Abstract
Background
Immunocompromised (IC) patients are at higher risk of more severe COVID-19 infections than the general population. Special considerations should be dedicated to such patients. We aimed to investigate the efficacy of COVID-19 vaccines based on the vaccine type and etiology as well as the necessity of booster dose in this high-risk population.
Materials and methods
We searched PubMed, Web of Science, and Scopus databases for observational studies published between June 1st, 2020, and September 1st, 2021, which investigated the seroconversion after COVID-19 vaccine administration in adult patients with IC conditions. For investigation of sources of heterogeneity, subgroup analysis and sensitivity analysis were conducted. Statistical analysis was performed using R software.
Results
According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, we included 81 articles in the meta-analysis. The overall crude prevalence of seroconversion after the first (n: 7460), second (n: 13,181), and third (n: 909, all population were transplant patients with mRNA vaccine administration) dose administration was 26.17% (95% CI 19.01%, 33.99%, I2 = 97.1%), 57.11% (95% CI: 49.22%, 64.83%, I2 = 98.4%), and 48.65% (95% CI: 34.63%, 62.79%, I2 = 94.4%). Despite the relatively same immunogenicity of mRNA and vector-based vaccines after the first dose, the mRNA vaccines induced higher immunity after the second dose. Regarding the etiologic factor, transplant patients were less likely to develop immunity after both first and second dose rather than patients with malignancy (17.0% vs 37.0% after first dose, P = 0.02; 38.3% vs 72.1% after second dose, P < 0.001) or autoimmune disease (17.0% vs 36.4%, P = 0.04; 38.3% vs 80.2%, P < 0.001). To evaluate the efficacy of the third dose, we observed an increasing trend in transplant patients after the first (17.0%), second (38.3%), and third (48.6%) dose.
Conclusion
The rising pattern of seroconversion after boosting tends to be promising. In this case, more attention should be devoted to transplant patients who possess the lowest response rate.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was firstly reported in Wuhan, Hubei Province, China, in December 2019 [1, 2]. Due to the rapid global spread of SARS-CoV-2, leading to thousands of deaths by the coronavirus disease (COVID-19), the World Health Organization (WHO) declared a pandemic on March 12th, 2020. COVID-19 has put a massive burden on the world in the case of human lives lost, economic consequences, and increasing poverty over the last two years [3]. From the first waves of the pandemic, researchers have struggled to develop an effective and safe vaccine against this virus, and some were developed and passed the trial phase expeditiously [4].
Some vaccines have been approved by the WHO so far, including messenger RNA (mRNA) vaccines, including mRNA-1273 Moderna and BNT162b2 Pfizer BioNTech, viral vector vaccines, namely AstraZeneca and Janssen Ad26.COV2.S, and inactivated virus vaccines, including Sinovac and Sinopharm [5]. Concerning immunogenicity and safety of these vaccines, preliminary reports from phase II/III and some real-world data are available to date [6,7,8,9]; however, little attention has been paid to immunocompromised (IC) patients since such patients were not included in the primary trials of the above-mentioned vaccines [10]. IC patients, including those with primary immunodeficiencies, autoimmune diseases, malignancies, human immunodeficiency virus (HIV) infection, and those taking immunosuppressive agents, are at higher risk of more severe SARS-CoV-2 infections than the general population [11,12,13,14,15]. So, special considerations should be dedicated to such patients, and investigating the efficacy and safety of vaccines against SARS-CoV-2 is crucial in these patients.
Heterogeneous studies have recently assessed the immune response against SARS-CoV-2 in IC patients after receiving the first, second, or the third dose of approved vaccines, mostly by assessing the SARS-CoV-2 anti-spike or anti-receptor-binding domain (RBD) antibodies [16,17,18]. In this systematic review and meta-analysis, we aimed to provide a more explicit vision by systematically reviewing the literature and complementing the reported clinical outcomes around the efficacy of vaccines in IC patients.
Methods
Seroconversion frequencies following vaccination were studied using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework [19] and a systematic search to locate relevant research papers.
Search strategy and databases
PubMed-MEDLINE, Scopus, and Web of Science were searched for original articles reporting the seroconversion after COVID-19 vaccine administration in adult patients with IC conditions between June 1st, 2020, and September 1st, 2021. The search terms were as follows: ((COVID-19) OR (SARS-CoV-2) OR (novel coronavirus)) AND ((vaccine) OR (vaccination) OR (vaccinated)) AND ((immunocompromised) OR (immunosuppressed) OR (corticosteroid) OR (chemotherapy) OR (cancer) OR (malignancy) OR (rheumatologic disease) OR (immunodeficiency) OR (autoimmune) OR (AIDS) OR (HIV) OR (transplant)).
Selection criteria
Studies examining the prevalence of seroconversion following COVID-19 immunization in IC patients met the inclusion criteria. The papers considered in this review satisfied the following criteria: (1) Population: studies including ≥ 30 IC patients. IC patients included those receiving chemotherapy for solid organ or hematologic malignancies, those with hereditary or acquired immunodeficiency illnesses, those with autoimmune or rheumatologic diseases, and those with other ailments (e.g., asthma) getting long-term corticosteroid treatment. (2) Intervention: immunization against COVID-19 (3) Outcomes: The primary outcome measure in this study was seroconversion in IC patients who had anti-SARS-CoV-2 spike IgG ≥ 14 days after receiving the first, second, and third doses of COVID-19 vaccinations. (4) Design of the study: we included all retrospective and prospective observational studies. The following articles were excluded from consideration: (1) reviews and editorials; (2) case reports or case series including < 30 patients; (3) partially overlapping patient cohorts; (4) non-English literature; and (5) non-human experiments. Two reviewers separately conducted a consensual evaluation of the literature.
Data extraction
Two experts independently assessed eligible studies and retrieved the following data from each included publication: author, publication date, country of origin, study design, study sample size, the definition of IC conditions, inclusion and exclusion criteria, number of IC patients, variables matched, male/female ratio, mean age, duration of disease, type and etiology of immunodeficiency and its proportion in the total population, and the type of vaccine. Any discrepancies in data extraction were handled by discussion or consultation with a third expert.
Quality assessment
We evaluated the included studies using the National Institutes of Health (NIH) quality assessment tool [20]. If an element of the criteria was inadequately addressed, not applicable, or not reported in a study, and it could not be identified indirectly, we did not allocate a score to that element. For cohort and cross-sectional studies, 11–14 was considered good, 6–10 fair, and 0–5 poor. The corresponding values were 7–9, 4–6, and 0–3 for the case series and 9–12, 5–8, and 0–4 for case-control studies, respectively.
Statistical analysis
We used the 'metaprop' function to estimate Der Simonian and Laird's pooled effect on the prevalence of seroconversion following vaccine delivery using a random-effect model. A forest plot was created to depict the summary of meta-analysis findings and heterogeneity. A funnel plot was used to check for publication bias, and Egger's regression tests were used to test for it more objectively, with a p < 0.05 deemed to suggest possible publication bias. The Cochrane Q statistic was used to assess between-study heterogeneity [21]. I2 was used to assess between-study heterogeneity, with values of 0, 25, 50, and 75% representing no, low, medium, and substantial heterogeneity, respectively [22]. A leave-one-out sensitivity analysis was used to determine the impact of a single study on the total meta-analysis estimate (Additional file 1: Figs. S1-3). The final results were given as text, tables, and figures. All computations and visualizations were carried out using R version 4.0.4 (R Core Team [2020]. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria), and STATA 16 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC) for Egger’s plots. We used following packages: “meta” (version 4.17-0), “metafor” (version 2.4-0), “dmetar” (version 0.0-9), and “tidyverse” (version 1.3.0). All forest plots, funnel plots, and the drapery plot were designed using R. A p < 0.05 was considered statistically significant.
Results
Selection of studies
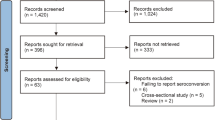
After implementing our strategy, we reached a total of 2093 research publications. Then, we screened both the titles and abstracts for relevant studies and 151 research articles were selected for full-text screening. Ultimately, 80 research publications [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102] were included in our systematic review and meta-analyses (Fig. 1; PRISMA diagram).
Study characteristics
Table 1 summarizes the characteristics of the 80 included studies, which were published in 2021. Forty [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62] studies assessed seroconversion in immunocompromised patients after the administration of the first dose of the vaccines. Also, 64 [23,24,25, 28, 30, 33,34,35,36,37,38,39,40, 42, 43, 45,46,47,48,49,50, 52, 60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101] studies were included as they evaluated seroconversion after the second injection in immunocompromised patients. Lastly, seven [28, 38, 61, 87, 97, 100, 102] studies investigated seroconversion and its prevalence after the third dose of the vaccines. Considering the type of the administered vaccine, we grouped the included studies as mRNA, vector, and inactivated virus. Moreover, regarding the etiology, studies were grouped into autoimmune, malignancy, and transplant.
Quality assessment of the included studies is presented in Additional file 1: Table S1. The majority of the studies (n = 64) were of good quality and 16 had fair quality.
Meta-analysis
First dose
Results of overall efficacy and between-group meta-analyses following the first, second, and third doses are presented in Table 2. The crude overall prevalence of seroconversion after the first dose administration in the pooled sample of 7460 individuals was 26.17% (95% CI: 19.01%; 33.99%, test of heterogeneity: I2 = 97.1%, p < 0.0001). Considering the type of vaccine, the test for subgroup differences showed significant results (p = 0.04, Fig. 2A). To investigate more, we conducted a pair-wised analysis to find whether there is a significant difference between mRNA and vector group. Accordingly, no significant difference was observed (p = 0.17). In addition, a pair-wised meta-analysis of combined group of mRNA and vector vaccines compared to inactivated group demonstrated a significant difference (30% vs. 18%, respectively; p = 0.04). Regarding the etiology, our primary analysis demonstrated a significant between-group difference (p = 0.02, Fig. 2B). Moreover, pair-wised analysis showed that the difference between malignancy and autoimmune group was not statistically significant (p = 0.95); however, malignancy vs. transplant (37% vs. 17%, p = 0.01) and autoimmune vs. transplant (36% vs. 17%, p = 0.04) exhibited statistically significant differences. Eggers' test does not indicate the presence of funnel plot asymmetry (p = 0.68); thus, the funnel plot implied no publication bias (Fig. 3A). There were no significant changes in the pooled prevalence or heterogeneity after eliminating each study in the sensitivity analysis (leave-one-out analysis) (Additional file 1: Fig. S1). As a result, none of the studies were able to explain the observed heterogeneity of results.
Second dose
Overall seroconversion prevalence following the second dosage in the pooled sample of 13,181 patients was 57.11% (95% CI: 49.22%; 64.83%, test of heterogeneity: I2 = 98.4%, p < 0.01). Given the vaccine's type, the test for subgroup differences yielded significant findings (p < 0.01, Fig. 4A). We performed a pair-wised analysis to see if the mRNA and vector groups differed significantly. As a result, a large disparity was discovered (p < 0.0001), mainly due to various patient recruitment methods. Furthermore, a significant difference was found in a pair-wised meta-analysis comparing the combined group of mRNA and vector vaccines to the inactivated group (83% vs. 76%, respectively; p = 0.04). A substantial between-groups difference was found with regards to the etiology (p < 0.01, Fig 4B). In addition, a pair-wise comparison of malignancy vs. transplant (72% vs. 38%, p < 0.001) and autoimmune vs. transplant (80% vs. 38%, p < 0.0001) groups found statistically significant differences between the analyzed groups; however, malignancy vs. autoimmune did not show any significant difference (72% vs. 80%, p = 0.34). Using Eggers' test, there was no evidence of asymmetry in the funnel plot (p = 0.06), suggesting no publication bias (Fig. 3B). After excluding each study in the sensitivity analysis (leave-one-out analysis), the aggregated prevalence and heterogeneity did not change (Additional file 1: Fig S2). For this reason, no one study could account for this wide range of outcomes.
Notably, considering immunocompromised patients due to autoimmune diseases on anti-TNF treatment, the seroconversion prevalence was estimated as 86.07% (95% CI: 63.16%; 99.23%, test of heterogeneity: I2 = 99.1%, p < 0.01).
Third dose
All the included original studies in this analysis measured seroconversion after three doses of mRNA vaccines in transplant recipients. Overall prevalence of seroconversion in the combined sample of 909 transplant patients following the third dose of vaccine was 48.65% (95% CI: 34.63%; 62.79%, test of heterogeneity: I2 = 94.4%, p < 0.0001, Fig 5). Eggers' test revealed no indication of funnel plot asymmetry (p = 0.18), confirming that there was no publication bias (Fig. 3C). The pooled prevalence and heterogeneity remained unchanged after the sensitivity analysis (leave-one-out analysis) when each study was excluded (Additional file 1: Fig. S3). Thus, no single study could explain the heterogeneity of outcomes.
Discussion
The pooled findings demonstrated a growing pattern of seroconversion rate after the administration of the second dose of COVID-19 vaccine compared to the first dose regardless of either vaccine type or the etiology of immunosuppression. Our findings also revealed a better response to mRNA vaccines compared to vector vaccines reaching significance after the administration of the second dose. In addition, transplant patients responded less robust compared to other IC patients regardless of the number of doses. It is worth mentioning that all the studies included in the pooled analysis of third-dose booster evaluated transplant patients; nevertheless, the rising pattern of seroconversion was observed even in this group of patients compared to the findings from both the first and second doses.
Viral vectors are modified viruses utilized to deliver the immunogenic part of the target virus [103]. On the other hand, mRNA vaccines deploy mRNAs coding specific viral proteins to trigger an immune response [103]. mRNA and vector vaccines seem to induce immunity with different mechanisms in healthy controls. Induction of SARS-CoV-2–specific IgG and neutralizing antibodies seems to be more pronounced with mRNA priming, while cellular immunity (including both SARS-CoV-2–specific CD4 and CD8 T cell levels) tends to be induced more robustly after vector priming [104]. However, this difference has been less prominent in IC patients [104]. Although our findings revealed higher rates of seroconversion after the second dose of mRNA vaccines, antibody assessment might be insufficient to compare immune response, and cellular immunity should be assessed as well [104].
Data regarding inactivated vaccines are rare; however, our findings show a significant difference between inactivated vaccines and combined groups of mRNA and vector vaccines. A previous report has also implicated lower efficacy of inactivated vaccines compared to vector vaccines in terms of antibody level and neutralization in immunosuppressed patients with rheumatic diseases [105]. These findings should be interpreted with caution as more studies are needed to unravel the efficacy of inactivated vaccines.
Intriguingly, a lower seroconversion rate was observed in transplant patients compared to other IC patients, even though a rising response rate was observed after boosting in this group of patients. Generally, transplant patients receive drugs that interfere with T and B cell activation and proliferation, posing an obstacle in the way of antibody generation [106]. Conspicuously, boosting seems to raise an immune response in all IC patients according to our findings, the fact which was observed with previous vaccines such as influenza [107].
Although we showed an acceptable rate of seroconversion among patients using anti-TNF therapy, reports show a persistent reduction in the titers of anti-SARS-CoV-2 spike protein antibody with time in patients with inflammatory bowel disease (IBD) who are on anti-TNF treatments [108]. While anti-TNF therapies can mitigate detrimental outcomes in severe COVID-19 due to dampening of the systemic inflammatory response, the reduction of antibodies over time might necessitate considering booster doses in these patients [108, 109].
We should mention that our study has some limitations. There was a lack of data regarding HIV and other hereditary or acquired immunodeficiency disorders and also inactivated vaccines. Besides, we included studies with both prospective and retrospective designs, which may decrease the level of evidence.
Conclusion
For the first time, this meta-analysis compared seroconversion rate after administering different types of COVID-19 vaccines in IC patients at different time points of vaccination. The rising pattern of seroconversion after boosting tends to be promising; however, more attention should be devoted to transplant patients who possess the lowest response rate.
Availability of data and materials
The authors stated that all information provided in this article could be shared.
References
Wu F, Zhao S, Yu B, Chen Y-M, Wang W, Song Z-G, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–9.
Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–3.
Ciotti M, Ciccozzi M, Terrinoni A, Jiang W-C, Wang C-B, Bernardini S. The COVID-19 pandemic. Critical Rev Clin Lab Sci. 2020;57(6):365–88.
Mehraeen E, Dadras O, Afsahi AM, Karimi A, MohsseniPour M, Mirzapour P, et al. Vaccines for COVID-19: a systematic review of feasibility and effectiveness. Infect Disord Drug Targets. 2022;22(2):e230921196758.
Shekhar R, Garg I, Pal S, Kottewar S, Sheikh AB. COVID-19 vaccine booster: to boost or not to boost. Infect Dis Rep. 2021;13(4):924–9.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–16.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603.
Knoll MD, Wonodi C. Oxford–AstraZeneca COVID-19 vaccine efficacy. The Lancet. 2021;397(10269):72–4.
Thomas SJ, Moreira ED Jr, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. N Engl J Med. 2021;385(19):1761–73.
Sonani B, Aslam F, Goyal A, Patel J, Bansal P. COVID-19 vaccination in immunocompromised patients. Clin Rheumatol. 2021;40(2):797–8.
Fung M, Babik JM. COVID-19 in immunocompromised hosts: what we know so far. Clin Infect Dis. 2021;72(2):340–50.
Tesoriero JM, Swain C-AE, Pierce JL, Zamboni L, Wu M, Holtgrave DR, et al. COVID-19 outcomes among persons living with or without diagnosed HIV infection in New York State. JAMA Netw Open. 2021;4(2):e2037069-e.
Haidar G, Mellors JW. Improving the outcomes of immunocompromised patients with COVID-19. Clin Infect Dis. 2021;73:e1397.
Salahshour F, Mehrabinejad M-M, Toosi MN, Gity M, Ghanaati H, Shakiba M, et al. Clinical and chest CT features as a predictive tool for COVID-19 clinical progress: introducing a novel semi-quantitative scoring system. Eur Radiol. 2021;31:1–11.
Yazdi NA, Ghadery AH, Seyedalinaghi SA, Jafari F, Jafari S, Hasannezad M, et al. Predictors of the chest CT score in COVID-19 patients: a cross-sectional study. Virol J. 2021;18(1):1–8.
Hall VG, Ferreira VH, Lerullo M, Ku T, Marinelli T, Majchrzak-Kita B, et al. Humoral and cellular immune response and safety of two-dose SARS-CoV-2 mRNA-1273 vaccine in solid organ transplant recipients. Am J Transpl. 2021;12:3980.
Furer V, Eviatar T, Zisman D, Peleg H, Paran D, Levartovsky D, et al. LB0003 Immunogenicity And Safety Of The BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and general population: a multicenter study. BMJ; 2021.
Mehrabi Nejad MM, Moosaie F, Dehghanbanadaki H, Haji Ghadery A, Shabani M, Tabary M, et al. Immunogenicity of COVID-19 mRNA vaccines in immunocompromised patients: a systematic review and meta-analysis. Eur J Med Res. 2021;27:1–3.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
National Heart L, Institute B. Study Quality Assessment Tools. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 2019.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111.
Addeo A, Shah PK, Bordry N, Hudson RD, Albracht B, Di Marco M, et al. Immunogenicity of SARS-CoV-2 messenger RNA vaccines in patients with cancer. Cancer Cell. 2021;39(8):1091-8.e2.
Bertrand D, Hamzaoui M, Lemée V, Lamulle J, Hanoy M, Laurent C, et al. Antibody and T cell response to SARS-CoV-2 messenger RNA BNT162b2 vaccine in kidney transplant recipients and hemodialysis patients. J Am Soc Nephrol JASN. 2021;32:2147.
Boekel L, Steenhuis M, Hooijberg F, Besten YR, van Kempen ZLE, Kummer LY, et al. Antibody development after COVID-19 vaccination in patients with autoimmune diseases in the Netherlands: a substudy of data from two prospective cohort studies. Lancet Rheumatol. 2021;3:e778.
Chevallier P, Coste-Burel M, Le Bourgeois A, Peterlin P, Garnier A, Béné MC, et al. Safety and immunogenicity of a first dose of SARS-CoV-2 mRNA vaccine in allogeneic hematopoietic stem-cells recipients. EJHaem. 2021;2:520.
Danthu C, Hantz S, Dahlem A, Duval M, Ba B, Guibbert M, et al. Humoral response after SARS-CoV-2 mRNA vaccination in a cohort of hemodialysis patients and kidney transplant recipients. J Am Soc Nephrol JASN. 2021;32:2153.
Del Bello A, Abravanel F, Marion O, Couat C, Esposito L, Lavayssière L, et al. Efficiency of a boost with a third dose of anti-SARS-CoV-2 messenger RNA-based vaccines in solid organ transplant recipients. Am J Transp Off J Am Soc Transp Am Soc Transp Surg. 2021;22:322.
Easdale S, Shea R, Ellis L, Bazin J, Davis K, Dallas F, et al. Serologic responses following a single dose of SARS-Cov-2 vaccination in allogeneic stem cell transplantation recipients. Transp Cell Ther. 2021;27:880.e1.
Firket L, Descy J, Seidel L, Bonvoisin C, Bouquegneau A, Grosch S, et al. Serological response to mRNA SARS-CoV-2 BNT162b2 vaccine in kidney transplant recipients depends on prior exposure to SARS-CoV-2. Am J Transp Off J Am Soc Transp Am Soc Transp Surg. 2021;21:3806.
Gavriatopoulou M, Terpos E, Kastritis E, Briasoulis A, Gumeni S, Ntanasis-Stathopoulos I, et al. Low neutralizing antibody responses in WM, CLL and NHL patients after the first dose of the BNT162b2 and AZD1222 vaccine. Clin Exp Med. 2022;22:319.
Ghandili S, Schoenlein M, Luetgehetmann M, Zur Wiesch JS, Becher H, Bokemeyer C, et al. Post-vaccination anti-SARS-CoV-2-antibody response in patients with multiple myeloma correlates with low CD19+B-lymphocyte count and anti-CD38 treatment. Cancers. 2021;13(15):3800.
Goshen-Lago T, Waldhorn I, Holland R, Szwarcwort-Cohen M, Reiner-Benaim A, Shachor-Meyouhas Y, et al. Serologic status and toxic effects of the SARS-CoV-2 BNT162b2 vaccine in patients undergoing treatment for cancer. JAMA Oncol. 2021;7:1507.
Hall VG, Ferreira VH, Ierullo M, Ku T, Marinelli T, Majchrzak-Kita B, et al. Humoral and cellular immune response and safety of two-dose SARS-CoV-2 mRNA-1273 vaccine in solid organ transplant recipients. Am J Transplant. 2021;21:3980.
Havlin J, Svorcova M, Dvorackova E, Lastovicka J, Lischke R, Kalina T, et al. Immunogenicity of BNT162b2 mRNA COVID-19 vaccine and SARS-CoV-2 infection in lung transplant recipients. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2021;40(8):754–8.
Herrera S, Colmenero J, Pascal M, Escobedo M, Castel MA, Sole-Gonzalez E, et al. Cellular and humoral immune response after mRNA-1273 SARS-CoV-2 vaccine in liver and heart transplant recipients. Am J Transplant. 2021;21:3971.
Itzhaki Ben Zadok O, Shaul AA, Ben-Avraham B, Yaari V, Ben Zvi H, Shostak Y, et al. Immunogenicity of the BNT162b2 mRNA vaccine in heart transplant recipients: a prospective cohort study. Eur J Heart Failure. 2021;2021(23):1555.
Kamar N, Abravanel F, Marion O, Couat C, Izopet J, Del Bello A. Three doses of an mRNA Covid-19 vaccine in solid-organ transplant recipients. N Engl J Med. 2021;385(7):661–2.
Kennedy NA, Lin S, Goodhand JR, Chanchlani N, Hamilton B, Bewshea C, et al. Infliximab is associated with attenuated immunogenicity to BNT162b2 and ChAdOx1 nCoV-19 SARS-CoV-2 vaccines in patients with IBD. Gut. 2021;70:1884.
Malard F, Gaugler B, Gozlan J, Bouquet L, Fofana D, Siblany L, et al. Weak immunogenicity of SARS-CoV-2 vaccine in patients with hematologic malignancies. Blood Cancer J. 2021;11(8):1.
Mazzola A, Todesco E, Drouin S, Hazan F, Marot S, Thabut D, et al. Poor antibody response after two doses of SARS-CoV-2 vaccine in transplant recipients. Clin Infect Dis Off Publ Infect Dis Soc Am. 2021;74:1093.
Medeiros-Ribeiro AC, Aikawa NE, Saad CGS, Yuki EFN, Pedrosa T, Fusco SRG, et al. Immunogenicity and safety of the CoronaVac inactivated vaccine in patients with autoimmune rheumatic diseases: a phase 4 trial. Nat Med. 2021;27:1744.
Monin L, Laing AG, Munoz-Ruiz M, McKenzie DR, Del Barrio ID, Alaguthurai T, et al. Safety and immunogenicity of one versus two doses of the COVID-19 vaccine BNT162b2 for patients with cancer: interim analysis of a prospective observational study. Lancet Oncol. 2021;22(6):765–78.
Palich R, Veyri M, Marot S, Vozy A, Gligorov J, Maingon P, et al. Weak immunogenicity after a single dose of SARS-CoV-2 mRNA vaccine in treated cancer patients. Ann Oncol Off J Eur Soc Med Oncol. 2021;32(8):1051–3.
Pimpinelli F, Marchesi F, Piaggio G, Giannarelli D, Papa E, Falcucci P, et al. Fifth-week immunogenicity and safety of anti-SARS-CoV-2 BNT162b2 vaccine in patients with multiple myeloma and myeloproliferative malignancies on active treatment: preliminary data from a single institution. J Hematol Oncol. 2021;14(1):81.
Prendecki M, Clarke C, Edwards H, McIntyre S, Mortimer P, Gleeson S, et al. Humoral and T-cell responses to SARS-CoV-2 vaccination in patients receiving immunosuppression. Ann Rheum Dis. 2021;80:1322.
Reuken PA, Andreas N, Grunert PC, Glöckner S, Kamradt T, Stallmach A. T cell response after SARS-CoV-2 vaccination in immunocompromised patients with inflammatory bowel disease. J Crohn’s Colitis. 2021;16:251.
Schramm R, Costard-Jackle A, Rivinius R, Fischer B, Muller B, Boeken U, et al. Poor humoral and T-cell response to two-dose SARS-CoV-2 messenger RNA vaccine BNT162b2 in cardiothoracic transplant recipients. Clin Res Cardiol. 2021;110(8):1142–9.
Strauss AT, Hallett AM, Boyarsky BJ, Ou MT, Werbel WA, Avery RK, et al. Antibody response to SARS-CoV-2 messenger RNA vaccines in liver transplant recipients. Liver Transplant Off Publ Am Assoc Study Liver Dis Int Liver Transplant Soc. 2021;27:1852.
Terpos E, Gavriatopoulou M, Ntanasis-Stathopoulos I, Briasoulis A, Gumeni S, Malandrakis P, et al. The neutralizing antibody response post COVID-19 vaccination in patients with myeloma is highly dependent on the type of anti-myeloma treatment. Blood Cancer J. 2021;11(8):1.
Terpos E, Zagouri F, Liontos M, Sklirou AD, Koutsoukos K, Markellos C, et al. Low titers of SARS-CoV-2 neutralizing antibodies after first vaccination dose in cancer patients receiving checkpoint inhibitors. J Hematol Oncol. 2021;14(1):86.
Thakkar A, Gonzalez-Lugo JD, Goradia N, Gali R, Shapiro LC, Pradhan K, et al. Seroconversion rates following COVID-19 vaccination among patients with cancer. Cancer Cell. 2021;39(8):1081-90.e2.
Yi SG, Knight RJ, Graviss EA, Moore LW, Nguyen DT, Ghobrial RM, et al. Kidney transplant recipients rarely show an early antibody response following the first COVID-19 vaccine administration. Transplantation. 2021;105(7):e72–3.
Benotmane I, Gautier-Vargas G, Cognard N, Olagne J, Heibel F, Braun-Parvez L, et al. Weak anti-SARS-CoV-2 antibody response after the first injection of an mRNA COVID-19 vaccine in kidney transplant recipients. Kidney Int. 2021;99(6):1487–9.
Boyarsky BJ, Ruddy JA, Connolly CM, Ou MT, Werbel WA, Garonzik-Wang JM, et al. Antibody response to a single dose of SARS-CoV-2 mRNA vaccine in patients with rheumatic and musculoskeletal diseases. Ann Rheum Dis. 2021;80:1098.
Boyarsky BJ, Werbel WA, Avery RK, Tobian AAR, Massie AB, Segev DL, et al. Immunogenicity of a single dose of SARS-CoV-2 messenger RNA vaccine in solid organ transplant recipients. JAMA. 2021;325(17):1784–6.
Boyarsky BJ, Barbur I, Chiang TP, Ou MT, Greenberg RS, Teles AT, et al. SARS-CoV-2 messenger RNA vaccine immunogenicity in solid organ transplant recipients with prior COVID-19. Transplantation. 2021;105:e270.
Chavarot N, Ouedrani A, Marion O, Leruez-Ville M, Vilain E, Baaziz M, et al. Poor anti-SARS-CoV-2 humoral and T-cell responses after 2 injections of mRNA vaccine in kidney transplant recipients treated with belatacept. Transplantation. 2021;105(9):e94–5.
Harrington P, de Lavallade H, Doores KJ, O’Reilly A, Seow J, Graham C, et al. Single dose of BNT162b2 mRNA vaccine against SARS-CoV-2 induces high frequency of neutralising antibody and polyfunctional T-cell responses in patients with myeloproliferative neoplasms. Leukemia. 2021;35:1–5.
Ou MT, Boyarsky BJ, Chiang TPY, Bae S, Werbel WA, Avery RK, et al. Immunogenicity and reactogenicity After SARS-CoV-2 mRNA vaccination in kidney transplant recipients taking belatacept. Transplantation. 2021;105(9):2119–23.
Stumpf J, Tonnus W, Paliege A, Rettig R, Steglich A, Gembardt F, et al. Cellular and humoral immune responses after three doses of BNT162b2 mRNA SARS-Cov-2 vaccine in kidney transplant. Transplantation. 2021;105:e267.
Benotmane I, Gautier-Vargas G, Cognard N, Olagne J, Heibel F, Braun-Parvez L, et al. Low immunization rates among kidney transplant recipients who received 2 doses of the mRNA-1273 SARS-CoV-2 vaccine. Kidney Int. 2021;99(6):1498–500.
Agbarya A, Sarel I, Ziv-Baran T, Agranat S, Schwartz O, Shai A, et al. Efficacy of the mRNA-Based BNT162b2 COVID-19 vaccine in patients with solid malignancies treated with anti-neoplastic drugs. Cancers. 2021;13(16):4191.
Agha ME, Blake M, Chilleo C, Wells A, Haidar G. Suboptimal response to coronavirus disease 2019 messenger RNA vaccines in patients with hematologic malignancies: a need for vigilance in the postmasking era. Open forum infectious diseases. 2021;8(7).
Ammitzbøll C, Bartels LE, Bøgh Andersen J, Risbøl Vils S, Elbaek Mistegård C, Dahl Johannsen A, et al. Impaired antibody response to the BNT162b2 messenger RNA coronavirus disease 2019 vaccine in patients with systemic lupus erythematosus and rheumatoid arthritis. ACR Open Rheumatol. 2021;3:622.
Braun-Moscovici Y, Kaplan M, Braun M, Markovits D, Giryes S, Toledano K, et al. Disease activity and humoral response in patients with inflammatory rheumatic diseases after two doses of the Pfizer mRNA vaccine against SARS-CoV-2. Ann Rheum Dis. 2021;80:1317.
Cao J, Liu X, Muthukumar A, Gagan J, Jones P, Zu Y. Poor humoral response in solid organ transplant recipients following complete mRNA SARS-CoV-2 vaccination. Clin Chem. 2021;68:251.
Chiang TP, Connolly CM, Ruddy JA, Boyarsky BJ, Alejo JL, Werbel WA, et al. Antibody response to the Janssen/Johnson & Johnson SARS-CoV-2 vaccine in patients with rheumatic and musculoskeletal diseases. Ann Rheum Dis. 2021;80:1365.
Cohen D, Hazut Krauthammer S, Cohen YC, Perry C, Avivi I, Herishanu Y, et al. Correlation between BNT162b2 mRNA Covid-19 vaccine-associated hypermetabolic lymphadenopathy and humoral immunity in patients with hematologic malignancy. Eur J Nucl Med Mol Imaging. 2021;48:1–10.
Cucchiari D, Egri N, Bodro M, Herrera S, Del Risco-Zevallos J, Casals-Urquiza J, et al. Cellular and humoral response after MRNA-1273 SARS-CoV-2 vaccine in kidney transplant recipients. Am J Transplant. 2021;21(8):2727–39.
Ehmsen S, Asmussen A, Jeppesen SS, Nilsson AC, Østerlev S, Vestergaard H, et al. Antibody and T cell immune responses following mRNA COVID-19 vaccination in patients with cancer. Cancer Cell. 2021;39(8):1034–6.
Eliakim-Raz N, Massarweh A, Stemmer A, Stemmer SM. Durability of response to SARS-CoV-2 BNT162b2 vaccination in patients on active anticancer treatment. JAMA Oncol. 2021;7:1716.
Furer V, Eviatar T, Zisman D, Peleg H, Paran D, Levartovsky D, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann Rheum Dis. 2021;80:1330.
Grupper A, Rabinowich L, Schwartz D, Schwartz IF, Ben-Yehoyada M, Shashar M, et al. Reduced humoral response to mRNA SARS-CoV-2 BNT162b2 vaccine in kidney transplant recipients without prior exposure to the virus. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2021;21(8):2719–26.
Hagin D, Freund T, Navon M, Halperin T, Adir D, Marom R, et al. Immunogenicity of Pfizer-BioNTech COVID-19 vaccine in patients with inborn errors of immunity. J Allergy Clin Immunol. 2021;148:739.
Haskin O, Ashkenazi-Hoffnung L, Ziv N, Borovitz Y, Dagan A, Levi S, et al. Serological response to the BNT162b2 COVID-19 mRNA vaccine in adolescent and young adult kidney transplant recipients. Transplantation. 2021;105:e226.
Herishanu Y, Avivi I, Aharon A, Shefer G, Levi S, Bronstein Y, et al. Efficacy of the BNT162b2 mRNA COVID-19 vaccine in patients with chronic lymphocytic leukemia. Blood. 2021;137(23):3165–73.
Herzog Tzarfati K, Gutwein O, Apel A, Rahimi-Levene N, Sadovnik M, Harel L, et al. BNT162b2 COVID-19 vaccine is significantly less effective in patients with hematologic malignancies. Am J Hematol. 2021;96:1195.
Hod T, Ben-David A, Olmer L, Levy I, Ghinea R, Mor E, et al. Humoral response of renal transplant recipients to the BNT162b2 SARS-CoV-2 mRNA vaccine using both RBD IgG and neutralizing antibodies. Transplantation. 2021;105:e234.
Holden IK, Bistrup C, Nilsson AC, Hansen JF, Abazi R, Davidsen JR, et al. Immunogenicity of SARS-CoV-2 mRNA vaccine in solid organ transplant recipients. J Intern Med. 2021;290:1264.
Iacono D, Cerbone L, Palombi L, Cavalieri E, Sperduti I, Cocchiara RA, et al. Serological response to COVID-19 vaccination in patients with cancer older than 80 years. J Geriatr Oncol. 2021;12:1253.
Karacin C, Eren T, Zeynelgil E, Imamoglu GI, Altinbas M, Karadag I, et al. Immunogenicity and safety of the CoronaVac vaccine in patients with cancer receiving active systemic therapy. Future Oncol (London, England). 2021;17:4447.
Korth J, Jahn M, Dorsch O, Anastasiou OE, Sorge-Hadicke B, Eisenberger U, et al. Impaired humoral response in renal transplant recipients to SARS-CoV-2 vaccination with BNT162b2 (Pfizer-BioNTech). Viruses-Basel. 2021;13(5):756.
Marinaki S, Adamopoulos S, Degiannis D, Roussos S, Pavlopoulou ID, Hatzakis A, et al. Immunogenicity of SARS-CoV-2 BNT162b2 vaccine in solid organ transplant recipients. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2021;21(8):2913–5.
Massarweh A, Eliakim-Raz N, Stemmer A, Levy-Barda A, Yust-Katz S, Zer A, et al. Evaluation of seropositivity following BNT162b2 messenger RNA vaccination for SARS-CoV-2 in patients undergoing treatment for cancer. JAMA Oncol. 2021;7:1133.
Narasimhan M, Mahimainathan L, Clark AE, Usmani A, Cao J, Araj E, et al. Serological response in lung transplant recipients after two doses of SARS-CoV-2 mRNA vaccines. Vaccines. 2021;9(7):708.
Noble J, Langello A, Bouchut W, Lupo J, Lombardo D, Rostaing L. Immune response post-SARS-CoV-2 mRNA vaccination in kidney-transplant recipients receiving belatacept. Transplantation. 2021;105:e259.
Peled Y, Ram E, Lavee J, Sternik L, Segev A, Wieder-Finesod A, et al. BNT162b2 vaccination in heart transplant recipients: clinical experience and antibody response. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2021;40(8):759–62.
Rabinowich L, Grupper A, Baruch R, Ben-Yehoyada M, Halperin T, Turner D, et al. Low immunogenicity to SARS-CoV-2 vaccination among liver transplant recipients. J Hepatol. 2021;75(2):435–8.
Rashidi-Alavijeh J, Frey A, Passenberg M, Korth J, Zmudzinski J, Anastasiou OE, et al. Humoral response to SARS-Cov-2 vaccination in liver transplant recipients—a single-center experience. Vaccines. 2021;9(7):738.
Rincon-Arevalo H, Choi M, Stefanski AL, Halleck F, Weber U, Szelinski F, et al. Impaired humoral immunity to SARS-CoV-2 BNT162b2 vaccine in kidney transplant recipients and dialysis patients. Sci Immunol. 2021;6(60):eabj1031.
Rozen-Zvi B, Yahav D, Agur T, Zingerman B, Ben-Zvi H, Atamna A, et al. Antibody response to SARS-CoV-2 mRNA vaccine among kidney transplant recipients: a prospective cohort study. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2021;27(8):1173.e1-e4.
Ruddy JA, Connolly CM, Boyarsky BJ, Werbel WA, Christopher-Stine L, Garonzik-Wang J, et al. High antibody response to two-dose SARS-CoV-2 messenger RNA vaccination in patients with rheumatic and musculoskeletal diseases. Ann Rheum Dis. 2021;80:1351.
Sattler A, Schrezenmeier E, Weber UA, Potekhin A, Bachmann F, Straub-Hohenbleicher H, et al. Impaired humoral and cellular immunity after SARS-CoV-2 BNT162b2 (tozinameran) prime-boost vaccination in kidney transplant recipients. J Clin Investig. 2021;131(14).
Seyahi E, Bakhdiyarli G, Oztas M, Kuskucu MA, Tok Y, Sut N, et al. Antibody response to inactivated COVID-19 vaccine (CoronaVac) in immune-mediated diseases: a controlled study among hospital workers and elderly. Rheumatol Int. 2021;41(8):1429–40.
Stumpf J, Siepmann T, Lindner T, Karger C, Schwöbel J, Anders L, et al. Humoral and cellular immunity to SARS-CoV-2 vaccination in renal transplant versus dialysis patients: a prospective, multicenter observational study using mRNA-1273 or BNT162b2 mRNA vaccine. Lancet Region Health Eur. 2021;9:100178.
Werbel WA, Boyarsky BJ, Ou MT, Massie AB, Tobian AAR, Garonzik-Wang JM, et al. Safety and immunogenicity of a third dose of SARS-CoV-2 vaccine in solid organ transplant recipients: a case series. Ann Intern Med. 2021;174:1330.
Boyarsky BJ, Chiang TP, Ou MT, Werbel WA, Massie AB, Segev DL, et al. Antibody response to the janssen COVID-19 vaccine in solid organ transplant recipients. Transplantation. 2021;105(8):e82–3.
Boyarsky BJ, Werbel WA, Avery RK, Tobian AAR, Massie AB, Segev DL, et al. Antibody response to 2-dose SARS-CoV-2 mRNA vaccine series in solid organ transplant recipients. JAMA. 2021;325(21):2204–6.
Chavarot N, Morel A, Leruez-Ville M, Villain E, Divard G, Burger C, et al. Weak antibody response to 3 doses of mRNA vaccine in kidney transplant recipients treated with belatacept. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2021;21:4043.
Geisen UM, Berner DK, Tran F, Sümbül M, Vullriede L, Ciripoi M, et al. Immunogenicity and safety of anti-SARS-CoV-2 mRNA vaccines in patients with chronic inflammatory conditions and immunosuppressive therapy in a monocentric cohort. Ann Rheum Dis. 2021;80:1306.
Benotmane I, Gautier G, Perrin P, Olagne J, Cognard N, Fafi-Kremer S, et al. Antibody response after a third dose of the mRNA-1273 SARS-CoV-2 vaccine in kidney transplant recipients with minimal serologic response to 2 doses. JAMA. 2021.
Negahdaripour M, Shafiekhani M, Moezzi SMI, Amiri S, Rasekh S, Bagheri A, et al. Administration of COVID-19 Vaccines in immunocompromised patients. Int Immunopharmacol. 2021;99:108021.
Schmidt T, Klemis V, Schub D, Schneitler S, Reichert MC, Wilkens H, et al. Cellular immunity predominates over humoral immunity after homologous and heterologous mRNA and vector-based COVID-19 vaccine regimens in solid organ transplant recipients. Am J Transplant. 2021;21:3990.
Shenoy P, Ahmed S, Paul A, Cherian S, Vijayan A, Babu SA, et al. Inactivated vaccines may not provide adequate protection in immunosuppressed patients with rheumatic diseases. Ann Rheum Dis. 2022;81(2):295–6.
Caillard S, Thaunat O. COVID-19 vaccination in kidney transplant recipients. Nat Rev Nephrol. 2021;17(12):785–7.
Felldin M, Andersson B, Studahl M, Svennerholm B, Friman V. Antibody persistence 1 year after pandemic H1N1 2009 influenza vaccination and immunogenicity of subsequent seasonal influenza vaccine among adult organ transplant patients. Transpl Int. 2014;27(2):197–203.
Alexander JL, Kennedy NA, Ibraheim H, Anandabaskaran S, Saifuddin A, Seoane RC, et al. COVID-19 vaccine-induced antibody responses in immunosuppressed patients with inflammatory bowel disease (VIP): a multicentre, prospective, case-control study. Lancet Gastroenterol Hepatol. 2022;7:342.
Chhibba T, Targownik LE. Is the attenuated humoral response to COVID-19 vaccination in anti-TNF users relevant? Lancet Gastroenterol Hepatol. 2022;7:280.
Acknowledgements
Not applicable
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
The conception and design of the study: MM, HD, SS, NR; acquisition of data: MM, AH, AA, MS, MT; analysis and drafting the article: MM, PS, HD, MT; revising it critically for important intellectual content: SS, MM, NR, HD, FM; final approval of the version to be submitted: NR, SS. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that there is no conflict of interest regarding the publication of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Figure S1
. Results of Sensitivity analysis (leave-one-out analysis) of the First Dose meta-analysis (I2 and effect size plot). Figure S2. Results of Sensitivity analysis (leave-one-out analysis) of the Second Dose meta-analysis (I2 and effect size plot). Figure S3. Results of Sensitivity analysis (leave-one-out analysis) of the Third Dose meta-analysis (I2 and effect size plot). Table S1. Quality assessment using NIH tool.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mehrabi Nejad, MM., Shobeiri, P., Dehghanbanadaki, H. et al. Seroconversion following the first, second, and third dose of SARS-CoV-2 vaccines in immunocompromised population: a systematic review and meta-analysis. Virol J 19, 132 (2022). https://doi.org/10.1186/s12985-022-01858-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-022-01858-3