Abstract
Hydrocephalus (HC) is a heterogenous disease characterized by alterations in cerebrospinal fluid (CSF) dynamics that may cause increased intracranial pressure. HC is a component of a wide array of genetic syndromes as well as a secondary consequence of brain injury (intraventricular hemorrhage (IVH), infection, etc.) that can present across the age spectrum, highlighting the phenotypic heterogeneity of the disease. Surgical treatments include ventricular shunting and endoscopic third ventriculostomy with or without choroid plexus cauterization, both of which are prone to failure, and no effective pharmacologic treatments for HC have been developed. Thus, there is an urgent need to understand the genetic architecture and molecular pathogenesis of HC. Without this knowledge, the development of preventive, diagnostic, and therapeutic measures is impeded. However, the genetics of HC is extraordinarily complex, based on studies of varying size, scope, and rigor. This review serves to provide a comprehensive overview of genes, pathways, mechanisms, and global impact of genetics contributing to all etiologies of HC in humans.
Similar content being viewed by others
Introduction
Hydrocephalus (HC) is characterized by aberrant cerebrospinal fluid (CSF) dynamics (with or without ventricular dilation) that can lead to increased intracranial pressure. When left untreated, HC may be fatal and cause severe impairment in neurodevelopment. While classical theories of CSF posited that CSF is produced predominantly in the lateral ventricles via the choroid plexus and flows through the foramina of Monroe, third ventricle, cerebral aqueduct, and the fourth ventricle where it is disseminated through the central canal of the spinal cord and the subarachnoid space to be reabsorbed by arachnoid granulations [1], this model is no longer considered dogmatic [2]. Anatomical disruption of CSF flow and/or CSF pulsatility may result in a buildup of CSF to be classified as obstructive or non-communicating HC. However, HC can be communicating (i.e., no obvious anatomical blockade of absorption or obstruction), the result from increased production of CSF in response to injury, impaired absorption from the subarachnoid space, or result from defects in cortical development. These insults, in turn, may lead to ventricular dilation, among other potential and highly debated pathophysiologic mechanisms. Importantly, the global burden of HC is high [3], with significant morbidity and mortality regardless of treatment [4]. However, the genetic and mechanistic basis of HC remains poorly understood, largely due to the genetic complexity and phenotypic heterogeneity of the disease as well as cost of large-scale human genetics studies.
HC is a component of a wide-array of genetic syndromes [5], a secondary consequence of brain injury (intraventricular hemorrhage (IVH), infection, etc.) [6, 7], and a component of many central nervous system congenital abnormalities (i.e., neural tube defects, Chiari malformation, etc.) with a number of comorbid phenotypes including epilepsy and autism, among others. HC is a highly polygenic disease [8,9,10], with genes of varying functions and mechanisms conferring risk to the disease. The current treatments for HC are surgical interventions such as insertion of a ventricular (-peritoneal, atrial, etc.) shunt or endoscopic third ventriculostomy (ETV), which may be combined with choroid plexus cauterization (CPC) [6, 11]. While many studies have evaluated the efficacy and cost of these procedures [12], long-term morbidity of HC remains high and both treatments are prone to failure [13, 14]. Furthermore, while clinical trials have attempted pharmacological strategies to treat HC [15], no pharmacological treatment has been successful. In addition, HC may present in adulthood as normal pressure hydrocephalus (NPH). A more sophisticated and detailed understanding the genetic architecture and molecular pathogenesis of HC may lead to development of targeted pharmacologic treatments.
While numerous studies have aimed to identify causative genetic mechanisms leading to HC, largely based on isolated human case studies and murine models [5], critical limitations include cost, patient/family recruitment, number of patients (small by population-genetics’ standards), individual variant validation (typically de novo mutations), and very important species differences between model-organisms and human disease. Proposed pathophysiological mechanisms of HC include impaired development of the neural stem cell niche [16,17,18,19,20], abnormal ciliated ependymal cells [21,22,23], disruption of the ventricular zone [24, 25], and primary alterations in CSF absorption and/or secretion [26,27,28,29]. However, our understanding of these mechanisms is derived from varied model systems, which do not always accurately recapitulate the genetic and pathophysiological basis of human HC. Furthermore, there is increasing evidence that germline genetic variation contributes to risk of HC [5, 8, 10, 30]; however, most cases of HC remain genetically undefined and clinical genetic testing is rarely performed.
Elucidation of the genetic architecture of both shared and etiology-specific forms of HC may uncover pathophysiological mechanisms and correlate genetic risk factors with clinical and surgical outcomes, with the potential to directly influence surgical counseling and clinical management. While many genes have been implicated in the pathogenesis of HC in humans, the study designs, approaches, and levels of evidence identifying and validating these genetic findings vary greatly. Uncovering the genetic basis of HC relies on many factors, but most importantly on the clinical phenotype in question because HC rarely occurs in isolation. Comorbid phenotypes (neural tube defects, primary structural brain disorders, epilepsy, cognitive delay, etc.), and antecedent injuries – IVH and/or infection (meningitis, intracranial abscess, and/or sepsis), alone and in concert, confound most classical approaches to understanding genetic disease. Advancing our understanding of HC genetics, therefore, will necessitate understanding the extent to which co-occurring phenotypes are present and integration of multiple molecular and genetic data. Furthermore, elucidation of human-specific molecular mechanisms necessitates study in human tissue representative of the diverse populations HC affects. Here we summarize genetic studies of HC in humans and offer suggestions for advancing the field forward.
Methods
Search criteria
The US National Library of Medicine PubMed database and the Online Mendelian Inheritance in Man (OMIM) were queried for English-language studies using Title/Abstract, MeSH headings, key words, and genetic descriptors relevant to genetic causes of HC and ventriculomegaly. The OMIM database was used as an additional adjunct database as well. Our search terms are included below. Duplicates identified across multiple databases were identified. We strictly adhered to PRISMA guidelines [31].
Our PubMed search syntax included the following: (HC[Title/Abstract]) OR (Ventriculomegaly[Title/Abstract]); ((HC[MeSH Major Topic]) OR (Ventriculomegaly[MeSH Major Topic])) AND ("mendelian" OR "de novo" OR "functional genomics" OR "whole exome sequencing" OR "whole-genome sequencing" OR "genotyping" OR "genotype" OR "microarray" OR "genome-wide association study" OR "genome wide association study" OR "GWAS" OR "transcriptome wide association study" OR "transcriptome-wide association study" OR "TWAS" OR "gene expression" OR "copy number variation" OR "insertion" OR "deletion" OR "mosaic" OR "mosaicism" OR "genetic variation" OR "consanguineous" OR "consanguinity" OR "autosomal recessive" OR "autosomal dominant" OR "x-linked recessive" OR "x-linked dominant" OR "inherited" OR "inheritance" OR "non-coding" OR "coding" OR "co-expression" OR "germline" OR "linkage" OR "linkage disequilibrium" OR "genetic counseling" OR "syndrome" OR "syndromic" OR "genetic testing" OR "aqueductal stenosis" OR "obstructive HC" OR "acquired HC" OR "congenital HC" OR "proteomics" OR "proteomic" OR "metabolomic" OR "metabolomics" OR "methylation" OR "mutation" OR "genetic deficiency" OR "gain of function" OR "gain-of-function" OR "loss of function" OR "loss-of-function" OR "molecular"[Title/Abstract]).
We next queried the Online Mendelian Inheritance in Man (OMIM) database [32] using the search terms: “HC” or “ventriculomegaly” to identify genetic disease of which HC is a component. The search returned 671 entries which were manually reviewed. Duplicates within the OMIM database were excluded (n = 95). The resulting search query resulted in 3,709 studies.
Inclusion and exclusion criteria
Records (n = 3,709) from the above search were initially evaluated via abstract and screened for exclusion criteria: (1) Records published before 1970; (2) no genetic data of any kind; (3) no HC diagnosis; or (4) animal subjects. A total of 2,652 studies were excluded. Full text screening of the remaining papers (n = 1,057) was then screened for inclusion criteria. The second round of screening was carried out by full text review (n = 1,057). The same exclusion criteria were applied, while inclusion criteria were implemented: (1) Records published after 1970; (2) pediatric cohort (0–18 years of age); (3) primary genetic analysis; (4) confirmed diagnosis of human HC; and (5) human subjects. The final records were assessed for eligibility and records unavailable in English were excluded (n = 2). The final studies included (n = 327) were then evaluated for the methodology and type of genetic analysis performed. The papers included in our study (n = 327) were then subject to secondary analyses to assess for (1) change in number of publications over time; (2) geographic and ethnic associations of HC; (3) size of study; (4) central nervous system and non-central nervous system phenotypic associations. Figures were created using BioRender.
Author affiliation and subject country of origin
Authors’ institutional affiliation was obtained via PubMed’s “Affiliations” tab within the respective research articles PubMed webpage. Authors were then cross-referenced via Google search to increase validity of institutional affiliation at the time the study was performed. Articles were individually queried for the country of origin of patients with HC. If not explicitly stated, it was assumed that the patients were from the same country as the senior author’s affiliation. The total number of cases were tallied and tabulated on a world map using OpenStreetMap.
Results
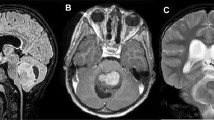
HC in humans can be caused by or is secondary to several factors including structural brain disorders, cilia abnormalities, brain tumors resulting in CSF obstruction requiring CSF diversion, neural tube defects, prematurity and germinal matrix fragility, neonatal systemic and CNS infections, intracranial hemorrhage, evolutionary selection pressures, and ‘genetic’ anomalies, classically thought as Mendelian disorders (Fig. 1). Thus, we conducted a systematic review of human genetic studies of HC to quantify and summarize the current state of genetic contributions to HC of various etiologies (Fig. 2). However, genetic susceptibility confers risk to all these preceding factors as well as to HC directly. Thus, understanding the pleiotropic effect of genes on both risk factors and development of HC is needed and requires highly detailed phenomics analysis [33]. Here, we summarize all genetic studies of human HC across the age spectrum, including discussion of animal models of HC only as corroborating findings of genes and pathways identified in humans where there is a reasonable degree of evolutionary conservation. We believe this is essential as regulation of CSF and brain development is highly divergent across evolution, necessitating clarification and specificity of how genetics plays a role in human disease. Categories are defined a priori based on either phenotypic, molecular, or known genetic classifications. While many forms of HC can reasonably be classified into multiple categories, we attempt to simplify the groupings below.
Hydrocephalus secondary to aqueductal stenosis (AS)
Human genetics studies of HC secondary to aqueductal stenosis (AS) are summarized in Table 1. Fifteen unique gene mutations on 11 chromosomes inherited in both X-linked and autosomal patterns underlying HC secondary to AS have been identified. These genes include protocadherin 9 (PCDH9), immunoglobulin superfamily containing leucine rich repeat 2 (ISLR2), ATPase Na + /K + transporting subunit alpha 3 (ATP1A3), L1 cell adhesion molecule (L1CAM), FA complementation group C (FAC), fibroblast growth factor receptor 3 (FGFR3), solute carrier family 12 member 6 (SLC12A6), crumbs cell polarity complex component 2 (CRB2), Bardet-Biedl syndrome 7 (BBS7), podocin gene (NPHS2), multiple PDZ domain crumbs cell polarity complex component (MPDZ), laminin subunit beta 1 (LAMB1), alpha glucosidase (GAA), A-Disintegrin and Metalloproteinase with Thrombospondin motifs like 2 (ADAMTSL2), collagen type IV alpha 2 chain (COL4A2). A duplication in the Xp22.33 region and deletions of the long arm of chromosome 9, 12q22-q23.1, mutation in SRY-box transcription factor 2 (SOX2) gene, and mutation in the solute carrier family 12-member 7 (SLC12A7) gene were also identified.
Understanding the function of these genes may confer a mechanistic and phenotypic understanding of HC secondary to AS. For example, some patients with AS will display abnormal brainstem development leading to near complete obliteration of the aqueduct, whereas other children may display relatively normal anatomy associated with a web obscuring CSF flow. Genetics factors contributing to AS include ATP1A3, which encodes an ATPase ion channel that has been associated with CNS development and ventricular dilatation when disrupted in zebrafish [34]. In addition, SLC12A6 codes for the ion transporter KCC3 (K-Cl co transporter) that has been associated with AS among other phenotypes including peripheral neuropathy and agenesis of the corpus callosum in mice [35]. These ion channels are localized to the choroid plexus and are involved in neural stem cell development [36]. ADAMTSL2, encoding a glycoprotein, has been shown to interact with fibrillin 1 to enhance transforming growth factor- β (TGFβ) and fibroblast function. Additionally, TGFβ has been implicated in skeletal dysplasia and developmental dysfunction [37]. Thus, it is evident that genes with varying functions may contribute to AS and the diverse co-occurring phenotypes observed in these patients.
X-linked hydrocephalus
Genes contributing to X-linked HC include apoptosis inducing factor mitochondria associated 1 (AIFM1), adaptor related protein complex 1 subunit sigma 2 (AP1S2), EBP cholestenol delta-isomerase (EBP), FA complementation group B (FANCB), histone deacetylase 6 (HDAC6), OFD1 centriole and centriolar satellite protein (OFD1), OTU deubiquitinase 5 (OTUD5), coiled-coil domain containing 22 (CCDC22), and porcupine O-acyltransferase (PORCN). Table 2 summarizes the genetic studies of X-linked HC in humans. AIFM1 is involved in regulation of apoptosis [38]. In addition, AP1S2 regulates endosomal protein trafficking and structural integrity [39]. HDAC6 has been shown to interact with Runx2, a transcription factor involved in osteoblast differentiation, and other HDACs exhibit high expression patterns in prehypertrophic chondrocytes, indicating their role in endochondral ossification and skeletal dysplasias [40]. OTUD5 mutations also impact transcriptional regulation with its inability to prevent HDAC degradation and maintain neural stem cell development [41]. OFD1 and PORCN mutations affect signaling pathways such as hedgehog signaling or wingless/integrated (Wnt) signaling [42, 43].
L1CAM associated hydrocephalus
Next, we discuss L1CAM associated HC, as this entity is well described and distinct phenotypically. Early linkage analysis studies of HC identified a mutation within the long arm of chromosome X, specifically Xq28. Further genomic analyses localized to a region between the gene loci of DXS52 and F8C, within which L1 cell adhesion molecule (L1CAM) resides. The genetic understanding of X-linked HC has primarily been linked to genetic alterations at the L1CAM locus. L1CAM duplications include the 3’ end of the open reading frame and exons 2–10. L1CAM insertions include exon 18 and the junction sequence between L1CAM and AVPR2. L1CAM deletions/microdeletions include exons 2, 5–8, 10, 11, 18, 19, 21–23, 26, intron 18, and whole gene deletion. L1CAM missense mutations include exons 1–16, 18, 20, 21, 24, 27, 28 and introns 2–4, 6–8, 10–15, 18, 21, 22, 24, and 26. L1CAM nonsense mutations include exons 1, 3, 8, 10–14, and 20–22. A silent mutation in Exon 8 of L1CAM has been associated with HC. A summary of all mutations across L1CAM can be found in Fig. 3 and Table 3. Mutations in L1CAM are also associated with MASA syndrome (characterized by mental retardation, aphasia, shuffling gait, and adducted thumb), and spastic paraplegia, highlighting the pleiotropic role of L1CAM in human disease.
Dandy walker malformation
Dandy Walker malformation is a cerebellar structural anomaly that can impede CSF flow but can also be related to primary brain developmental alterations and contribute to HC development. Missense mutations are found in forkhead box C1 (FOXC1), fukutin (FKTN), laminin subunit gamma 1 (LAMC1), sphingosine-1-phosphate phosphatase 2 (SGPP2), and exocyst complex component 3 like 2 (EXOC3L2). Nonsense mutations are found in FKTN, nidogen 1 (NID1), and potassium channel tetramerization domain containing 3 (KCTD3). SIL1 nucleotide exchange factor (SIL1) displayed a nonstop mutation and carnitine palmitoyltransferase 2 (CPT2) displayed a deletion-insertion variant. Additional mutations included Zic family member 2 (ZIC2) and Zic family member 5 (ZIC5). Deletions were found in lysine methyltransferase 2D (KMT2D), chromosome 2 (2q36.1), chromosome 3 (3q25.1), chromosome 6 (6p24.1, 6p25.3), chromosome 7 (7p21.3), chromosome 8 (8q21), chromosome 12 (12q24), chromosome 13 (13q32), and chromosome 16 (16q21). The deletion of 8p21 resulted in the downregulation of fibroblast growth factor 17 (FGF17). Duplications were found in chromosome 6 (6p25.3), chromosome 7 (7p21.3), and chromosome 12 (12q24). In addition, EXOC3L2 regulates vesicular trafficking at synapses and cell polarity; a mutation within this gene locus can impact normal brain development [44]. KCTD3 is also highly expressed in the brain and kidneys and regulates ion channels such as hyperpolarization activated cyclic nucleotide-gated channel 3 (HCN3) [45]. SIL1 is a glycoprotein that regulates protein trafficking into the ER and ATPase activity, suggesting a mutated implication in protein folding through development [46, 47]. A patient with a mutation in CPT2, an enzyme responsible for breaking down long chain fatty acids, suggests a role of metabolic enzymes in the genetic susceptibility of HC secondary to Dandy Walker malformation [48]. Thus, Dandy Walker malformation related HC may be caused by a wide variety of genes involved in many biological processes. These data are summarized in Table 4.
Ciliopathy
Genes involved in cilia function that are associated with HC are summarized in Table 5. Primary cilia dysfunction has been demonstrated to play a role in HC with numerous Mendelian ‘ciliopathies’ resulting in HC. Missense mutations were observed in Meckel-Gruber syndrome gene (MKS3), MKS transition zone complex subunit 1 (MKS1), intraflagellar transport 43 (IFT43), WD repeat domain 35 (IFT121), coiled-coil and C2 domain containing 2A (CC2D2A), transmembrane protein 216 (TMEM216), PKHD1 ciliary IPT domain containing fibrocystin/polyductin (PKHD1), intestinal cell kinase (ICK), exon 14 of KIAA0586, exons 4 and 13 of centrosomal protein 83 (CEP83), exons 6, 11, 12, 20, 23, 24, 28, 29, 32, and 36 of SET binding factor 2 (SBF2), exon 9 of zinc finger E-box binding homeobox 1 (ZEB1), and exon 5 of G protein subunit alpha i2 (GNAI2). Nonsense mutations were identified in CC2D2A, IFT121, forkhead box J1 (FOXJ1), exon 2 of KIAA0586, exon 3 of centrosomal protein 55 (CEP55), exons 3, 4, 7, and 13 of CEP83, and exon 11 of SBF2. Deletions and duplications resulting in frameshift mutations were found in CC2D2A, MKS3, MKS1, dynein axonemal intermediate chain 2 (DNAI2), IFT121, FOXJ1, exon 5 and 17 of CEP83, and exon 4 of ZEB1. Exon 2 was deleted in WD repeat-containing protein 16 (WDR16). Additional mutations were found in WD repeat domain 93 (WDR93). Loss of MKS3 and MKS1 are associated with ciliary shortening and dysfunction, suggesting a role in primary ciliary development. TMEM216 also contributes to ciliary development through apical polarization and formation and may result in Joubert, Meckel and related syndromes [49]. IFT43 and IFT121 maintain cilium organization and regulate intraflagellar transport in interaction with the IFT-A complex [50]. In addition, CEP83 also interacts with IFT proteins and guides vesicular docking ciliogenesis [51]. One patient was identified with a mutation in DNAI2, a component of the outer dynein arm complex (ODA), which is involved in cilia motility [52]. ZEB1, SBF2, and GNAI2 are involved in other signaling pathways previously identified in association with HC [53].
PI3K-Akt-mTOR
Genes involved in PI3K-Akt-mTOR cell signaling pathway underlying HC are summarized in Table 6. Missense mutations were identified in ring finger protein 125 (RNF125), HECT and RLD domain containing E3 ubiquitin protein ligase family member 1 (HERC1), AKT serine/threonine kinase 3 (AKT3), mechanistic target of rapamycin kinase (mTOR), phosphatase and tensin homolog (PTEN), cyclin D2 (CCND2), phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA) (exon 18 and others), phosphoinositide-3-kinase regulatory subunit 2 (PIK3R2) (exon 13 and others), and platelet derived growth factor receptor beta (PDGFRB) (exon 12 and others). Deletions were observed in PIK3CA, and nonsense mutations were seen in PTEN [54]. Deletions in chromosome 1 (1q42.3-q44) resulted in the deletion of AKT serine/threonine kinase 3 (AKT3). Additional genetic mutations implicated in this pathway included those in tripartite motif containing 71 (TRIM71), SWI/SNF related matrix associated, actin dependent regulator of chromatin (SMARCC1), forkhead box J1 (FOXJ1), formin 2 (FMN2), patched 1 (PTCH1), and FXYD domain containing ion transport regulator 2 (FXYD2). Multiple genes within the PI3K-AKT-MTOR pathway highlight convergence on molecular mechanisms conferring risk to HC. Murine models have demonstrated the role of HERC1, which codes for an E3 ubiquitin ligase, to affect Purkinje cell physiology and mTOR activity [55]. TRIM71 and SMARCC1 are expressed within the ventricles and epithelium of mice brains (determined via in situ hybridization) suggesting that a mutation within this gene locus can affect this region may lead to HC [8]. Mutations in FOXJ1 and FMN2 have been shown to alter neuroepithelial integrity and lead to HC in mice [56, 57]. Mice harboring mutations in PTCH1 also display defects in ependymal cell integrity [58]. Thus, mutations within many genes converging on PI3K-Akt-mTOR signaling have been widely implicated in HC pathophysiology.
Vesicle regulation & cell adhesion
Table 7 details mutations in genes responsible for vesicle regulation and cell adhesion that contribute to the development of HC. Missense mutations were found in and glial fibrillary acidic protein (GFAP). Sorting nexin 10 (SNX10) displayed a nonsense mutation and clathrin heavy chain (CLTC) displayed a frameshift mutation. Additional mutations include ArfGAP with FG repeats 1 (RAB), multiple PDZ domain crumbs cell polarity complex component (MPDZ), beta 1,3-glucosyltransferase (B3GALTL), SEC24 homolog D, COPII coat complex component (SEC24D), and actin beta (ACTB).
GFAP is required for white-matter architectural development and myelination, perhaps accounting for the neurodevelopmental comorbidities frequently observed in patients with HC [59]. Mutations in the phosphoinositide binding domain of SNX10 alters endosomal integrity, suggesting a potential pathogenic mechanism in vesicular trafficking [60]. Additionally, mutations in this gene locus can disrupt interactions between sorting nexins and the V-ATPase complex further contributing to vesicle dysfunction and ciliopathy [61]. CLTC contributes to the development of the vesicular coat, and a mutation within this gene locus may disrupt vesicle stability [62]. Mutations in RAB27A are associated with Griscelli syndrome, characterized by albinism, hematological abnormalities, and organ malformation which can also present with HC [63]. SEC24 is also involved in intracellular trafficking by interacting with export signals from the endoplasmic reticulum and regulating cargo transport [64]. In addition, MPDZ is highly expressed in tight junctions suggesting that a mutation within this gene locus may disrupt alter tissue permeability [65]. Finally, B3GALTL interacts with the thrombospondin type 1 repeat (TSR) protein family which play varied roles in maintain and regulating cell–cell adhesion [66].
Glycosylation defects
Table 8 summarizes genes implicated in human HC associated with defects in glycosylation. Nonsense mutations were seen in protein O-mannose kinase (POMK), and protein O-mannosyltransferase 1 (POMT1). Loss of function mutations were identified in dystroglycan 1 (DAG1) and isoprenoid synthase domain containing gene (ISPD). Additional mutations included those in protein C, inactivator of coagulation factors Va and VIIIa (PROC), fukutin related protein (FKRP), protein O-mannosyltransferase 2 (POMT2), protein O-linked mannose N-acetylglucosaminyltransferase 1 (beta 1,2-) (POMGNT1), LARGE xylosyl and glucuronyltransferase 1 (LARGE1) and a translocation between chromosome 5 and 6, t(5;6) (q35;q21). In addition, DAG1 codes for dystroglycan, a protein involved in extracellular matrix integrity and the genetic etiology of many neurological syndromes. Mutations in DAG1 have been found to contribute to Walker-Warburg syndrome and other muscular dystrophy-dystroglycanopathies which can be associated with HC [67]. Dystroglycan may also be affected through defects in its glycosylation patterns. For instance, mutations in POMK have been shown to impair the glycosylation of a-dystroglycan affecting cytoskeleton stability [68]. Other genes contributing to dystroglycanopathies through glycosylation errors include POMT1, POMT2, POMGNT1, FKRP, ISPD and LARGE1 [69].
Growth factor related signaling
Table 9 summarizes genetic mutations associated with growth factor related signaling dysfunction. Mutations were observed in fibroblast growth factor receptor 1 (FGFR1), fibroblast growth factor receptor 2 (FGFR2), fibroblast growth factor receptor 3 (FGFR3), ZPR1 zinc finger (ZPR1), and fibrillin 1 (FBN1). Specifically, exon 7 displayed a missense mutation in FGFR2 and exon 64 displayed a mutation in FBN1. Mutations in FGFR play pleiotropic roles in numerous syndromes including Crouzon syndrome, Jackson-Weiss syndrome, Apert syndrome and Pfeiffer syndrome [70,71,72,73]. These craniosynostoses have been associated with HC and FGFR mutations contributing to bony abnormalities, which may explain the venous and CSF outflow obstructions leading to this phenotype [74]. The FGFR mutations identified are predominantly gain of function mutations altering ligand binding and tyrosine kinase activity [75]. In addition, ZPR1 contributes to cell proliferation and FBN1 is associated with TGF beta signaling suggesting their mechanistic contributions to the HC phenotype seen in patients with these phenotypes [76].
Extracellular matrix defects
Table 10 highlights the genetic mutations contributing to extracellular matrix defects. Mutations were found in fukutin (FKTN), cartilage associated protein (CRTAP), collagen type VIII alpha 2 chain (COL8A2), collagen type III alpha 1 chain (COL3A1), collagen type IV alpha 1 chain (COL4A1), vascular cell adhesion molecule 1 (VCAM1), protein tyrosine phosphatase receptor type F (PTPRF), fibrillin 1 (FBN1), laminin subunit beta 1 (LAMB1), FRAS1 related extracellular matrix 1 (FREM1), and the plasminogen gene. CRTAP is involved in proline hydroxylation which ultimately contributes to collagen stability and functionality [77]. Mutations within the CRTAP gene locus can lead to Cole-Carpenter syndrome, which is associated with HC [77]. Other basement membrane proteins encoded by COL8A2, COL3A1, COL4A1, VCAM1, and PTPRF may alert the extracellular matrix and contribute to HC. For instance, a mutation in COL3A1 affects its triple helix stability leading to degradation and further defects in the basement membrane [78]. LAMB1 knockdown in zebrafish disrupted laminin integrity, a component of the basal lamina, leading to brain structural abnormalities [79], suggesting a potential pathogenic link to HC.
Neurogenesis and neural stem cell biology
Table 11 summaries gene mutations implicating neurogenesis. Mutations were identified in SRY-box transcription factor 9 (SOX9), solute carrier family 29 member 3 (SLC29A3), adhesion G protein-coupled receptor (ADGRG1), katanin interacting protein (KIAA0556), G protein signaling modulator 2 (GPSM2), tripartite motif containing 71 (TRIM71) [80], SWI/SNF related, matrix associated, actin dependent regulator of chromatin subfamily c member 1 (SMARCC1) [81], patched 1 (PTCH1), FLVCR heme transporter 2 (FLVCR2), intestinal cell kinase (ICK), cystathionine beta-synthase (CBS), 5-methyltetrahydrofolate-homocysteine methyltransferase reductase (MTRR), interleukin 4 induced 1 (IL4I1), scribble planar cell polarity protein (SCRIB1), protein tyrosine kinase 7 (PTK7), frizzled class receptor 1 (FZD1), VANGL planar cell polarity protein 2 (VANGL2), dishevelled segment polarity protein (DVL2), transcription elongation factor B polypeptide 3B (TCEB3B), phospholipase C delta 4 (PLCD4), Ras associated domain family member 4 (RASSF4), phenylalanyl-tRNA synthetase 2, mitochondrial (FARS2), tubulin beta 3 class III (TUBB3), and discs large MAGUK scaffold protein 5 (DLG5). Frameshift mutations were seen in WD repeat domain 81 (WDR81), kinase D interacting substrate 220 (KIDINS220). Deletions were seen in chromosome 6 (6q25.3 and 6p25), chromosome 13 (13q), chromosome 16 (16p12.2), and chromosome 22 (22q11.2). The 6p25 deletion resulted in the deletion of forkhead box C1 (FOXC1), forkhead box F2 (FOXF2), and forkhead box Q1 (FOXQ1).
The heterogeneity of neurogenesis-associated HC suggests that numerous genes involved in development may confer susceptibility to this phenotype. SOX9 knockdown in mice suggest a role in neural stem cell development and ependymal cell maintenance as a pathogenic mechanism that causes HC [82]. In addition, mutations in ADGRG1 have been shown to impact cerebral cortex development and neuronal migration via the perturbation of the RhoA pathway [83]. In addition, GPSM2 has been shown to alter neuroepithelial function through disruption of cellular orientation and planarity leading to aberrant brain development [84]. Finally, mice lacking KIDINS220 display attenuated responses to neurotrophic factors and have impaired development in multiple signaling pathways [85]. Understanding the genetic influence of neurogenesis may elucidate a better understanding of patient characteristics and poor outcomes in the HC phenotype [86,87,88,89].
Inherited cancer syndromes
Table 12 summarizes genes that contributed to tumor pathogenesis, and which result in the development of HC. Mutations are seen in NRAS proto-oncogene, GTPase (NRAS), von Hippel-Lindau tumor suppressor (VHL), patched 1 (PTCH1) and FA complementation group C (FANCC). Germline mutations are seen in phosphatase and tensin homolog (PTEN) and SUFU negative regulator of hedgehog signaling (SUFU). Deletions within chromosome 11 (11p13) and chromosome 9 (9q22.3 and 9q22-q31) were also identified. NRAS is an oncogene contributing to the development of congenital melanocytic nevi, a condition associated with HC [90]. Clinically relevant mutations in Von Hippau Lindau (VHL) affect protein expression and degradation where patients with or without a mass lesion (i.e., hemangioblastoma) develop HC [91]. Gorlin syndrome is disorder characterized with bony abnormalities and an increased risk for multiple CNS and non-CNS tumors. Previous studies have mapped this syndrome to deletions in the 9q22 locus which is consistent with the patients identified in this review with mutations specifically affecting PTCH1 and FANCC genes [92, 93]. Finally, mutations in SUFU have also been associated with Gorlin syndrome [94, 95].
WNT signaling
WNT signal transduction is involved in numerous pathways regulating cell function and development. Table 13 summarizes gene mutations identified in HC patients with this pathway. Numerous studies have reported gene mutations in coiled-coil and C2 domain containing 2A (CC2D2A) and coiled-coil domain containing 88C (CCDC88C). COACH syndrome is defined as cerebellar vermis hypoplasia, oligophrenia, ataxia, colobomas, and hepatic fibrosis [96]. This gene locus has been shown to interact with the WNT signaling pathway and is associated with centrosome stability [97]. In addition, CCDC88C is associated with the WNT signaling pathway through interaction with the Dishevelled protein [98]. The dishevelled protein contains a binding domain which interacts with a hook related protein transcribed from the CCDC88C locus [99]. WNT signaling plays numerous roles in cell communication and embryonic development, suggesting potential mechanisms contributing to HC [100].
Transcriptional, post-transcriptional, and epigenetic regulation
Table 14 summarizes mutations in genes that regulate transcription, post-transcriptional, and epigenetic processes. Missense mutations were seen in THO complex subunit 6 (THOC6) and HYLS1, genes involved in transcriptional regulation. Patients with loss of function mutations in FA complementation group L (FANCL) we identified. Additional mutations observed included interferon regulatory factory 6 (IRF6), small nucleolar RNA, C/D box 118 (SNORD118), nuclear factor I A (NFIA), SET binding protein 1 (SETBP1), SWI/SNF related, matrix associated, actin dependent regulator of chromatin, subfamily b, member 1 (SMARCB1), maelstrom spermatogenic transposon (MAEL), a deletion in chromosome 5 (5q35.3), and 20q13.3 trisomy. Deletions in chromosome 1 (1q42.3-q44) resulted in the deletion of zinc finger and BTB domain containing 18 (ZBTB18) and heterogeneous nuclear ribonucleoprotein U (HNRNPU). THOC6 is a part the TREX complex responsible for mRNA export and is localized to the 5’ cap of mRNA [101]. It has been associated with Beaulieu-Boycott-Innes syndrome, which is charactered by developmental delay and organ dysgenesis [102]. Patients identified in this review with Beaulieu-Boycott-Innes syndrome and THOC6 mutations have been shown to develop HC, suggesting a role for mRNA export regulation in association with HC phenotypes [103]. HYLS1 is associated with Hydrolethalus syndrome, a disorder characterized by HC and craniofacial abnormalities [104]. Expression analysis of this gene suggests a role in CNS development, where a HC associated mutation gene causes nuclear localization whereas the WT form is expressed in the cytoplasm [104]. SNORD118 is involved in regulation of ribosome biology and associated with the hydrocephalic phenotype of Labrune syndrome, characterized by leukoencephalopathy, intracranial cysts, and calcification [105]. While the function of SETBP1 remains largely unknown, mutations in this gene are associated with Schinzel-Giedion syndrome, characterized by facial abnormalities, intellectual disability, congenital malformations, and HC [106]. SMARCB1 is involved in chromatin remodeling to further enhance or repress transcription [107]. Finally, a transcriptome-wide association study (TWAS) and multi-omics study of HC identified maelstrom (MAEL), a gene that regulates transposons and epigenetic modifications, as an experiment-wide predictor of HC in the cortex [9, 108]. These studies identified transcriptional regulators and further emphasize the need to explore these mechanisms to understand the mechanistic associations with HC.
Ion transport and regulation
Table 15 summarizes gene mutations implicating ion transport. Mutations were seen in aquaporin 4 (AQP4) and FLVCR heme transporter 2 (FLVCR2). Mutations on chromosome 17 (17p13) implicated transient receptor potential cation channel subfamily V member 3 (TRPV3). Aquaporin 4 (AQP4) regulates water transport on ependymal cells and knockout of this gene in mice show disrupted gap junctions which alter the ependymal zone and CSF flow contributing to HC development [109; 110]. Mutations in the enhancer of TMEM50b alter expression of TTF, a direct transcriptional regulator of AQP1, have also been identified [101]. Mutations in FLVCR2 are associated with Fowler’s syndrome, a disorder characterized by HC and hydranencephaly [111]. This gene locus encodes a transmembrane protein involved in solute transport, suggesting that defects in chemiosmotic regulation contribute to HC development [112].
Normal pressure hydrocephalus
Normal pressure HC (NPH) is a form of communicating HC in which the progressive pressure of CSF is believed to result in in ventricular dilatation and further CSF accumulation. Table 16 summarizes the genes implicated in human studies of NPH. Scm like with four mbt domains 1 (SFMBT1) displayed an intron 2 deletion. Cilia and flagella associated protein 43 (CFAP43) was found to have a nonsense mutation. The gene locus contributing to the development of ETINPH, a disorder characterized with essential tremors and idiopathic NPH, was localized to 19q12-13.31 on chromosome 19. SFMBT1 is highly expressed in ependymal cells and epithelial cells of the brain, suggesting that a mutation in this gene locus may contribute to the dysfunctional CSF circulation [113]. Furthermore, a binding site had been identified within intron 2 of this gene locus, suggesting that the deletion of this intron, as seen in our review, will impact function [114; 115]. Deletion of cell wall biogenesis 43 (CWH43) in humans has also been associated with NPH [116].
Metabolism
Table 17 indicates genes involved in metabolic pathways. Mutations were seen in cytochrome c oxidase subunit 6B1 (COX6B1), methylenetetrahydrofolate reductase (MTHFR), and sulfatase modifying factor 1 (SUMF1). Mutations in COX6B1 have been shown to disrupt the electron transport chain suggesting that alterations in cellular energetics can contribute to HC [117] [118]. SUMF1 encodes formylglycine generating enzyme (FGE) involved in modifying cysteine residues in the endoplasmic reticulum [119]. MTHFR regulates folate metabolism, and mutations within this gene locus have been identified in congenital HC patients providing rationale to explore metabolic genes and their association with pathology [120].
Cell cycle and cytoarchitecture
Table 18 displays genes involved in cell cycle regulation and cytoarchitecture. Mutations were seen in spindle apparatus coiled-coil protein 1 (SPDL1), tubulin alpha 3e (TUBA3E), nidogen 1 (NID1), tRNA splicing endonuclease subunit 15 (TSEN15), clathrin heavy chain linker domain containing 1 (CLHC1), TBC1 domain containing kinase (TBCK), xin actin binding repeat containing 1 (XIRP1), nucleoporin 107 (NUP107), erythrocyte membrane protein band 4.1 like 4A (EPB41L4A), protein phosphatase 2 regulatory subunit B delta (PPP2R5D), protein phosphatase 2 scaffold subunit Alpha (PPP2R1A), prolyl 4-hydroxylase subunit beta (P4HB), and crumbs cell polarity complex component 2 (CRB2). SPDL1 has been shown to regulate mitotic checkpoints, and mutations arrested affected cells in metaphase [121]. TUBA3E maintains microtubule integrity by encoding for part of the microtubule heterodimer, alpha tubulin [122]. TSEN15 contributes to an endonuclease complex involved in tRNA splicing, and mutations affecting this gene locus can lead to defects in cell division [123]. XIRP1 has been shown to maintain actin integrity and stability [124]. P4HB encodes an enzyme subunit involved in collagen formation, and mutations affecting this gene location are associated with reduced cytoarchitectural stability [125].
Lipid structure and regulation
Table 19 summarizes genes involved in lipid structure and regulation associated with HC in humans. Mutations were seen in bridge-like lipid transfer protein family member 1 (KIAA1109), and glucosylceramidase beta 1 (GBA). The KIAA1109 ortholog in Drosophila melanogaster has shown to affect synaptic growth at the neuromuscular junction through modulation of phosphatidylinositol 4,5-bisphosphate (PIP2) [126]. GBA encodes for a lysosomal enzyme responsible for metabolizing glycolipids [127].
Genes of unknown function
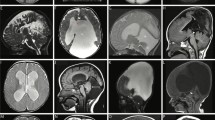
Table 20 summarizes genes that are associated with HC pathology without a clear function. Additional variants include partial 1q trisomy, tetrasomy 5p, tetraploidy of chromosome 9, trisomy 9p, and chromosome 21 trisomy. Studies that have identified mutations in chromone 6 displayed microdeletions or mosaicism of monosomy. Deletions in chromosome 8 (8q12.2-q21.2) and chromosome 16 (16q) were also identified, and microduplications in chromosome 17 (17p13.1) have been reported. The vast genetic influence on HC emphasizes importance of exploring and understanding the factors that confer genetic risk to improve diagnostic and prognostic efficiency. Autosomal and sex chromosomal location of all genetic findings included in this review is summarized in Figs. 3, 4.
Global burden of genetic hydrocephalus
We next aimed to quantify the country of origin for patients included in this review (Fig. 5). Given the wide range of HC disease burden across the world [3], we aimed to determine if genetic studies of HC were similarly representative. What is clear is that for regions of the world where HC prevalence is highest (Africa, East Asia, etc.), there is an obvious lack of genetic studies of HC of any kind. For example, there is not a single study performed by authors in Sub-Saharan Africa (SSA) or including people from SSA. Given that African genomes are the most diverse and complex with generations of environmental pressures (including emerging pathogens) shaping the genome, understanding genetic risk factors in these populations is essential. While epidemiological estimates of the contribution of genetically linked forms of HC is not feasible at present, these data begin to highlight disparities in representation of genetic studies and the need for large-scale genetic studies of HC in diverse populations. These data also provide a reasonable estimate of the potential burden, although likely underestimated, contribution of genetic factors contributing to HC. It is our hope that this review highlights the diverse mechanisms underlying HC, the complex molecular pathways that may contribute to HC pathogenesis, and the need to greatly expand the representation of diverse peoples in HC genetics research.
Discussion
HC is a complex, heterogenous condition that can be a component of a wide range of genetic conditions and can be caused by a variety of preceding environmental factors. Because HC is a component of many syndromes with a wide range of concomitant phenotypes, understanding the genetic pleiotropism of contributing genes is important for delineating the pathophysiologic basis of the disease. This review provides a broad overview of the associations between genetic mechanisms underlying HC. The variability in phenotypes observed, methodology used to uncover genetic information, and wide range of validation of genetic findings highlights the major challenges in the field. While many studies are descriptive, a wide range of hypotheses are generated based on implicated genes and potential mechanisms. Specifically, many studies implicate alterations in neurogenesis and primary brain development, as opposed to direct alterations in CSF regulation, as potential pathophysiologic mechanisms. Overall, as genomic technologies become more ubiquitous in clinical practice and more patients undergo unbiased genomic sequencing, our understanding of HC will improve. However, there are several limitations and points to consider as this field evolves.
An ongoing challenge in human genetics is proving causality of implicated genetic findings. Classical validation technique requires reproducing the implicated mutation (if evolutionarily conserved) in a model organism such as a mouse or rat. However, the physiologic regulation of CSF and mechanisms underlying brain development are markedly different in these model organisms and often do not recapitulate human disease. Many genes underlying HC are associated with other phenotypes, and it may not be possible to identify a secondary causative genetic factor that unmasks the phenotype. Since this approach relies on the gene product being evolutionarily conserved, identification of human-specific disease mechanisms is impaired. Alternative approaches to determining the relationship of a gene variant to a HC phenotype include structural biologic modeling of presumed deleterious mutations; however, this approach does not consider physiological and phenotypic heterogeneity. Similarly, these approaches often rely on protein expression in prokaryotic systems, limiting interpretation of post-translational modifications and other physiologic contributors to protein function.
Based on the significant co-occurrence of traits affecting other organ systems, it is likely that genes associated with HC display significant pleiotropy. A simplistic model of monogenic contributions to HC is unlikely to capture the genetic etiology of most cases. Even among monogenic contributions to HC, there is significant phenotypic and genetic variability (i.e., L1CAM). As quantitative genetic methodology improves to identify polygenic contributors to disease, we suspect that a much larger proportion of cases will have polygenic contributions. Because HC is a heterogenous disease, accrual of large numbers of ‘homogenous’ cases are needed to accurately quantify reproductible genetic associations.
The variability in genomic technology used to determine potential genetic contributions to HC is significant. Agnostic methods such as genome wide association studies (GWAS), transcriptome-wide association studies (TWAS), whole-exome sequencing (WES), and whole-genome sequencing (WGS) have been used, but are limited by cost, sample size, and technical expertise involved in analysis. In contrast, targeted sequencing approaches rely on hypothesis-driven identification of implicated genetic loci introducing significant experimental bias.
Our review highlights that most genetic studies of HC are performed in countries where disease burden, paradoxically, is amongst the lowest in the world. This reflects disproportionately low resources for genetic studies in low- and middle-income countries. For example, Sub Saharan Africa the most genetically diverse and complex region in the world, where the burden of HC is also the highest, yet there are no genetic studies of HC of any kind in these populations. Although the burden of HC is largely the result of infections, the genetic contributors to infection susceptibility are largely uncharacterized in these populations. Evolutionary selection pressures have been differentially shaped by exposure to infectious pathogens, geographic shifts of ancestral peoples, and population isolation. Therefore, understanding genetic factors specific to these populations is paramount to improve secondary prevention and moving towards non-surgical treatment options.
Advances in genetic technology and interpretation coupled with decreased costs will garner a new era of precision medicine that can be applied in the clinic [128]. The extent to which genetic information may guide treatment in HC has not been fully realized. As more patients are rigorously studied using complementary and convergent genomic approaches coupled with long-term clinical outcomes, we may be able to incorporate genetic information into clinical care. Owing to the genetic architecture of HC highlighted here and across many studies, we anticipate that creation of polygenic risk scores (PRS) may be the most clinically meaningful and practical for disease prognostication and understanding comorbid disease risks.
Conclusions
HC is a phenotypically and genetically complex disease. While the literature describing the genetic causes of HC is vast, this comprehensive review highlights opportunities for further mechanistic study and disparities in ancestral representation. The varying rigor with which genetic studies are conducted highlights the challenge of determining causality of implicated genomic alterations, inadequacies of current model systems, and the need for human-specific molecular validation studies. What is clear is that our genetic understanding of HC is incomplete and our understanding of pleiotropy of implicated HC genes requires further maturation. This study represents the first large-scale systematic literature review of the genetic basis of HC in humans and highlights many areas ripe for future investigation.
Availability of data and materials
All data are contained within the manuscript.
References
Khasawneh AH, Garling RJ, Harris CA. Cerebrospinal fluid circulation: what do we know and how do we know it? Brain Circ. 2018;4:14–8.
Atchley TJ, Vukic B, Vukic M, Walters BC. Review of cerebrospinal fluid physiology and dynamics: a call for medical education reform. Neurosurgery. 2022;91:1–7.
Dewan MC, Rattani A, Mekary R, Glancz LJ, Yunusa I, Baticulon RE, Fieggen G, Wellons JC, Park KB, Warf BC. Global hydrocephalus epidemiology and incidence: systematic review and meta-analysis. J Neurosurg. 2018;1:1–15.
Gmeiner M, Wagner H, Zacherl C, Polanski P, Auer C, van Ouwerkerk WJ, Holl K. Long-term mortality rates in pediatric hydrocephalus-a retrospective single-center study. Childs Nerv Syst. 2017;33:101–9.
Kousi M, Katsanis N. The Genetic Basis of Hydrocephalus. Annu Rev Neurosci. 2016;39:409–35.
Kahle KT, Kulkarni AV, Limbrick DD Jr, Warf BC. Hydrocephalus in children. Lancet. 2016;387:788–99.
Tomycz LD, Hale AT, George TM. Emerging insights and new perspectives on the nature of hydrocephalus. Pediatr Neurosurg. 2017;52:361–8.
Furey CG, Choi J, Jin SC, Zeng X, Timberlake AT, Nelson-Williams C, Mansuri MS, Lu Q, Duran D, Panchagnula S, Allocco A, Karimy JK, Khanna A, Gaillard JR, DeSpenza T, Antwi P, Loring E, Butler WE, Smith ER, Warf BC, Strahle JM, Limbrick DD, Storm PB, Heuer G, Jackson EM, Iskandar BJ, Johnston JM, Tikhonova I, Castaldi C, López-Giráldez F, Bjornson RD, Knight JR, Bilguvar K, Mane S, Alper SL, Haider S, Guclu B, Bayri Y, Sahin Y, Apuzzo MLJ, Duncan CC, DiLuna ML, Günel M, Lifton RP, Kahle KT. De novo mutation in genes regulating neural stem cell fate in human congenital hydrocephalus. Neuron. 2018;99:302-314.e4.
Hale AT, Bastarache L, Morales DM, Wellons JC 3rd, Limbrick DD Jr, Gamazon ER. Multi-omic analysis elucidates the genetic basis of hydrocephalus. Cell Rep. 2021;35: 109085.
Jin SC, Dong W, Kundishora AJ, Panchagnula S, Moreno-De-Luca A, Furey CG, Allocco AA, Walker RL, Nelson-Williams C, Smith H, Dunbar A, Conine S, Lu Q, Zeng X, Sierant MC, Knight JR, Sullivan W, Duy PQ, DeSpenza T, Reeves BC, Karimy JK, Marlier A, Castaldi C, Tikhonova IR, Li B, Peña HP, Broach JR, Kabachelor EM, Ssenyonga P, Hehnly C, Ge L, Keren B, Timberlake AT, Goto J, Mangano FT, Johnston JM, Butler WE, Warf BC, Smith ER, Schiff SJ, Limbrick DD Jr, Heuer G, Jackson EM, Iskandar BJ, Mane S, Haider S, Guclu B, Bayri Y, Sahin Y, Duncan CC, Apuzzo MLJ, DiLuna ML, Hoffman EJ, Sestan N, Ment LR, Alper SL, Bilguvar K, Geschwind DH, Günel M, Lifton RP, Kahle KT. Exome sequencing implicates genetic disruption of prenatal neuro-gliogenesis in sporadic congenital hydrocephalus. Nat Med. 2020;26:1754–65.
Kulkarni AV, Schiff SJ, Mbabazi-Kabachelor E, Mugamba J, Ssenyonga P, Donnelly R, Levenbach J, Monga V, Peterson M, MacDonald M, Cherukuri V, Warf BC. Endoscopic treatment versus shunting for infant hydrocephalus in Uganda. N Engl J Med. 2017;377:2456–64.
J. Lim, A.R. Tang, C. Liles, A.A. Hysong, A.T. Hale, C.M. Bonfield, R.P. Naftel, J.C. Wellons, and C.N. Shannon, The cost of hydrocephalus: a cost-effectiveness model for evaluating surgical techniques. (2018) 1.
Hale AT, Riva-Cambrin J, Wellons JC, Jackson EM, Kestle JRW, Naftel RP, Hankinson TC, Shannon CN. Machine learning predicts risk of cerebrospinal fluid shunt failure in children: a study from the hydrocephalus clinical research network. Childs Nerv Syst. 2021;37:1485–94.
Hale AT, Stanton AN, Zhao S, Haji F, Gannon SR, Arynchyna A, Wellons JC, Rocque BG, Naftel RP. Predictors of endoscopic third ventriculostomy ostomy status in patients who experience failure of endoscopic third ventriculostomy with choroid plexus cauterization. J Neurosurg Pediatr. 2019;24:41–6.
Whitelaw A, Kennedy CR, Brion LP. Diuretic therapy for newborn infants with posthemorrhagic ventricular dilatation. Cochrane Database Syst Rev. 2001;1:cd002270.
C.G. Furey, J. Choi, S.C. Jin, X. Zeng, A.T. Timberlake, C. Nelson-Williams, M.S. Mansuri, Q. Lu, D. Duran, S. Panchagnula, A. Allocco, J.K. Karimy, A. Khanna, J.R. Gaillard, T. DeSpenza, P. Antwi, E. Loring, W.E. Butler, E.R. Smith, B.C. Warf, J.M. Strahle, D.D. Limbrick, P.B. Storm, G. Heuer, E.M. Jackson, B.J. Iskandar, J.M. Johnston, I. Tikhonova, C. Castaldi, F. Lopez-Giraldez, R.D. Bjornson, J.R. Knight, K. Bilguvar, S. Mane, S.L. Alper, S. Haider, B. Guclu, Y. Bayri, Y. Sahin, M.L.J. Apuzzo, C.C. Duncan, M.L. DiLuna, M. Gunel, R.P. Lifton, and K.T. Kahle, De Novo Mutation in Genes Regulating Neural Stem Cell Fate in Human Congenital Hydrocephalus. Neuron (2018).
Lehtinen MK, Bjornsson CS, Dymecki SM, Gilbertson RJ, Holtzman DM, Monuki ES. The choroid plexus and cerebrospinal fluid: emerging roles in development, disease, and therapy. J Neurosci. 2013;33:17553–9.
Lehtinen MK, Walsh CA. Neurogenesis at the brain-cerebrospinal fluid interface. Annu Rev Cell Dev Biol. 2011;27:653–79.
Lehtinen MK, Zappaterra MW, Chen X, Yang YJ, Hill AD, Lun M, Maynard T, Gonzalez D, Kim S, Ye P, D’Ercole AJ, Wong ET, LaMantia AS, Walsh CA. The cerebrospinal fluid provides a proliferative niche for neural progenitor cells. Neuron. 2011;69:893–905.
Carter CS, Vogel TW, Zhang Q, Seo S, Swiderski RE, Moninger TO, Cassell MD, Thedens DR, Keppler-Noreuil KM, Nopoulos P, Nishimura DY, Searby CC, Bugge K, Sheffield VC. Abnormal development of NG2+PDGFR-alpha+ neural progenitor cells leads to neonatal hydrocephalus in a ciliopathy mouse model. Nat Med. 2012;18:1797–804.
Takagishi M, Sawada M, Ohata S, Asai N, Enomoto A, Takahashi K, Weng L, Ushida K, Ara H, Matsui S, Kaibuchi K, Sawamoto K, Takahashi M. Daple coordinates planar polarized microtubule dynamics in ependymal cells and contributes to hydrocephalus. Cell Rep. 2017;20:960–72.
Wilson GR, Wang HX, Egan GF, Robinson PJ, Delatycki MB, O’Bryan MK, Lockhart PJ. Deletion of the Parkin co-regulated gene causes defects in ependymal ciliary motility and hydrocephalus in the quakingviable mutant mouse. Hum Mol Genet. 2010;19:1593–602.
Wodarczyk C, Rowe I, Chiaravalli M, Pema M, Qian F, Boletta A. A novel mouse model reveals that polycystin-1 deficiency in ependyma and choroid plexus results in dysfunctional cilia and hydrocephalus. PLoS ONE. 2009;4: e7137.
Castaneyra-Ruiz L, Morales DM, McAllister JP, Brody SL, Isaacs AM, Strahle JM, Dahiya SM, Limbrick DD. Blood exposure causes ventricular zone disruption and glial activation in vitro. J Neuropathol Exp Neurol. 2018;77:803–13.
McAllister JP, Guerra MM, Ruiz LC, Jimenez AJ, Dominguez-Pinos D, Sival D, den Dunnen W, Morales DM, Schmidt RE, Rodriguez EM, Limbrick DD. Ventricular zone disruption in human neonates with intraventricular hemorrhage. J Neuropathol Exp Neurol. 2017;76:358–75.
Karimy JK, Zhang J, Kurland DB, Theriault BC, Duran D, Stokum JA, Furey CG, Zhou X, Mansuri MS, Montejo J, Vera A, DiLuna ML, Delpire E, Alper SL, Gunel M, Gerzanich V, Medzhitov R, Simard JM, Kahle KT. Inflammation-dependent cerebrospinal fluid hypersecretion by the choroid plexus epithelium in posthemorrhagic hydrocephalus. Nat Med. 2017;23:997–1003.
Lun MP, Monuki ES, Lehtinen MK. Development and functions of the choroid plexus-cerebrospinal fluid system. Nat Rev Neurosci. 2015;16:445–57.
Robert SM, Reeves BC, Marlier A, Duy PQ, DeSpenza T, Kundishora A, Kiziltug E, Singh A, Allington G, Alper SL, Kahle KT. Inflammatory hydrocephalus. Childs Nerv Syst. 2021;37:3341–53.
Robert SM, Reeves BC, Kiziltug E, Duy PQ, Karimy JK, Mansuri MS, Marlier A, Allington G, Greenberg ABW, DeSpenza T Jr, Singh AK, Zeng X, Mekbib KY, Kundishora AJ, Nelson-Williams C, Hao LT, Zhang J, Lam TT, Wilson R, Butler WE, Diluna ML, Feinberg P, Schafer DP, Movahedi K, Tannenbaum A, Koundal S, Chen X, Benveniste H, Limbrick DD Jr, Schiff SJ, Carter BS, Gunel M, Simard JM, Lifton RP, Alper SL, Delpire E, Kahle KT. The choroid plexus links innate immunity to CSF dysregulation in hydrocephalus. Cell. 2023;186:764-785.e21.
Zhang J, Williams MA, Rigamonti D. Genetics of human hydrocephalus. J Neurol. 2006;253:1255–66.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Hamosh A, Scott AF, Amberger JS, Bocchini CA, McKusick VA. Online Mendelian Inheritance in Man (OMIM), a knowledgebase of human genes and genetic disorders. Nucleic Acids Res. 2005;33:D514–7.
T.H. Andrew, Z. Dan, L.S. Rebecca, B. Lisa, W. Liuyang, S.Z. Sandra, J.S. Steven, C.K. Dennis, and R.G. Eric, The genetic architecture of human infectious diseases and pathogen-induced cellular phenotypes. medRxiv (2021) 2020.07.19.20157404.
Doğanli C, Beck HC, Ribera AB, Oxvig C, Lykke-Hartmann K. α3Na+/K+-ATPase deficiency causes brain ventricle dilation and abrupt embryonic motility in zebrafish. J Biol Chem. 2013;288:8862–74.
Howard HC, Mount DB, Rochefort D, Byun N, Dupré N, Lu J, Fan X, Song L, Rivière JB, Prévost C, Horst J, Simonati A, Lemcke B, Welch R, England R, Zhan FQ, Mercado A, Siesser WB, George AL Jr, McDonald MP, Bouchard JP, Mathieu J, Delpire E, Rouleau GA. The K-Cl cotransporter KCC3 is mutant in a severe peripheral neuropathy associated with agenesis of the corpus callosum. Nat Genet. 2002;32:384–92.
Jin SC, Furey CG, Zeng X, Allocco A, Nelson-Williams C, Dong W, Karimy JK, Wang K, Ma S, Delpire E. SLC12A ion transporter mutations in sporadic and familial human congenital hydrocephalus. Mol Genet Genomic Med. 2019;7: e892.
Le Goff C, Morice-Picard F, Dagoneau N, Wang LW, Perrot C, Crow YJ, Bauer F, Flori E, Prost-Squarcioni C, Krakow D. ADAMTSL2 mutations in geleophysic dysplasia demonstrate a role for ADAMTS-like proteins in TGF-β bioavailability regulation. Nat Genet. 2008;40:1119–23.
Berger I, Ben-Neriah Z, Dor-Wolman T, Shaag A, Saada A, Zenvirt S, Raas-Rothschild A, Nadjari M, Kaestner KH, Elpeleg O. Early prenatal ventriculomegaly due to an AIFM1 mutation identified by linkage analysis and whole exome sequencing. Mol Genet Metab. 2011;104:517–20.
Saillour Y, Zanni G, Des-Portes V, Heron D, Guibaud L, Iba-Zizen MT, Pedespan JL, Poirier K, Castelnau L, Julien C, Franconnet C, Bonthron D, Porteous ME, Chelly J, Bienvenu T. Mutations in the AP1S2 gene encoding the sigma 2 subunit of the adaptor protein 1 complex are associated with syndromic X-linked mental retardation with hydrocephalus and calcifications in basal ganglia. J Med Genetics. 2007;44:739–44.
Westendorf JJ, Zaidi SK, Cascino JE, Kahler R, van Wijnen AJ, Lian JB, Yoshida M, Stein GS, Li X. Runx2 (Cbfa1, AML-3) interacts with histone deacetylase 6 and represses the p21(CIP1/WAF1) promoter. Mol Cell Biol. 2002;22:7982–92.
Beck DB, Basar MA, Asmar AJ, Thompson JJ, Oda H, Uehara DT, Saida K, Pajusalu S, Talvik I, D’Souza P, Bodurtha J, Mu W, Barañano KW, Miyake N, Wang R, Kempers M, Tamada T, Nishimura Y, Okada S, Kosho T, Dale R, Mitra A, Macnamara E, Matsumoto N, Inazawa J, Walkiewicz M, Õunap K, Tifft CJ, Aksentijevich I, Kastner DL, Rocha PP, Werner A. Linkage-specific deubiquitylation by OTUD5 defines an embryonic pathway intolerant to genomic variation. Sci Adv. 2021;7:1.
Peters T, Perrier R, Haber RM. Focal dermal hypoplasia: report of a case with myelomeningocele, Arnold-Chiari malformation and hydrocephalus with a review of neurologic manifestations of Goltz syndrome. Pediatr Dermatol. 2014;31:220–4.
Zhang YW, Qu HB, Long N, Leng XY, Liu YQ, Yang Y. A rare mutant of OFD1 gene responsible for Joubert syndrome with significant phenotype variation. Mol Genet Genomics. 2021;296:33–40.
Grindstaff KK, Yeaman C, Anandasabapathy N, Hsu SC, Rodriguez-Boulan E, Scheller RH, Nelson WJ. Sec6/8 complex is recruited to cell-cell contacts and specifies transport vesicle delivery to the basal-lateral membrane in epithelial cells. Cell. 1998;93:731–40.
Cao-Ehlker X, Zong X, Hammelmann V, Gruner C, Fenske S, Michalakis S, Wahl-Schott C, Biel M. Up-regulation of hyperpolarization-activated cyclic nucleotide-gated channel 3 (HCN3) by specific interaction with K+ channel tetramerization domain-containing protein 3 (KCTD3). J Biol Chem. 2013;288:7580–9.
Chung KT, Shen Y, Hendershot LM. BAP, a mammalian BiP-associated protein, is a nucleotide exchange factor that regulates the ATPase activity of BiP. J Biol Chem. 2002;277:47557–63.
Tyson JR, Stirling CJ. LHS1 and SIL1 provide a lumenal function that is essential for protein translocation into the endoplasmic reticulum. Embo J. 2000;19:6440–52.
Yahyaoui R, Espinosa MG, Gómez C, Dayaldasani A, Rueda I, Roldán A, Ugarte M, Lastra G, Pérez V. Neonatal carnitine palmitoyltransferase II deficiency associated with Dandy-Walker syndrome and sudden death. Mol Genet Metab. 2011;104:414–6.
Valente EM, Logan CV, Mougou-Zerelli S, Lee JH, Silhavy JL, Brancati F, Iannicelli M, Travaglini L, Romani S, Illi B. Mutations in TMEM216 perturb ciliogenesis and cause Joubert, Meckel and related syndromes. Nat Genet. 2010;42:619–25.
Duran I, Taylor SP, Zhang W, Martin J, Qureshi F, Jacques SM, Wallerstein R, Lachman RS, Nickerson DA, Bamshad M. Mutations in IFT-A satellite core component genes IFT43 and IFT121 produce short rib polydactyly syndrome with distinctive campomelia. Cilia. 2017;6:1–13.
Joo K, Kim CG, Lee M-S, Moon H-Y, Lee S-H, Kim MJ, Kweon H-S, Park W-Y, Kim C-H, Gleeson JG. CCDC41 is required for ciliary vesicle docking to the mother centriole. Proc Natl Acad Sci. 2013;110:5987–92.
Rocca MS, Piatti G, Michelucci A, Guazzo R, Bertini V, Vinanzi C, Caligo MA, Valetto A, Foresta C. A novel genetic variant in DNAI2 detected by custom gene panel in a newborn with Primary Ciliary Dyskinesia: case report. BMC Med Genet. 2020;21:1–6.
Mei H-F, Dong X-R, Chen H-Y, Lu Y-L, Wu B-B, Wang H-J, Cheng G-Q, Wang L-S, Cao Y, Yang L. Genetic etiologies associated with infantile hydrocephalus in a Chinese infantile cohort. World J Pediatr. 2021;17:305–16.
DeSpenza T Jr, Carlson M, Panchagnula S, Robert S, Duy PQ, Mermin-Bunnell N, Reeves BC, Kundishora A, Elsamadicy AA, Smith H, Ocken J, Alper SL, Jin SC, Hoffman EJ, Kahle KT. PTEN mutations in autism spectrum disorder and congenital hydrocephalus: developmental pleiotropy and therapeutic targets. Trends Neurosci. 2021;44:961–76.
Mashimo T, Hadjebi O, Amair-Pinedo F, Tsurumi T, Langa F, Serikawa T, Sotelo C, Guénet JL, Rosa JL. Progressive Purkinje cell degeneration in tambaleante mutant mice is a consequence of a missense mutation in HERC1 E3 ubiquitin ligase. PLoS Genet. 2009;5: e1000784.
Jacquet BV, Salinas-Mondragon R, Liang H, Therit B, Buie JD, Dykstra M, Campbell K, Ostrowski LE, Brody SL, Ghashghaei HT. FoxJ1-dependent gene expression is required for differentiation of radial glia into ependymal cells and a subset of astrocytes in the postnatal brain. Development. 2009;136:4021–31.
Lian G, Chenn A, Ekuta V, Kanaujia S, Sheen V. Formin 2 regulates lysosomal degradation of Wnt-associated β-catenin in neural progenitors. Cerebral Cortex. 2019;29:1938–52.
Gavino C, Richard S. Patched1 haploinsufficiency impairs ependymal cilia function of the quaking viable mice, leading to fatal hydrocephalus. Mol Cell Neurosci. 2011;47:100–7.
Liedtke W, Edelmann W, Bieri PL, Chiu FC, Cowan NJ, Kucherlapati R, Raine CS. GFAP is necessary for the integrity of CNS white matter architecture and long-term maintenance of myelination. Neuron. 1996;17:607–15.
Qin B, He M, Chen X, Pei D. Sorting nexin 10 induces giant vacuoles in mammalian cells. J Biol Chem. 2006;281:36891–6.
Chen Y, Wu B, Xu L, Li H, Xia J, Yin W, Li Z, Shi D, Li S, Lin S, Shu X, Pei D. A SNX10/V-ATPase pathway regulates ciliogenesis in vitro and in vivo. Cell Res. 2012;22:333–45.
DeMari J, Mroske C, Tang S, Nimeh J, Miller R, Lebel RR. CLTC as a clinically novel gene associated with multiple malformations and developmental delay. Am J Med Genet A. 2016;170:958–66.
Rajadhyax M, Neti G, Crow Y, Tyagi A. Neurological presentation of Griscelli syndrome: obstructive hydrocephalus without haematological abnormalities or organomegaly. Brain Develop. 2007;29:247–50.
Miller EA, Schekman R. COPII—a flexible vesicle formation system. Curr Opin Cell Biol. 2013;25:420–7.
Hamazaki Y, Itoh M, Sasaki H, Furuse M, Tsukita S. Multi-PDZ domain protein 1 (MUPP1) is concentrated at tight junctions through its possible interaction with claudin-1 and junctional adhesion molecule. J Biol Chem. 2002;277:455–61.
Adams JC, Tucker RP. The thrombospondin type 1 repeat (TSR) superfamily: diverse proteins with related roles in neuronal development. Dev Dyn. 2000;218:280–99.
Michele DE, Barresi R, Kanagawa M, Saito F, Cohn RD, Satz JS, Dollar J, Nishino I, Kelley RI, Somer H, Straub V, Mathews KD, Moore SA, Campbell KP. Post-translational disruption of dystroglycan-ligand interactions in congenital muscular dystrophies. Nature. 2002;418:417–22.
von Renesse A, Petkova MV, Lützkendorf S, Heinemeyer J, Gill E, Hübner C, von Moers A, Stenzel W, Schuelke M. POMK mutation in a family with congenital muscular dystrophy with merosin deficiency, hypomyelination, mild hearing deficit and intellectual disability. J Med Genet. 2014;51:275–82.
Godfrey C, Clement E, Mein R, Brockington M, Smith J, Talim B, Straub V, Robb S, Quinlivan R, Feng L, Jimenez-Mallebrera C, Mercuri E, Manzur AY, Kinali M, Torelli S, Brown SC, Sewry CA, Bushby K, Topaloglu H, North K, Abbs S, Muntoni F. Refining genotype phenotype correlations in muscular dystrophies with defective glycosylation of dystroglycan. Brain. 2007;130:2725–35.
Jabs EW, Li X, Scott AF, Meyers G, Chen W, Eccles M, Mao JI, Charnas LR, Jackson CE, Jaye M. Jackson-Weiss and Crouzon syndromes are allelic with mutations in fibroblast growth factor receptor 2. Nat Genet. 1994;8:275–9.
Lajeunie E, Ma HW, Bonaventure J, Munnich A, Le Merrer M, Renier D. FGFR2 mutations in Pfeiffer syndrome. Nat Genet. 1995;9:108.
Reardon W, Winter RM, Rutland P, Pulleyn LJ, Jones BM, Malcolm S. Mutations in the fibroblast growth factor receptor 2 gene cause Crouzon syndrome. Nat Genet. 1994;8:98–103.
Wilkie AO, Slaney SF, Oldridge M, Poole MD, Ashworth GJ, Hockley AD, Hayward RD, David DJ, Pulleyn LJ, Rutland P, et al. Apert syndrome results from localized mutations of FGFR2 and is allelic with Crouzon syndrome. Nat Genet. 1995;9:165–72.
Rich PM, Cox TC, Hayward RD. The jugular foramen in complex and syndromic craniosynostosis and its relationship to raised intracranial pressure. AJNR Am J Neuroradiol. 2003;24:45–51.
Kan SH, Elanko N, Johnson D, Cornejo-Roldan L, Cook J, Reich EW, Tomkins S, Verloes A, Twigg SR, Rannan-Eliya S, McDonald-McGinn DM, Zackai EH, Wall SA, Muenke M, Wilkie AO. Genomic screening of fibroblast growth-factor receptor 2 reveals a wide spectrum of mutations in patients with syndromic craniosynostosis. Am J Hum Genet. 2002;70:472–86.
Ito YA, Smith AC, Kernohan KD, Pena IA, Ahmed A, McDonell LM, Beaulieu C, Bulman DE, Smidt A, Sawyer SL, Dyment DA, Boycott KM, Clericuzio CL. A ZPR1 mutation is associated with a novel syndrome of growth restriction, distinct craniofacial features, alopecia, and hypoplastic kidneys. Clin Genet. 2018;94:303–12.
Balasubramanian M, Pollitt RC, Chandler KE, Mughal MZ, Parker MJ, Dalton A, Arundel P, Offiah AC, Bishop NJ. CRTAP mutation in a patient with Cole-Carpenter syndrome. Am J Med Genet A. 2015;167:587–91.
Kroes HY, Pals G, van Essen AJ. Ehlers-Danlos syndrome type IV: unusual congenital anomalies in a mother and son with a COL3A1 mutation and a normal collagen III protein profile. Clin Genet. 2003;63:224–7.
Lee J, Gross JM. Laminin beta1 and gamma1 containing laminins are essential for basement membrane integrity in the zebrafish eye. Invest Ophthalmol Vis Sci. 2007;48:2483–90.
Duy PQ, Weise SC, Marini C, Li XJ, Liang D, Dahl PJ, Ma S, Spajic A, Dong W, Juusola J, Kiziltug E, Kundishora AJ, Koundal S, Pedram MZ, Torres-Fernández LA, Händler K, De Domenico E, Becker M, Ulas T, Juranek SA, Cuevas E, Hao LT, Jux B, Sousa AMM, Liu F, Kim SK, Li M, Yang Y, Takeo Y, Duque A, Nelson-Williams C, Ha Y, Selvaganesan K, Robert SM, Singh AK, Allington G, Furey CG, Timberlake AT, Reeves BC, Smith H, Dunbar A, DeSpenza T Jr, Goto J, Marlier A, Moreno-De-Luca A, Yu X, Butler WE, Carter BS, Lake EMR, Constable RT, Rakic P, Lin H, Deniz E, Benveniste H, Malvankar NS, Estrada-Veras JI, Walsh CA, Alper SL, Schultze JL, Paeschke K, Doetzlhofer A, Wulczyn FG, Jin SC, Lifton RP, Sestan N, Kolanus W, Kahle KT. Impaired neurogenesis alters brain biomechanics in a neuroprogenitor-based genetic subtype of congenital hydrocephalus. Nat Neurosci. 2022;25:458–73.
A.K. Singh, G. Allington, S. Viviano, S. McGee, E. Kiziltug, S. Ma, S. Zhao, K.Y. Mekbib, J.P. Shohfi, P.Q. Duy, T. DeSpenza, Jr., C.G. Furey, B.C. Reeves, H. Smith, A.M.M. Sousa, A. Cherskov, A. Allocco, C. Nelson-Williams, S. Haider, S.R.A. Rizvi, S.L. Alper, N. Sestan, H. Shimelis, L.K. Walsh, R.P. Lifton, A. Moreno-De-Luca, S.C. Jin, P. Kruszka, E. Deniz, and K.T. Kahle, A novel SMARCC1 BAFopathy implicates neural progenitor epigenetic dysregulation in human hydrocephalus. Brain (2023).
Scott CE, Wynn SL, Sesay A, Cruz C, Cheung M, Gomez-Gaviro MV, Booth S, Gao B, Cheah KS, Lovell-Badge R, Briscoe J. SOX9 induces and maintains neural stem cells. Nat Neurosci. 2010;13:1181–9.
Luo R, Jeong SJ, Jin Z, Strokes N, Li S, Piao X. G protein-coupled receptor 56 and collagen III, a receptor-ligand pair, regulates cortical development and lamination. Proc Natl Acad Sci USA. 2011;108:12925–30.
Morin X, Jaouen F, Durbec P. Control of planar divisions by the G-protein regulator LGN maintains progenitors in the chick neuroepithelium. Nat Neurosci. 2007;10:1440–8.
Cesca F, Yabe A, Spencer-Dene B, Scholz-Starke J, Medrihan L, Maden CH, Gerhardt H, Orriss IR, Baldelli P, Al-Qatari M, Koltzenburg M, Adams RH, Benfenati F, Schiavo G. Kidins220/ARMS mediates the integration of the neurotrophin and VEGF pathways in the vascular and nervous systems. Cell Death Differ. 2012;19:194–208.
Duy PQ, Rakic P, Alper SL, Robert SM, Kundishora AJ, Butler WE, Walsh CA, Sestan N, Geschwind DH, Jin SC, Kahle KT. A neural stem cell paradigm of pediatric hydrocephalus. Cerebral Cortex. 2023;33:4262–79.
Duy PQ, Rakic P, Alper SL, Butler WE, Walsh CA, Sestan N, Geschwind DH, Jin SC, Kahle KT. Brain ventricles as windows into brain development and disease. Neuron. 2022;110:12–5.
Duy PQ, Mehta NH, Kahle KT. The “microcephalic hydrocephalus” paradox as a paradigm of altered neural stem cell biology. Cerebral Cortex. 2024;34:1.
Duy PQ, Kahle KT. “Floppy brain” in congenital hydrocephalus. Cerebral Cortex. 2023;33:9339–42.
Kinsler VA, Thomas AC, Ishida M, Bulstrode NW, Loughlin S, Hing S, Chalker J, McKenzie K, Abu-Amero S, Slater O, Chanudet E, Palmer R, Morrogh D, Stanier P, Healy E, Sebire NJ, Moore GE. Multiple congenital melanocytic nevi and neurocutaneous melanosis are caused by postzygotic mutations in codon 61 of NRAS. J Invest Dermatol. 2013;133:2229–36.
Jagannathan J, Lonser RR, Smith R, DeVroom HL, Oldfield EH. Surgical management of cerebellar hemangioblastomas in patients with von Hippel-Lindau disease. J Neurosurg. 2008;108:210–22.
Reichert SC, Zelley K, Nichols KE, Eberhard M, Zackai EH, Martinez-Poyer J. Diagnosis of 9q22.3 microdeletion syndrome in utero following identification of craniosynostosis, overgrowth, and skeletal anomalies. Am J Med Genet A. 2015;167:862–5.
Shimkets R, Gailani MR, Siu VM, Yang-Feng T, Pressman CL, Levanat S, Goldstein A, Dean M, Bale AE. Molecular analysis of chromosome 9q deletions in two Gorlin syndrome patients. Am J Hum Genet. 1996;59:417–22.
Pastorino L, Ghiorzo P, Nasti S, Battistuzzi L, Cusano R, Marzocchi C, Garrè ML, Clementi M, Scarrà GB. Identification of a SUFU germline mutation in a family with Gorlin syndrome. Am J Med Genet A. 2009;149:1539–43.
Taylor MD, Liu L, Raffel C, Hui CC, Mainprize TG, Zhang X, Agatep R, Chiappa S, Gao L, Lowrance A, Hao A, Goldstein AM, Stavrou T, Scherer SW, Dura WT, Wainwright B, Squire JA, Rutka JT, Hogg D. Mutations in SUFU predispose to medulloblastoma. Nat Genet. 2002;31:306–10.
Doherty D, Parisi MA, Finn LS, Gunay-Aygun M, Al-Mateen M, Bates D, Clericuzio C, Demir H, Dorschner M, van Essen AJ, Gahl WA, Gentile M, Gorden NT, Hikida A, Knutzen D, Ozyurek H, Phelps I, Rosenthal P, Verloes A, Weigand H, Chance PF, Dobyns WB, Glass IA. Mutations in 3 genes (MKS3, CC2D2A and RPGRIP1L) cause COACH syndrome (Joubert syndrome with congenital hepatic fibrosis). J Med Genet. 2010;47:8–21.
Gupta GD, Coyaud É, Gonçalves J, Mojarad BA, Liu Y, Wu Q, Gheiratmand L, Comartin D, Tkach JM, Cheung SW, Bashkurov M, Hasegan M, Knight JD, Lin ZY, Schueler M, Hildebrandt F, Moffat J, Gingras AC, Raught B, Pelletier L. A dynamic protein interaction landscape of the human centrosome-cilium interface. Cell. 2015;163:1484–99.
Ekici AB, Hilfinger D, Jatzwauk M, Thiel CT, Wenzel D, Lorenz I, Boltshauser E, Goecke TW, Staatz G, Morris-Rosendahl DJ, Sticht H, Hehr U, Reis A, Rauch A. Disturbed Wnt signalling due to a Mutation in CCDC88C causes an autosomal recessive non-syndromic hydrocephalus with medial diverticulum. Mol Syndromol. 2010;1:99–112.
Enomoto A, Ping J, Takahashi M. Girdin, a novel actin-binding protein, and its family of proteins possess versatile functions in the Akt and Wnt signaling pathways. Ann N Y Acad Sci. 2006;1086:169–84.
Logan CY, Nusse R. The Wnt signaling pathway in development and disease. Annu Rev Cell Dev Biol. 2004;20:781–810.
Cheng H, Dufu K, Lee CS, Hsu JL, Dias A, Reed R. Human mRNA export machinery recruited to the 5’ end of mRNA. Cell. 2006;127:1389–400.
Zhang Q, Chen S, Qin Z, Zheng H, Fan X. The first reported case of Beaulieu-Boycott-Innes syndrome caused by two novel mutations in THOC6 gene in a Chinese infant. Medicine (Baltimore). 2020;99: e19751.
Mattioli F, Isidor B, Abdul-Rahman O, Gunter A, Huang L, Kumar R, Beaulieu C, Gecz J, Innes M, Mandel JL, Piton A. Clinical and functional characterization of recurrent missense variants implicated in THOC6-related intellectual disability. Hum Mol Genet. 2019;28:952–60.
Mee L, Honkala H, Kopra O, Vesa J, Finnilä S, Visapää I, Sang TK, Jackson GR, Salonen R, Kestilä M, Peltonen L. Hydrolethalus syndrome is caused by a missense mutation in a novel gene HYLS1. Hum Mol Genet. 2005;14:1475–88.
Jenkinson EM, Rodero MP, Kasher PR, Uggenti C, Oojageer A, Goosey LC, Rose Y, Kershaw CJ, Urquhart JE, Williams SG, Bhaskar SS, O’Sullivan J, Baerlocher GM, Haubitz M, Aubert G, Barañano KW, Barnicoat AJ, Battini R, Berger A, Blair EM, Brunstrom-Hernandez JE, Buckard JA, Cassiman DM, Caumes R, Cordelli DM, De Waele LM, Fay AJ, Ferreira P, Fletcher NA, Fryer AE, Goel H, Hemingway CA, Henneke M, Hughes I, Jefferson RJ, Kumar R, Lagae L, Landrieu PG, Lourenço CM, Malpas TJ, Mehta SG, Metz I, Naidu S, Õunap K, Panzer A, Prabhakar P, Quaghebeur G, Schiffmann R, Sherr EH, Sinnathuray KR, Soh C, Stewart HS, Stone J, Van Esch H, Van Mol CE, Vanderver A, Wakeling EL, Whitney A, Pavitt GD, Griffiths-Jones S, Rice GI, Revy P, van der Knaap MS, Livingston JH, O’Keefe RT, Crow YJ. Mutations in SNORD118 cause the cerebral microangiopathy leukoencephalopathy with calcifications and cysts. Nat Genet. 2016;48:1185–92.
Hishimura N, Watari M, Ohata H, Fuseya N, Wakiguchi S, Tokutomi T, Okuhara K, Takahashi N, Iizuka S, Yamamoto H, Mishima T, Fujieda S, Kobayashi R, Cho K, Kuroda Y, Kurosawa K, Tonoki H. Genetic and prenatal findings in two Japanese patients with Schinzel-Giedion syndrome. Clin Case Rep. 2017;5:5–8.
Wang X, Lee RS, Alver BH, Haswell JR, Wang S, Mieczkowski J, Drier Y, Gillespie SM, Archer TC, Wu JN. SMARCB1-mediated SWI/SNF complex function is essential for enhancer regulation. Nat Genet. 2017;49:289–95.
Sienski G, Dönertas D, Brennecke J. Transcriptional silencing of transposons by Piwi and maelstrom and its impact on chromatin state and gene expression. Cell. 2012;151:964–80.
Domínguez-Pinos MD, Páez P, Jiménez AJ, Weil B, Arráez MA, Pérez-Fígares JM, Rodríguez EM. Ependymal denudation and alterations of the subventricular zone occur in human fetuses with a moderate communicating hydrocephalus. J Neuropathol Exp Neurol. 2005;64:595–604.
Li X, Kong H, Wu W, Xiao M, Sun X, Hu G. Aquaporin-4 maintains ependymal integrity in adult mice. Neuroscience. 2009;162:67–77.
Meyer E, Ricketts C, Morgan NV, Morris MR, Pasha S, Tee LJ, Rahman F, Bazin A, Bessières B, Déchelotte P, Yacoubi MT, Al-Adnani M, Marton T, Tannahill D, Trembath RC, Fallet-Bianco C, Cox P, Williams D, Maher ER. Mutations in FLVCR2 are associated with proliferative vasculopathy and hydranencephaly-hydrocephaly syndrome (Fowler syndrome). Am J Hum Genet. 2010;86:471–8.
Pao SS, Paulsen IT, Saier MH Jr. Major facilitator superfamily. Microbiol Mol Biol Rev. 1998;62:1–34.
Kato T, Sato H, Emi M, Seino T, Arawaka S, Iseki C, Takahashi Y, Wada M, Kawanami T. Segmental copy number loss of SFMBT1 gene in elderly individuals with ventriculomegaly: a community-based study. Intern Med. 2011;50:297–303.
Kim JK, Huh SO, Choi H, Lee KS, Shin D, Lee C, Nam JS, Kim H, Chung H, Lee HW, Park SD, Seong RH. Srg3, a mouse homolog of yeast SWI3, is essential for early embryogenesis and involved in brain development. Mol Cell Biol. 2001;21:7787–95.
Sato H, Takahashi Y, Kimihira L, Iseki C, Kato H, Suzuki Y, Igari R, Sato H, Koyama S, Arawaka S, Kawanami T, Miyajima M, Samejima N, Sato S, Kameda M, Yamada S, Kita D, Kaijima M, Date I, Sonoda Y, Kayama T, Kuwana N, Arai H, Kato T. A segmental copy number loss of the SFMBT1 gene is a genetic risk for shunt-responsive, Idiopathic Normal Pressure Hydrocephalus (iNPH): a case-control study. PLoS ONE. 2016;11: e0166615.
Yang HW, Lee S, Yang D, Dai H, Zhang Y, Han L, Zhao S, Zhang S, Ma Y, Johnson MF, Rattray AK, Johnson TA, Wang G, Zheng S, Carroll RS, Park PJ, Johnson MD. Deletions in CWH43 cause idiopathic normal pressure hydrocephalus. EMBO Mol Med. 2021;13: e13249.
Abdulhag UN, Soiferman D, Schueler-Furman O, Miller C, Shaag A, Elpeleg O, Edvardson S, Saada A. Mitochondrial complex IV deficiency, caused by mutated COX6B1, is associated with encephalomyopathy, hydrocephalus and cardiomyopathy. Eur J Human Genetics. 2015;23:159–64.
Sheftel AD, Wilbrecht C, Stehling O, Niggemeyer B, Elsässer HP, Mühlenhoff U, Lill R. The human mitochondrial ISCA1, ISCA2, and IBA57 proteins are required for [4Fe-4S] protein maturation. Mol Biol Cell. 2012;23:1157–66.
Schlotawa L, Ennemann EC, Radhakrishnan K, Schmidt B, Chakrapani A, Christen HJ, Moser H, Steinmann B, Dierks T, Gärtner J. SUMF1 mutations affecting stability and activity of formylglycine generating enzyme predict clinical outcome in multiple sulfatase deficiency. Eur J Human Genetics. 2011;19:253–61.
Cizmeci MN, Akelma AZ, Kosehan D, Kutukoglu I, Sonmez FM. Multiloculated hydrocephalus of intrauterine-onset: a case report of an unexpected MTHFR A1298C positive test result. Genet Couns. 2013;24:265–71.
Barisic M, Sohm B, Mikolcevic P, Wandke C, Rauch V, Ringer T, Hess M, Bonn G, Geley S. Spindly/CCDC99 is required for efficient chromosome congression and mitotic checkpoint regulation. Mol Biol Cell. 2010;21:1968–81.
Khodiyar VK, Maltais LJ, Ruef BJ, Sneddon KM, Smith JR, Shimoyama M, Cabral F, Dumontet C, Dutcher SK, Harvey RJ, Lafanechère L, Murray JM, Nogales E, Piquemal D, Stanchi F, Povey S, Lovering RC. A revised nomenclature for the human and rodent alpha-tubulin gene family. Genomics. 2007;90:285–9.
Paushkin SV, Patel M, Furia BS, Peltz SW, Trotta CR. Identification of a human endonuclease complex reveals a link between tRNA splicing and pre-mRNA 3’ end formation. Cell. 2004;117:311–21.
Pacholsky D, Vakeel P, Himmel M, Löwe T, Stradal T, Rottner K, Fürst DO, van der Ven PF. Xin repeats define a novel actin-binding motif. J Cell Sci. 2004;117:5257–68.
Qi HH, Ongusaha PP, Myllyharju J, Cheng D, Pakkanen O, Shi Y, Lee SW, Peng J, Shi Y. Prolyl 4-hydroxylation regulates Argonaute 2 stability. Nature. 2008;455:421–4.
Khuong TM, Habets RL, Slabbaert JR, Verstreken P. WASP is activated by phosphatidylinositol-4,5-bisphosphate to restrict synapse growth in a pathway parallel to bone morphogenetic protein signaling. Proc Natl Acad Sci USA. 2010;107:17379–84.
Beutler E. Gaucher disease: new molecular approaches to diagnosis and treatment. Science. 1992;256:794–9.
Sullivan W, Reeves BC, Duy PQ, Nelson-Williams C, Dong W, Jin SC, Kahle KT. Exome sequencing as a potential diagnostic adjunct in sporadic congenital hydrocephalus. JAMA Pediatr. 2021;175:310–3.
Alazami AM, Maddirevula S, Seidahmed MZ, Albhlal LA, Alkuraya FS. A novel ISLR2-linked autosomal recessive syndrome of congenital hydrocephalus, arthrogryposis and abdominal distension. Hum Genet. 2019;138:105–7.
Allocco AA, Jin SC, Duy PQ, Furey CG, Zeng X, Dong W, Nelson-Williams C, Karimy JK, DeSpenza T, Hao LT, Reeves B, Haider S, Gunel M, Lifton RP, Kahle KT. Recessive inheritance of congenital hydrocephalus with other structural brain abnormalities caused by compound heterozygous mutations in ATP1A3. Front Cell Neurosci. 2019;13:425.
Chassaing N, Gilbert-Dussardier B, Nicot F, Fermeaux V, Encha-Razavi F, Fiorenza M, Toutain A, Calvas P. Germinal mosaicism and familial recurrence of a SOX2 mutation with highly variable phenotypic expression extending from AEG syndrome to absence of ocular involvement. Am J Med Genet A. 2007;143:289–91.
Cox PM, Gibson RA, Morgan N, Brueton LA. VACTERL with hydrocephalus in twins due to Fanconi anemia (FA): mutation in the FAC gene. Am J Med Genet. 1997;68:86–90.
De Keersmaecker B, Van Esch H, Van Schoubroeck D, Claus F, Moerman P, De Catte L. Prenatal diagnosis of MPPH syndrome. Prenat Diagn. 2013;33:292–5.
Escobar LF, Hiett AK, Marnocha A. Significant phenotypic variability of Muenke syndrome in identical twins. Am J Med Genet A. 2009;149:1273–6.
Gomy I, Heck B, Santos AC, Figueiredo MS, Martinelli CE Jr, Nogueira MP, Pina-Neto JM. Two new Brazilian patients with Gómez-López-Hernández syndrome: reviewing the expanded phenotype with molecular insights. Am J Med Genet A. 2008;146:649–57.
Isik E, Onay H, Atik T, Akgun B, Cogulu O, Ozkinay F. Clinical and genetic features of L1 syndrome patients: Definition of two novel mutations. Clin Neurol Neurosurg. 2018;172:20–3.
Jin SC, Furey CG, Zeng X, Allocco A, Nelson-Williams C, Dong W, Karimy JK, Wang K, Ma S, Delpire E, Kahle KT. SLC12A ion transporter mutations in sporadic and familial human congenital hydrocephalus. Mol Genet Genomic Med. 2019;7: e892.
Jouet M, Feldman E, Yates J, Donnai D, Paterson J, Siggers D, Kenwrick S. Refining the genetic location of the gene for X linked hydrocephalus within Xq28. J Med Genet. 1993;30:214–7.
Khattab M, Xu F, Li P, Bhandari V. A de novo 3.54 Mb deletion of 17q22-q23.1 associated with hydrocephalus: a case report and review of literature. Am J Med Genet A. 2011;155:3082–6.
Lamont RE, Tan WH, Innes AM, Parboosingh JS, Schneidman-Duhovny D, Rajkovic A, Pappas J, Altschwager P, DeWard S, Fulton A, Gray KJ, Krall M, Mehta L, Rodan LH, Saller DN Jr, Steele D, Stein D, Yatsenko SA, Bernier FP, Slavotinek AM. Expansion of phenotype and genotypic data in CRB2-related syndrome. Eur J Human Genet. 2016;24:1436–44.
Lyonnet S, Pelet A, Royer G, Delrieu O, Serville F, le Marec B, Gruensteudel A, Pfeiffer RA, Briard ML, Dubay C, et al. The gene for X-linked hydrocephalus maps to Xq28, distal to DXS52. Genomics. 1992;14:508–10.
Maurya MR, Ravi R, Pungavkar SA. A case report of Arnold Chiari type 1 malformation in acromesomelic dwarf infant. Pan Afr Med J. 2021;38:58.
Porayette P, Fruitman D, Lauzon JL, Le Goff C, Cormier-Daire V, Sanders SP, Pinto-Rojas A, Perez-Atayde AR. Novel mutations in geleophysic dysplasia type 1. Pediatr Dev Pathol. 2014;17:209–16.
Serville F, Benit P, Saugier P, Vibert M, Royer G, Pelet A, Chery M, Munnich A, Lyonnet S. Prenatal exclusion of X-linked hydrocephalus-stenosis of the aqueduct of Sylvius sequence using closely linked DNA markers. Prenat Diagn. 1993;13:435–9.
Strain L, Gosden CM, Brock DJ, Bonthron DT. Genetic heterogeneity in X-linked hydrocephalus: linkage to markers within Xq273. Am J Hum Genet. 1994;54:236–43.
Tzschach A, Grasshoff U, Schäferhoff K, Bonin M, Dufke A, Wolff M, Haas-Lude K, Bevot A, Riess O. Interstitial 9q34.11-q34.13 deletion in a patient with severe intellectual disability, hydrocephalus, and cleft lip/palate. Am J Med Genet A. 2012;158:1709–12.
Verbeek E, Meuwissen ME, Verheijen FW, Govaert PP, Licht DJ, Kuo DS, Poulton CJ, Schot R, Lequin MH, Dudink J, Halley DJ, de Coo RI, den Hollander JC, Oegema R, Gould DB, Mancini GM. COL4A2 mutation associated with familial porencephaly and small-vessel disease. Eur J Human Genet. 2012;20:844–51.
Vieira JP, Lopes P, Silva R. Primary ciliary dyskinesia and hydrocephalus with aqueductal stenosis. J Child Neurol. 2012;27:938–41.
Alhousseini A, Zeineddine S, Husseini A, Baddah H, Saker H, Mody S, Ibrahim SA, Thakur M, Hernandez-Andrade E, Bahado-Singh R. Familial Hydrocephalus and Dysgenesis of the Corpus Callosum Associated with Xp22.33 Duplication and Stenosis of the Aqueduct of Sylvius with X-Linked Recessive Inheritance Pattern. Gynecol Obstet Invest. 2019;84:412–6.
Beggs AH, Neumann PE, Arahata K, Arikawa E, Nonaka I, Anderson MS, Kunkel LM. Possible influences on the expression of X chromosome-linked dystrophin abnormalities by heterozygosity for autosomal recessive Fukuyama congenital muscular dystrophy. Proc Natl Acad Sci USA. 1992;89:623–7.
Cacciagli P, Desvignes JP, Girard N, Delepine M, Zelenika D, Lathrop M, Lévy N, Ledbetter DH, Dobyns WB, Villard L. AP1S2 is mutated in X-linked Dandy-Walker malformation with intellectual disability, basal ganglia disease and seizures (Pettigrew syndrome). Eur J Human Genet. 2014;22:363–8.
Chassaing N, Siani V, Carles D, Delezoide AL, Alberti EM, Battin J, Chateil JF, Gilbert-Dussardier B, Coupry I, Arveiler B, Saura R, Lacombe D. X-linked dominant chondrodysplasia with platyspondyly, distinctive brachydactyly, hydrocephaly, and microphthalmia. Am J Med Genet A. 2005;136:307–12.
Furtado LV, Bayrak-Toydemir P, Hulinsky B, Damjanovich K, Carey JC, Rope AF. A novel X-linked multiple congenital anomaly syndrome associated with an EBP mutation. Am J Med Genet A. 2010;152:2838–44.
Holden ST, Cox JJ, Kesterton I, Thomas NS, Carr C, Woods CG. Fanconi anaemia complementation group B presenting as X linked VACTERL with hydrocephalus syndrome. J Med Genet. 2006;43:750–4.
Jouet M, Moncla A, Paterson J, McKeown C, Fryer A, Carpenter N, Holmberg E, Wadelius C, Kenwrick S. New domains of neural cell-adhesion molecule L1 implicated in X-linked hydrocephalus and MASA syndrome. Am J Hum Genet. 1995;56:1304–14.
Kaepernick L, Legius E, Higgins J, Kapur S. Clinical aspects of the MASA syndrome in a large family, including expressing females. Clin Genet. 1994;45:181–5.
Kenwrick S, Ionasescu V, Ionasescu G, Searby C, King A, Dubowitz M, Davies KE. Linkage studies of X-linked recessive spastic paraplegia using DNA probes. Hum Genet. 1986;73:264–6.
Ko TM, Hwa HL, Tseng LH, Hsieh FJ, Huang SF, Lee TY. Prenatal diagnosis of X-linked hydrocephalus in a Chinese family with four successive affected pregnancies. Prenat Diagn. 1994;14:57–60.
Kolanczyk M, Krawitz P, Hecht J, Hupalowska A, Miaczynska M, Marschner K, Schlack C, Emmerich D, Kobus K, Kornak U, Robinson PN, Plecko B, Grangl G, Uhrig S, Mundlos S, Horn D. Missense variant in CCDC22 causes X-linked recessive intellectual disability with features of Ritscher-Schinzel/3C syndrome. Eur J Human Genet. 2015;23:720.
Kroes HY, Nievelstein RJ, Barth PG, Nikkels PG, Bergmann C, Gooskens RH, Visser G, van Amstel HK, Beemer FA. Cerebral, cerebellar, and colobomatous anomalies in three related males: Sex-linked inheritance in a newly recognized syndrome with features overlapping with Joubert syndrome. Am J Med Genet A. 2005;135:297–301.
Legius E, Kaepernick L, Higgins JV, Glover TW. Fine mapping of X-linked clasped thumb and mental retardation (MASA syndrome) in Xq28. Clin Genet. 1994;45:165–8.
McCauley J, Masand N, McGowan R, Rajagopalan S, Hunter A, Michaud JL, Gibson K, Robertson J, Vaz F, Abbs S, Holden ST. X-linked VACTERL with hydrocephalus syndrome: further delineation of the phenotype caused by FANCB mutations. Am J Med Genet A. 2011;155:2370–80.
Mikat B, Roll C, Schindler D, Gembruch U, Klempert I, Buiting K, Bramswig NC, Wieczorek D. X-linked recessive VACTERL-H due to a mutation in FANCB in a preterm boy. Clin Dysmorphol. 2016;25:73–6.
Rietschel M, Friedl W, Uhlhaas S, Neugebauer M, Heimann D, Zerres K. MASA syndrome: clinical variability and linkage analysis. Am J Med Genet. 1991;41:10–4.
Rosenthal A, Jouet M, Kenwrick S. Aberrant splicing of neural cell adhesion molecule L1 mRNA in a family with X-linked hydrocephalus. Nat Genet. 1992;2:107–12.
Schrander-Stumpel C, Legius E, Fryns JP, Cassiman JJ. MASA syndrome: new clinical features and linkage analysis using DNA probes. J Med Genet. 1990;27:688–92.
Serville F, Lyonnet S, Pelet A, Reynaud M, Louail C, Munnich A, Le Merrer M. X-linked hydrocephalus: clinical heterogeneity at a single gene locus. Eur J Pediatr. 1992;151:515–8.
Sheen VL, Basel-Vanagaite L, Goodman JR, Scheffer IE, Bodell A, Ganesh VS, Ravenscroft R, Hill RS, Cherry TJ, Shugart YY, Barkovich J, Straussberg R, Walsh CA. Etiological heterogeneity of familial periventricular heterotopia and hydrocephalus. Brain Develop. 2004;26:326–34.
Simon D, Laloo B, Barillot M, Barnetche T, Blanchard C, Rooryck C, Marche M, Burgelin I, Coupry I, Chassaing N, Gilbert-Dussardier B, Lacombe D, Grosset C, Arveiler B. A mutation in the 3’-UTR of the HDAC6 gene abolishing the post-transcriptional regulation mediated by hsa-miR-433 is linked to a new form of dominant X-linked chondrodysplasia. Hum Mol Genet. 2010;19:2015–27.
Tripolszki K, Sasaki E, Hotakainen R, Kassim AH, Pereira C, Rolfs A, Bauer P, Reardon W, Bertoli-Avella AM. An X-linked syndrome with severe neurodevelopmental delay, hydrocephalus, and early lethality caused by a missense variation in the OTUD5 gene. Clin Genet. 2021;99:303–8.
Watanabe N, Tsutsumi S, Miyano Y, Sato H, Nagase S. X-linked VACTERL-H caused by deletion of exon 3 in FANCB: A case report. Congenit Anom (Kyoto). 2018;58:171–2.
Willems PJ, Dijkstra I, Van der Auwera BJ, Vits L, Coucke P, Raeymaekers P, Van Broeckhoven C, Consalez GG, Freeman SB, Warren ST, et al. Assignment of X-linked hydrocephalus to Xq28 by linkage analysis. Genomics. 1990;8:367–70.
Willems PJ, Vits L, Raeymaekers P, Beuten J, Coucke P, Holden JJ, Van Broeckhoven C, Warren ST, Sagi M, Robinson D, et al. Further localization of X-linked hydrocephalus in the chromosomal region Xq28. Am J Hum Genet. 1992;51:307–15.
Bott L, Boute O, Mention K, Vinchon M, Boman F, Gottrand F. Congenital idiopathic intestinal pseudo-obstruction and hydrocephalus with stenosis of the aqueduct of sylvius. Am J Med Genet A. 2004;130:84–7.
Brewer CM, Fredericks BJ, Pont JM, Stephenson JB, Tolmie JL. X-linked hydrocephalus masquerading as spina bifida and destructive porencephaly in successive generations in one family. Dev Med Child Neurol. 1996;38:632–6.
Chidsey BA, Baldwin EE, Toydemir R, Ahles L, Hanson H, Stevenson DA. L1CAM whole gene deletion in a child with L1 syndrome. Am J Med Genet A. 2014;164:1555–8.
Claes S, Aguirre T, Simosa V, Bustos T, Lander R, Piras M, Legius E, Cassiman JJ, Raeymaekers P. Hydrocephalus and spastic paraplegia result from a donor splice site mutation (2872 + 1G to A) in the L1CAM gene in a Venezuelan pedigree. Hum Mutat Suppl. 1998;1:S240–1.
Coucke P, Vits L, Van Camp G, Serville F, Lyonnet S, Kenwrick S, Rosenthal A, Wehnert M, Munnich A, Willems PJ. Identification of a 5’ splice site mutation in intron 4 of the L1CAM gene in an X-linked hydrocephalus family. Hum Mol Genet. 1994;3:671–3.
Du YZ, Dickerson C, Aylsworth AS, Schwartz CE. A silent mutation, C924T (G308G), in the L1CAM gene results in X linked hydrocephalus (HSAS). J Med Genet. 1998;35:456–62.
Du YZ, Srivastava AK, Schwartz CE. Multiple exon screening using restriction endonuclease fingerprinting (REF): detection of six novel mutations in the L1 cell adhesion molecule (L1CAM) gene. Hum Mutat. 1998;11:222–30.
Du JS, Bason L, Woffendin H, Zackai E, Kenwrick S. Somatic and germ line mosaicism and mutation origin for a mutation in the L1 gene in a family with X-linked hydrocephalus. Am J Med Genet. 1998;75:200–2.
Ferese R, Zampatti S, Griguoli AM, Fornai F, Giardina E, Barrano G, Albano V, Campopiano R, Scala S, Novelli G, Gambardella S. A new splicing mutation in the L1CAM gene responsible for X-linked hydrocephalus (HSAS). J Mol Neurosci. 2016;59:376–81.
Fernández RM, Núñez-Torres R, García-Díaz L, de Agustín JC, Antiñolo G, Borrego S. Association of X-linked hydrocephalus and Hirschsprung disease: report of a new patient with a mutation in the L1CAM gene. Am J Med Genet A. 2012;158:816–20.
Finckh U, Schröder J, Ressler B, Veske A, Gal A. Spectrum and detection rate of L1CAM mutations in isolated and familial cases with clinically suspected L1-disease. Am J Med Genet. 2000;92:40–6.
Fransen E, Schrander-Stumpel C, Vits L, Coucke P, Van Camp G, Willems PJ. X-linked hydrocephalus and MASA syndrome present in one family are due to a single missense mutation in exon 28 of the L1CAM gene. Hum Mol Genet. 1994;3:2255–6.
Gigarel N, Frydman N, Burlet P, Kerbrat V, Steffann J, Frydman R, Munnich A, Ray PF. Single cell co-amplification of polymorphic markers for the indirect preimplantation genetic diagnosis of hemophilia A, X-linked adrenoleukodystrophy, X-linked hydrocephalus and incontinentia pigmenti loci on Xq28. Hum Genet. 2004;114:298–305.
Graf WD, Born DE, Shaw DW, Thomas JR, Holloway LW, Michaelis RC. Diffusion-weighted magnetic resonance imaging in boys with neural cell adhesion molecule L1 mutations and congenital hydrocephalus. Ann Neurol. 2000;47:113–7.
Gregory LC, Shah P, Sanner JRF, Arancibia M, Hurst J, Jones WD, Spoudeas H, Stabej P, Williams HJ, Ocaka LA, Loureiro C, Martinez-Aguayo A, Dattani MT. Mutations in MAGEL2 and L1CAM are associated with congenital hypopituitarism and arthrogryposis. J Clin Endocrinol Metab. 2019;104:5737–50.
Griseri P, Vos Y, Giorda R, Gimelli S, Beri S, Santamaria G, Mognato G, Hofstra RM, Gimelli G, Ceccherini I. Complex pathogenesis of Hirschsprung’s disease in a patient with hydrocephalus, vesico-ureteral reflux and a balanced translocation t(3;17)(p12;q11). Eur J Human Genet. 2009;17:483–90.
Gu SM, Orth U, Veske A, Enders H, Klunder K, Schlosser M, Engel W, Schwinger E, Gal A. Five novel mutations in the L1CAM gene in families with X linked hydrocephalus. J Med Genet. 1996;33:103–6.
Guo D, Shi Y, Jian W, Fu Y, Yang H, Guo M, Yong W, Chen G, Deng H, Qin Y, Liao W, Yao R. A novel nonsense mutation in the L1CAM gene responsible for X-linked congenital hydrocephalus. J Gene Med. 2020;22: e3180.
Hübner CA, Utermann B, Tinschert S, Krüger G, Ressler B, Steglich C, Schinzel A, Gal A. Intronic mutations in the L1CAM gene may cause X-linked hydrocephalus by aberrant splicing. Hum Mutat. 2004;23:526.
Jouet M, Kenwrick S. Gene analysis of L1 neural cell adhesion molecule in prenatal diagnosis of hydrocephalus. Lancet. 1995;345:161–2.
Jouet M, Strain L, Bonthron D, Kenwrick S. Discordant segregation of Xq28 markers and a mutation in the L1 gene in a family with X linked hydrocephalus. J Med Genet. 1996;33:248–50.
Kanemura Y, Okamoto N, Sakamoto H, Shofuda T, Kamiguchi H, Yamasaki M. Molecular mechanisms and neuroimaging criteria for severe L1 syndrome with X-linked hydrocephalus. J Neurosurg. 2006;105:403–12.
Kong W, Wang X, Zhao J, Kang M, Xi N, Li S. A new frameshift mutation in L1CAM producing X-linked hydrocephalus. Mol Genet Genomic Med. 2020;8: e1031.
Liebau MC, Gal A, Superti-Furga A, Omran H, Pohl M. L1CAM mutation in a boy with hydrocephalus and duplex kidneys. Pediatr Nephrol. 2007;22:1058–61.
Limbrick DD Jr, Baksh B, Morgan CD, Habiyaremye G, McAllister JP 2nd, Inder TE, Mercer D, Holtzman DM, Strahle J, Wallendorf MJ, Morales DM. Cerebrospinal fluid biomarkers of infantile congenital hydrocephalus. PLoS ONE. 2017;12: e0172353.
MacFarlane JR, Du JS, Pepys ME, Ramsden S, Donnai D, Charlton R, Garrett C, Tolmie J, Yates JR, Berry C, Goudie D, Moncla A, Lunt P, Hodgson S, Jouet M, Kenwrick S. Nine novel L1 CAM mutations in families with X-linked hydrocephalus. Hum Mutat. 1997;9:512–8.
Marín R, Ley-Martos M, Gutiérrez G, Rodríguez-Sánchez F, Arroyo D, Mora-López F. Three cases with L1 syndrome and two novel mutations in the L1CAM gene. Eur J Pediatr. 2015;174:1541–4.
Marx M, Diestel S, Bozon M, Keglowich L, Drouot N, Bouché E, Frebourg T, Minz M, Saugier-Veber P, Castellani V, Schäfer MK. Pathomechanistic characterization of two exonic L1CAM variants located in trans in an obligate carrier of X-linked hydrocephalus. Neurogenetics. 2012;13:49–59.
Michaelis RC, Du YZ, Schwartz CE. The site of a missense mutation in the extracellular Ig or FN domains of L1CAM influences infant mortality and the severity of X linked hydrocephalus. J Med Genet. 1998;35:901–4.
Nakakimura S, Sasaki F, Okada T, Arisue A, Cho K, Yoshino M, Kanemura Y, Yamasaki M, Todo S. Hirschsprung’s disease, acrocallosal syndrome, and congenital hydrocephalus: report of 2 patients and literature review. J Pediatr Surg. 2008;43:E13–7.
Okamoto N, Wada Y, Goto M. Hydrocephalus and Hirschsprung’s disease in a patient with a mutation of L1CAM. J Med Genet. 1997;34:670–1.
Okamoto N, Del Maestro R, Valero R, Monros E, Poo P, Kanemura Y, Yamasaki M. Hydrocephalus and Hirschsprung’s disease with a mutation of L1CAM. J Hum Genet. 2004;49:334–7.
Panayi M, Gokhale D, Mansour S, Elles R. Prenatal diagnosis in a family with X-linked hydrocephalus. Prenat Diagn. 2005;25:930–3.
Parisi MA, Kapur RP, Neilson I, Hofstra RM, Holloway LW, Michaelis RC, Leppig KA. Hydrocephalus and intestinal aganglionosis: is L1CAM a modifier gene in Hirschsprung disease? Am J Med Genet. 2002;108:51–6.
Pomili G, Venti-Donti G, Alunni-Carrozza L, Ardisia C, Servidio F, Hofstra RM, Gilardi G, Donti E. MASA syndrome: ultrasonographic evidence in a male fetus. Prenat Diagn. 2000;20:1012–4.
Rehnberg M, Jonasson J, Gunnarsson C. Novel L1CAM splice site mutation in a young male with L1 syndrome. Am J Med Genet A. 2011;155:439–41.
G. Rodríguez-Criado, A. Pérez-Aytés, F. Martínez, Y.J. Vos, E. Verlind, A. González-Meneses López, I. Sánchez, and C. Schrander-Stumpel. X-linked hydrocephalus: another two families with an L1 mutation. Genet Couns 14 (2003) 57–65.
Ruiz JC, Cuppens H, Legius E, Fryns JP, Glover T, Marynen P, Cassiman JJ. Mutations in L1-CAM in two families with X linked complicated spastic paraplegia, MASA syndrome, and HSAS. J Med Genet. 1995;32:549–52.
Saugier-Veber P, Martin C, Le Meur N, Lyonnet S, Munnich A, David A, Hénocq A, Héron D, Jonveaux P, Odent S, Manouvrier S, Moncla A, Morichon N, Philip N, Satge D, Tosi M, Frébourg T. Identification of novel L1CAM mutations using fluorescence-assisted mismatch analysis. Hum Mutat. 1998;12:259–66.
Senat MV, Bernard JP, Delezoide A, Saugier-Veber P, Hillion Y, Roume J, Ville Y. Prenatal diagnosis of hydrocephalus-stenosis of the aqueduct of Sylvius by ultrasound in the first trimester of pregnancy Report of two cases. Prenat Diagn. 2001;21:1129–32.
Serikawa T, Nishiyama K, Tohyama J, Tazawa R, Goto K, Kuriyama Y, Haino K, Kanemura Y, Yamasaki M, Nakata K, Takakuwa K, Enomoto T. Prenatal molecular diagnosis of X-linked hydrocephalus via a silent C924T mutation in the L1CAM gene. Congenit Anom (Kyoto). 2014;54:243–5.
Silan F, Ozdemir I, Lissens W. A novel L1CAM mutation with L1 spectrum disorders. Prenat Diagn. 2005;25:57–9.
Stowe RC, Lyons-Warren AM, Emrick L. Clinical Reasoning: Ventriculomegaly detected on 20-week anatomic fetal ultrasound. Neurology. 2018;91:e1265–8.
Sztriha L, Frossard P, Hofstra RM, Verlind E, Nork M. Novel missense mutation in the L1 gene in a child with corpus callosum agenesis, retardation, adducted thumbs, spastic paraparesis, and hydrocephalus. J Child Neurol. 2000;15:239–43.
Sztriha L, Vos YJ, Verlind E, Johansen J, Berg B. X-linked hydrocephalus: a novel missense mutation in the L1CAM gene. Pediatr Neurol. 2002;27:293–6.
Takahashi S, Makita Y, Okamoto N, Miyamoto A, Oki J. L1CAM mutation in a Japanese family with X-linked hydrocephalus: a study for genetic counseling. Brain Develop. 1997;19:559–62.
Takechi T, Tohyama J, Kurashige T, Maruta K, Uyemura K, Ohi T, Matsukura S, Sakuragawa N. A deletion of five nucleotides in the L1CAM gene in a Japanese family with X-linked hydrocephalus. Hum Genet. 1996;97:353–6.
Takenouchi T, Nakazawa M, Kanemura Y, Shimozato S, Yamasaki M, Takahashi T, Kosaki K. Hydrocephalus with Hirschsprung disease: severe end of X-linked hydrocephalus spectrum. Am J Med Genet A. 2012;158:812–5.
Tegay DH, Lane AH, Roohi J, Hatchwell E. Contiguous gene deletion involving L1CAM and AVPR2 causes X-linked hydrocephalus with nephrogenic diabetes insipidus. Am J Med Genet A. 2007;143:594–8.
Van Camp G, Vits L, Coucke P, Lyonnet S, Schrander-Stumpel C, Darby J, Holden J, Munnich A, Willems PJ. A duplication in the L1CAM gene associated with X-linked hydrocephalus. Nat Genet. 1993;4:421–5.
Verhagen WI, Bartels RH, Fransen E, van Camp G, Renier WO, Grotenhuis JA. Familial congenital hydrocephalus and aqueduct stenosis with probably autosomal dominant inheritance and variable expression. J Neurol Sci. 1998;158:101–5.
Vits L, Van Camp G, Coucke P, Fransen E, De Boulle K, Reyniers E, Korn B, Poustka A, Wilson G, Schrander-Stumpel C, et al. MASA syndrome is due to mutations in the neural cell adhesion gene L1CAM. Nat Genet. 1994;7:408–13.
Vos YJ, de Walle HE, Bos KK, Stegeman JA, Ten Berge AM, Bruining M, van Maarle MC, Elting MW, den Hollander NS, Hamel B, Fortuna AM, Sunde LE, Stolte-Dijkstra I, Schrander-Stumpel CT, Hofstra RM. Genotype-phenotype correlations in L1 syndrome: a guide for genetic counselling and mutation analysis. J Med Genet. 2010;47:169–75.
Wilson PL, Kattman BB, Mulvihill JJ, Li S, Wilkins J, Wagner AF, Goodman JR. Prenatal identification of a novel R937P L1CAM missense mutation. Genet Test Mol Biomarkers. 2009;13:515–9.
Xie B, Luo J, Lei Y, Yang Q, Li M, Yi S, Luo S, Wang J, Qin Z, Yang Z, Wei H, Fan X. Two novel pathogenic variants of L1CAM gene in two fetuses with isolated X-linked hydrocephaly: a case report. Mol Med Rep. 2018;18:5760–4.
Yamasaki M, Nonaka M, Suzumori N, Nakamura H, Fujita H, Namba A, Kamei Y, Yamada T, Pooh RK, Tanemura M, Sudo N, Nagasaka M, Yoshioka E, Shofuda T, Kanemura Y. Prenatal molecular diagnosis of a severe type of L1 syndrome (X-linked hydrocephalus). J Neurosurg Pediatr. 2011;8:411–6.
Aldinger KA, Lehmann OJ, Hudgins L, Chizhikov VV, Bassuk AG, Ades LC, Krantz ID, Dobyns WB, Millen KJ. FOXC1 is required for normal cerebellar development and is a major contributor to chromosome 6p25.3 Dandy-Walker malformation. Nat Genet. 2009;41:1037–42.
Arora V, Bijarnia-Mahay S, Kulshreshtra S, Singh K, Puri RD, Verma IC. Prenatal presentation of a rare genetic disorder: a clinical, autopsy and molecular correlation. Autops Case Rep. 2019;9: e2019124.
Chen CP, Tzen CY, Chern SR, Tsai FJ, Hsu CY, Lee CC, Lee MS, Pan CW, Wang W. A 12 Mb deletion of 6p24.1–>pter in an 18-gestational-week fetus with orofacial clefting, the Dandy-Walker malformation and bilateral multicystic kidneys. Eur J Med Genet. 2009;52:59–61.
Darbro BW, Mahajan VB, Gakhar L, Skeie JM, Campbell E, Wu S, Bing X, Millen KJ, Dobyns WB, Kessler JA, Jalali A, Cremer J, Segre A, Manak JR, Aldinger KA, Suzuki S, Natsume N, Ono M, Hai HD, Vietle T, Loddo S, Valente EM, Bernardini L, Ghonge N, Ferguson PJ, Bassuk AG. Mutations in extracellular matrix genes NID1 and LAMC1 cause autosomal dominant Dandy-Walker malformation and occipital cephaloceles. Hum Mutat. 2013;34:1075–9.
Faqeih EA, Almannai M, Saleh MM, AlWadei AH, Samman MM, Alkuraya FS. Phenotypic characterization of KCTD3-related developmental epileptic encephalopathy. Clin Genet. 2018;93:1081–6.
Gai N, Jiang C, Zou YY, Zheng Y, Liang DS, Wu LQ. Novel SIL1 nonstop mutation in a Chinese consanguineous family with Marinesco-Sjögren syndrome and Dandy-Walker syndrome Clinica Chimica Acta. Int J Clin Chem. 2016;458:1–4.
Guo W, Zhao Y, Li S, Wang J, Liu X. Hypoglycemia and Dandy-Walker variant in a Kabuki syndrome patient: a case report. BMC Med Genet. 2020;21:193.
Jalali A, Aldinger KA, Chary A, McLone DG, Bowman RM, et al. Linkage to chromosome 2q361 in autosomal dominant Dandy-Walker malformation with occipital cephalocele and evidence for genetic heterogeneity. Hum Genet. 2008;123:237–45.
Liao C, Fu F, Li R, Yang X, Xu Q, Li DZ. Prenatal diagnosis and molecular characterization of a novel locus for Dandy-Walker malformation on chromosome 7p213. Eur J Med Genet. 2012;55:472–5.
Linpeng S, Liu J, Pan J, Cao Y, Teng Y, Liang D, Li Z, Wu L. Diagnosis of Joubert Syndrome 10 in a Fetus with Suspected Dandy-Walker Variant by WES: a novel splicing mutation in OFD1. Biomed Res Int. 2018;2018:4032543.
MacDonald EA, Holden JJ. Duplication 12q24––qter in an infant with Dandy-Walker syndrome. J Neurogenet. 1985;2:123–9.
Mademont-Soler I, Morales C, Armengol L, Soler A, Sánchez A. Description of the smallest critical region for Dandy-Walker malformation in chromosome 13 in a girl with a cryptic deletion related to t(6;13)(q23;q32). Am J Med Genet A. 2010;152:2308–12.
Matsukura H, Nagamori M, Miya K, Yorifuji T. MODY3, renal cysts, and Dandy-Walker variants with a microdeletion spanning the HNF1A gene. Clin Nephrol. 2017;88:162–6.
Mimaki M, Shiihara T, Watanabe M, Hirakata K, Sakazume S, Ishiguro A, Shimojima K, Yamamoto T, Oka A, Mizuguchi M. Holoprosencephaly with cerebellar vermis hypoplasia in 13q deletion syndrome: critical region for cerebellar dysgenesis within 13q322q34. Brain Dev. 2015;37:714–8.
Shalata A, Lauhasurayotin S, Leibovitz Z, Li H, Hebert D, Dhanraj S, Hadid Y, Mahroum M, Bajar J, Egenburg S, Arad A, Shohat M, Haddad S, Bakry H, Moshiri H, Scherer SW, Tzur S, Dror Y. Biallelic mutations in EXOC3L2 cause a novel syndrome that affects the brain, kidney and blood. J Med Genet. 2019;56:340–6.
Sudha T, Dawson AJ, Prasad AN, Konkin D, de Groot GW, Prasad C. De novo interstitial long arm deletion of chromosome 3 with facial dysmorphism, Dandy-Walker variant malformation and hydrocephalus. Clin Dysmorphol. 2001;10:193–6.
Traversa A, Bernardo S, Paiardini A, Giovannetti A, Marchionni E, Genovesi ML, Guadagnolo D, Torres B, Paolacci S, Bernardini L, Mazza T, Carella M, Caputo V, Pizzuti A. Prenatal whole exome sequencing detects a new homozygous fukutin (FKTN) mutation in a fetus with an ultrasound suspicion of familial Dandy-Walker malformation. Mol Genet Genomic Med. 2020;8: e1054.
Zaki MS, Masri A, Gregor A, Gleeson JG, Rosti RO. Dandy-Walker malformation, genitourinary abnormalities, and intellectual disability in two families. Am J Med Genet A. 2015;167:2503–7.
Zanni G, Barresi S, Travaglini L, Bernardini L, Rizza T, Digilio MC, Mercuri E, Cianfarani S, Valeriani M, Ferraris A, Da Sacco L, Novelli A, Valente EM, Dallapiccola B, Bertini ES. FGF17, a gene involved in cerebellar development, is downregulated in a patient with Dandy-Walker malformation carrying a de novo 8p deletion. Neurogenetics. 2011;12:241–5.
Alby C, Piquand K, Huber C, Megarbané A, Ichkou A, Legendre M, Pelluard F, Encha-Ravazi F, Abi-Tayeh G, Bessières B, El Chehadeh-Djebbar S, Laurent N, Faivre L, Sztriha L, Zombor M, Szabó H, Failler M, Garfa-Traore M, Bole C, Nitschké P, Nizon M, Elkhartoufi N, Clerget-Darpoux F, Munnich A, Lyonnet S, Vekemans M, Saunier S, Cormier-Daire V, Attié-Bitach T, Thomas S. Mutations in KIAA0586 Cause Lethal Ciliopathies Ranging from a Hydrolethalus Phenotype to Short-Rib Polydactyly Syndrome. Am J Hum Genet. 2015;97:311–8.
Al-Shroof M, Karnik AM, Karnik AA, Longshore J, Sliman NA, Khan FA. Ciliary dyskinesia associated with hydrocephalus and mental retardation in a Jordanian family. Mayo Clin Proc. 2001;76:1219–24.
Bachmann-Gagescu R, Ishak GE, Dempsey JC, Adkins J, O’Day D, Phelps IG, Gunay-Aygun M, Kline AD, Szczaluba K, Martorell L, Alswaid A, Alrasheed S, Pai S, Izatt L, Ronan A, Parisi MA, Mefford H, Glass I, Doherty D. Genotype-phenotype correlation in CC2D2A-related Joubert syndrome reveals an association with ventriculomegaly and seizures. J Med Genet. 2012;49:126–37.
Bondeson ML, Ericson K, Gudmundsson S, Ameur A, Pontén F, Wesström J, Frykholm C, Wilbe M. A nonsense mutation in CEP55 defines a new locus for a Meckel-like syndrome, an autosomal recessive lethal fetal ciliopathy. Clin Genet. 2017;92:510–6.
Boycott KM, Parboosingh JS, Scott JN, McLeod DR, Greenberg CR, Fujiwara TM, Mah JK, Midgley J, Wade A, Bernier FP, Chodirker BN, Bunge M, Innes AM. Meckel syndrome in the Hutterite population is actually a Joubert-related cerebello-oculo-renal syndrome. Am J Med Genet A. 2007;143:1715–25.
Dawe HR, Smith UM, Cullinane AR, Gerrelli D, Cox P, Badano JL, Blair-Reid S, Sriram N, Katsanis N, Attie-Bitach T, Afford SC, Copp AJ, Kelly DA, Gull K, Johnson CA. The Meckel-Gruber Syndrome proteins MKS1 and meckelin interact and are required for primary cilium formation. Hum Mol Genet. 2007;16:173–86.
Duran I, Taylor SP, Zhang W, Martin J, Qureshi F, Jacques SM, Wallerstein R, Lachman RS, Nickerson DA, Bamshad M, Cohn DH, Krakow D. Mutations in IFT-A satellite core component genes IFT43 and IFT121 produce short rib polydactyly syndrome with distinctive campomelia. Cilia. 2017;6:7.
Edvardson S, Shaag A, Zenvirt S, Erlich Y, Hannon GJ, Shanske AL, Gomori JM, Ekstein J, Elpeleg O. Joubert syndrome 2 (JBTS2) in Ashkenazi Jews is associated with a TMEM216 mutation. Am J Hum Genet. 2010;86:93–7.
Failler M, Gee HY, Krug P, Joo K, Halbritter J, Belkacem L, Filhol E, Porath JD, Braun DA, Schueler M, Frigo A, Alibeu O, Masson C, Brochard K, Hurault de Ligny B, Novo R, Pietrement C, Kayserili H, Salomon R, Gubler MC, Otto EA, Antignac C, Kim J, Benmerah A, Hildebrandt F, Saunier S. Mutations of CEP83 cause infantile nephronophthisis and intellectual disability. Am J Hum Genet. 2014;94:905–14.
Kosaki K, Ikeda K, Miyakoshi K, Ueno M, Kosaki R, Takahashi D, Tanaka M, Torikata C, Yoshimura Y, Takahashi T. Absent inner dynein arms in a fetus with familial hydrocephalus-situs abnormality. Am J Med Genet A. 2004;129:308–11.
Mei HF, Dong XR, Chen HY, Lu YL, Wu BB, Wang HJ, Cheng GQ, Wang LS, Cao Y, Yang L, Zhou WH. Genetic etiologies associated with infantile hydrocephalus in a Chinese infantile cohort. World J Pediatr. 2021;17:305–16.
Nabhan MM, Abdelaziz H, Xu Y, El Sayed R, Santibanez-Koref M, Soliman NA, Sayer JA. Case report: whole-exome analysis of a child with polycystic kidney disease and ventriculomegaly. Genet Mol Res. 2015;14:3618–24.
Oud MM, Bonnard C, Mans DA, Altunoglu U, Tohari S, Ng AYJ, Eskin A, Lee H, Rupar CA, de Wagenaar NP, Wu KM, Lahiry P, Pazour GJ, Nelson SF, Hegele RA, Roepman R, Kayserili H, Venkatesh B, Siu VM, Reversade B, Arts HH. A novel ICK mutation causes ciliary disruption and lethal endocrine-cerebro-osteodysplasia syndrome. Cilia. 2016;5:8.
Rocca MS, Piatti G, Michelucci A, Guazzo R, Bertini V, Vinanzi C, Caligo MA, Valetto A, Foresta C. A novel genetic variant in DNAI2 detected by custom gene panel in a newborn with Primary Ciliary Dyskinesia: case report. BMC Med Genet. 2020;21:220.
Wallmeier J, Frank D, Shoemark A, Nöthe-Menchen T, Cindric S, Olbrich H, Loges NT, Aprea I, Dougherty GW, Pennekamp P, Kaiser T, Mitchison HM, Hogg C, Carr SB, Zariwala MA, Ferkol T, Leigh MW, Davis SD, Atkinson J, Dutcher SK, Knowles MR, Thiele H, Altmüller J, Krenz H, Wöste M, Brentrup A, Ahrens F, Vogelberg C, Morris-Rosendahl DJ, Omran H. De Novo Mutations in FOXJ1 result in a motile ciliopathy with hydrocephalus and randomization of left/right body asymmetry. Am J Hum Genet. 2019;105:1030–9.
Cappuccio G, Ugga L, Parrini E, D’Amico A, Brunetti-Pierri N. Severe presentation and complex brain malformations in an individual carrying a CCND2 variant. Mol Genet Genomic Med. 2019;7: e708.
Maguolo A, Antoniazzi F, Spano A, Fiorini E, Gaudino R, Mauro M, Cantalupo G, Biban P, Maitz S, Cavarzere P. Clinical pitfalls in the diagnosis of segmental overgrowth syndromes: a child with the c2740G > A mutation in PIK3CA gene. Ital J Pediatr. 2018;44:110.
Maini I, Farnetti E, Caraffi SG, Ivanovski I, De Bernardi ML, Gelmini C, Pollazzon M, Rosato S, Laurie S, Matalonga L, Baldo C, Garavelli L. A Novel CCND2 mutation in a previously reported case of megalencephaly and perisylvian polymicrogyria with postaxial polydactyly and hydrocephalus. Neuropediatrics. 2018;49:222–4.
McDermott JH, Hickson N, Banerjee I, Murray PG, Ram D, Metcalfe K, Clayton-Smith J, Douzgou S. Hypoglycaemia represents a clinically significant manifestation of PIK3CA- and CCND2-associated segmental overgrowth. Clin Genet. 2018;93:687–92.
Mirzaa GM, Conti V, Timms AE, Smyser CD, Ahmed S, Carter M, Barnett S, Hufnagel RB, Goldstein A, Narumi-Kishimoto Y, Olds C, Collins S, Johnston K, Deleuze JF, Nitschké P, Friend K, Harris C, Goetsch A, Martin B, Boyle EA, Parrini E, Mei D, Tattini L, Slavotinek A, Blair E, Barnett C, Shendure J, Chelly J, Dobyns WB, Guerrini R. Characterisation of mutations of the phosphoinositide-3-kinase regulatory subunit, PIK3R2, in perisylvian polymicrogyria: a next-generation sequencing study. The Lancet Neurol. 2015;14:1182–95.
Mirzaa GM, Rivière JB, Dobyns WB. Megalencephaly syndromes and activating mutations in the PI3K-AKT pathway: MPPH and MCAP. Am J Med Genet C Semin Med Genet. 2013;163:122–30.
Ortega-Recalde O, Beltrán OI, Gálvez JM, Palma-Montero A, Restrepo CM, Mateus HE, Laissue P. Biallelic HERC1 mutations in a syndromic form of overgrowth and intellectual disability. Clin Genet. 2015;88:e1-3.
Poduri A, Evrony GD, Cai X, Elhosary PC, Beroukhim R, Lehtinen MK, Hills LB, Heinzen EL, Hill A, Hill RS, Barry BJ, Bourgeois BF, Riviello JJ, Barkovich AJ, Black PM, Ligon KL, Walsh CA. Somatic activation of AKT3 causes hemispheric developmental brain malformations. Neuron. 2012;74:41–8.
Rivière JB, Mirzaa GM, O’Roak BJ, Beddaoui M, Alcantara D, Conway RL, St-Onge J, Schwartzentruber JA, Gripp KW, Nikkel SM, Worthylake T, Sullivan CT, Ward TR, Butler HE, Kramer NA, Albrecht B, Armour CM, Armstrong L, Caluseriu O, Cytrynbaum C, Drolet BA, Innes AM, Lauzon JL, Lin AE, Mancini GM, Meschino WS, Reggin JD, Saggar AK, Lerman-Sagie T, Uyanik G, Weksberg R, Zirn B, Beaulieu CL, Majewski J, Bulman DE, O’Driscoll M, Shendure J, Graham JM Jr, Boycott KM, Dobyns WB. De novo germline and postzygotic mutations in AKT3, PIK3R2 and PIK3CA cause a spectrum of related megalencephaly syndromes. Nat Genet. 2012;44:934–40.
Sameshima T, Morisada N, Egawa T, Kugo M, Iijima K. MPPH syndrome with aortic coarctation and macrosomia due to CCND2 mutations. Pediatr Int. 2020;62:115–7.
Szalai R, Melegh BI, Till A, Ripszam R, Csabi G, Acharya A, Schrauwen I, Leal SM, Komoly S, Kosztolanyi G, Hadzsiev K. Maternal mosaicism underlies the inheritance of a rare germline AKT3 variant which is responsible for megalencephaly-polymicrogyria-polydactyly-hydrocephalus syndrome in two Roma half-siblings. Exp Mol Pathol. 2020;115: 104471.
Tapper WJ, Foulds N, Cross NC, Aranaz P, Score J, Hidalgo-Curtis C, Robinson DO, Gibson J, Ennis S, Temple IK, Collins A. Megalencephaly syndromes: exome pipeline strategies for detecting low-level mosaic mutations. PLoS ONE. 2014;9: e86940.
Tenorio J, Mansilla A, Valencia M, Martínez-Glez V, Romanelli V, Arias P, Castrejón N, Poletta F, Guillén-Navarro E, Gordo G, Mansilla E, García-Santiago F, González-Casado I, Vallespín E, Palomares M, Mori MA, Santos-Simarro F, García-Miñaur S, Fernández L, Mena R, Benito-Sanz S, del Pozo Á, Silla JC, Ibañez K, López-Granados E, Martín-Trujillo A, Montaner D, Heath KE, Campos-Barros Á, Dopazo J, Nevado J, Monk D, Ruiz-Pérez VL, Lapunzina P. A new overgrowth syndrome is due to mutations in RNF125. Hum Mutat. 2014;35:1436–41.
Terrone G, Voisin N, Abdullah-Alfaiz A, Cappuccio G, Vitiello G, Guex N, D’Amico A, James-Barkovich A, Brunetti-Pierri N, Del-Giudice E, Reymond A. De novo PIK3R2 variant causes polymicrogyria, corpus callosum hyperplasia and focal cortical dysplasia. Eur J Human Genet. 2016;24:1359–62.
Zarate YA, Boccuto L, Srikanth S, Pauly R, Ocal E, Balmakund T, Hinkle K, Stefans V, Schaefer GB, Collins RT 2nd. Constitutive activation of the PI3K-AKT pathway and cardiovascular abnormalities in an individual with Kosaki overgrowth syndrome. Am J Med Genet A. 2019;179:1047–52.
Al-Dosari MS, Al-Owain M, Tulbah M, Kurdi W, Adly N, Al-Hemidan A, Masoodi TA, Albash B, Alkuraya FS. Mutation in MPDZ causes severe congenital hydrocephalus. J Med Genet. 2013;50:54–8.
Al-Jezawi NK, Al-Shamsi AM, Suleiman J, Ben-Salem S, John A, Vijayan R, Ali BR, Al-Gazali L. Compound heterozygous variants in the multiple PDZ domain protein (MPDZ) cause a case of mild non-progressive communicating hydrocephalus. BMC Med Genet. 2018;19:34.
Mégarbané A, Pangrazio A, Villa A, Chouery E, Maarawi J, Sabbagh S, Lefranc G, Sobacchi C. Homozygous stop mutation in the SNX10 gene in a consanguineous Iraqi boy with osteopetrosis and corpus callosum hypoplasia. Eur J Med Genet. 2013;56:32–5.
Reis LM, Tyler RC, Abdul-Rahman O, Trapane P, Wallerstein R, Broome D, Hoffman J, Khan A, Paradiso C, Ron N, Bergner A, Semina EV. Mutation analysis of B3GALTL in Peters Plus syndrome. Am J Med Genet A. 2008;146:2603–10.
Rodriguez D, Gauthier F, Bertini E, Bugiani M, Brenner M, N’Guyen S, Goizet C, Gelot A, Surtees R, Pedespan JM, Hernandorena X, Troncoso M, Uziel G, Messing A, Ponsot G, Pham-Dinh D, Dautigny A, Boespflug-Tanguy O. Infantile Alexander disease: spectrum of GFAP mutations and genotype-phenotype correlation. Am J Hum Genet. 2001;69:1134–40.
Sakakibara T, Takahashi Y, Fukuda K, Inoue T, Kurosawa T, Nishikubo T, Shima M, Taoka T, Aida N, Tsujino S, Kanazawa N, Yoshioka A. A case of infantile Alexander disease diagnosed by magnetic resonance imaging and genetic analysis. Brain Develop. 2007;29:525–8.
Saugier-Veber P, Marguet F, Lecoquierre F, Adle-Biassette H, Guimiot F, Cipriani S, Patrier S, Brasseur-Daudruy M, Goldenberg A, Layet V, Capri Y, Gérard M, Frébourg T, Laquerrière A. Hydrocephalus due to multiple ependymal malformations is caused by mutations in the MPDZ gene. Acta Neuropathol Commun. 2017;5:36.
Takeyari S, Kubota T, Miyata K, Yamamoto K, Nakayama H, Yamamoto K, Ohata Y, Kitaoka T, Yanagi K, Kaname T, Ozono K. Japanese patient with Cole-carpenter syndrome with compound heterozygous variants of SEC24D. Am J Med Genet A. 2018;176:2882–6.
van der Knaap MS, Salomons GS, Li R, Franzoni E, Gutiérrez-Solana LG, Smit LM, Robinson R, Ferrie CD, Cree B, Reddy A, Thomas N, Banwell B, Barkhof F, Jakobs C, Johnson A, Messing A, Brenner M. Unusual variants of Alexander’s disease. Ann Neurol. 2005;57:327–38.
Zhang K, Cox E, Strom S, Xu ZL, Disilvestro A, Usrey K. Prenatal presentation and diagnosis of Baraitser-Winter syndrome using exome sequencing. Am J Med Genet A. 2020;182:2124–8.
Beltran-Valero de Bernabé D, Voit T, Longman C, Steinbrecher A, Straub V, Yuva Y, Herrmann R, Sperner J, Korenke C, Diesen C, Dobyns WB, Brunner HG, van Bokhoven H, Brockington M, Muntoni F. Mutations in the FKRP gene can cause muscle-eye-brain disease and Walker-Warburg syndrome. J Med Genet. 2004;41: e61.
Beltrán-Valero de Bernabé D, Currier S, Steinbrecher A, Celli J, van Beusekom E, van der Zwaag B, Kayserili H, Merlini L, Chitayat D, Dobyns WB, Cormand B, Lehesjoki AE, Cruces J, Voit T, Walsh CA, van Bokhoven H, Brunner HG. Mutations in the O-mannosyltransferase gene POMT1 give rise to the severe neuronal migration disorder Walker-Warburg syndrome. Am J Hum Genet. 2002;71:1033–43.
Biancheri R, Bertini E, Falace A, Pedemonte M, Rossi A, D’Amico A, Scapolan S, Bergamino L, Petrini S, Cassandrini D, Broda P, Manfredi M, Zara F, Santorelli FM, Minetti C, Bruno C. POMGnT1 mutations in congenital muscular dystrophy: genotype-phenotype correlation and expanded clinical spectrum. Arch Neurol. 2006;63:1491–5.
Bouchet C, Gonzales M, Vuillaumier-Barrot S, Devisme L, Lebizec C, Alanio E, Bazin A, Bessières-Grattagliano B, Bigi N, Blanchet P, Bonneau D, Bonnières M, Carles D, Delahaye S, Fallet-Bianco C, Figarella-Branger D, Gaillard D, Gasser B, Guimiot F, Joubert M, Laurent N, Liprandi A, Loget P, Marcorelles P, Martinovic J, Menez F, Patrier S, Pelluard-Nehmé F, Perez MJ, Rouleau-Dubois C, Triau S, Laquerrière A, Encha-Razavi F, Seta N. Molecular heterogeneity in fetal forms of type II lissencephaly. Hum Mutat. 2007;28:1020–7.
Cormand B, Pihko H, Bayés M, Valanne L, Santavuori P, Talim B, Gershoni-Baruch R, Ahmad A, van Bokhoven H, Brunner HG, Voit T, Topaloglu H, Dobyns WB, Lehesjoki AE. Clinical and genetic distinction between Walker-Warburg syndrome and muscle-eye-brain disease. Neurology. 2001;56:1059–69.
Currier SC, Lee CK, Chang BS, Bodell AL, Pai GS, Job L, Lagae LG, Al-Gazali LI, Eyaid WM, Enns G, Dobyns WB, Walsh CA. Mutations in POMT1 are found in a minority of patients with Walker-Warburg syndrome. Am J Med Genet A. 2005;133:53–7.
Geis T, Rödl T, Topaloğlu H, Balci-Hayta B, Hinreiner S, Müller-Felber W, Schoser B, Mehraein Y, Hübner A, Zirn B, Hoopmann M, Reutter H, Mowat D, Schuierer G, Schara U, Hehr U, Kölbel H. Clinical long-time course, novel mutations and genotype-phenotype correlation in a cohort of 27 families with POMT1-related disorders. Orphanet J Rare Dis. 2019;14:179.
Hehr U, Uyanik G, Gross C, Walter MC, Bohring A, Cohen M, Oehl-Jaschkowitz B, Bird LM, Shamdeen GM, Bogdahn U, Schuierer G, Topaloglu H, Aigner L, Lochmüller H, Winkler J. Novel POMGnT1 mutations define broader phenotypic spectrum of muscle-eye-brain disease. Neurogenetics. 2007;8:279–88.
Ichiyama M, Ohga S, Ochiai M, Fukushima K, Ishimura M, Torio M, Urata M, Hotta T, Kang D, Hara T. Fetal hydrocephalus and neonatal stroke as the first presentation of protein C deficiency. Brain Develop. 2016;38:253–6.
Kano H, Kobayashi K, Herrmann R, Tachikawa M, Manya H, Nishino I, Nonaka I, Straub V, Talim B, Voit T, Topaloglu H, Endo T, Yoshikawa H, Toda T. Deficiency of alpha-dystroglycan in muscle-eye-brain disease. Biochem Biophys Res Commun. 2002;291:1283–6.
Karadeniz N, Zenciroğlu A, Gürer YK, Senbil N, Karadeniz Y, Topalŏlu H. De novo translocation t(5;6)(q35;q21) in an infant with Walker-Warburg syndrome. Am J Med Genet. 2002;109:67–9.
Preiksaitiene E, Voisin N, Gueneau L, Benušienė E, Krasovskaja N, Blažytė EM, Ambrozaitytė L, Rančelis T, Reymond A, Kučinskas V. Pathogenic homozygous variant in POMK gene is the cause of prenatally detected severe ventriculomegaly in two Lithuanian families. Am J Med Genet A. 2020;182:536–42.
van Reeuwijk J, Janssen M, van den Elzen C, Beltran-Valero de Bernabé D, Sabatelli P, Merlini L, Boon M, Scheffer H, Brockington M, Muntoni F, Huynen MA, Verrips A, Walsh CA, Barth PG, Brunner HG, van Bokhoven H. POMT2 mutations cause alpha-dystroglycan hypoglycosylation and Walker-Warburg syndrome. J Med Genet. 2005;42:907–12.
van Reeuwijk J, Maugenre S, van den Elzen C, Verrips A, Bertini E, Muntoni F, Merlini L, Scheffer H, Brunner HG, Guicheney P, van Bokhoven H. The expanding phenotype of POMT1 mutations: from Walker-Warburg syndrome to congenital muscular dystrophy, microcephaly, and mental retardation. Hum Mutat. 2006;27:453–9.
Van Reeuwijk J, Olderode-Berends MJ, Van den Elzen C, Brouwer OF, Roscioli T, Van Pampus MG, Scheffer H, Brunner HG, Van Bokhoven H, Hol FA. A homozygous FKRP start codon mutation is associated with Walker-Warburg syndrome, the severe end of the clinical spectrum. Clin Genet. 2010;78:275–81.
Riemersma M, Mandel H, van Beusekom E, Gazzoli I, Roscioli T, Eran A, Gershoni-Baruch R, Gershoni M, Pietrokovski S, Vissers LE, Lefeber DJ, Willemsen MA, Wevers RA, van Bokhoven H. Absence of α- and β-dystroglycan is associated with Walker-Warburg syndrome. Neurology. 2015;84:2177–82.
Saredi S, Ardissone A, Ruggieri A, Mottarelli E, Farina L, Rinaldi R, Silvestri E, Gandioli C, D’Arrigo S, Salerno F, Morandi L, Grammatico P, Pantaleoni C, Moroni I, Mora M. Novel POMGNT1 point mutations and intragenic rearrangements associated with muscle-eye-brain disease. J Neurol Sci. 2012;318:45–50.
Vervoort VS, Holden KR, Ukadike KC, Collins JS, Saul RA, Srivastava AK. POMGnT1 gene alterations in a family with neurological abnormalities. Ann Neurol. 2004;56:143–8.
Willer T, Lee H, Lommel M, Yoshida-Moriguchi T, de Bernabe DB, Venzke D, Cirak S, Schachter H, Vajsar J, Voit T, Muntoni F, Loder AS, Dobyns WB, Winder TL, Strahl S, Mathews KD, Nelson SF, Moore SA, Campbell KP. ISPD loss-of-function mutations disrupt dystroglycan O-mannosylation and cause Walker-Warburg syndrome. Nat Genet. 2012;44:575–80.
Yis U, Uyanik G, Kurul S, Dirik E, Ozer E, Gross C, Hehr U. A case of Walker-Warburg syndrome resulting from a homozygous POMT1 mutation. Eur J Paediatr Neurol. 2007;11:46–9.
Yoshida A, Kobayashi K, Manya H, Taniguchi K, Kano H, Mizuno M, Inazu T, Mitsuhashi H, Takahashi S, Takeuchi M, Herrmann R, Straub V, Talim B, Voit T, Topaloglu H, Toda T, Endo T. Muscular dystrophy and neuronal migration disorder caused by mutations in a glycosyltransferase, POMGnT1. Dev Cell. 2001;1:717–24.
Abdel-Salam GM, Flores-Sarnat L, El-Ruby MO, Parboosingh J, Bridge P, Eid MM, El-Badry TH, Effat L, Curatolo P, Temtamy SA. Muenke syndrome with pigmentary disorder and probable hemimegalencephaly: An expansion of the phenotype. Am J Med Genet A. 2011;155:207–14.
Arnaud-López L, Fragoso R, Mantilla-Capacho J, Barros-Núñez P. Crouzon with acanthosis nigricans. Further delineation of the syndrome. Clin Genet. 2007;72:405–10.
Chen CP, Chern SR, Shih JC, Wang W, Yeh LF, Chang TY, Tzen CY. Prenatal diagnosis and genetic analysis of type I and type II thanatophoric dysplasia. Prenat Diagn. 2001;21:89–95.
Chen CP, Lin SP, Su YN, Chien SC, Tsai FJ, Wang W. Craniosynostosis and congenital tracheal anomalies in an infant with Pfeiffer syndrome carrying the W290C FGFR2 mutation. Genet Couns. 2008;19:165–72.
Chen CP, Lin SP, Liu YP, Chern SR, Chen SW, Lai ST, Wang W. Pfeiffer syndrome with FGFR2 C342R mutation presenting extreme proptosis, craniosynostosis, hearing loss, ventriculomegaly, broad great toes and thumbs, maxillary hypoplasia, and laryngomalacia. Taiwan J Obstet Gynecol. 2017;56:412–4.
Fonseca R, Costa-Lima MA, Cosentino V, Orioli IM. Second case of Beare-Stevenson syndrome with an FGFR2 Ser372Cys mutation. Am J Med Genet A. 2008;146:658–60.
González-Del-Angel A, Estandía-Ortega B, Alcántara-Ortigoza MA, Martínez-Cruz V, Gutiérrez-Tinajero DJ, Rasmussen A, Gómez-González CS. Expansion of the variable expression of Muenke syndrome: Hydrocephalus without craniosynostosis. Am J Med Genet A. 2016;170:3189–96.
Gripp KW, Stolle CA, McDonald-McGinn DM, Markowitz RI, Bartlett SP, Katowitz JA, Muenke M, Zackai EH. Phenotype of the fibroblast growth factor receptor 2 Ser351Cys mutation: Pfeiffer syndrome type III. Am J Med Genet. 1998;78:356–60.
Gupta S, Prasad A, Sinha U, Singh R, Gupta G. Crouzon syndrome in a ten-week-old infant: a case report. Saudi J Med Med Sci. 2020;8:146–50.
Lajeunie E, Heuertz S, El Ghouzzi V, Martinovic J, Renier D, Le Merrer M, Bonaventure J. Mutation screening in patients with syndromic craniosynostoses indicates that a limited number of recurrent FGFR2 mutations accounts for severe forms of Pfeiffer syndrome. Eur J Human Genet. 2006;14:289–98.
Priolo M, Lerone M, Baffico M, Baldi M, Ravazzolo R, Cama A, Capra V, Silengo M. Pfeiffer syndrome type 2 associated with a single amino acid deletion in the FGFR2 gene. Clin Genet. 2000;58:81–3.
Przylepa KA, Paznekas W, Zhang M, Golabi M, Bias W, Bamshad MJ, Carey JC, Hall BD, Stevenson R, Orlow S, Cohen MM Jr, Jabs EW. Fibroblast growth factor receptor 2 mutations in Beare-Stevenson cutis gyrata syndrome. Nat Genet. 1996;13:492–4.
Rump P, Letteboer TG, Gille JJ, Torringa MJ, Baerts W, van Gestel JP, Verheij JB, van Essen AJ. Severe complications in a child with achondroplasia and two FGFR3 mutations on the same allele. Am J Med Genet A. 2006;140:284–90.
Rutland P, Pulleyn LJ, Reardon W, Baraitser M, Hayward R, Jones B, Malcolm S, Winter RM, Oldridge M, Slaney SF, et al. Identical mutations in the FGFR2 gene cause both Pfeiffer and Crouzon syndrome phenotypes. Nat Genet. 1995;9:173–6.
Schaefer F, Anderson C, Can B, Say B. Novel mutation in the FGFR2 gene at the same codon as the Crouzon syndrome mutations in a severe Pfeiffer syndrome type 2 case. Am J Med Genet. 1998;75:252–5.
Takenouchi T, Hida M, Sakamoto Y, Torii C, Kosaki R, Takahashi T, Kosaki K. Severe congenital lipodystrophy and a progeroid appearance: Mutation in the penultimate exon of FBN1 causing a recognizable phenotype. Am J Med Genet A. 2013;161:3057–62.
Çiftçi E, Ince E, Akar N, Dogru Ü, Tefs K, Schuster V. Ligneous conjunctivitis, hydrocephalus, hydrocele, and pulmonary involvement in a child with homozygous type I plasminogen deficiency. Eur J Pediatr. 2003;162:462–5.
Cormand B, Avela K, Pihko H, Santavuori P, Talim B, Topaloglu H, de la Chapelle A, Lehesjoki AE. Assignment of the muscle-eye-brain disease gene to 1p32-p34 by linkage analysis and homozygosity mapping. Am J Hum Genet. 1999;64:126–35.
Cotarelo RP, Valero MC, Prados B, Peña A, Rodríguez L, Fano O, Marco JJ, Martínez-Frías ML, Cruces J. Two new patients bearing mutations in the fukutin gene confirm the relevance of this gene in Walker-Warburg syndrome. Clin Genet. 2008;73:139–45.
de Bernabé DB, van Bokhoven H, van Beusekom E, Van den Akker W, Kant S, Dobyns WB, Cormand B, Currier S, Hamel B, Talim B, Topaloglu H, Brunner HG. A homozygous nonsense mutation in the fukutin gene causes a Walker-Warburg syndrome phenotype. J Med Genet. 2003;40:845–8.
Horn D, Robinson PN. Progeroid facial features and lipodystrophy associated with a novel splice site mutation in the final intron of the FBN1 gene. Am J Med Genet A. 2011;155:721–4.
Kondo-Iida E, Kobayashi K, Watanabe M, Sasaki J, Kumagai T, Koide H, Saito K, Osawa M, Nakamura Y, Toda T. Novel mutations and genotype-phenotype relationships in 107 families with Fukuyama-type congenital muscular dystrophy (FCMD). Hum Mol Genet. 1999;8:2303–9.
Radmanesh F, Caglayan AO, Silhavy JL, Yilmaz C, Cantagrel V, Omar T, Rosti B, Kaymakcalan H, Gabriel S, Li M, Sestan N, Bilguvar K, Dobyns WB, Zaki MS, Gunel M, Gleeson JG. Mutations in LAMB1 cause cobblestone brain malformation without muscular or ocular abnormalities. Am J Hum Genet. 2013;92:468–74.
Saito K, Osawa M, Wang ZP, Ikeya K, Fukuyama Y, Kondo-Iida E, Toda T, Ohashi H, Kurosawa K, Wakai S, Kaneko K. Haplotype-phenotype correlation in Fukuyama congenital muscular dystrophy. Am J Med Genet. 2000;92:184–90.
Schott D, Dempfle CE, Beck P, Liermann A, Mohr-Pennert A, Goldner M, Mehlem P, Azuma H, Schuster V, Mingers AM, Schwarz HP, Kramer MD. Therapy with a purified plasminogen concentrate in an infant with ligneous conjunctivitis and homozygous plasminogen deficiency. N Engl J Med. 1998;339:1679–86.
Schuster V, Mingers AM, Seidenspinner S, Nüssgens Z, Pukrop T, Kreth HW. Homozygous mutations in the plasminogen gene of two unrelated girls with ligneous conjunctivitis. Blood. 1997;90:958–66.
Schuster V, Seidenspinner S, Müller C, Rempen A. Prenatal diagnosis in a family with severe type I plasminogen deficiency, ligneous conjunctivitis and congenital hydrocephalus. Prenat Diagn. 1999;19:483–7.
Tonduti D, Dorboz I, Renaldo F, Masliah-Planchon J, Elmaleh-Bergès M, Dalens H, Rodriguez D, Boespflug-Tanguy O. Cystic leukoencephalopathy with cortical dysplasia related to LAMB1 mutations. Neurology. 2015;84:2195–7.
van der Knaap MS, Smit LM, Barkhof F, Pijnenburg YA, Zweegman S, Niessen HW, Imhof S, Heutink P. Neonatal porencephaly and adult stroke related to mutations in collagen IV A1. Ann Neurol. 2006;59:504–11.
Yang YD, Huang LY, Yan JM, Han J, Zhang Y, Li DZ. Novel FREM1 mutations are associated with severe hydrocephalus and shortened limbs in a prenatal case. Eur J Obstet Gynecol Reprod Biol. 2017;215:262–4.
Antwi P, Hong CS, Duran D, Jin SC, Dong W, DiLuna M, Kahle KT. A novel association of campomelic dysplasia and hydrocephalus with an unbalanced chromosomal translocation upstream of SOX9. Cold Spring Harbor molecular case studies. 2018;4:1.
Avitan-Hersh E, Mandel H, Indelman M, Bar-Joseph G, Zlotogorski A, Bergman R. A case of H syndrome showing immunophenotye similarities to Rosai-Dorfman disease. Am J Dermatopathol. 2011;33:47–51.
Cauley ES, Hamed A, Mohamed IN, Elseed M, Martinez S, Yahia A, Abozar F, Abubakr R, Koko M, Elsayed L, Piao X, Salih MA, Manzini MC. Overlap of polymicrogyria, hydrocephalus, and Joubert syndrome in a family with novel truncating mutations in ADGRG1/GPR56 and KIAA0556. Neurogenetics. 2019;20:91–8.
Christofolini DM, Yoshimoto M, Squire JA, Brunoni D, Melaragno MI, Carvalheira G. Hydrocephaly, penoscrotal transposition, and digital anomalies associated with de novo pseudodicentric rearranged chromosome 13 characterized by classical cytogenetic methods and mBAND analysis. Am J Med Genet A. 2006;140:1321–5.
Doherty D, Chudley AE, Coghlan G, Ishak GE, Innes AM, Lemire EG, Rogers RC, Mhanni AA, Phelps IG, Jones SJ, Zhan SH, Fejes AP, Shahin H, Kanaan M, Akay H, Tekin M, Triggs-Raine B, Zelinski T. GPSM2 mutations cause the brain malformations and hearing loss in Chudley-McCullough syndrome. Am J Hum Genet. 2012;90:1088–93.
Forrester S, Kovach MJ, Smith RE, Rimer L, Wesson M, Kimonis VE. Kousseff syndrome caused by deletion of chromosome 22q11-13. Am J Med Genet. 2002;112:338–42.
Grosso S, Cioni M, Garibaldi G, Pucci L, Galluzzi P, Canapicchi R, Morgese G, Balestri P. De novo complete trisomy 5p: clinical and neuroradiological findings. Am J Med Genet. 2002;112:56–60.
Jacquemin V, Antoine M, Duerinckx S, Massart A, Desir J, Perazzolo C, Cassart M, Thomas D, Segers V, Lecomte S, Abramowicz M, Pirson I. TrkA mediates effect of novel KIDINS220 mutation in human brain ventriculomegaly. Hum Mol Genet. 2021;29:3757–64.
Kline-Fath BM, Merrow AC Jr, Calvo-Garcia MA, Nagaraj UD, Saal HM. Fowler syndrome and fetal MRI findings: a genetic disorder mimicking hydranencephaly/hydrocephalus. Pediatr Radiol. 2018;48:1032–4.
Koenigstein K, Gramsch C, Kolodziej M, Neubauer BA, Weber A, Lechner S, Hahn A. Chudley-McCullough syndrome: variable clinical picture in twins with a novel GPSM2 mutation. Neuropediatrics. 2016;47:197–201.
Lahiry P, Wang J, Robinson JF, Turowec JP, Litchfield DW, Lanktree MB, Gloor GB, Puffenberger EG, Strauss KA, Martens MB, Ramsay DA, Rupar CA, Siu V, Hegele RA. A multiplex human syndrome implicates a key role for intestinal cell kinase in development of central nervous, skeletal, and endocrine systems. Am J Hum Genet. 2009;84:134–47.
Li Y, Choy KW, Xie HN, Chen M, He WY, Gong YF, Liu HY, Song YQ, Xian YX, Sun XF, Chen XJ. Congenital hydrocephalus and hemivertebrae associated with de novo partial monosomy 6q (6q253→qter). Balkan J Med Genet. 2015;18:77–84.
K. Maclean, J. Smith, L. St Heaps, N. Chia, R. Williams, G.B. Peters, E. Onikul, T. McCrossin, O.J. Lehmann, and L.C. Adès, Axenfeld-Rieger malformation and distinctive facial features: Clues to a recognizable 6p25 microdeletion syndrome. Am J Med Genet A 132 (2005) 381–5.
Mero IL, Mørk HH, Sheng Y, Blomhoff A, Opheim GL, Erichsen A, Vigeland MD, Selmer KK. Homozygous KIDINS220 loss-of-function variants in fetuses with cerebral ventriculomegaly and limb contractures. Hum Mol Genet. 2017;26:3792–6.
Pappa L, Kals M, Kivistik PA, Metspalu A, Paal A, Nikopensius T. Exome analysis in an Estonian multiplex family with neural tube defects-a case report. Childs Nerv Syst. 2017;33:1575–81.
Powis Z, Chamberlin AC, Alamillo CL, Ceulemans S, Bird LM, Tang S. Postmortem diagnostic exome sequencing identifies a de novo TUBB3 alteration in a newborn with prenatally diagnosed hydrocephalus and suspected walker-warburg syndrome. Pediatr Dev Pathol. 2018;21:319–23.
Rai B, Sharif F. Cervicomedullary spinal stenosis and ventriculomegaly in a child with developmental delay due to chromosome 16p12.1 microdeletion syndrome. J Child Neurol. 2015;30:394–6.
Su J, Lu W, Li M, Zhang Q, Chen F, Yi S, Yang Q, Yi S, Zhou X, Huang L, Shen Y, Luo J, Qin Z. Novel compound heterozygous frameshift variants in WDR81 associated with congenital hydrocephalus 3 with brain anomalies: First Chinese prenatal case confirms WDR81 involvement. Mol Genet Genomic Med. 2021;9: e1624.
Yüksel Z, Vogel F, Alhashem AM, Alanzi TSA, Tabarki B, Kampe K, Kandaswamy KK, Werber M, Bertoli-Avella AM, Beetz C, Rolfs A, Bauer P. A homozygous frameshift variant in an alternatively spliced exon of DLG5 causes hydrocephalus and renal dysplasia. Clin Genet. 2019;95:631–3.
Demir HA, Varan A, Utine EG, Aktaş D, Oğuz B, Rama D, Büyükpamukçu M. WAGR syndrome with tetralogy of Fallot and hydrocephalus. J Pediatr Hematol Oncol. 2011;33:e174–5.
Fukino K, Teramoto A, Adachi K, Takahashi H, Emi M. A family with hydrocephalus as a complication of cerebellar hemangioblastoma: identification of Pro157Leu mutation in the VHL gene. J Hum Genet. 2000;45:47–51.
Kusakabe K, Kohno S, Inoue A, Seno T, Yonezawa S, Moritani K, Mizuno Y, Kurata M, Kitazawa R, Tauchi H, Watanabe H, Iwata S, Hirato J, Kunieda T. Combined morphological, immunohistochemical and genetic analyses of medulloepithelioma in the posterior cranial fossa. Neuropathology. 2018;38:179–84.
Reardon W, Zhou XP, Eng C. A novel germline mutation of the PTEN gene in a patient with macrocephaly, ventricular dilatation, and features of VATER association. J Med Genet. 2001;38:820–3.
Uguen A, Laurent C, Samaison L, Boisselier B, Talagas M, Costa S, Aziza J, Mokhtari K, Le Maréchal C, Marcorelles P. Severe hydrocephalus caused by diffuse leptomeningeal and neurocutaneous melanocytosis of antenatal onset: a clinical, pathologic, and molecular study of 2 cases. Hum Pathol. 2015;46:1189–96.
Drielsma A, Jalas C, Simonis N, Désir J, Simanovsky N, Pirson I, Elpeleg O, Abramowicz M, Edvardson S. Two novel CCDC88C mutations confirm the role of DAPLE in autosomal recessive congenital hydrocephalus. J Med Genet. 2012;49:708–12.
Ruggeri G, Timms AE, Cheng C, Weiss A, Kollros P, Chapman T, Tully H, Mirzaa GM. Bi-allelic mutations of CCDC88C are a rare cause of severe congenital hydrocephalus. Am J Med Genet A. 2018;176:676–81.
Wallis M, Baumer A, Smaili W, Jaouad IC, Sefiani A, Jacobson E, Bowyer L, Mowat D, Rauch A. Surprisingly good outcome in antenatal diagnosis of severe hydrocephalus related to CCDC88C deficiency. Eur J Med Genet. 2018;61:189–96.
Chen CP, Ko TM, Wang LK, Chern SR, Wu PS, Chen SW, Wu FT, Chen YY, Chen WL, Wang W. Prenatal diagnosis and molecular cytogenetic characterization of a chromosome 1q42.3-q44 deletion in a fetus associated with ventriculomegaly on prenatal ultrasound. Taiwan J Obstet Gynecol. 2020;59:598–603.
Diets IJ, Prescott T, Champaigne NL, Mancini GMS, Krossnes B, Frič R, Kocsis K, Jongmans MCJ, Kleefstra T. A recurrent de novo missense pathogenic variant in SMARCB1 causes severe intellectual disability and choroid plexus hyperplasia with resultant hydrocephalus. Genet Med. 2019;21:572–9.
Negishi Y, Miya F, Hattori A, Mizuno K, Hori I, Ando N, Okamoto N, Kato M, Tsunoda T, Yamasaki M, Kanemura Y, Kosaki K, Saitoh S. Truncating mutation in NFIA causes brain malformation and urinary tract defects. Hum Genome Var. 2015;2:15007.
Nyboe D, Kreiborg S, Kirchhoff M, Hove HB. Familial craniosynostosis associated with a microdeletion involving the NFIA gene. Clin Dysmorphol. 2015;24:109–12.
Shtaya A, Elmslie F, Crow Y, Hettige S. Leukoencephalopathy, Intracranial Calcifications, Cysts, and SNORD118 Mutation (Labrune Syndrome) with Obstructive Hydrocephalus. World Neurosurg. 2019;125:271–2.
Verkerk AJ, Schot R, van Waterschoot L, Douben H, Poddighe PJ, Lequin MH, de Vries LS, Terhal P, Hahnemann JM, de Coo IF, de Wit MC, Wafelman LS, Garavelli L, Dobyns WB, Van der Spek PJ, de Klein A, Mancini GM. Unbalanced der(5)t(5;20) translocation associated with megalencephaly, perisylvian polymicrogyria, polydactyly and hydrocephalus. Am J Med Genet A. 2010;152:1488–97.
A. Vetro, M. Iascone, I. Limongelli, N. Ameziane, S. Gana, E. Della Mina, U. Giussani, R. Ciccone, A. Forlino, L. Pezzoli, M.A. Rooimans, A.J. van Essen, J. Messa, T. Rizzuti, P. Bianchi, J. Dorsman, J.P. de Winter, F. Lalatta, and O. Zuffardi. Loss-of-Function FANCL Mutations Associate with Severe Fanconi Anemia Overlapping the VACTERL Association. Hum Mutat 36 (2015) 562–8.
Zechi-Ceide RM, Guion-Almeida ML, de Rodini ES, Jesus-Oliveira NA, Passos-Bueno MR. Hydrocephalus and moderate mental retardation in a boy with Van der Woude phenotype and IRF6 gene mutation. Clin Dysmorphol. 2007;16:163–6.
Castañeyra-Ruiz L, González-Marrero I, González-Toledo JM, Castañeyra-Ruiz A, de Paz-Carmona H, Castañeyra-Perdomo A, Carmona-Calero EM. Aquaporin-4 expression in the cerebrospinal fluid in congenital human hydrocephalus. Fluids Barriers CNS. 2013;10:18.
Kvarnung M, Taylan F, Nilsson D, Albåge M, Nordenskjöld M, Anderlid BM, Nordgren A, Syk-Lundberg E. Mutations in FLVCR2 associated with Fowler syndrome and survival beyond infancy. Clin Genet. 2016;89:99–103.
Lalonde E, Albrecht S, Ha KC, Jacob K, Bolduc N, Polychronakos C, Dechelotte P, Majewski J, Jabado N. Unexpected allelic heterogeneity and spectrum of mutations in Fowler syndrome revealed by next-generation exome sequencing. Hum Mutat. 2010;31:918–23.
Martínez-Glez V, Romanelli V, Mori MA, Gracia R, Segovia M, González-Meneses A, López-Gutierrez JC, Gean E, Martorell L, Lapunzina P. Macrocephaly-capillary malformation: Analysis of 13 patients and review of the diagnostic criteria. Am J Med Genet A. 2010;152:3101–6.
Özdemir M, Çırali C, Yılmaz-Ağladıoğlu S, Evrengül H, Tepeli E, Ergin H. Neonatal Bartter syndrome with cholelithiasis and hydrocephalus: rare association. Pediatr Int. 2016;58:912–5.
Thomas S, Encha-Razavi F, Devisme L, Etchevers H, Bessieres-Grattagliano B, Goudefroye G, Elkhartoufi N, Pateau E, Ichkou A, Bonnière M, Marcorelle P, Parent P, Manouvrier S, Holder M, Laquerrière A, Loeuillet L, Roume J, Martinovic J, Mougou-Zerelli S, Gonzales M, Meyer V, Wessner M, Feysot CB, Nitschke P, Leticee N, Munnich A, Lyonnet S, Wookey P, Gyapay G, Foliguet B, Vekemans M, Attié-Bitach T. High-throughput sequencing of a 41 Mb linkage interval reveals FLVCR2 deletions and mutations in lethal cerebral vasculopathy. Hum Mutat. 2010;31:1134–41.
Visapää I, Salonen R, Varilo T, Paavola P, Peltonen L. Assignment of the locus for hydrolethalus syndrome to a highly restricted region on 11q23-25. Am J Hum Genet. 1999;65:1086–95.
Morimoto Y, Yoshida S, Kinoshita A, Satoh C, Mishima H, Yamaguchi N, Matsuda K, Sakaguchi M, Tanaka T, Komohara Y, Imamura A, Ozawa H, Nakashima M, Kurotaki N, Kishino T, Yoshiura KI, Ono S. Nonsense mutation in CFAP43 causes normal-pressure hydrocephalus with ciliary abnormalities. Neurology. 2019;92:e2364–74.
Zhang J, Carr CW, Rigamonti D, Badr A. Genome-wide linkage scan maps ETINPH gene to chromosome 19q12–1331. Hum Hered. 2010;69:262–7.
Schaaf CP, Koster J, Katsonis P, Kratz L, Shchelochkov OA, Scaglia F, Kelley RI, Lichtarge O, Waterham HR, Shinawi M. Desmosterolosis-phenotypic and molecular characterization of a third case and review of the literature. Am J Med Genet A. 2011;155:1597–604.
Alazami AM, Patel N, Shamseldin HE, et al. Accelerating novel candidate gene discovery in neurogenetic disorders via whole-exome sequencing of prescreened multiplex consanguineous families. Cell Rep. 2015;10:148–61.
Houge G, Haesen D, Vissers LE, Mehta S, Parker MJ, Wright M, Vogt J, McKee S, Tolmie JL, Cordeiro N, Kleefstra T, Willemsen MH, Reijnders MR, Berland S, Hayman E, Lahat E, Brilstra EH, van Gassen KL, Zonneveld-Huijssoon E, de Bie CI, Hoischen A, Eichler EE, Holdhus R, Steen VM, Døskeland SO, Hurles ME, FitzPatrick DR, Janssens V. B56δ-related protein phosphatase 2A dysfunction identified in patients with intellectual disability. J Clin Invest. 2015;125:3051–62.
Ouyang L, Yang F. Cole-Carpenter syndrome-1 with a de novo heterozygous deletion in the P4HB gene in a Chinese girl: a case report. Medicine (Baltimore). 2017;96: e9504.
Rauch F, Fahiminiya S, Majewski J, Carrot-Zhang J, Boudko S, Glorieux F, Mort JS, Bächinger HP, Moffatt P. Cole-Carpenter syndrome is caused by a heterozygous missense mutation in P4HB. Am J Hum Genet. 2015;96:425–31.
Slavotinek A, Kaylor J, Pierce H, Cahr M, DeWard SJ, Schneidman-Duhovny D, Alsadah A, Salem F, Schmajuk G, Mehta L. CRB2 mutations produce a phenotype resembling congenital nephrosis, Finnish type, with cerebral ventriculomegaly and raised alpha-fetoprotein. Am J Hum Genet. 2015;96:162–9.
Zhang L, Zhang Z, Bi X, Mao Y, Cheng Y, Zhu P, Xu S, Wang Y, Zhan X, Fan J, Yuan Y, Bi H, Wu X. Genetic and preimplantation diagnosis of cystic kidney disease with ventriculomegaly. J Hum Genet. 2020;65:455–9.
Meszarosova AU, Lastuvkova J, Rennerova L, Hitka P, Cihlar F, Seeman P, Safka-Brozkova D. Two novel pathogenic variants in KIAA1109 causing Alkuraya-Kučinskas syndrome in two Czech Roma brothers. Clin Dysmorphol. 2020;29:197–201.
Shiihara T, Oka A, Suzaki I, Ida H, Takeshita K. Communicating hydrocephalus in a patient with Gaucher’s disease type 3. Pediatr Neurol. 2000;22:234–6.
Basel-Vanagaite L, Raas-Rotchild A, Kornreich L, Har-Zahav A, Yeshaya J, Latarowski V, Lerer I, Dobyns WB, Shohat M. Familial hydrocephalus with normal cognition and distinctive radiological features. Am J Med Genet A. 2010;152:2743–8.
Bernstock JD, Tafel I, Segar DJ, Dowd R, Kappel A, Chen JA, Aglan O, Montaser A, Gupta S, Johnston B, Judge J, Fehnel K, Stone S, Warf BC. Complex management of hydrocephalus secondary to choroid plexus hyperplasia. World neurosurgery. 2020;141:101–9.
Boxill M, Becher N, Sunde L, Thelle T. Choroid plexus hyperplasia and chromosome 9p gains. Am J Med Genet A. 2018;176:1416–22.
Brock JA, Dyack S, Ludman M, Dumas N, Gaudet M, Morash B. Mosaic tetrasomy 5p resulting from an isochromosome 5p marker chromosome: case report and review of literature. Am J Med Genet A. 2012;158:406–11.
Brunetti-Pierri N, Berg JS, Scaglia F, Belmont J, Bacino CA, Sahoo T, Lalani SR, Graham B, et al. Recurrent reciprocal 1q211 deletions and duplications associated with microcephaly or macrocephaly and developmental and behavioral abnormalities. Nat Genet. 2008;40:1466–71.
Cai M, Huang H, Xu L, Lin N. Classifying and evaluating fetuses with ventriculomegaly in genetic etiologic studies. Front Genet. 2021;12: 682707.
Cambosu F, Capobianco G, Fogu G, Bandiera P, Pirino A, Moro MA, Sanna R, Soro G, Dessole M, Montella A. Partial trisomy of the long arm of chromosome 1: prenatal diagnosis, clinical evaluation and cytogenetic findings Case report and review of the literature. J Obstet Gynaecol Res. 2013;39:592–7.
Capra V, De Marco P, Merello E, Baffico AM, Baldi M, Divizia MT, Gimelli S, Mallet D, Raso A, Mascelli S, Tomà P, Rossi A, Pavanello M, Cama A, Magnani C. Craniosynostosis, hydrocephalus, Chiari I malformation and radioulnar synostosis: probably a new syndrome. Eur J Med Genet. 2009;52:17–22.
Castro-Gago M, Pintos-Martínez E, Forteza-Vila J, Iglesias-Diz M, Ucieda-Somoza R, Silva-Villar I, Codesido-López J, Viso-Lorenzo A, Campos Y, Arenas J, Eirís-Puñal J. Congenital hydranencephalic-hydrocephalic syndrome with proliferative vasculopathy: a possible relation with mitochondrial dysfunction. J Child Neurol. 2001;16:858–62.
Chen CP, Su YN, Hsu CY, Liu YP, Chern SR, Chen LF, Wang W. Prenatal diagnosis of a de novo 17p131 microduplication in a fetus with ventriculomegaly and lissencephaly. Taiwan J Obstet Gynecol. 2011;50:554–7.
Chen CP, Chang TY, Chen YY, Chern SR, Su JW, Wang W. VACTERL association with hydrocephalus in a fetus conceived by in vitro fertilization and embryo transfer. Taiwan J Obstet Gynecol. 2013;52:575–9.
Descipio C, Schneider L, Young TL, Wasserman N, Yaeger D, Lu F, Wheeler PG, Williams MS, Bason L, Jukofsky L, Menon A, Geschwindt R, Chudley AE, Saraiva J, Schinzel AA, Guichet A, Dobyns WE, Toutain A, Spinner NB, Krantz ID. Subtelomeric deletions of chromosome 6p: molecular and cytogenetic characterization of three new cases with phenotypic overlap with Ritscher-Schinzel (3C) syndrome. Am J Med Genet A. 2005;134:3–11.
Dubé P, Der Kaloustian VM, Demczuk S, Saabti H, Koenekoop RK. A new association of congenital hydrocephalus, albinism, megalocornea, and retinal coloboma in a syndromic child: a clinical and genetic study. Ophthalmic Genet. 2000;21:211–6.
Forcelini CM, Mallmann AB, Crusius PS, Seibert CA, Crusius MU, Zandoná DI, Carazzo C, Crusius CU, Goellner E, Ragnini J, Manzato LB, Winkelmann G, Lima AV, Bauermann MG. Down syndrome with congenital hydrocephalus: case report. Arq Neuropsiquiatr. 2006;64:869–71.
Garavelli L, Guareschi E, Errico S, Simoni A, Bergonzini P, Zollino M, Gurrieri F, Mancini GM, Schot R, Van Der Spek PJ, Frigieri G, Zonari P, Albertini E, Giustina ED, Amarri S, Banchini G, Dobyns WB, Neri G. Megalencephaly and perisylvian polymicrogyria with postaxial polydactyly and hydrocephalus (MPPH): report of a new case. Neuropediatrics. 2007;38:200–3.
Inui K, Yanagihara K, Otani K, Suzuki Y, Akagi M, Nakayama M, Ida H, Okada S. A new variant neuropathic type of Gaucher’s disease characterized by hydrocephalus, corneal opacities, deformed toes, and fibrous thickening of spleen and liver capsules. J Pediatr. 2001;138:137–9.
Kariminejad A, Radmanesh F, Rezayi AR, Tonekaboni SH, Gleeson JG. Megalencephaly-polymicrogyria-polydactyly-hydrocephalus syndrome: a case report. J Child Neurol. 2013;28:651–7.
Lemire EG, Stoeber GP. Chudley-McCullough syndrome: bilateral sensorineural deafness, hydrocephalus, and other structural brain abnormalities. Am J Med Genet. 2000;90:127–30.
Lowry RB, Gould DB, Walter MA, Savage PR. Absence of PITX2, BARX1, and FOXC1 mutations in De Hauwere syndrome (Axenfeld-Rieger anomaly, hydrocephaly, hearing loss): a 25-year follow up. Am J Med Genet A. 2007;143:1227–30.
Matteucci F, Tarantino E, Bianchi MC, Cingolani C, Fattori B, Nacci A, Ursino F. Sensorineural deafness, hydrocephalus and structural brain abnormalities in two sisters: the Chudley-McCullough syndrome. Am J Med Genet A. 2006;140:1183–8.
Naritomi K, Shiroma N, Izumikawa Y, Sameshima K, Ohdo S, Hirayama K. 16q21 is critical for 16q deletion syndrome. Clin Genet. 1988;33:372–5.
Østergaard E, Pedersen VF, Skriver EB, Brøndum-Nielsen K. Brothers with Chudley-McCullough syndrome: sensorineural deafness, agenesis of the corpus callosum, and other structural brain abnormalities. Am J Med Genet A. 2004;124:74–8.
Remes AM, Rantala H, Hiltunen JK, Leisti J, Ruokonen A. Fumarase deficiency: two siblings with enlarged cerebral ventricles and polyhydramnios in utero. Pediatrics. 1992;89:730–4.
Silan F, Yoshioka M, Kobayashi K, Simsek E, Tunc M, Alper M, Cam M, Guven A, Fukuda Y, Kinoshita M, Kocabay K, Toda T. A new mutation of the fukutin gene in a non-Japanese patient. Ann Neurol. 2003;53:392–6.
Tohyama J, Akasaka N, Saito N, Yoshimura J, Nishiyama K, Kato M. Megalencephaly and polymicrogyria with polydactyly syndrome. Pediatr Neurol. 2007;37:148–51.
Toren A, Alpern S, Berkenstadt M, Bar-Yosef O, Pras E, Katorza E. Chromosomal Microarray Evaluation of Fetal Ventriculomegaly. Isr Med Assoc J. 2020;22:639–44.
Vincent C, Kalatzis V, Compain S, Levilliers J, Slim R, Graia F, Pereira ML, Nivelon A, Croquette MF, Lacombe D, et al. A proposed new contiguous gene syndrome on 8q consists of Branchio-Oto-Renal (BOR) syndrome, Duane syndrome, a dominant form of hydrocephalus and trapeze aplasia; implications for the mapping of the BOR gene. Hum Mol Genet. 1994;3:1859–66.
Wadt K, Jensen LN, Bjerglund L, Lundstrøm M, Kirchhoff M, Kjaergaard S. Fetal ventriculomegaly due to familial submicroscopic terminal 6q deletions. Prenat Diagn. 2012;32:1212–7.
Walker ME, Lynch-Salamon DA, Milatovich A, Saal HM. Prenatal diagnosis of ring chromosome 6 in a fetus with hydrocephalus. Prenat Diagn. 1996;16:857–61.
Wang J, Zhang Z, Li Q, Zhu H, Lai Y, Luo W, Liu S, Wang H, Hu T. Prenatal diagnosis of chromosomal aberrations by chromosomal microarray analysis in foetuses with ventriculomegaly. Sci Rep. 2020;10:20765.
Welch KO, Tekin M, Nance WE, Blanton SH, Arnos KS, Pandya A. Chudley-McCullough syndrome: expanded phenotype and review of the literature. Am J Med Genet A. 2003;119:71–6.
Yoshioka M, Kuroki S. Clinical spectrum and genetic studies of Fukuyama congenital muscular dystrophy. Am J Med Genet. 1994;53:245–50.
Acknowledgements
Not applicable.
Funding
A.T.H., B.G.R., and Z.C. are supported by R21 NS135321. Z.C. is supported by R35GM138212. J.S. is supported by R01 NS110793. S.J.S. is supported by R01HD085853. K.T.K. is supported by R01 NS109358 and R01 NS111029. The views and conclusions contained in this article are soley those of the authors and should not interpreted as representing the official policies, either implied or expressed, of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
ATH: Conceptualization, Funding Acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, and Writing – review & editing. HB and RD: Investigation, Methodology, Writing – original draft, and Writing – review & editing. PQ, TJA, MCD, MG, GF, HLS, AAS, JPB, JMM, and CJR: Writing – review & editing. BGR, ZC, JMS, SJS: Funding Acquisition, Writing – review & editing. KTK: Supervision, Funding Acquisition, Writing – review & editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that the have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hale, A.T., Boudreau, H., Devulapalli, R. et al. The genetic basis of hydrocephalus: genes, pathways, mechanisms, and global impact. Fluids Barriers CNS 21, 24 (2024). https://doi.org/10.1186/s12987-024-00513-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12987-024-00513-z