Abstract
Background
Multiple studies have provided evidence of suboptimal or poor immune responses to SARS-CoV-2 vaccines in recipients of hematopoietic stem cell transplantation (HSCT) and chimeric antigen receptor-T (CAR-T) cell therapy compared to healthy individuals. Given the dynamic nature of SARS-CoV2, characterized by the emergence of many viral variations throughout the general population, there is ongoing discussion regarding the optimal quantity and frequency of additional doses required to sustain protection against SARS-CoV2 especially in this susceptible population. This systematic review and meta-analysis investigated the immune responses of HSCT and CAR-T cell therapy recipients to additional doses of the SARS-CoV-2 vaccines.
Methods
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, the study involved a comprehensive search across PubMed, Scopus, Web of Science Core Collection, Embase, and Cochrane Biorxiv and medRxiv, focusing on the serological responses to the third and fourth vaccine doses in HSCT and CAR-T cell patients.
Results
This study included 32 papers, with 31 qualifying for the meta-analysis. Results showed that after the third dose, the seroconversion rate in HSCT and CAR-T cell therapy recipients who didn’t respond to the second dose was 46.10 and 17.26%, respectively. Following the fourth dose, HSCT patients had a seroconversion rate of 27.23%. Moreover, post-third-dose seropositivity rates were 87.14% for HSCT and 32.96% for CAR-T cell therapy recipients. Additionally, the seropositive response to the fourth dose in the HSCT group was 90.04%.
Conclusion
While a significant portion of HSCT recipients developed antibodies after additional vaccinations, only a minority of CAR-T cell therapy patients showed a similar response. This suggests that alternative vaccination strategies are needed to protect these vulnerable groups effectively. Moreover, few studies have reported cellular responses to additional SARS-CoV-2 vaccinations in these patients. Further studies evaluating cellular responses are required to determine a more precise assessment of immunogenicity strength against SARS-CoV-2 after additional doses.
Similar content being viewed by others
Introduction
As severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) evolves, giving rise to highly transmissible new variants of concern, and the possibility of the pandemic transitioning into a more endemic state becomes apparent, populations at high risk, including those with compromised immune systems, will continue to face a significant risk of developing severe disease [1]. Vaccination has proven to be a highly successful strategy in decreasing the incidence of Coronavirus disease of 2019 (COVID-19) and its associated complications, particularly severe illness and death caused by the disease [2, 3].
Patients who have undergone hematopoietic stem cell transplantation (HSCT) or different types of immune cell therapies experience a range of disease-related and therapeutic-induced immunosuppression, which may result in reduced capacity to develop a robust immune response by vaccination [4]. While it is presumed that immune responses to SARS-CoV-2 vaccines may vary after transplantation or other types of cell therapy, many scientific organizations recommend administering the vaccine as early as 3 months following stem cell infusion or immune cell therapy [5].
Multiple studies have provided evidence of suboptimal or poor immune responses to SARS-CoV-2 vaccines in recipients of HSCT and chimeric antigen receptor (CAR)-T cell therapy compared to healthy individuals [5,6,7,8,9,10,11]. Several factors were suggested for inadequate immune response, such as the duration of time between HSCT and vaccination, the occurrence of graft-versus-host disease (GVHD), and the application of anti-CD20 therapies [10, 12]. The results of studies indicate that an additional dose of vaccination is necessary, specifically for populations at higher risk, to provide a heightened level of protection against SARS-CoV-2 or to enhance the already suboptimal immune response [13,14,15,16,17]. Moreover, given the dynamic nature of SARS-CoV2, characterized by the emergence of many viral variations throughout the general population, there is ongoing discussion regarding the optimal quantity and frequency of additional doses required to sustain protection against SARS-CoV2. This is due to the recognized phenomenon of vaccine efficacy diminishing over time [18, 19]. Therefore, there is an urgent need to obtain extensive information on the efficacy of additional doses of SARS-CoV-2 vaccines to improve protection strategies in these susceptible groups.
The purpose of this study was to explore immunogeneity to additional doses of SARS-CoV-2 vaccine in patients who have undergone HSCT and CAR-T cell therapy through a systematic review and meta-analysis.
Method and materials
To evaluate the serologic response of HSCT and CAR-T cell therapy recipients to additional doses of COVID-19 vaccines, the current study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20] (Tables S1 and S2, see Additional file 1). Our protocol was registered on PROSPERO (CRD42022323375; February 5, 2023).
Search strategy
We conducted a comprehensive search in PubMed, Scopus, Web of Science Core Collection, Embase, and cochrane Biorxiv and medRxiv from inception until September 2023. Terms related to COVID-19 vaccines, hematopoietic stem cell transplantation, chimeric antigen receptor T-cell therapy and adoptive T cell therapy. The search strategy was developed using a combination of Mesh term searching and title-abstract searching, incorporating AND and OR operators. (Table S3, see Additional file 1).
Eligibility criteria
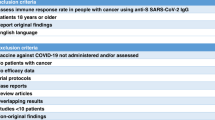
The inclusion criteria were established following the PICOS framework as outlined below:
Population
Adults with hematologic malignancies necessitating interventions, including HSCT and CAR-T cell therapy.
Intervention
Studies involving individuals who have received at least one additional dose (third and fourth dose) of the COVID-19 vaccine following cell therapy.
Comparison
The comparison group was the patients who received the previous doses.
Outcome
The primary outcome of interest focuses on the seroconversion in response to additional COVID-19 vaccine doses among patients who did not respond to the previous doses. Secondary outcomes include humoral response after third and fourth dose and assessing the difference in seropositivity rate following the additional dose compared to the previous dose, which is defined as the seropositive rate difference, and cellular response after the third dose.
Study design
Both retrospective and prospective studies and also clinical trials were eligible for inclusion in the analysis. Only studies published in English were considered. Case reports, case series were excluded. Two reviewers meticulously assessed these eligibility criteria to ensure alignment with the research question and the population of interest, thereby preventing the inadvertent omission of any critical studies.
Risk of bias assessment
For conducting the quality assessment, we utilized JBI Tools for the evaluation of quasi experimental studies and randomized controlled trials (RCTs) [21]. These tools consist of sets of 9 and 13 questions, respectively, dedicated to assessing the quality of both the execution and reporting of studies employing these research designs. The scoring in this checklist is based on a scale comprising “No,” “Yes,” “Unclear,” and “Not Applicable” categories. It’s worth noting that, while there isn’t a standardized reference guide for scoring the checklist questions, we devised a scoring system consistently. Specifically, we assigned a score of 1 for responses indicating “Yes,” 0.5 for responses indicating “Unclear,” and 0 for responses indicating “No” for each question. Subsequently, the Total JBI score for each study was calculated by summing the scores derived from all the answers and then dividing this sum by the total number of questions.
Studies that attained a Total JBI score of 0.75 or higher were categorized as low-risk studies, while those with a JBI score below 0.75 were identified as high-risk of bias studies.
Data extraction
Two authors (LSA and MRT) independently screened the titles and abstracts to exclude studies that did not meet the inclusion criteria and resolved differences through discussion. Data were gathered from eligible research by two professional reviewers (MA and MA), with a focus on important factors such as the name of the authors, release year, and location of the study. Furthermore, we meticulously gathered data regarding the study design, distinguishing between HSCT and CAR-T cell therapy as cell therapy types, and determining the mean or median age of participants. We also collected the percentage of female participants and recorded the time elapsed since receiving the vaccine following cell therapy. Additionally, we documented the type of primary and additional vaccine doses, the number of additional doses and the time elapsed since the previous vaccine dose was administered. Furthermore, we ensured the collection of the requisite data for calculating the seroconversion rate, seropositivity rate after the additional doses, the difference in seropositivity rates before and after the additional doses, the seropositivity rate of the immune responses to previous doses, and cellular response after the third dose. In the event that essential data were not reported, we took note of the contact information for the study authors, allowing for future inquiries.
Statistical analysis
We employed a Dersimonian and Laird random effects model with a double arcsine transformation to determine the overall seropositive rate. In instances where a single study yielded multiple effect sizes, the assessment of the overall response to additional vaccine doses involved calculating a pooled estimate through a Generalized Linear Mixed Model (GLMM) meta-analysis with a logit transformation. Results were presented along with 95% confidence intervals, determined using the exact method for confidence interval calculation. To evaluate heterogeneity, the I2 and Tau2 threshold were applied. Furthermore, we conducted a subgroup analysis to investigate variations based on relevant variables of interest. Publication bias was assessed using Egger’s test and a doiplot [22]. Data analysis was conducted using the Metaprop one and admeten Stata packages [23]. Forest plots were used to illustrate pooled effect size from meta-analysis of multiple quantitative studies.
Results
Study selection
Upon applying the search strategy designed, we attained a cumulative total of 2327 records from the database. After removal of duplicates, titles and abstracts were scanned to identify relevant publications. Full texts of 54 articles were thoroughly evaluated. Finally, 32 studies were included in this systematic review and 31 studies were eligible for meta-analysis based on the inclusion and exclusion criteria (Fig. 1). Overall, 1273 allo-, 218 auto-, 260 combined allo-HSCT and auto-HSCT (without exact report of the number or requisite data of allo- and auto-HSCT recipients separately), and 85 CAR-T cell therapy recipients who had received three-dose SARS-CoV-2 vaccination were included in this study. Moreover, 157 allo-, 10 combined allo- and auto-HSCT, and 3 CAR-T cell therapy recipients who were vaccinated with a fourth dose were also included in this study. Additionally, 18 studies employed a prospective design, while 7 studies utilized a retrospective approach. Furthermore, 6 studies were non-randomized controlled trials, and only one was RCT.
Characteristics of the included studies
24 studies enrolled allo-HSCT participants, while only 6 included auto-HSCT and 6 studies a combination of allo- and auto-HSCT recipients, respectively. Furthermore, five studies that were conducted on CAR-T cell therapy subjects were also included in this study. The patients’ age ranged from 16 to 81 years old. Table 1 summarizes the main characteristics of the studies incorporated. Of the total studies, six studies had reported immunologic response to 4th dose (only one study in CAR-T cell therapy recipients). All the studies administered mRNA vaccines (BNT162b2 or mRNA-1273) for booster immunization, except for three studies which used either recombinant protein (Receptor-binding domain (RBD)–tetanus toxoid (TT)-conjugated SARS-CoV-2 vaccine (Soberana 2)) [24, 25] or inactivated virus vaccines (CoronaVac) [25]. Table 2 provides additional information regarding these investigations.
Cellular responses were reported only after third dose vaccinations. Intracellular cytokine staining was utilized as an indicator to evaluate cellular responses, with the markers analyzed across the studies showing significant variation. Therefore, we decided not to perform a meta-analysis on cellular responses to SARS-CoV-2 vaccines’ additional doses.
Seroconversion following the third or fourth dose
Roughly, between 0 and 100% of HSCT recipients who received two doses of the vaccine and were initially seronegative, subsequently developed a positive serological response after receiving a third dose. The overall seroconversion rate following the third dose administration in HSCT group who had not responded to the second dose was 46.10% (95% CI: 34.49–57.90%, Tau2 = 0.13; P = 0.00) (Fig. 2). The post-fourth dose analysis, also, unveiled a pooled seroconversion rate of 27.23% (95% CI: 7.19–52.12%, Tau2 = 0.06; P = 0.22) in this subset of individuals who tested negative after the third vaccination (Fig. 3). Additionally, the overall seroconversion rate subsequent to the third dose in CAR-T cell group exhibiting a negative humoral response to the second dose turned out to be 17.26% (95% CI: 7.84–28.60%, Tau2 = 0.00; P = 0.54) (Fig. 4).
Humoral response after third or fourth dose
The pooled humoral response for HSCT recipients following the third dose administration was 87.14% (95% CI: 82.34–90.78%, Tau2 = 0.79; P = 0.00) (Fig. 5). Specifically, allo-HSCT recipients showed an 85.41% (95% CI: 80.40–89.31%, Tau2 = 0.50; P = 0.00) response rate, which was slightly diminished than auto-HSCT and combined allo- and auto-HSCT groups with an overall response rate of 89.96% (95% CI: 75.14–96.37%, Tau2 = 1.23; P = 0.00) and 90.54% (95% CI: 75.23–96.79%, Tau2 = 1.55; P = 0.00), respectively (Fig. 5). Furthermore, our analysis demonstrated an overall seropositive rate of 90.04% (95% CI: 78.68–97.85%, Tau2 = 0.05; P = 0.05) following the administration of fourth dose of SARS-CoV2 vaccines in patients who had received HSCT (Fig. 6). Notably, CAR-T cell patients displayed an overall seropositivity rate of 32.96% (95% CI: 22.23–44.47%, Tau2 = 0.00; P = 0.90) after receiving the third vaccine dose (Fig. 7).
Seropositive difference rate after three or four vaccines
Our meta-analysis revealed an increase of overall seropositive response by 11% (95% CI: 7–15%, I2 = 70.1%; P = 0.91) after the administration of third dose when compared to the second dose in HSCT recipients (Fig. S1, see Additional file 2). The rate of elevated pooled humoral response after receiving the third dose in allo-, auto-, and combined allo- and auto-HSCT recipients was 12% (95% CI: 7–17%, I2 = 61.7%), 12% (95% CI: -3-27%, I2 = 88.2%), and 7% (95% CI: -1-15, I2 = 53.6%), respectively (Fig. S1). Moreover, the overall seropositive rate of patients transplanted with HSCs was improved by 6% (95% CI: 0–13%, Tau2 = 0.00; P = 0.90) post-fourth dose comparing to third dose (Fig. S2, see Additional file 2). In addition, individuals treated with CAR-T cells and received three vaccine doses indicated an augmented pooled seropositivity rate of 16% (95% CI: 3–29%, Tau2 = 0.002; P = 0.36) compared to second dose (Fig. S3, see Additional file 2).
Subgroup analysis
We performed subgroup analyses of seroconversion post-third dose by type of transplant in HSCT recipients, median time since cell therapy to first dose vaccination, and brand of mRNA vaccines (as the most common platform reported in studies). Patients who received auto-HSCT and had negative humoral response after primary doses appeared to have a higher overall seroconversion rate than allo-HSCT recipients post-third dose (50.95%, Tau2 = 0.06 versus 40.94%, Tau2 = 0.91) (Fig. 8). Sixteen studies had reported a median interval from cell therapy to first dose administration. The analysis presented an overall seroconversion rate of 44.01% (95% CI: 26.94–61.65%, I2 = 71.7%; P = 0.00) and 40.96% (95% CI: 16.61–67.49%, I2 = 78.2%; P = 0.00) post-third dose in patients with a negative humoral response to second dose and a median interval of > 12 and < 12 months since cell therapy to first dose vaccination, respectively (Fig. S4, see Additional file 2). Additionally, among the studies that reported post-third-dose seroconversion data, five studies had applied BNT162b2 (from Pfizer-BioNTech) vaccines exclusively [27,28,29,30,31], whereas only two studies had administered only mRNA1273 (from Moderna) for three-dose immunization of patients against SARS-CoV-2 [32, 33]. The overall seroconversion rate after the third dose application in patients with a prior negative serologic response to the second dose was 61.25% (95% CI: 27.07–91.26%, I2 = 59.7%; P = 0.04) for studies using only BNT162b2 vaccines, which was considerably higher than the studies that administered only mRNA1273 vaccines, with a pooled seroconversion rate of 30.26% (95% CI: 19.90–41.67%) (Fig. S5, see Additional file 2).
Cellular response after third dose
Six studies evaluated the cellular immune response to a third vaccine dose, focusing on interferon-gamma (IFN-γ) production by CD4+ and CD8+ T-lymphocytes. Additional assessments included IL-2 release, CD154 upregulation, and tumor necrosis factor alpha (TNF-α) production [29, 33,34,35,36,37].
Albiol et al.’s study [33] found that 76.6% of patients vaccinated within three to 24 months (G1) and 94.4% vaccinated after 24 months (G2) from HSCT had a positive response, with no significant statistical difference. The administration of third dose was associated with a substantial elevation in positivity rates in G1 (overall increase of 18%), whereas G2 cohort witnessed a comparatively modest increment of 10% [33]. Einarsdottir et al. [34] noted that 49% (18/37) lacked detectable responses 4 weeks after the third dose. Moreover, they reported that T-cell responses were generally lower in individuals with chronic Graft-versus-Host Disease (GvHD) and were significantly reduced in patients undergoing Immunosuppressive Therapy (IST), especially those being treated with prednisone [34]. In a subgroup of allo-HSCT recipients, Kimura et al. [38] reported measurable responses in S-specific polyfunctional CD4+ T-cells (55%), IFN-γ monofunctional CD4+ T-cells (85%), IL-2 monofunctional CD4+ T-cells (85%), and CD8+ T-cells (75%). They also documented a statistically significant rise in the frequency of both polyfunctional CD4+ T-cells and IL-2 monofunctional CD4+ T-cells after administration of the third dose [38]. Using multiple assay formats and pertained to the cytokines IFN-γ and IL-2, in the study conducted by by Thümmler et al. [37], no significant enhancement in SARS-CoV-2-specific responses was observed in recipients of HSCT post-third-dose vaccination. Another study by Ram et al. [29] reported that 83% of CAR-T patients (5/6) and 100% of allo-HSCT patients (10/10) showed a positive cellular response post-third-dose injection. Furthermore, Marco et al. [36] demonstrated a significant augmentation in the SARS-CoV-2 S specific T-cell responses among HSCT recipients after third dose by performing a before-after analysis.
Risk of bias
In the critical appraisal process, all of the included studies got a JBI score of more than 0.75, indicating the high quality of all the studies (Table S4 and S5, see Additional file 1).
Publication bias
While publication bias was evaluated, minor assymetry was observed in the Doi plot and the Luis Furuya–Kanamori (LFK) index was equal to 0.26, representing the low probability of publication bias. The results of Doi plot and LFK index were in accordance with Egger’s test, with a p-value of 0.86 (Fig. 9).
Discussion
This meta-analysis provides important new information about the serologic response of patients undergoing HSCT and CAR-T cell treatment to additional doses of the SARS-CoV-2 vaccine. The findings illustrate a varied humoral response among these patients, highlighting the complexities of vaccine response in immunocompromised populations.
Our analysis indicated that the pooled humoral response after the third dose in HSCT recipients was notably high at 87.14%, with allo-HSCT at 85.41% and auto-HSCT at 89.96%, indicating that an important percentage of these recipients can achieve an adequate immune response. However, the response rate for patients receiving CAR-T cell therapy was significantly lower at 32.96%, indicating a significant gap in vaccine efficacy for this subgroup. For HSCT recipients initially seronegative, the seroconversion rate was 46.10% after the third dose and 27.23% after the fourth dose. In CAR-T cell patients, 17.26% of patients obtained seroconversion following the third dosage.
Comparing our analysis’s findings with those of similar meta-analyses [39,40,41,42]; Wu et al. found that 78.6% of HSCT patients exhibited a humoral response after three doses of vaccination [39]. A recent meta-analytical study revealed that 66.1% of transplant recipients (including both solid organ and hematopoietic stem cells) exhibited a humoral response after receiving three doses of the mRNA SARS-CoV-2 vaccine [40]. Also, another meta-analysis revealed an overall seropositive response rate of 68.8% (95% CI: 56.1–79.1, I2 = 80.91) for patients receiving HSCT or CAR-T cell therapy after three doses of the vaccine in five included studies [42]. Taheri [43] conducted a systematic review and meta-analysis to investigate the efficacy of booster doses (third and fourth doses) in dialysis and renal transplant patients. This study reported an overall humoral response rate of 88 and 69% in dialysis and kidney transplanted patients, respectively. Mai et al. [44] observed that the boosting dose yielded a considerably heightened seroconversion rate among patients with solid tumors compared with hematological cancer participants (80% vs. 44%). Another systematic review and meta-analysis found that the third and fourth doses of SARS-CoV-2 vaccinations resulted in a pooled humoral immune response of 75 and 85% in solid organ transplanted (SOT) individuals, respectively [45]. Furthermore, a meta-analysis of 21 studies including 1518 patients with hematologic malignancies with a negative antibody response to primary vaccinations indicated a pooled seroconversion rate of 40.5% after booster dose [46]. In a systematic review by Petrelli et al. [47], among over 2.7 million Israeli patients drawn from the general population, the decrease in infection risk was observed to be between 88 and 92%. The conversion rates for IgG antibodies targeting the spike protein ranged from 95 to 100%. Moreover, in patients with cancer or those who are immunocompromised, the average rate of seroconversion increased from 39.4% before receiving the third dose to 66.6% following the administration of the third dose [47]. In another systematic review and meta-analysis in general population, the relative Vaccine Effectiveness (rVE) observed at a median duration of 9 weeks post-booster administration was found to be 66.9% (95% CI: 59.8–72.7), 75.9% (95% CI: 62.6–84.5), 74.1% (95% CI: 66.9–79.8), 86.1% (95% CI: 78.7–90.9), and 84.2% (95% CI: 78.3–88.5) against overall infection, symptomatic infection, hospital admission, severe infection, and COVID-19-related mortality, respectively [48]. The effectiveness of heterologous booster vaccine regimens was found to be comparable to that of the homologous regimens. Furthermore, the rVE associated with the second homologous booster vaccination, recorded at a median of 7 weeks following the booster shot, was 41.9% (95% CI: 31.2–51.0), 53.1% (95% CI: 24.5–70.9), 60.6% (95% CI: 55.3–65.3), 56.4% (95% CI: 45.3–65.2), and 68.2% (95% CI: 51.2–79.2) for the five respective outcomes mentioned earlier, without a significant reduction in the rVE of the second booster vaccination noted [48]. Moreover, in a study on patients who received two doses of the SARS-CoV-2 vaccine during the first year following auto-HSCT, a heterologous prime-boost COVID-19 vaccination strategy using an inactivated vaccine platform significantly improved the serological response in comparison with the homologous prime-boost regimen [25]. Nevertheless, the data required for comparing the efficacy of heterologous prime-boost strategy with homologous regimen in our systematic review and meta-analysis was not adequate.
Certain studies have indicated a relatively low seropositivity rate among CAR-T cells recipients following the third dose of vaccine, underscoring the potential need for additional vaccine doses. Nonetheless, the overall seropositivity rate among these patients after receiving additional vaccine doses remains unclear [41, 49, 50]. Uyemura et al. [41] reported a seroconversion rate of 24.3% (95% CI: 10.4–47%, I2 = 0.00) for CAR-T cells recipients following the third or fourth dose of the vaccine across 4 studies. Piñana et al. observed that while the booster dose demonstrated a significant rise in antibody levels in both allo- and auto-HSCT recipients, recipients of CAR-T cells therapy who exhibited poor serologic response to the first two vaccine doses of SARS-CoV-2 failed to show any advantageous effects from the additional vaccine dose [50].
Potential explanations for the persistently compromised immune responses to SARS-CoV-2 vaccines among CAR-T cell therapy recipients include pre-existing and robust immunosuppression, extended B cell aplasia, prior toxicities including cytokine release syndrome, and neurotoxicity syndrome requiring corticosteroids and tocilizumab. These conditions may contribute to the failure of the vaccines [51, 52].
Regarding the factors affecting the serologic response to additional doses, we observed a superior overall seroconversion rate after third dose application in HSCT recipients with a median duration of greater than 12 months between transplantation and first dose immunization than patients vaccinated at less than 12 months interval since transplantation (44.01% versus 40.96%). A previous systematic review and meta-analysis suggested that the implementation of a suitable time interval, beyond 6 months, between vaccine administration and HSCT or CAR-T cell treatment can yield a greater serologic response rate [42]. Several studies have also revealed a positive correlation between an enhanced humoral response and an extended duration since HSCT [6, 16, 29, 53, 54]. Unlike previous studies, Hütter-Krönke et al. [55] could not identify a significant association between the duration of time following allo-SCT and the likelihood of acquiring a robust humoral response against SARS-CoV-2. Moreover, the prolonged period required for both quantitative and functional restoration of B and T cells following HSCT, potentially extending beyond a year, coupled with the application of immunosuppressive agents for GVHD prophylaxis in the context of allogeneic transplants, could elucidate the reduced antibody levels and increased prevalence of non-responders observed in patients vaccinated within 1 year since HSCT [56]. Conversely, the observed differences between autologous and allogeneic cohorts in patients who underwent transplantation over 5 years prior to vaccination could be attributed to the more common occurrence of ongoing active disease and the receipt of continuous salvage therapies among autologous HSCT recipients, which are widely acknowledged as significant risk factors for suboptimal response to vaccination [56]. Furthermore, several studies have explored molecular mechanisms associated with diverse immunological responses to different COVID-19 vaccines [57,58,59]. In a retrospective study to examine the relationship between Human Leukocyte Antigen (HLA) evolutionary divergence (HED) and the immune response to the SARS-CoV-2 vaccine in patients who received allo-HSCT, Villemonteix et al. [60] found that low levels of anti-spike IgG (< 30 BAU/mL) were linked to both a shorter duration since the allo-HSCT procedure and lower HED at the donor DPB1 locus, which was mainly attributed to the homozygosity of the donor’s DPB1 allele. The results of this study suggest that the genetic diversity of the donor HLA-DP molecules, determined by either heterozygosity or sequence variation, may play a significant role in enhancing the effectiveness of donor-derived CD4 T cells in sustaining an antibody response to the vaccine in allo-HSCT recipients [60].
Because of the waning immunogenicity against SARS-CoV-2 vaccination and the profound vulnerability of immunocompromised patients, more than one additional dose may be needed to preserve humoral immunity in this population. In this regard, SOT recipients obtained a substantially augmented serologic response to the fourth vaccine dose than the third shot (81.7% versus 55.2%) in a meta-analysis conducted by Tang et al. [61]. In line with these results, we also noted an enhanced serologic response to the fourth shot in the HSCT group compared with the third vaccine dose. Furthermore, Mittal. et al. [62] demonstrated a significant rise in the levels of anti-RBD antibodies post-fourth dose administration compared with the third dose vaccination. However, the overall seropositivity rate among these patients after receiving additional vaccine doses remains unclear, and there is still a significant gap in our understanding of the overall response rate after administering a fourth vaccine dose.
The scant research available has centered on examining the cellular immune response to a third dose of the COVID-19 vaccine, specifically the production of IFN-γ by T lymphocytes. Significant findings derived from these investigations encompass a considerably elevated response rates and a broad spectrum of responses among individuals who have undergone allogeneic HSCT and CAR-T therapy. The aforementioned collection of studies sheds light on the complex and diverse fabric of the immune system’s defense mechanisms following triadic COVID-19 vaccination.
Study limitations and future directions
One limitation to consider is the potential discrepancy in populations receiving booster doses compared to those who received previous doses, which may influence the comparison of seropositive responses between an additional dose and a previous one. For instance, variations in the number of individuals receiving a third or fourth dose compared to earlier doses within the same study cohort could lead to differences in baseline characteristics and vaccine responsiveness. Additionally, variations in the distribution of seropositive and seronegative patients among those receiving additional doses may exist between studies, potentially affecting the comparison of seropositive response rates between different vaccine doses. While acknowledging this limitation, it’s important to interpret the findings cautiously and recognize the need for future studies with more homogeneous study populations and consistent methodologies to further elucidate the difference in seropositive responses between additional and previous vaccine doses. Furthermore, this study’s reliance on serologic response as the primary outcome may not fully capture the nuances of immune response, including cellular immunity, which can also play a critical role in protection against COVID-19.
Subsequent investigations need to concentrate on a more comprehensive assessment of immune response, including cellular immunity, and the exploration of alternative strategies such as prophylactic antivirals or passive immunization for those who do not respond adequately to vaccines.
Conclusion
Overall, this study provides remarkable evidence for the varying degrees of vaccine responsiveness among HSCT and CAR-T cell therapy recipients. The fact that a significant portion of these patients, especially those who have undergone CAR-T cell therapy, did not achieve a robust humoral response after the additional doses reinforces the need for tailored vaccination strategies in these vulnerable populations. This research also paves the way for future investigations to optimize protective measures against COVID-19 in immunocompromised individuals.
Availability of data and materials
Not applicable.
Abbreviations
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome Coronavirus 2
- HSCT:
-
Hematopoietic stem cell transplantation
- CAR-T:
-
Chimeric antigen receptor-T
- COVID-19:
-
Coronavirus disease of 2019
- GVHD:
-
Graft-versus-host disease
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- JBI:
-
Joanna Briggs Institute
- RCT:
-
Randomized controlled trial
- GLMM:
-
Generalized Linear Mixed Model
- CI:
-
Confidence interval
- IFN-γ:
-
Interferon gamma
- IL-2:
-
Interlukin 2
- TNF-α:
-
Tumor necrosis factor alpha
- LFK:
-
Luis Furuya–Kanamori
- SOT:
-
Solid organ transplant
- rVE:
-
relative Vaccine Effectiveness
- HLA:
-
Human Leukocyte Antigen
- HED:
-
Human Leukocyte Antigen evolutionary divergence
References
Bonanni P, Ceddia F, Dawson R. A call to action: current challenges and considerations for COVID-19 vaccination in immunocompromised populations. J Infect Dis. 2023;228(Supplement_1):S70–S6.
Hussein T, Hammad MH, Fung PL, Al-Kloub M, Odeh I, Zaidan MA, Wraith D. COVID-19 pandemic development in Jordan—short-term and long-term forecasting. Vaccines. 2021;9(7):728.
Al-Qerem W, Jarab A, Shawabkeh Y, Ling J, Hammad A, Ba A, Alasmari F. COVID-19 vaccination booster dose: knowledge, practices, and intention among pregnant/planning to get pregnant and lactating women. Vaccines. 2023;11(7):1249.
Kokogho A, Crowell TA, Aleissa M, Lupan AM, Davey S, Park Chang JB, et al. SARS-CoV-2 vaccine-induced immune responses among hematopoietic stem cell transplant recipients. Open forum Infect Dis. 2023;10(7):ofad349.
Huang A, Cicin-Sain C, Pasin C, Epp S, Audigé A, Müller NJ, et al. Antibody response to SARS-CoV-2 vaccination in patients following allogeneic hematopoietic cell transplantation. Transplant cellular Therapy. 2022;28(4):214–e1-e11.
Ram R, Hagin D, Kikozashvilli N, Freund T, Amit O, Bar-On Y, et al. Safety and immunogenicity of the BNT162b2 mRNA COVID-19 vaccine in patients after allogeneic HCT or CD19-based CART therapy—a single-center prospective cohort study. Transplant cellular therapy. 2021;27(9):788–94.
Hill JA, Martens MJ, Young JH, Bhavsar K, Kou J, Chen M, Lee LW, Baluch A, Dhodapkar MV, Nakamura R, Peyton K, Shahid Z, Armistead P, Westervelt P, McCarty J, McGuirk J, Hamadani M, DeWolf S, Hosszu K, Sharon E, Spahn A, Toor AA, Waldvogel S, Greenberger LM, Auletta JJ, Horowitz MM, Riches ML, Perales MA. SARS-CoV-2 vaccination in the first year after allogeneic hematopoietic cell transplant: a prospective, multicentre, observational study. EClinicalMedicine. 2023;59:101983.https://doi.org/10.1016/j.eclinm.2023.101983.
Mamez A-C, Pradier A, Giannotti F, Petitpas A, Urdiola MF, Vu D-L, et al. Antibody responses to SARS-CoV2 vaccination in allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2021;56(12):3094–6.
Dhakal B, Abedin S, Fenske T, Chhabra S, Ledeboer N, Hari P, Hamadani M. Response to SARS-CoV-2 vaccination in patients after hematopoietic cell transplantation and CAR T-cell therapy. Blood J Am Soc Hematol. 2021;138(14):1278–81.
Redjoul R, Le Bouter A, Beckerich F, Fourati S, Maury S. Antibody response after second BNT162b2 dose in allogeneic HSCT recipients. Lancet. 2021;398(10297):298–9.
Abid MA, Abid MB. SARS-CoV-2 vaccine response in CAR T-cell therapy recipients: a systematic review and preliminary observations. Hematol Oncol. 2022;40(2):287–91.
O-k C, Gomez-Arteaga A, Chen Z, Soave R, Shore T, Mayer S, et al. Predictors of Covid-19 Vaccination Response After In-Vivo T-Cell–Depleted Stem Cell Transplantation. Transplant Cellular Therapy. 2022;28(9):618–e1-e10.
Werbel WA, Boyarsky BJ, Ou MT, Massie AB, Tobian AA, Garonzik-Wang JM, Segev DL. Safety and immunogenicity of a third dose of SARS-CoV-2 vaccine in solid organ transplant recipients: a case series. Ann Intern Med. 2021;174(9):1330–2.
Hall VG, Ferreira VH, Ku T, Ierullo M, Majchrzak-Kita B, Chaparro C, et al. Randomized trial of a third dose of mRNA-1273 vaccine in transplant recipients. N Engl J Med. 2021;385(13):1244–6.
Peled Y, Ram E, Lavee J, Segev A, Matezki S, Wieder-Finesod A, et al. Third dose of the BNT162b2 vaccine in heart transplant recipients: immunogenicity and clinical experience. J Heart Lung Transplant. 2022;41(2):148–57.
Redjoul R, Le Bouter A, Parinet V, Fourati S, Maury S. Antibody response after third BNT162b2 dose in recipients of allogeneic HSCT. Lancet Haematol. 2021;8(10):e681–e3.
Pettini E, Ciabattini A, Pastore G, Polvere J, Lucchesi S, Fiorino F, et al. A third dose of mRNA-1273 vaccine improves SARS-CoV-2 immunity in HCT recipients with low antibody response after 2 doses. Blood Adv. 2022;6(7):2247–9.
Goldberg Y, Mandel M, Bar-On YM, Bodenheimer O, Freedman L, Haas EJ, et al. Waning immunity after the BNT162b2 vaccine in Israel. N Engl J Med. 2021;385(24):e85.
Thomas SJ, Moreira ED Jr, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. N Engl J Med. 2021;385(19):1761–73.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Barker TH, Habibi N, Aromataris E, Stone JC, Leonardi-Bee J, Sears K, et al. The revised JBI critical appraisal tool for the assessment of risk of bias quasi-experimental studies. JBI Evid Synth. 2024;22(3):378-88.
Chang X, Luis F-K, Suhail ARD. DOIPLOT: Stata module for visualization of asymmetry and heterogeneity in meta-analysis. Statistical Software Components S459011 ed: Boston College Department of Economics; 2021.
Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72(1):39.
Barkhordar M, Chahardouli B, Biglari A, Ahmadvand M, Bahri T, Alaeddini F, et al. Three doses of a recombinant conjugated SARS-CoV-2 vaccine early after allogeneic hematopoietic stem cell transplantation: predicting indicators of a high serologic response—a prospective, single-arm study. Front Immunol. 2023;14:1169666.
Sharifi Aliabadi L, Karami M, Barkhordar M, Hashemi Nazari SS, Kavousi A, Ahmadvand M, Vaezi M. Homologous versus Heterologous prime-boost COVID-19 Vaccination in autologous hematopoietic stem cell transplantation recipients: a blindedrandomized controlled trial. Front Immunol. 2023;14:1237916. https://doi.org/10.3389/fimmu.2023.1237916.
Tsoutsoukis M, Easdale S, Anthias C, Ethell M, Arias C, Ismail S, Mir F, Shea R, Neoh C, Nicholson E. Re-vaccination against SARS-COV2 in allogeneic HSCT patients: Repeated primary vaccines doses increases seroconversion rates. Br J Haematol. 2023:59-59.
Debie Y, Vandamme T, Goossens ME, Van Dam PA, Peeters M. Antibody titres before and after a third dose of the SARS-CoV-2 BNT162b2 vaccine in patients with cancer. Eur J Cancer. 2022;163:177–9.
Canti L, Ariën KK, Desombere I, Humblet-Baron S, Pannus P, Heyndrickx L, et al. Antibody response against SARS-CoV-2 Delta and omicron variants after third-dose BNT162b2 vaccination in Allo-HCT recipients. Cancer Cell. 2022;40(4):335–7.
Ram R, Freund T, Halperin T, Ben-Ami R, Amit O, Bar-On Y, et al. Immunogenicity of a third dose of the BNT162b2 mRNA Covid-19 vaccine in patients with impaired B cell reconstitution after cellular therapy—a single center prospective cohort study. Transplant cellular Therapy. 2022;28(5):278–e1-e4.
Fatobene G, Santos CF, Otuyama LJ, Fernandes TH, Lima AHSB, Moraes BDGC, et al. Immunogenicity and safety of a heterologous COVID-19 vaccine regimen in hematopoietic stem cell transplant recipients. Transplant Cellular Therapy. 2023;29(2):S331.
Henig I, Isenberg J, Yehudai-Ofir D, Leiba R, Ringelstein-Harlev S, Ram R, et al. Third BNT162b2 mRNA SARS-CoV-2 vaccine dose significantly enhances immunogenicity in recipients of allogeneic hematopoietic stem cell transplantation. Vaccines. 2023;11(4):775.
Haggenburg S, Hofsink Q, Lissenberg-Witte BI, Broers AE, Van Doesum JA, Van Binnendijk RS, et al. Antibody response in immunocompromised patients with hematologic cancers who received a 3-dose mRNA-1273 vaccination schedule for COVID-19. JAMA oncol. 2022;8(10):1477–83.
Albiol N, Lynton-Pons E, Aso O, Moga E, Vidal S, Gómez-Pérez L, Santiago JA, Triquell M, Roch N, Lázaro E, González I, López-Contreras J, Esquirol A, Sierra J, Martino R, García-Cadenas I. mRNA-1273 SARS-CoV-2 vaccine in recently transplanted allogeneic hematopoietic cell transplant recipients: Dynamics of cellular and humoral immune responses and booster effect. Leuk Res. 2023;132:107347. https://doi.org/10.1016/j.leukres.2023.107347.
Einarsdottir S, Martner A, Nicklasson M, Wiktorin HG, Arabpour M, Törnell A, et al. Reduced immunogenicity of a third COVID-19 vaccination among recipients of allogeneic hematopoietic stem cell transplantation. Haematol. 2022;107(6):1479.
Kokogho A, Crowell TA, Aleissa M, Lupan A-M, Davey S, Park Chang JB, et al., editors. SARS-CoV-2 Vaccine-Induced Immune Responses Among Hematopoietic Stem Cell Transplant Recipients. Open Forum Infectious Diseases; 2023: Oxford University Press US.
Marco I, Spalliera I, Mallegni F, Mercante L, Imeneo A, Crea A, et al., editors. 1970. SARS-CoV-2 T-cell specific responses in allogeneic hematopoietic stem cell transplant recipients after second and third dose of BNT162b2 mRNA vaccine. Open Forum Infectious Diseases; 2022: Oxford University Press.
Thümmler L, Koldehoff M, Fisenkci N, Brochhagen L, Horn PA, Krawczyk A, Lindemann M. Cellular and humoral immunity after the third vaccination against SARS-CoV-2 in hematopoietic stem-cell transplant recipients. Vaccines. 2022;10(6):972.
Kimura M, Ferreira VH, Kothari S, Pasic I, Mattsson JI, Kulasingam V, et al. Safety and immunogenicity after a three-dose SARS-CoV-2 vaccine schedule in allogeneic stem cell transplant recipients. Transplant cellular therapy. 2022;28(10):706–e1-e10.
Wu X, Wang L, Shen L, He L, Tang K. Immune response to vaccination against SARS-CoV-2 in hematopoietic stem cell transplantation and CAR T-cell therapy recipients. J Hematol Oncol. 2022;15(1):81.
Bailey AJM, Maganti HB, Cheng W, Shorr R, Arianne Buchan C, Allan DS. Humoral and cellular response of transplant recipients to a third dose of mRNA SARS-CoV-2 vaccine: a systematic review and Meta-analysis. Transplant. 2023;107(1):204–15.
Uyemura BS, Abid MA, Suelzer E, Abid MB. Efficacy of SARS-CoV-2 primary and booster vaccine doses in CAR-T recipients–targeting the target antigen. Bone Marrow Transplant. 2022;57(11):1727–31.
Ge C, Du K, Luo M, Shen K, Zhou Y, Guo K, et al. Serologic response and safety of COVID-19 vaccination in HSCT or CAR T-cell recipients: a systematic review and meta-analysis. Experiment hematol oncol. 2022;11(1):46.
Taheri S. Efficacy and safety of booster vaccination against SARS-CoV-2 in dialysis and renal transplant patients: systematic review and meta-analysis. Int Urol Nephrol. 2023;55(4):791–802.
Mai AS, Lee ARYB, Tay RYK, Shapiro L, Thakkar A, Halmos B, et al. Booster doses of COVID-19 vaccines for patients with haematological and solid cancer: a systematic review and individual patient data meta-analysis. Eur J Cancer. 2022;172:65–75.
Mu Y, Wu H, Jiang Z, Liu K, Xue X, Zhang W, Chen Z. Serological responses after a fourth dose of SARS-CoV-2 vaccine in solid organ transplant recipients: a systematic review and Meta-analysis. Vaccines. 2023;11(7):1130.
Uaprasert N, Pitakkitnukun P, Tangcheewinsirikul N, Chiasakul T, Rojnuckarin P. Immunogenicity and risks associated with impaired immune responses following SARS-CoV-2 vaccination and booster in hematologic malignancy patients: an updated meta-analysis. Blood Cancer J. 2022;12(12):173.
Petrelli F, Luciani A, Borgonovo K, Ghilardi M, Parati MC, Petrò D, et al. Third dose of SARS-CoV-2 vaccine: a systematic review of 30 published studies. J Med Virol. 2022;94(6):2837–44.
Liu D, Jiang Y, Wang S, Li F, Lin T, Li B, et al. Relative effectiveness and durability of booster doses of SARS-CoV-2 vaccines: a systematic review and meta-analysis. Innov Med. 2024;2(1):100051.
Gössi S, Bacher U, Haslebacher C, Nagler M, Suter F, Staehelin C, et al. Humoral responses to repetitive doses of COVID-19 mRNA vaccines in patients with CAR-T-cell therapy. Cancers. 2022;14(14)
Piñana JL, Martino R, Vazquez L, López-Corral L, Pérez A, Chorão P, et al. SARS-CoV-2-reactive antibody waning, booster effect and breakthrough SARS-CoV-2 infection in hematopoietic stem cell transplant and cell therapy recipients at one year after vaccination. Bone Marrow Transplant. 2023;58(5):567–80.
Meir J, Abid MA, Abid MB. State of the CAR-T: risk of infections with chimeric antigen receptor T-cell therapy and determinants of SARS-CoV-2 vaccine responses. Transplantat Cell Therapy. 2021;27(12):973–87.
Abid MB. Early immunomodulators with CAR T-cell immunotherapy in the COVID-19 era. Lancet Oncol. 2022;23(1):16–8.
Matkowska-Kocjan A, Owoc-Lempach J, Chruszcz J, Kuźnik E, Szenborn F, Jurczenko L, et al. The COVID-19 mRNA BNT163b2 vaccine was well tolerated and highly immunogenic in Young adults in long follow-up after Haematopoietic stem cell transplantation. Vaccines. 2021;9(10):1209.
Maillard A, Redjoul R, Klemencie M, Labussière Wallet H, Le Bourgeois A, d'Aveni M, et al. Antibody response after 2 and 3 doses of SARS-CoV-2 mRNA vaccine in allogeneic hematopoietic cell transplant recipients. Blood J Am Soc Hematol. 2022;139(1):134–7.
Hütter-Krönke ML, Neagoie A, Blau IW, Wais V, Vuong L, Gantner A, et al. Risk factors and characteristics influencing humoral response to COVID-19 vaccination in patients after allogeneic stem cell transplantation. Front Immunol. 2023;14:1174289.
Attolico I, Tarantini F, Carluccio P, Musto P. Serological response following anti-SARS-CoV-2 vaccination in hematopoietic stem cell transplantation patients depends upon time from transplant, type of transplant and “booster” dose. Haematol. 2022;107(5):1218.
Li J, Huang F, Ma Q, Guo W, Feng K, Huang T, Cai Y-D. Identification of genes related to immune enhancement caused by heterologous ChAdOx1–BNT162b2 vaccines in lymphocytes at single-cell resolution with machine learning methods. Front Immunol. 2023;14
Ren J, Zhou X, Huang K, Chen L, Guo W, Feng K, et al. Identification of key genes associated with persistent immune changes and secondary immune activation responses induced by influenza vaccination after COVID-19 recovery by machine learning methods. Comput Biol Med. 2024;169:107883.
Li H, Ma Q, Ren J, Guo W, Feng K, Li Z, et al. Immune responses of different COVID-19 vaccination strategies by analyzing single-cell RNA sequencing data from multiple tissues using machine learning methods. Front Genet. 2023;14:1157305.
Villemonteix J, Allain V, Verstraete E, Jorge-Cordeiro D, Socié G, Xhaard A, et al. HLA-DP diversity is associated with improved response to SARS-Cov-2 vaccine in hematopoietic stem cell transplant recipients. Iscience. 2023;26(5)
Tang K, Wu X, Luo Y, Wei Z, Feng L, Wu L. Meta-analysis of immunologic response after COVID-19 mRNA vaccination in solid organ transplant recipients. J Infect. 2022;84(5):e73–e5.
Mittal A, Solera JT, Ferreira VH, Kothari S, Kimura M, Pasic I, Mattsson JI, Humar A, Kulasingam V, Ierullo M, Kumar D, Hosseini-Moghaddam SM. Immunogenicity and Safety of Booster SARS-CoV-2 mRNA Vaccine Dose in Allogeneic Hematopoietic Stem Cell Transplantation Recipients. Transplant Cell Ther. 2023;29(11):706.e1-706.e7. https://doi.org/10.1016/j.jtct.2023.08.008.
Abid MB, Rubin M, Ledeboer N, Szabo A, Longo W, Mohan M, et al. Efficacy of a third SARS-CoV-2 mRNA vaccine dose among hematopoietic cell transplantation, CAR T cell, and BiTE recipients. Cancer Cell. 2022;40(4):340–2.
Attolico I, Tarantini F, Schifone CP, Mestice A, De Tullio G, Carluccio P, Delia M, Gagliardi VP, Perrone T, Gaudio F, Longo C. The third dose of bnt162b2 anti-sars-cov-2 mrna vaccination is effective and can rescue hematopoietic stem cell transplantationpatients not responding to the first two doses. Haematologica. 2022:89-90.
Chevallier P, Jullien M, Peterlin P, Garnier A, Le Bourgeois A, Coste-Burel M, et al. Effectiveness of a third dose of BNT162b2 anti-SARS-CoV-2 mRNA vaccine over a 6-month follow-up period in allogenic hematopoietic stem cells recipients. Hematol Oncol. 2022;40(5):1097–9.
Federico L, Tvedt THA, Gainullin M, Osen JR, Chaban V, Lund KP, et al. Robust spike-specific CD4+ and CD8+ T cell responses in SARS-CoV-2 vaccinated hematopoietic cell transplantation recipients: a prospective, cohort study. Front Immunol. 2023;14
Khan QJ, Bivona CR, Liu B, Nelson M, Martin GA, Mushtaq MU, et al. Prospective longitudinal study of kinetics of humoral response to one, two, or three doses of SARS-CoV-2 vaccine in hematopoietic cell transplant recipients. Bone Marrow Transplant. 2022;57(6):1013–6.
Le Bourgeois A, Coste-Burel M, Guillaume T, Peterlin P, Garnier A, Imbert BM, et al. Interest of a third dose of BNT162b2 anti-SARS-CoV-2 messenger RNA vaccine after allotransplant. Br J Haematol. 2022;196(5):e38.
Liga M, Tsokanas D, Gkikas A, Sagiadinou E, Vamvakopoulou S, Paliogianni F, Spyridonidis A. Antibody responses to SARS-CoV-2 vaccination in allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2022;292
Loubet P, Wittkop L, Ninove L, Chalouni M, Barrou B, Blay J-Y, et al. One-month humoral response following two or three doses of messenger RNA coronavirus disease 2019 vaccines as primary vaccination in specific populations in France: first results from the Agence Nationale Recherche contre le Sida (ANRS) 0001S COV-POPART cohort. Clin Microbiol Infect. 2023;29(3):388–e1-e8.
Majcherek M, Matkowska-Kocjan A, Szymczak D, Karasek M, Przeorski K, Szeremet A, Kiraga A, Milanowska A, Kuznik E, Kujawa K, Wrobel T, Szenborn L, Czyz A. The booster dose of BNT162b2 mRNA vaccine in patients after hematopoietic stem cell transplantation: humoral and clinical response and serological conversion predictors. Acta Oncol. 2023;62(12):1939-1941. https://doi.org/10.1080/0284186X.2023.2254923.
Nikoloudis A, Neumann IJ, Buxhofer-Ausch V, Machherndl-Spandl S, Binder M, Kaynak E, et al. Successful SARS-CoV-2 mRNA vaccination program in allogeneic hematopoietic stem cell transplant recipients—a retrospective single-center analysis. Vaccines. 2023;11(10):1534.
Vanlerberghe B, Vrij C, Bogaerts K, Vermeersch P, Lagrou K, Molenberghs G, et al. SARS-CoV-2 vaccine antibody response and breakthrough infections in transplant recipients. J Med Virol. 2023;95(4):e28736.
Watanabe M, Yakushijin K, Funakoshi Y, Ohji G, Ichikawa H, Sakai H, et al. A third dose COVID-19 vaccination in allogeneic hematopoietic stem cell transplantation patients. Vaccines. 2022;10(11):1830.
Acknowledgments
Thanks to Dr. Manouchehr Karami and Mr. Aram Halimi for his support.
Funding
None.
Author information
Authors and Affiliations
Contributions
LSA and MB brought the conception and design of the study; acquisition of data: MA and MA; analysis and drafting the article: MRT, LSA, MA, MA, SR, and MB; revising it critically for important intellectual content: MB, SAMA, ZS, and MV; final approval of the version to be submitted: MB and LSA. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. PRISMA 2020 abstract checklist. Table S2. PRISMA 2020 checklist. Table S3. Search strategy. Table S4. Risk of bias assessment of the eligible studies using the JBI tool for quasi-experimental studies. Table S5. Risk of bias assessment of the included randomized controlled trial study using the JBI tool
Additional file 2:
Fig. S1. Forest plot of pooled seropositive rate difference between third and second dose in HSCT patients. Fig. S2. Forest plot of pooled seropositive rate difference between fourth and third dose in HSCT patients. Fig. S3. Forest plot of pooled seropositive rate difference between third and second dose in CAR-T cell patients. Fig. S4. Forest plot of seroconversion after the third dose in HSCT recipients by the interval between transplantation and vaccination initiation. This plot demonstrates higher seroconversion rates among patients with a median interval of more than 12 months from cell therapy to the first dose of immunization. Fig. S5. Forest plot of seroconversion after third dose in HSCT recipients by brand of the mRNA vaccine received.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sharifi Aliabadi, L., Azari, M., Taherian, M.R. et al. Immunologic responses to the third and fourth doses of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccines in cell therapy recipients: a systematic review and meta-analysis. Virol J 21, 103 (2024). https://doi.org/10.1186/s12985-024-02375-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-024-02375-1