsive behavior on SIP. HD animals presented increased general WM volume compared to LD animals without differences in GM or CSF volume. HD rats also showed increased volume in white matter structures such as CC and AC. Altered volume of cortical areas were found in HD rats: decreased volume in mPFC and increased volume of Motor Cortex and dlOFC. Moreover, subcortical areas have been increased in HD phenotype: striatum, DG, amygdala, midbrain, PAG and STN. This pattern of alterations might be related to a vulnerability to develop compulsive behavior, which might be exacerbated by SIP exposure, and point toward SIP as a suitable preclinical model for enhancing the knowledge about the vulnerability to OCRDs.
Availability of data and materials
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Chamberlain SR, Odlaug BL, Boulougouris V, Fineberg NA, Grant JE. Trichotillomania: neurobiology and treatment. Neurosci Biobehav Rev. 2009;33(6):831–42. https://doi.org/10.1016/j.neubiorev.2009.02.002.
Figee M, Pattij T, Willuhn I, Luigjes J, van den Brink W, Goudriaan A, Potenza MN, Robbins TW, Denys D. Compulsivity in obsessive-compulsive disorder and addictions. Eur Neuropsychopharmacol. 2016;26(5):586. https://doi.org/10.1016/j.euroneuro.2015.12.003.
Robbins TW, Crockett MJ. Role of Central Serotonin in Impulsivity and Compulsivity: Comparative Studies in Experimental Animals and Humans. In Handbook of Behavioral Neuroscience. 2010;21:415. https://doi.org/10.1016/S1569-7339(10)70093-X.
Bowles T. Book review: diagnostic and statistical manual of mental disorders, fifth edition. Mental Health Clinician. 2013;3(2):107. https://doi.org/10.9740/mhc.n163617.
Hollander E, Kim S, Khanna S, Pallanti S. Obsessive-compulsive disorder and obsessive-compulsive spectrum disorders: diagnostic and dimensional issues. CNS Spectr. 2007;12(S3):5. https://doi.org/10.1017/S1092852900002467.
Robbins TW, Vaghi MM, Banca P. Obsessive-compulsive disorder: puzzles and prospects. Neuron. 2019;102(1):27–47. https://doi.org/10.1016/j.neuron.2019.01.046.
Fineberg NA, Hollander E, Pallanti S, Walitza S, Grünblatt E, Dell’Osso BM, Albert U, Geller DA, Brakoulias V, Reddy YCJ, Arumugham SS, Shavitt RG, Drummond L, Grancini B, De Carlo V, Cinosi E, Chamberlain SR, Ioannidis K, Rodriguez CI, Garg K, Castle D, Van Ameringen V, Stein DJ, Carmi L, Zohar J, Menchon JM. Clinical advances in obsessive-compulsive disorder: a position statement by the International College of Obsessive-Compulsive Spectrum Disorders. Int Clin Psychopharmacol. 2020. https://doi.org/10.1097/YIC.0000000000000314.
Alexander GE, DeLong MR, Strick PL. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Ann Rev Neurosci. 1986. https://doi.org/10.1146/annurev.ne.09.030186.002041.
Haber SN. Corticostriatal circuitry. Dial Clin Neurosci. 2016;18(1):7. https://doi.org/10.31887/dcns.2016.18.1/shaber.
Figee M, Koning PD, Klaassen S, Vulink N, Mantione M, Munckhof PV, Schuurman R, Van Wingen G, Van Amelsvoort T, Booij J, Denys D. Deep brain stimulation induces striatal dopamine release in obsessive-compulsive disorder. Biol Psychiatry. 2014;75(8):647. https://doi.org/10.1016/j.biopsych.2013.06.021.
Harrison BJ, Pujol J, Cardoner N, Deus J, Alonso P, López-Solà M, Contreras-Rodríguez O, Real E, Segalàs C, Blanco-Hinojo L, Menchon JM, Soriano-Mas C. Brain corticostriatal systems and the major clinical symptom dimensions of obsessive-compulsive disorder. Biol Psychiatry. 2013;73(4):321. https://doi.org/10.1016/j.biopsych.2012.10.006.
Harrison BJ, Soriano-Mas C, Pujol J, Ortiz H, López-Solà M, Hernández-Ribas R, Deus J, Alonso P, Yücel M, Pantelis C, Menchon JM, Cardoner N. Altered corticostriatal functional connectivity in obsessive-compulsive disorder. Arch General Psychiatry. 2009;66(11):1189. https://doi.org/10.1001/archgenpsychiatry.2009.152.
Van Den Heuvel OA, Veltman DJ, Groenewegen HJ, Cath DC, Van Balkom AJLM, Van Hartskamp J, Barkhof F, Dyck RV. Frontal-striatal dysfunction during planning in obsessive-compulsive disorder. Arch General Psychiatry. 2005;62(3):301. https://doi.org/10.1001/archpsyc.62.3.301.
Vaghi MM, Hampshire A, Fineberg NA, Kaser M, Brühl AB, Sahakian BJ, Chamberlain SR, Robbins TW. Hypoactivation and dysconnectivity of a frontostriatal circuit during goal-directed planning as an endophenotype for obsessive-compulsive disorder. Biol Psychiatry. 2017;2(8):655. https://doi.org/10.1016/j.bpsc.2017.05.005.
Milad MR, Furtak SC, Greenberg JL, Keshaviah A, Im JJ, Falkenstein MJ, Jenike M, Rauch SL, Wilhelm S. Deficits in conditioned fear extinction in obsessive-compulsive disorder and neurobiological changes in the fear circuit. JAMA Psychiat. 2013;70(6):608. https://doi.org/10.1001/jamapsychiatry.2013.914.
Banca P, Vestergaard MD, Rankov V, Baek K, Mitchell S, Lapa T, Castelo-Branco M, Voon V. Evidence accumulation in obsessive-compulsive disorder: the role of uncertainty and monetary reward on perceptual decision-making thresholds. Neuropsychopharmacology. 2015. https://doi.org/10.1038/npp.2014.303.
Apergis-Schoute AM, Gillan CM, Fineberg NA, Fernandez-Egea E, Sahakian BJ, Robbins TW. Neural basis of impaired safety signaling in obsessive compulsive disorder. Proc Natl Acad Sci USA. 2017;114(12):3216. https://doi.org/10.1073/pnas.1609194114.
Whiteside SP, Port JD, Abramowitz JS. A meta-analysis of functional neuroimaging in obsessive-compulsive disorder. Psychiatry Res Neuroimaging. 2004;132(1):69. https://doi.org/10.1016/j.pscychresns.2004.07.001.
Morgiève M, N’diaye K, Haynes WIA, Granger B, Clair AH, Pelissolo A, Mallet L. Dynamics of psychotherapy-related cerebral haemodynamic changes in obsessive compulsive disorder using a personalized exposure task in functional magnetic resonance imaging. Psychol Med. 2014;44(7):1461. https://doi.org/10.1017/S0033291713002237.
Dunlop K, Woodside B, Olmsted M, Colton P, Giacobbe P, Downar J. Reductions in cortico-striatal hyperconnectivity accompany successful treatment of obsessive-compulsive disorder with dorsomedial prefrontal rTMS. Neuropsychopharmacology. 2016;41(5):1395. https://doi.org/10.1038/npp.2015.292.
Everitt BJ, Robbins TW. Drug addiction: Updating actions to habits to compulsions ten years on. Annu Rev Psychol. 2016;67:23–50. https://doi.org/10.1146/annurev-psych-122414-033457.
Lüscher C. The emergence of a circuit model for addiction. Ann Rev Neurosci. 2016. https://doi.org/10.1146/annurev-neuro-070815-013920.
Volkow ND, Morales M. The brain on drugs: from reward to addiction. Cell. 2015;162(4):712. https://doi.org/10.1016/j.cell.2015.07.046.
Lipton DM, Gonzales BJ, Citri A. Dorsal striatal circuits for habits, compulsions and addictions. Front Syst Neurosci. 2019. https://doi.org/10.3389/fnsys.2019.00028.
Sonne J, Reddy V, Beato MR. Neuroanatomy, Substantia Nigra. In StatPearls (Issue December 2018). 2020.
Atmaca M, Yildirim H, Ozdemir H, Ozler S, Kara B, Ozler Z, Kanmaz E, Mermi O, Tezcan E. Hippocampus and amygdalar volumes in patients with refractory obsessive-compulsive disorder. Progr Neuro-Psychopharmacol Biol Psychiatry. 2008;32(5):1283. https://doi.org/10.1016/j.pnpbp.2008.04.002.
Boedhoe PSW, Schmaal L, Abe Y, Ameis SH, Arnold PD, Batistuzzo MC, Benedetti F, Beucke JC, Bollettini I, Bose A, Brem S, Calvo A, Cheng Y, Cho KK, Dallaspezia S, Denys D, Fitzgerald KD, Fouche J-P, Giménez M, Gruner P, Hanna GL, Hibar DP, Hoexter MQ, Hu H, Huyser C, Ikari K, Jahanshad N, Kathmann N, Kaufmann C, Koch K, Kwon JS, Lazaro L, Liu Y, Lochner C, Marsh R, Martínez-Zalacaín I, Mataix-Cols D, Menchón JM, Minuzzi L, Nakamae T, Nakao T, Narayanaswamy JC, Piras F, Piras F, Pittenger C, Janardhan Reddy YC, Sato JR, Simpson HB, Soreni N, Soriano-Mas C, Spalletta G, Stevens MC, Szeszko PR, Tolin DF, Venkatasubramanian G, Walitza S, Wang Z, van Wingen GA, Xu J, Xu X, Yun J-Y, Zhao Q, Thompson PM, Stein DJ, vanden Heuvel OA, Abe OA, Alonso P,Ameis SH, Arnold PD, Bargalló N, Batistuzzo MC, Benedetti, Beucke JC, Boedhoe PSW, Bollettini I, Bose A, Brem S, Busatto GF, Calvo A, Calvo R, Cath DC, Cheng Y, Cho KK, Dallaspezia S, FE Vries de, Wit SJ, Denys D, Fang Y, Fitzgerald KD, Fontaine M, Fouche J-P, Giménez M, GrunerP, Hanna GL, Hibar DP, Hoexter MQ, Hu H, Huyser C, Ikari K, Jahanshad N, Kathmann N, Kaufmann C, Khadka S, Koch K, SooKwon J, Lazaro L, Liu Y, Lochner C, Marsh R, Martínez-Zalacaín I, Mataix-Cols D, Menchón JM, Miguel EC, Minuzzii L, Morer A, Nakamae T, Nakao T, Narayanaswamy JC, Piras F, Piras F, Pittenger C, JanardhanReddy YC, Sato JR, Simpson HB, Schmaal L, Soreni N, Soriano-Mas C, Spalletta G, Stein DJ, Stevens MC, Szeszko PR, Thompson PM, Tolin DF, Veltman DJ, Venkatasubramanian G, van den Heuvel OA, van der Werf YD, van Wingen GA, Walitza S, Wang Z, Xu J, Xu X, Yun J-Y, Zhao Q. Distinct subcortical volume alterations in pediatric and adult OCD: a worldwide meta- and mega-analysis. Am J Psychiatry. 2017;174(1):60. https://doi.org/10.1176/appi.ajp.2016.16020201.
Hong SB, Shin YW, Kim SH, Yoo SY, Lee JM, Kim IY, Kim SI, Kwon JS. Hippocampal shape deformity analysis in obsessive-compulsive disorder. Eur Arch Psychiatry Clin Neurosci. 2007;257(4):185. https://doi.org/10.1007/s00406-006-0655-5.
Rao S, Raveendranathan D, Shivakumar V, Narayanaswamy JC, Venkatasubramanian G, Reddy YCJ. Hippocampus volume alterations and the clinical correlates in medication naïve obsessive compulsive disorder. J Affect Disord. 2018. https://doi.org/10.1016/j.jad.2018.04.048.
Szeszko PR, Robinson D, Alvir JMJ, Bilder RM, Lencz T, Ashtari M, Wu H, Bogerts B. Orbital frontal and amygdala volume reductions in obsessive-compulsive disorder. Arch General Psychiatry. 1999;56(10):913. https://doi.org/10.1001/archpsyc.56.10.913.
Ahmed-Leitao F, Rosenstein D, Marx M, Young S, Korte K, Seedat S. Posttraumatic stress disorder, social anxiety disorder and childhood trauma: differences in hippocampal subfield volume. Psychiatry Res Neuroimaging. 2019. https://doi.org/10.1016/j.pscychresns.2018.12.015.
Al-Amin M, Zinchenko A, Geyer T. Hippocampal subfield volume changes in subtypes of attention deficit hyperactivity disorder. Brain Res. 2018. https://doi.org/10.1016/j.brainres.2018.02.007.
Vattimo EFQ, dos Santos AC, Hoexter MQ, Frudit P, Miguel EC, Shavitt RG, Batistuzzo MC. Higher volumes of hippocampal subfields in pediatric obsessive-compulsive disorder. Psychiatry Res Neuroimaging. 2021. https://doi.org/10.1016/j.pscychresns.2020.111200.
Kubota Y, Sato W, Kochiyama T, Uono S, Yoshimura S, Sawada R, Toichi M. Corticostriatal-limbic correlates of sub-clinical obsessive-compulsive traits. Psychiatry Res Neuroimaging. 2019. https://doi.org/10.1016/j.pscychresns.2019.01.012.
Pursey KM, Contreras-Rodriguez O, Collins CE, Stanwell P, Burrows TL. Food addiction symptoms and amygdala response in fasted and fed states. Nutrients. 2019;11(6):1285. https://doi.org/10.3390/nu11061285.
Schmidt C, Morris LS, Kvamme TL, Hall P, Birchard T, Voon V. Compulsive sexual behavior: prefrontal and limbic volume and interactions. Hum Brain Mapping. 2017;38(3):1182. https://doi.org/10.1002/hbm.23447.
Szeszko PR, MacMillan S, McMeniman M, Lorch E, Madden R, Ivey J, Banerjee SP, Moore GJ, Rosenberg DR. Amygdala volume reductions in pediatric patients with obsessive-compulsive disorder treated with paroxetine: Preliminary findings. Neuropsychopharmacol. 2004;29(4):826. https://doi.org/10.1038/sj.npp.1300399.
Bation R, Mondino M, Le Camus F, Saoud M, Brunelin J. Transcranial direct current stimulation in patients with obsessive compulsive disorder: a randomized controlled trial. Eur Psychiatry. 2019. https://doi.org/10.1016/j.eurpsy.2019.08.011.
Gowda SM, Narayanaswamy JC, Hazari N, Bose A, Chhabra H, Balachander S, Bhaskarapillai B, Shivakumar V, Venkatasubramanian G, Reddy YCJ. Efficacy of pre-supplementary motor area transcranial direct current stimulation for treatment resistant obsessive compulsive disorder: a randomized, double blinded, sham controlled trial. Brain Stimul. 2019;12(4):922. https://doi.org/10.1016/j.brs.2019.02.005.
Rachid F. Transcranial direct current stimulation for the treatment of obsessive-compulsive disorder? A qualitative review of safety and efficacy. Psychiatry Res. 2019. https://doi.org/10.1016/j.psychres.2018.11.033.
Senço NM, Huang Y, D’Urso G, Parra LC, Bikson M, Mantovani A, Shavitt RG, Hoexter MQ, Miguel EC, Brunoni AR. Transcranial direct current stimulation in obsessive-compulsive disorder: emerging clinical evidence and considerations for optimal montage of electrodes. Expert Rev Med Dev. 2015;12(4):381. https://doi.org/10.1586/17434440.2015.1037832.
Silva AI, Haddon JE, Syed YA, Trent S, Lin TCE, Patel Y, Carter J, Haan N, Honey RC, Humby T, Assaf Y, Owen MJ, Linden DEJ, Hall J, Wilkinson LS. Cyfip1 haploinsufficient rats show white matter changes, myelin thinning, abnormal oligodendrocytes and behavioural inflexibility. Nat Commun. 2019. https://doi.org/10.1038/s41467-019-11119-7.
Chabardès S, Polosan M, Krack P, Bastin J, Krainik A, David O, Bougerol T, Benabid AL. Deep brain stimulation for obsessive-compulsive disorder: subthalamic nucleus target. World Neurosurg. 2013;80(3–4):S31. https://doi.org/10.1016/j.wneu.2012.03.010.
Fontaine D, Mattei V, Borg M, Langsdorff DV, Magnie MN, Chanalet S, Robert P, Paquis P. Effect of subthalamic nucleus stimulation on obsessive-compulsive disorder in a patient with Parkinson disease: case report. J Neurosurg. 2004;100(6):1084. https://doi.org/10.3171/jns.2004.100.6.1084.
Mallet L, Mesnage V, Houeto JL, Pelissolo A, Yelnik J, Behar C, Gargiulo M, Welter ML, Bonnet AM, Pillon B, Cornu P, Dormont D, Pidoux B, Allilaire JF, Agid Y. Compulsions, Parkinson’s disease, and stimulation. Lancet. 2002;360(9342):1302. https://doi.org/10.1016/S0140-6736(02)11339-0.
Anticevic A, Hu S, Zhang S, Savic A, Billingslea E, Wasylink S, Repovs G, Cole MW, Bednarski S, Krystal JH, Bloch MH, Li CSR, Pittenger C. Global resting-state functional magnetic resonance imaging analysis identifies frontal cortex, striatal, and cerebellar dysconnectivity in obsessive-compulsive disorder. Biol Psychiatry. 2014;75(8):595. https://doi.org/10.1016/j.biopsych.2013.10.021.
Barton RA. Embodied cognitive evolution and the cerebellum. Philos Trans Royal Soc B: Biol Sci. 2012;367(1599):2097. https://doi.org/10.1098/rstb.2012.0112.
Bostan AC, Dum RP, Strick PL. The basal ganglia communicate with the cerebellum. Proc Natl Acad Sci USA. 2010;107(18):854. https://doi.org/10.1073/pnas.1000496107.
Miquel M, Nicola SM, Gil-Miravet I, Guarque-Chabrera J, Sanchez-Hernandez A. A working hypothesis for the role of the cerebellum in impulsivity and compulsivity. Front Behav Neurosci. 2019. https://doi.org/10.3389/fnbeh.2019.00099.
Buckner RL. The cerebellum and cognitive function: 25 years of insight from anatomy and neuroimaging. Neuron. 2013;80(3):807. https://doi.org/10.1016/j.neuron.2013.10.044.
Strick PL, Dum RP, Fiez JA. Cerebellum and nonmotor function. Ann Rev Neurosci. 2009;32:413. https://doi.org/10.1146/annurev.neuro.31.060407.125606.
Falk JL. Schedule-induced polydipsia as a function of fixed interval length 1. J Exp Anal Behav. 1966;9(1):37–9. https://doi.org/10.1901/jeab.1966.9-37.
Falk JL. Production of polydipsia in normal rats by an intermittent food schedule. Science. 1961;133(3447):195–6.
De Leon J, Tracy J, McCann E, McGrory A. Polydipsia and schizophrenia in a psychiatric hospital: a replication study. Schizophrenia Res. 2002;57(2–3):293. https://doi.org/10.1016/S0920-9964(01)00292-4.
de Leon J, Verghese C, Tracy JI, Josiassen RC, Simpson GM. Polydipsia and water intoxication in psychiatric patients: a review of the epidemiological literature. Biol Psychiatry. 1994;35(6):408. https://doi.org/10.1016/0006-3223(94)90008-6.
Hawken ER, Crookall JM, Reddick D, Millson RC, Milev R, Delva N. Mortality over a 20-year period in patients with primary polydipsia associated with schizophrenia: a retrospective study. Schizophrenia Res. 2009;107(2–3):128. https://doi.org/10.1016/j.schres.2008.09.029.
Iftene F, Bowie C, Milev R, Hawken E, Talikowska-Szymczak E, Potopsingh D, Hanna S, Mulroy J, Groll D, Millson R. Identification of primary polydipsia in a severe and persistent mental illness outpatient population: a prospective observational study. Psychiatry Res. 2013;210(3):679. https://doi.org/10.1016/j.psychres.2013.04.011.
Gregory JG, Hawken ER, Banasikowski TJ, Dumont EC, Beninger RJ. A response strategy predicts acquisition of schedule-induced polydipsia in rats. Progr Neuro-Psychopharmacol Biol Psychiatry. 2015. https://doi.org/10.1016/j.pnpbp.2015.03.012.
Hawken ER, Beninger RJ. The amphetamine sensitization model of schizophrenia symptoms and its effect on schedule-induced polydipsia in the rat. Psychopharmacology. 2014;231(9):2001–8. https://doi.org/10.1007/s00213-013-3345-9.
Moreno M, Flores P. Schedule-induced polydipsia as a model of compulsive behavior: neuropharmacological and neuroendocrine bases. Psychopharmacology. 2012;219(2):647–59. https://doi.org/10.1007/s00213-011-2570-3.
Navarro SV, Alvarez R, Colomina MT, Sanchez-Santed F, Flores P, Moreno M. Behavioral biomarkers of schizophrenia in high drinker rats: a potential endophenotype of compulsive neuropsychiatric disorders. Schizophr Bull. 2017;43(4):778–87. https://doi.org/10.1093/schbul/sbw141.
Platt B, Beyer CE, Schechter LE, Rosenzweig-Lipson S. Schedule-induced polydipsia: a rat model of obsessive-compulsive disorder. Curr Protocols Neurosci. 2008. https://doi.org/10.1002/0471142301.ns0927s43.
Dantzer R, Terlouw C, Mormède P, Le Moal M. Schedule-induced polydipsia experience decreases plasma corticosterone levels but increases plasma prolactin levels. Physiol Behav. 1988;43(3):275. https://doi.org/10.1016/0031-9384(88)90187-4.
Dantzer R, Terlouw C, Tazi A, Koolhaas JM, Bohus B, Koob GF, Le Moal M. The propensity for schedule-induced polydipsia is related to differences in conditioned avoidance behaviour and in defense reactions in a defeat test. Physiol Behav. 1988;43(3):269. https://doi.org/10.1016/0031-9384(88)90186-2.
Mittleman G, Jones GH, Robbins TW. The relationship between schedule-induced polydipsia and pituitary-adrenal activity: pharmacological and behavioral manipulations. Behav Brain Res. 1988;28(3):315. https://doi.org/10.1016/0166-4328(88)90134-9.
Belin-Rauscent A, Daniel ML, Puaud M, Jupp B, Sawiak S, Howett D, McKenzie C, Caprioli D, Besson M, Robbins TW, Everitt BJ, Dalley JW, Belin D. From impulses to maladaptive actions: the insula is a neurobiological gate for the development of compulsive behavior. Mol Psychiatry. 2016;21(4):491–9. https://doi.org/10.1038/mp.2015.140.
Mora S, Merchán A, Vilchez O, Aznar S, Klein AB, Ultved L, Campa L, Suñol C, Flores P, Moreno M. Reduced cortical serotonin 5-HT2A receptor binding and glutamate activity in high compulsive drinker rats. Neuropharmacology. 2018. https://doi.org/10.1016/j.neuropharm.2018.09.004.
Sawiak SJ, Wood NI, Williams GB, Morton AJ, Carpenter TA. Voxel-based morphometry in the R6/2 transgenic mouse reveals differences between genotypes not seen with manual 2D morphometry. Neurobiol Dis. 2009;33(1):20. https://doi.org/10.1016/j.nbd.2008.09.016.
Tustison NJ, Avants BB, Cook PA, Zheng Y, Egan A, Yushkevich PA, Gee JC. N4ITK: Improved N3 bias correction. IEEE Trans Med Imaging. 2010;29(6):1310. https://doi.org/10.1109/TMI.2010.2046908.
Tobias W, Lythgoe D, Williams S. rBET: Making BET work for Rodent Brains. Proc Int Soc Magn Reson Med. 2013
Barrière DA, Magalhães R, Novais A, Marques P, Selingue E, Geffroy F, Marques F, Cerqueira J, Sousa JC, Boumezbeur F, Bottlaender M, Jay TM, Cachia A, Sousa N, Mériaux S. The SIGMA rat brain templates and atlases for multimodal MRI data analysis and visualization. Nat Commun. 2019. https://doi.org/10.1038/s41467-019-13575-7.
Tustison NJ, Cook PA, Holbrook AJ, Johnson HJ, Muschelli J, Devenyi GA, Duda JT, Das SR, Cullen NC, Gillen DL, Yassa MA, Stone JR, Gee JC, Avants BB. The ANTsX ecosystem for quantitative biological and medical imaging. Sci Rep. 2021. https://doi.org/10.1038/s41598-021-87564-6.
Martín-González E, Olmedo-Córdoba M, Flores P, Moreno-Montoya M. Differential neurobiological markers in phenotype-stratified rats modeling high or low vulnerability to compulsive behavior: a narrative review. Curr Neuropharmacol. 2023;21(9):1924–33. https://doi.org/10.2174/1570159X21666221121091454.
Moreno-Montoya M, Olmedo-Córdoba M, Martín-González E. Negative valence system as a relevant domain in compulsivity: review in a preclinical model of compulsivity. Emerg Topics Life Sci. 2022;6(5):491–500. https://doi.org/10.1042/ETLS20220005.
Paxinos G, Watson C. The rat brain in stereotaxic coordinates. 6th ed. Amsterdam: Elsevier; 2007.
Straathof M, Blezer ELA, van Heijningen C, Smeele CE, van der Toorn A, Buitelaar J, de Ruiter S, Naaijen J, Akkermans S, Mennes M, Zwiers M, Ilbegi S, Hennissen L, Glennon J, van de Vondervoort I, Kapusta K, Bielczyk NA, Amiri H, Havenith M, Dijkhuizen RM. Structural and functional MRI of altered brain development in a novel adolescent rat model of quinpirole-induced compulsive checking behavior. Eur Neuropsychopharmacol. 2020. https://doi.org/10.1016/j.euroneuro.2020.02.004.
Sharma P, Dedeurwaerdere S, Vandenberg MAD, Fang K, Johnston LA, Shultz SR, O’Brien TJ, Gilby KL. Neuroanatomical differences in FAST and SLOW rat strains with differential vulnerability to kindling and behavioral comorbidities. Epilepsy Behav. 2016. https://doi.org/10.1016/j.yebeh.2016.08.022.
Haar CV, Martens KM, Bashir A, McInnes KA, Cheng WH, Cheung H, Stukas S, Barron C, Ladner T, Welch KA, Cripton PA, Winstanley CA, Wellington CL. Repetitive closed-head impact model of engineered rotational acceleration (CHIMERA) injury in rats increases impulsivity, decreases dopaminergic innervation in the olfactory tubercle and generates white matter inflammation, tau phosphorylation and degener. Exp Neurol. 2019. https://doi.org/10.1016/j.expneurol.2019.02.012.
Golden CEM, Yee Y, Wang VX, Harony-Nicolas H, Hof PR, Lerch JP, Buxbaum JD. Reduced axonal caliber and structural changes in a rat model of Fragile X syndrome with a deletion of a K-Homology domain of Fmr1. Transl Psychiatry. 2020. https://doi.org/10.1038/s41398-020-00943-x.
Chen X, Yue J, Luo Y, Huang L, Li B, Wen S. Distinct behavioral traits and associated brain regions in mouse models for obsessive–compulsive disorder. Behav Brain Funct. 2021. https://doi.org/10.1186/s12993-021-00177-x.
Giona F, Pagano J, Verpelli C, Sala C. Another step toward understanding brain functional connectivity alterations in autism: an Editorial Highlight for “Neurobiological substrates underlying corpus callosum hypoconnectivity and brain metabolic patterns in the valproic acid rat model of autism. J Neurochem. 2021;159(1):12. https://doi.org/10.1111/jnc.15452.
Uccelli NA, Codagnone MG, Traetta ME, Levanovich N, Rosato Siri MV, Urrutia L, Falasco G, Vázquez S, Pasquini JM, Reinés AG. Neurobiological substrates underlying corpus callosum hypoconnectivity and brain metabolic patterns in the valproic acid rat model of autism spectrum disorder. J Neurochem. 2021;159(1):128. https://doi.org/10.1111/jnc.15444.
Wang Y, Zou L, Xie W, Yang Z, Zhu X, Cheung EFC, Sørensen TA, Møller A, Chan RCK. Altered grey matter volume and cortical thickness in patients with schizo-obsessive comorbidity. Psychiatry Res Neuroimaging. 2018. https://doi.org/10.1016/j.pscychresns.2018.03.009.
Radua J, Grau M, Van Den Heuvel OA, De Schotten MT, Stein DJ, Canales-Rodríguez EJ, Catani M, Mataix-Cols D. Multimodal voxel-based meta-analysis of white matter abnormalities in obsessive-compulsive disorder. Neuropsychopharmacology. 2014;39(7):1577. https://doi.org/10.1038/npp.2014.5.
Bigler ED, Abildskov TJ, Petrie JA, Johnson M, Lange N, Chipman J, Lu J, McMahon W, Lainhart JE. Volumetric and voxel-based morphometry findings in autism subjects with and without macrocephaly. Dev Neuropsychol. 2010;35(3):278. https://doi.org/10.1080/87565641003696817.
Courchesne E, Karns CM, Davis HR, Ziccardi R, Carper RA, Tigue ZD, Chisum HJ, Moses P, Pierce K, Lord C, Lincoln AJ, Pizzo S, Schreibman L, Haas RH, Akshoomoff NA, Courchesne RY. Unusual brain growth patterns in early life in patients with autistic disorder: an MRI study. Neurology. 2001;57(2):245. https://doi.org/10.1212/WNL.57.2.245.
Herbert MR, Ziegler DA, Makris N, Filipek PA, Kemper TL, Normandin JJ, Sanders HA, Kennedy DN, Caviness VS. Localization of white matter volume increase in autism and developmental language disorder. Ann Neurol. 2004;55(4):530. https://doi.org/10.1002/ana.20032.
Tadayonnejad R, Pizzagalli F, Murray SB, Pauli WM, Conde G, Bari AA, Strober M, O’Doherty JP, Feusner JD. White matter tracts characteristics in habitual decision-making circuit underlie ritual behaviors in anorexia nervosa. Sci Rep. 2021. https://doi.org/10.1038/s41598-021-95300-3.
Suñol M, Contreras-Rodríguez O, Macià D, Martínez-Vilavella G, Martínez-Zalacaín I, Subirà M, Pujol J, Sunyer J, Soriano-Mas C. Brain structural correlates of subclinical obsessive-compulsive symptoms in healthy children. J Am Acad Child Adolesc Psychiatry. 2018;57(1):41. https://doi.org/10.1016/j.jaac.2017.10.016.
Loomba N, Beckerson ME, Ammons CJ, Maximo JO, Kana RK. Corpus callosum size and homotopic connectivity in Autism spectrum disorder. Psychiatry Res Neuroimaging. 2021. https://doi.org/10.1016/j.pscychresns.2021.111301.
Huyser C, Van Den Heuvel OA, Wolters LH, De Haan E, Boer F, Veltman DJ. Increased orbital frontal gray matter volume after cognitive behavioural therapy in paediatric obsessive compulsive disorder. World J Biol Psychiatry. 2013;14(4):319. https://doi.org/10.3109/15622975.2012.674215.
Raviv N, Staudt MD, Rock AK, MacDonell J, Slyer J, Pilitsis JG. A systematic review of deep brain stimulation targets for obsessive compulsive disorder. Neurosurgery. 2020;87(6):1098. https://doi.org/10.1093/neuros/nyaa249.
Chen J, Silk T, Seal M, Dally K, Vance A. Widespread decreased grey and white matter in paediatric obsessive-compulsive disorder (OCD): a voxel-based morphometric MRI study. Psychiatry Res Neuroimaging. 2013;213(1):11. https://doi.org/10.1016/j.pscychresns.2013.02.003.
Zhou C, Xu J, Ping L, Zhang F, Chen W, Shen Z, Jiang L, Xu X, Cheng Y. Cortical thickness and white matter integrity abnormalities in obsessive–compulsive disorder: a combined multimodal surface-based morphometry and tract-based spatial statistics study. Depress Anxiety. 2018;35(8):742. https://doi.org/10.1002/da.22758.
Temur HO, Yurtsever I, Yesil G, Sharifov R, Yilmaz FT, Dundar TT, Alkan A. Correlation between DTI findings and volume of corpus callosum in children with AUTISM. Curr Med Imaging. 2018;15(9):895. https://doi.org/10.2174/1573405614666181005114315.
Amaya KA, Smith KS. Neurobiology of habit formation. Curr Opin Behav Sci. 2018;20:145. https://doi.org/10.1016/j.cobeha.2018.01.003.
Gourley SL, Taylor JR. Going and stopping: dichotomies in behavioral control by the prefrontal cortex. Nat Neurosci. 2016;19(6):656. https://doi.org/10.1038/nn.4275.
Smith RJ, Laiks LS. Behavioral and neural mechanisms underlying habitual and compulsive drug seeking. Prog Neuro-Psychopharmacol Biol Psychiatry. 2018. https://doi.org/10.1016/j.pnpbp.2017.09.003.
Íbias J, Soria-Molinillo E, Kastanauskaite A, Orgaz C, DeFelipe J, Pellón R, Miguéns M. Schedule-induced polydipsia is associated with increased spine density in dorsolateral striatum neurons. Neuroscience. 2015. https://doi.org/10.1016/j.neuroscience.2015.05.026.
Merchán A, Mora S, Gago B, Rodriguez-Ortega E, Fernández-Teruel A, Puga JL, Sánchez-Santed F, Moreno M, Flores P. Excessive habit formation in schedule-induced polydipsia: Microstructural analysis of licking among rat strains and involvement of the orbitofrontal cortex. Genes Brain Behav. 2019. https://doi.org/10.1111/gbb.12489.
Mora S, Merchán A, Aznar S, Flores P, Moreno M. Increased amygdala and decreased hippocampus volume after schedule-induced polydipsia in high drinker compulsive rats. Behav Brain Res. 2020. https://doi.org/10.1016/j.bbr.2020.112592.
Tapias-Espinosa C, Río-Álamos C, Sánchez-González A, Oliveras I, Sampedro-Viana D, del Mar Castillo-Ruiz M, Cañete T, Tobeña A, Fernández-Teruel A. Schizophrenia-like reduced sensorimotor gating in intact inbred and outbred rats is associated with decreased medial prefrontal cortex activity and volume. Neuropsychopharmacology. 2019;44(11):1975. https://doi.org/10.1038/s41386-019-0392-x.
Kozłowska A, Wojtacha P, Równiak M, Kolenkiewicz M, Huang ACW. ADHD pathogenesis in the immune, endocrine and nervous systems of juvenile and maturating SHR and WKY rats. Psychopharmacology. 2019;236(10):2937. https://doi.org/10.1007/s00213-019-5180-0.
Park SE, Kim BC, Yang JC, Jeong GW. Mri-based multimodal approach to the assessment of clinical symptom severity of obsessive-compulsive disorder. Psychiatry Investig. 2020;17(8):777. https://doi.org/10.30773/pi.2020.0124.
Zarei M, Mataix-Cols D, Heyman I, Hough M, Doherty J, Burge L, Winmill L, Nijhawan S, Matthews PM, James A. Changes in gray matter volume and white matter microstructure in adolescents with obsessive-compulsive disorder. Biol Psychiatry. 2011;70(11):1090. https://doi.org/10.1016/j.biopsych.2011.06.032.
Conti E, Retico A, Palumbo L, Spera G, Bosco P, Biagi L, Fiori S, Tosetti M, Cipriani P, Cioni G, Muratori F, Chilosi A, Calderoni S. Autism spectrum disorder and childhood apraxia of speech: Early language-related hallmarks across structural mri study. J Personal Med. 2020;10(4):275. https://doi.org/10.3390/jpm10040275.
Hollander E, Anagnostou E, Chaplin W, Esposito K, Haznedar MM, Licalzi E, Wasserman S, Soorya L, Buchsbaum M. Striatal volume on magnetic resonance imaging and repetitive behaviors in autism. Biol Psychiatry. 2005;58(3):226. https://doi.org/10.1016/j.biopsych.2005.03.040.
Montigny C, Castellanos-Ryan N, Whelan R, Banaschewski T, Barker GJ, Büche C, Gallinat J, Flor H, Mann K, Paillère-Martinot ML, Nees F, Lathrop M, Loth E, Paus T, Pausova Z, Rietsche M, Schumann G, Smolka MN, Struve M, Conrod PJ. A phenotypic structure and neural correlates of compulsive behaviors in adolescents. PLoS ONE. 2013;8(11):e80151. https://doi.org/10.1371/journal.pone.0080151.
Calderoni S, Bellani M, Hardan AY, Muratori F, Brambilla P. Basal ganglia and restricted and repetitive behaviours in Autism Spectrum Disorders: current status and future perspectives. Epidemiol Psychiatr Sci. 2014;23(3):235. https://doi.org/10.1017/S2045796014000171.
Weng CB, Qian RB, Fu XM, Lin B, Ji XB, Niu CS, Wang YH. A voxel-based morphometric analysis of brain gray matter in online game addicts. Natl Med J China. 2012. https://doi.org/10.3760/cma.j.issn.0376-2491.2012.45.017.
Seo S, Beck A, Matthis C, Genauck A, Banaschewski T, Bokde ALW, Bromberg U, Büchel C, Quinlan EB, Flor H, Frouin V, Garavan H, Gowland P, Ittermann B, Martinot JL, Martinot MLP, Nees F, Orfanos DP, Poustka L, Hohmann S, Fröhner JH, Smolka MN, Walter H, Whelan R, Desrivières S, Heinz A, Schumann G, Obermayer K. Risk profiles for heavy drinking in adolescence: differential effects of gender. Addict Biol. 2019;24(4):787. https://doi.org/10.1111/adb.12636.
Hoexter MQ, Dougherty DD, Shavitt RG, D’Alcante CC, Duran FLS, Lopes AC, Diniz JB, Batistuzzo MC, Evans KC, Bressan RA, Busatto GF, Miguel EC. Differential prefrontal gray matter correlates of treatment response to fluoxetine or cognitive-behavioral therapy in obsessive-compulsive disorder. Eur Neuropsychopharmacol. 2013;23(7):569. https://doi.org/10.1016/j.euroneuro.2012.06.014.
Fineberg NA, Apergis-Schoute AM, Vaghi MM, Banca P, Gillan CM, Voon V, Chamberlain SR, Cinosi E, Reid J, Shahper S, Bullmore ET, Sahakian BJ, Robbins TW. Mapping compulsivity in the DSM-5 obsessive compulsive and related disorders: cognitive domains, neural circuitry, and treatment. Int J Neuropsychopharmacol. 2018;21(1):42. https://doi.org/10.1093/ijnp/pyx088.
Whelan R, Conrod PJ, Poline JB, Lourdusamy A, Banaschewski T, Barker GJ, Bellgrove MA, Büchel C, Byrne M, Cummins TDR, Fauth-Bühler M, Flor H, Gallinat J, Heinz A, Ittermann B, Mann K, Martinot JL, Lalor EC, Lathrop M, Loth E, Nees F, Paus T, Rietschel M, Smolka MN, Spanagel R, Stephens DN, Struve M, Thyreau B, Robbins TW, Vollstaedt-Klein S, Schumann G, Garavan H. Adolescent impulsivity phenotypes characterized by distinct brain networks. Nat Neurosci. 2012;15(6):920. https://doi.org/10.1038/nn.3092.
Rothwell PE, Hayton SJ, Sun GL, Fuccillo MV, Lim BK, Malenka RC. Input- and output-specific regulation of serial order performance by corticostriatal circuits. Neuron. 2015;88(2):345. https://doi.org/10.1016/j.neuron.2015.09.035.
Lüscher C, Robbins TW, Everitt BJ. The transition to compulsion in addiction. Nat Rev Neurosci. 2020;21(5):247. https://doi.org/10.1038/s41583-020-0289-z.
Klavir O, Flash S, Winter C, Joel D. High frequency stimulation and pharmacological inactivation of the subthalamic nucleus reduces “compulsive” lever-pressing in rats. Exp Neurol. 2009;215(1):101. https://doi.org/10.1016/j.expneurol.2008.09.017.
Winter C, Mundt A, Jalali R, Joel D, Harnack D, Morgenstern R, Juckel G, Kupsch A. High frequency stimulation and temporary inactivation of the subthalamic nucleus reduce quinpirole-induced compulsive checking behavior in rats. Exp Neurol. 2008;210(1):217. https://doi.org/10.1016/j.expneurol.2007.10.020.
Wade CL, Kallupi M, Hernandez DO, Breysse E, Guglielmo G, Crawford E, Koob GF, Schweitzer P, Baunez C, George O. High-frequency stimulation of the subthalamic nucleus blocks compulsive-like re-escalation of heroin taking in rats. Neuropsychopharmacology. 2017;42(9):1850. https://doi.org/10.1038/npp.2016.270.
Adams WK, Haar CV, Tremblay M, Cocker PJ, Silveira MM, Kaur S, Baunez C, Winstanley CA. Deep-brain stimulation of the subthalamic nucleus selectively decreases risky choice in risk-preferring rats. ENeuro. 2017. https://doi.org/10.1523/ENEURO.0094-17.2017.
Kapor S, Aksić M, Puškaš L, Jukić M, Poleksić J, Milosavljević F, Bjelica S, Filipović B. Long-term effects of maternal deprivation on the volume of dopaminergic nuclei and number of dopaminergic neurons in substantia nigra and ventral tegmental area in rats. Front Neuroanat. 2020. https://doi.org/10.3389/fnana.2020.578900.
Cannella N, Cosa-Linan A, Büchler E, Falfan-Melgoza C, Weber-Fahr W, Spanagel R. In vivo structural imaging in rats reveals neuroanatomical correlates of behavioral sub-dimensions of cocaine addiction. Addicti Biol. 2018;23(1):182. https://doi.org/10.1111/adb.12500.
Yücel M, Harrison BJ, Wood SJ, Fornito A, Wellard RM, Pujol J, Clarke K, Phillips ML, Kyrios M, Velakoulis D, Pantelis C. Functional and biochemical alterations of the medial frontal cortex in obsessive-compulsive disorder. Arch General Psychiatry. 2007;64(8):946. https://doi.org/10.1001/archpsyc.64.8.946.
Huggins AA, Harvey AM, Miskovich TA, Lee HJ, Larson CL. Resting-state functional connectivity of supplementary motor area associated with skin-picking symptom severity. J Obsess Compuls Related Disord. 2020. https://doi.org/10.1016/j.jocrd.2020.100551.
Staudt MD, Pouratian N, Miller JP, Hamani C, Raviv N, McKhann GM, Gonzalez-Martinez JA, Pilitsis JG. Congress of neurological surgeons systematic review and evidence-based guidelines for deep brain stimulations for obsessive-compulsive disorder: update of the 2014 guidelines. Neurosurgery. 2021;88(4):710. https://doi.org/10.1093/neuros/nyaa596.
Gilbert AR, Mataix-Cols D, Almeida JRC, Lawrence N, Nutche J, Diwadkar V, Keshavan MS, Phillips ML. Brain structure and symptom dimension relationships in obsessive-compulsive disorder: a voxel-based morphometry study. J Affect Disord. 2008;109(1–2):117. https://doi.org/10.1016/j.jad.2007.12.223.
Devenport LD. Schedule-induced polydipsia in rats: Adrenocortical and hippocampal modulation. J Comp Physiol Psychol. 1978;92(4):651. https://doi.org/10.1037/h0077499.
Chiba S, Okawara T, Kawakami K, Ohta R, Kawaguchi M. Alterations between high and low-avoidance lines of Hatano rats in learning behaviors, ultrasonic vocalizations, and histological characteristics in hippocampus and amygdala. Physiol Behav. 2022. https://doi.org/10.1016/j.physbeh.2021.113670.
Yoon EJ, Choi JS, Kim H, Sohn BK, Jung HY, Lee JY, Kim DJ, Park SW, Kim YK. Altered hippocampal volume and functional connectivity in males with Internet gaming disorder comparing to those with alcohol use disorder. Sci Rep. 2017. https://doi.org/10.1038/s41598-017-06057-7.
Kobayashi T, Hirano Y, Nemoto K, Sutoh C, Ishikawa K, Miyata H, Matsumoto J, Matsumoto K, Masuda Y, Nakazato M, Shimizu E, Nakagawa A. Correlation between morphologic changes and autism spectrum tendency in obsessive-compulsive disorder. Magn Reson Med Sci. 2015;14(4):329. https://doi.org/10.2463/mrms.2014-0146.
Zhang L, Hu X, Li H, Lu L, Li B, Hu X, Bu X, Tang S, Tang W, Liu N, Yang Y, Gong Q, Huang X. Characteristic alteration of subcortical nuclei shape in medication-free patients with obsessive-compulsive disorder. NeuroImage Clin. 2019;24:102040. https://doi.org/10.1016/j.nicl.2019.102040.
Payne M, Mali I, McKinnell ZE, Vangsness L, Shrestha TB, Bossmann SH, Plakke B. Increased volumes of lobule VI in a valproic acid model of autism are associated with worse set-shifting performance in male Long-Evan rats. Brain Res. 2021. https://doi.org/10.1016/j.brainres.2021.147495.
Vazquez-Sanroman D, Carbo-Gas M, Leto K, Cerezo-Garcia M, Gil-Miravet I, Sanchis-Segura C, Carulli D, Rossi F, Miquel M. Cocaine-induced plasticity in the cerebellum of sensitised mice. Psychopharmacology. 2015;232(24):4455. https://doi.org/10.1007/s00213-015-4072-1.
Wilkes BJ, Bass C, Korah H, Febo M, Lewis MH. Volumetric magnetic resonance and diffusion tensor imaging of C58/J mice: neural correlates of repetitive behavior. Brain Imaging Behav. 2020;14(6):2084. https://doi.org/10.1007/s11682-019-00158-9.
Cauda F, Geda E, Sacco K, D’Agata F, Duca S, Geminiani G, Keller R. Grey matter abnormality in autism spectrum disorder: an activation likelihood estimation meta-analysis study. J Neurol Neurosurg Psychiatry. 2011;82(12):1304. https://doi.org/10.1136/jnnp.2010.239111.
Sparks BF, Friedman SD, Shaw DW, Aylward EH, Echelard D, Artru AA, Maravilla KR, Giedd JN, Munson J, Dawson G, Dager SR. Brain structural abnormalities in young children with autism spectrum disorder. Neurology. 2002;59(2):184. https://doi.org/10.1212/WNL.59.2.184.
Hu X, Du M, Chen L, Li L, Zhou M, Zhang L, Liu Q, Lu L, Mreedha K, Huang X, Gong Q. Meta-analytic investigations of common and distinct grey matter alterations in youths and adults with obsessive-compulsive disorder. Neurosci Biobehav Rev. 2017;78:91. https://doi.org/10.1016/j.neubiorev.2017.04.012.
Pujol J, Soriano-Mas C, Alonso P, Cardoner N, Menchón JM, Deus J, Vallejo J. Mapping structural brain alterations in obsessive-compulsive disorder. Arch General Psychiatry. 2004;61(7):720. https://doi.org/10.1001/archpsyc.61.7.720.
Tang W, Zhu Q, Gong X, Zhu C, Wang Y, Chen S. Cortico-striato-thalamo-cortical circuit abnormalities in obsessive-compulsive disorder: a voxel-based morphometric and fMRI study of the whole brain. Behav Brain Res. 2016. https://doi.org/10.1016/j.bbr.2016.07.004.
Tsai CJ, Lin HY, Tseng IWY, Gau SSF. Brain voxel-based morphometry correlates of emotion dysregulation in attention-deficit hyperactivity disorder. Brain Imaging Behav. 2021;15(3):1388. https://doi.org/10.1007/s11682-020-00338-y.
Abramovitch A, Abramowitz JS, Mittelman A. The neuropsychology of adult obsessive-compulsive disorder: a meta-analysis. Clin Psychol Rev. 2013;33(8):1163. https://doi.org/10.1016/j.cpr.2013.09.004.
Draganski B, Gaser C, Busch V, Schuierer G, Bogdahn U, May A. Neuroplasticity: changes in grey matter induced by training. Nature. 2004;427(6972):311.
Taubert M, Villringer A, Ragert P. Learning-related gray and white matter changes in humans: an update. Neuroscientist. 2012;18(4):320. https://doi.org/10.1177/1073858411419048.
Woollett K, Maguire EA. Acquiring “the knowledge” of London’s layout drives structural brain changes. Curr Biol. 2011;21(24):2109. https://doi.org/10.1016/j.cub.2011.11.018.
Funding
This work was supported by the following funding sources: PID2022-139286NB-I00 Proyectos de Generación de Conocimiento, Gobierno de España; PND-2022l024 Plan Nacional sobre Drogas, MISAN, Gobierno de España; and UAL2020-CTSD2068 with FEDER I+D+I funds “Una manera de hacer Europa”.
Author information
Authors and Affiliations
Contributions
All the authors contributed substantially to the manuscript. EM-G: Methodology, Investigation, data analysis, writing—original draft preparation. AP-P: Investigation, writing−review and editing. SS, DP, PR-C: methodology, review and editing. JD: Methodology, writing-review and editing, resources, supervision, project administration, funding acquisition. SM: Investigation, Writing—review and editing, Supervision. MM: Conceptualization, methodology, writing—review and editing, resources, supervision, project administration, funding acquisition. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were conducted in accordance with the Spanish Royal Decree 53/2013 and the European Community Directive (2010/63/EU) for animal research. The present study was also approved by the Animal Research Committee from the University of Almería and complied with the ARRIVE guidelines. The authors declare that the research shows commitment to the 3Rs principle (replacement, reduction, refinement). Throughout the entire experiment, adequate measures were taken to minimize pain, or discomfort for the experimental animals.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Information.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Martín-González, E., Prados-Pardo, Á., Sawiak, S.J. et al. Mapping the neuroanatomical abnormalities in a phenotype of male compulsive rats. Behav Brain Funct 19, 19 (2023). https://doi.org/10.1186/s12993-023-00221-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12993-023-00221-y