Abstract
Neurodegenerative diseases are a group of disorders characterized by progressive loss of certain populations of neurons, which eventually lead to dysfunction. These diseases include Alzheimer’s disease (AD), Parkinson’s disease (PD), and amyotrophic lateral sclerosis (ALS). Immune pathway dysregulation is one of the common features of neurodegeneration. Recently, there is growing interest in the specific role of T helper Th 17 cells and Interleukin-17A (IL-17A), the most important cytokine of Th 17 cells, in the pathogenesis of the central nervous system (CNS) of neurodegenerative diseases. In the present study, we summarized current knowledge about the function of Th17/IL-17A, the physiology of Th17/IL-17A in diseases, and the contribution of Th17/IL-17A in AD, PD, and ALS. We also update the findings on IL-17A-targeting drugs as potentially immunomodulatory therapeutic agents for neurodegenerative diseases. Although the specific mechanism of Th17/IL-17A in this group of diseases is still controversial, uncovering the molecular pathways of Th17/IL-17A in neurodegeneration allows the identification of suitable targets to modulate these cellular processes. Therapeutics targeting IL-17A might represent potentially novel anti-neurodegeneration drugs.
Similar content being viewed by others
Background
Neurodegenerative diseases are a group of disorders characterized by progressive loss of certain populations of neurons, which eventually lead to dysfunction. These diseases include Alzheimer’s disease (AD), Parkinson’s disease (PD), and amyotrophic lateral sclerosis (ALS). At present, the treatment of neurodegenerative diseases is still very difficult, so it is very important to understand the pathophysiological mechanism of neurodegenerative diseases. Neurodegenerative diseases are characterized by selective susceptibility of certain nerve cells, different protein aggregation, and abnormal immune responses [1]. The pathogenesis of neurodegeneration is the joint action of many factors, and neuroinflammation is considered to be part of the cause of neurodegeneration. Neuroinflammation is characterized by elevated levels of inflammatory mediators or cytokines in the central nervous system (CNS) parenchyma [2]. Recently, there is growing interest in the specific role of T helper 17 (TH17) cells and Interleukin-17A (IL-17A), the most important cytokine of Th 17 cells, in the pathogenesis of the CNS of neurodegenerative diseases. Studies have shown that IL-17A acts on multiple resident cells of the central nervous system, enhances neuroinflammatory response, and plays a pathogenic role in a variety of neurodegenerative diseases [3]. However, the role of TH17/IL-17A in neurodegenerative diseases is still unclear and contradictory. Therefore, we summarized current knowledge about the function of Th17/IL-17A, the physiology of Th17/IL-17A in diseases, and the contribution of Th17/IL-17A in AD, PD, and ALS. We also update the findings on IL-17A-targeting drugs as potentially immunomodulatory therapeutic agents for neurodegenerative diseases.
Biology of Th17 cells and IL-17A
Th17 cells were recognized in 2005 as a distinct lineage of T helper (Th) CD4+ cells [4, 5]. The differentiation of Th17 cells requires stimulation with certain cytokines, including IL-6, IL-23, IL-1β, transforming growth factor-β (TGF-β), and IL-21 [6,7,8,9,10,11,12,13,14]. These cytokines can trigger the JAK–STAT3 axis, and increase the expression of transcription factors, including retinoic orphan receptor (ROR)γt and RORα [15,16,17,18,19]. Th17 cells would achieve the pathogenic potential under the stimulation by pro-inflammatory cytokines IL-6, IL-23, and IL-1β, whereas cytokine TGF-β drives the development of protective Th17 cells by inducing the production of anti-inflammatory cytokine IL-10 [19,20,21]. IL-21 stimulates the expansion of Th17 cells in an autocrine loop [22]. IL-17A, initially called cytotoxic T-lymphocyte antigen (CTLA)-8 and cloned firstly in 1993, is the signature cytokine of Th17 cells [23], and it was described as an RNA transcript homologous to a Herpesvirus Saimiri gene. In 1995, the IL-17-binding receptor was first reported [24, 25]. Besides Th17 cells, other variable sources also produce IL-17A, including γδT, T-cell receptor (TCR)-β+ natural Th17, natural killer T (NKT), group 3 innate lymphoid cells (ILC3), Paneth cells, macrophages, and microglia in the CNS [26,27,28,29].
The function of Th17 cells and IL-17A
First, Th17 cells can trigger pro-inflammatory danger signals, recruit and activate neutrophil granulocytes, upregulate the expression of antimicrobial factors, and promote the clearance of extracellular bacteria and fungi [30, 31]. IL-17A has an important capacity to induce the expression of chemokines and cytokines [3]. The chemokines, including C-X-C motif ligand 1 (CXCL1), CXCL2, and CXCL8 can attract myeloid cells to infected or injured tissues [32]. The cytokines, including granulocyte colony-stimulating factor (G-CSF) and IL-6 can promote myeloid-driven innate inflammation [33]. The pro-inflammatory cytokines and antimicrobial peptides are upregulated to put a synergistic effect on limiting fungal overgrowth [34, 35]. For example, in healthy skin, the IL-17A production is induced by commensal microflora to provide anti-fungal protection [23]. When the epithelial barrier of the skin is destroyed by injury, IL-17A can promote the proliferation of epithelial cells and the clearance of the pathogenic agents [36]. In the intestine, the IL-17A production is driven by the microbiota from the local epithelium to provide the antimicrobial function, and it can be helpful to control dysbiosis and to maintain a homeostatic balance in the gut [37, 38]. In the lamina propria of the small intestine, Th17 cells can mediate the protection against pathogenic microorganisms. In the brain of AD patients, Malassezia species, one of the most common fungi detected can lead to neuroinflammation via activating Th17 immune response [39].
Second, Th17 cells and IL-17A are mainly pro-inflammatory, and they are considered to be associated with several autoimmune diseases, including psoriasis, ankylosing spondylitis (AS), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and inflammatory bowel disease (IBD) [40]. In psoriasis, the pathogenic inflammation was promoted by dysregulated IL-17 signaling. Th17 cells could infiltrate the psoriatic skin lesions, and inhibition of IL-17A had an effective treatment for psoriasis [41]. In AS, Th17 cells and IL-17A contribute to pathogenic inflammation, and it is effective to use an anti-IL-17A monoclonal antibody to treat AS [42]. In patients with RA, IL-17A was present at the sites of inflammatory arthritis, and higher numbers of IL-17+ CD4+ T cells were found in peripheral blood, but the efficacy of brodalumab, a human anti-IL-17A monoclonal antibody, in the treatment of RA was negative [40, 43, 44]. In patients with SLE, increased levels of IL-23, IL-21, and IL-17 were identified, which was associated with the expansion of Th17 cells [40, 45]. In patients with IBD, high levels of IL-17 and IL-21 in serum were reported [40, 46].
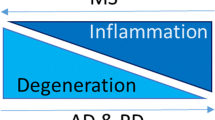
Third, the role of Th17 cells and IL-17A as indicated in the pathogenesis of CNS autoimmune disorders. Multiple sclerosis (MS) is a chronic CNS inflammatory disease, and the most characteristic animal model of MS is experimental autoimmune encephalomyelitis (EAE), used to explore the pathogenesis of MS. Th17 cells are one of the key effectors in MS and EAE, and MS was marked as a primarily IL-17-mediated autoimmune disease [47]. In MS patients, the expression of IL-17A and Th17-associated transcript IL-6 was increased in the demyelinated plaques [48], and the gene expression of IL-17 ranked at the highest in the CNS at autopsy [48]. The IL-17 level in serum was higher in MS patients with relapses and remissions [49], with an association to disease activity [50]. The proportion of Th17 cells in serum was increased during relapses [51, 52]. In the cerebral fluid (CSF), IL-17A level was elevated in patients with relapses and remissions, with a correlation to the level of the blood–brain barrier (BBB) dysfunction [53]. The EAE mouse model showed that Th17 cells could infiltrate the brain [54] and IL-17 could disrupt BBB [55]. In the cell model, Th17 cells were proved to cross the BBB, and the presence of Th17 cells in the lesions of CNS was related to enhanced neuroinflammation [56]. Th17 cells contribute to the disruption of the BBB [57], promote the activation of astrocytes and microglia within the CNS, and amplify neuroinflammation in EAE by targeting resident glial cells [58, 59]. Studies have shown that IL-17 neutralization could attenuate EAE progression through alleviating the generation of pathogenic cytokines [60], and EAE severity could be ameliorated in IL-17-deficient mice [61,62,63]. Phase IIa study of secukinumab showed that an IL-17A-neutralizing monoclonal antibody might be effective in reducing MRI lesion activity in MS [64].
Th17 cells and IL-17A in neurodegenerative diseases
Neurodegenerative diseases are characterized by the selective vulnerability of certain neuronal cells, diverse protein aggregation, and abnormal immune responses [1]. Studies have shown that IL-17A played a pathogenic role in several neurodegenerative diseases [3]. Regarding the contribution of Th17 cells and IL-17A in Alzheimer’s disease (AD), Parkinson’s disease (PD), and amyotrophic lateral sclerosis (ALS), we systematically retrieved and critically evaluated available literatures, aiming to provide a compendium to clarify the possible benefits of targeting Th17/IL-17 to develop novel treatments for these patients (Fig. 1). A total of 146 reports were retrieved by the following keywords: “TH17”, “IL-17”, “Parkinson’s disease”, “PD”, “Alzheimer’s disease”, “AD”, “Amyotrophic lateral sclerosis”, “ALS”, “neurodegenerative diseases”. Finally, six studies [65,66,67,68,69,70] on targeted therapy for IL-17 were screened out (Table 1).
Th17 cells and IL-17A in AD
AD is the most common neurodegenerative disease, contributing up to 70% of all cases of dementia, and has an exponentially increasing prevalence after the age of 65. Pathologically, AD is characterized by the deposition of extracellular senile plaques composed of amyloid-β (Aβ) and intracellular neurofibrillary tangles, resulting from the accumulation of hyperphosphorylated tau. Till now, there is no definite IL-17A alteration in AD patients. Some studies found that the IL-17A levels in the serum, brain and CSF of AD patients were increased, but other studies reported reduced IL-17A levels in AD patients. The conflicting results may be due to the lack of clinical dementia rating [71], but a recent meta-analysis showed a negative correlation between the disease progression of AD and the CSF IL-17A level [72]. Still, studies showed that plasma IL-17 levels could be used as a plasma biomarker to distinguish AD patients from cognitively healthy individuals [73], and CSF IL-17 concentrations could be used to identify frontotemporal lobar degeneration (FTD) with tau pathology [74]. Activated Th17 cells in the CNS could produce pathogenic cytokines IL-17A, recruit neutrophils, heighten the inflammatory cascade, and promote AD neuroinflammation and neurodegeneration [75, 76]. The genetic variations are considered to be an important candidate to induce AD via upregulation of IL-17A [77]. Increasing evidence showed that IL-17 did play a role in the neuronal degeneration of AD; the mechanisms included Aβ interaction, microglia activation, BBB disruption, systemic neuroinflammation, etc. [77].
Interaction with Aβ
The insoluble Aβ peptides could promote the production of reactive oxygen and nitrogen species, resulting in Th17 cells stimulation and IL-17 production [75, 78]. A previous study developed Aβ-reactive Th17 Teff cells, and adoptively transferred them into amyloid precursor protein/presenilin1 (APP/PS1) transgenic AD mice; the result showed that Aβ-specific Th17 Teffs cells play a role as disease perpetrators [79]. In the rat model generated by Aβ injection, IL-17 level was increased in both the circulation and CSF, and was also correlated with the cognitive function decline, indicating that Th17/Tregs balance was disrupted in AD [80]. Similarly, intraperitoneal injection of lipopolysaccharide (LPS) to transgenic mice (Tg2576), which overproduces human Aβ and develops plaques, resulted in the increase of eight cytokines, including IL-17A [81]. In an AD mouse model, Aβ aggregates were shown to mediate the recruitment of neutrophils in the CNS. The effects of IL-17A in AD pathogenesis are highly related to the attraction of neutrophils and the stimulation of neutrophils’ function [82]. Neutrophils were found to be present in areas with Aβ deposits, and this extravasation could lead to amplification of neutrophil entry in the CNS and IL-17 production [3]. In vitro study showed that IL-17A played a role in promoting neuronal autophagy and inducing neurodegeneration [83]. A previous study tested the therapeutic effect of salidroside (SAL), an herb-derived phenylpropanoid glycoside compound, in the senescence-accelerated mouse prone 8 (SAMP8) strain, which is a reliable and stable mouse model of AD strain, a reliable and stable mouse model of AD. The results showed that SAL decreased the IL-17A levels in the peripheral circulation, and alleviated hippocampus-dependent memory impairment [84].
Microglia activation
It was shown that exposure of microglia to IL-17A led to activation and increased production of pro-inflammatory cytokines [65]. In vitro study also showed that TLR-dependent activation of microglia could polarize γδ T cells toward neurotoxic IL-17+ γδT cells [85]. Periodontal bacteria were shown to be able to induce Aβ-42 accumulation and IL-17 expression in the cortex; IL-17 expression in microglia was negatively correlated with the memory test latency and positively correlated with Aβ-42 accumulation [86].
BBB disruption
IL-17A could disrupt BBB integrity by reducing BBB tight junctions (TJ) molecules and disrupting oxidant–antioxidant balance [61, 62]. The endothelial cells of BBB could express IL-17A receptors, and the binding of IL-17A to the receptors could cause the disruption of TJ [63] and downregulate the expression of the TJ molecules [62]. Blocking L-17A could reduce the BBB disruption and reverse the decrease of TJ molecules [64]. Zhang et al. constructed an AD rat model by intrathecal injection of Aβ-42 peptide, and they found that Th17 cells entered into the CNS with the disruption of the BBB, and levels of IL-17 and RORγt were increased in the hippocampus, CSF, and serum [87]. With the disruption of BBB integrity, more neutrophils and Th17 cells will migrate into the brain parenchyma, leading to more IL-17A production and more severe neuronal dysfunction [75, 78].
Systemic neuroinflammation
In a transgenic mouse model of AD, the activation of T and B lymphocytes was increased [88], and these lymphocytes could produce high levels of IL-2, granulocyte macrophage-colony stimulating factor (GM-CSF), tumor necrosis factor-alpha (TNF-α), and IL-17, which pointed to the Th17 polarization [88]. In AD patients, the number of CD4+ and CD8+ T lymphocytes was increased in vascular endothelium and brain parenchyma [89]. The production of Th17-related cytokine IL-21 was increased and the expression of Th17 transcription factor RORγt was upregulated in naive lymphocytes obtained from AD patients [90]. In AD patients, the circulating CD3+CD8−IL-17A+interferon-gamma (IFN-γ)−Th17 cells were found to be increased, indicating that the adaptive immune system is related to neuropathological changes in AD [91]. In an animal model, LPS injection in male Sprague-Dawley (SD) rats increased the IL-17A expression in serum and in the hippocampus [65]. It was reported that inadequate immune surveillance in the gut [92] or respiratory infection [93] could induce higher IL-17A production in the CNS, which would result in Aβ deposition. However, there may be opposite sequences of events, Aβ deposition and inadequate clearance of Aβ would stimulate the receptors of innate immune cells, promote IL-17 production, and induce AD pathogenesis. In a double transgenic APΔE9 mouse with overproduced Aβ, a higher frequency of CD4+ IL-17a and IFN-γ secreting T cells was revealed in the brain, indicating T-cell infiltration may be associated with the neuroinflammatory state in AD [94]. In AD patients, cognitive impairment progression was found to be related to Th17 cells and c-Jun N-terminal kinase (JNK) pathway-associated phosphatase (JKAP), the latter play a key role in regulating inflammation and immune responses; JKAP and Th17 cells were dysregulated and inter-correlated in AD [95]. Some compounds from plants could reduce the associated neuroinflammation in AD. For example, acid alpha-glucosidase (GAA), a kind of lanostane-type triterpenoid isolated from Ganoderma lucidum, was found to have an alleviating neuroinflammatory effect on AD mice via regulating the imbalance of the Th17/Tregs axis [96]. OMT, an alkaloid component extracted from the root of Sophora flavescens Ait, could reduce the level of pro-inflammatory cytokines including IL-6, IL-1β, TNF-α and IL-17A in AD mice [97]. Kavalactones, extracted from the rhizome and roots of kava, could decreased microgliosis, astrogliosis and secretion of the pro-inflammatory cytokines TNF-α and IL-17A, and attenuated the long-term memory decline of APP/Psen1 mice [98].
Strategic therapy targeting on IL-17A
In an AD mouse model, administration of anti-IL-17A antibody to block IL-17A generation could decrease the neuroinflammation induced by Aβ-42 injection, reduced neuronal neurodegeneration, and improve the cognitive impairment of the mice [66]. In male SD rats injected intraperitoneally with LPS, the use of IL-17A-neutralizing antibodies inhibited the expression of APP and Beta-site APP-cleaving enzyme 1 (BACE1), and prevented the expression of TNF-α, IL-6 and inflammatory proteins, indicating the role of anti-IL-17A strategy in the treatment of endotoxemia-induced neuroinflammation and cognitive dysfunction [65]. Anti-IL-17A antibodies could also interfere with neutrophil infiltration into the CNS and inhibit AD progression [99]. It was proposed that a desirable AD vaccine should be effective in inhibiting Th17/IL-17A immune responses to Aβ deposition aiming to limit the neuroinflammation in neurodegeneration [100]. A systemic review reported that none of the current AD drugs is specifically designed to target the dysregulated balance in the Th17/Treg axis, indicating that future therapeutic approaches should specifically consider inhibiting CD4+ Th17 in AD [101]. However, a protective role of IL-17A was also indicated in an animal model of AD, and overexpression of IL-17A intracranially could reduce cerebral amyloid angiopathy, improve glucose metabolism, decrease soluble Aβ levels in the hippocampus and CSF, relieve anxiety, and improve learning deficits [102]. Further, injected ICR mice with IL-17 could improve spatial learning, indicating a complex role of IL-17 in regulating adult neurogenesis [103]. These above-mentioned findings indicate that the role of IL-17A in AD is complicated, it may switch from a protective role to a pathogenic role depending on the disease state.
Th17 cells and IL-17A in PD
PD is the second most common neurodegenerative disease after AD, characterized by the progressive degeneration of dopaminergic (DA) neurons within the substantia nigra pars compacta (SNpc) in the midbrain, the formation of Lewy bodies with aggregated a-synuclein in intracellular inclusions, and the presence of neuroinflammation [104,105,106,107,108,109].
In PD, Th17 cells were assessed by means of surface markers or intracellular IL-17 staining. The former found similar or even reduced Th17 cells in PD patients [110,111,112], while the latter reported increased Th17 cells in PD patients or no differences in Th17 cells between PD patients and healthy subjects [67, 113,114,115,116]. Therefore, the results of different studies concerning the frequency of Th17 between PD patients and controls were contradictory, but the published studies consistently reported an increased frequency of IL-17-producing cells in PD patients [117]. However, some studies reported decreased plasma levels of the IL-17A in PD patients [118, 119].
Interaction with a-synuclein
In a mitochondrial permeability transition pore (MPTP) mouse model of PD, stimulation of Th17 cells with a-synuclein could cause neuronal cell death in the substantia nigra (SN) [119]. Liu et al. used rabies virus glycoprotein (RVG) peptide-modified exosome (EXO) curcumin/phenylboronic acid-poly(2-(dimethylamino)ethyl acrylate) nanoparticle/small interfering RNA targeting SNCA (REXO-C/ANP/S), a nano-scavenger for clearing α-synuclein aggregates in neurons, as a platform for PD treatment, and they found that REXO-C/ANP/S could achieve immune activation clearing by inhibiting Th17 and enhancing Treg to regulate the immune system in mice with PD [120].
Involvement of peripheral immune cells
The involvement of peripheral immune cells [121] was reported in PD patients [122]. A previous study found that global or CD4+ T cell-specific dopamine 2 receptor (DRD2) deficiency could exacerbate MPTP-induced dopaminergic neurodegeneration and CD4+ T-cell depolarization towards pro-inflammatory Th17 phenotypes, indicating that DRD2 expressed on CD4+ T cells is protective against neuroinflammation and developing a therapeutic strategy of stimulating DRD2 may be promising for amelioration of Th17-inflammatory response in PD [123]. In vitro analyses showed about threefold increase in Th17 cells frequency, a phenotype favored by DRD3-signalling, in ex vivo activated CD4+ T cells obtained from PD patients, indicating that DRD3-signalling in lymphocytes plays a relevant role favoring the development of PD, and selective DRD3-antagonism in CD4+ T lymphocytes may exert a therapeutic effect in PD [124]. Vitamin D was reported to inhibit the production of IL-17 and IFN-γ, and promote the differentiation and function of Treg in both rodent and human T cells [125,126,127]. The vitamin D-induced benefits in PD might partly depend on its immune effects of Th17 and Treg cells [117], but more studies are needed to verify the exact contribution of vitamin D in modulating Th17 and Treg in PD.
Neurotoxic effects
In cell models of PD, the co-culture of Th17 cells with MPTP-treated neurons could exacerbate neuronal cell death [68, 128]. Sommer et al. had shown that Th17 cells obtained from PD patients induced neuronal death in the midbrain, indicating the neurotoxic effect of Th17 cells in PD [67], and this neurotoxicity of Th17 cells was driven by T cell-derived IL-17, upregulated IL-17R, downstream Nuclear factor-kappa-B (NFκB) activation, as well as lymphocyte function-associated antigen-1/intercellular adhesion molecule-1(LFA-1/ICAM-1) system [67, 119]. Moreover, the rescue of Th17-mediated neuronal death could be achieved by blocking ICAM-1 and IL-17R, or by blocking LFA-1 and IL-17 in Th17 cells with anti-IL-17 antibodies, directs us toward new potential immunotherapeutic targets for PD [67, 119].
BBB disruption
In PD patients, the disruption of BBB was reported [122], and the increased permeabilization of BBB allowed infiltration of peripheral immune cells into the CNS [129]. In PD animal models, BBB was disrupted and IL-17A level was increased in the SN [68].
Systemic neuroinflammation
Previous studies had found increased circulating Th17 cells in PD patients at the early stages of the disease [84, 104], indicating an important role of Th17-driven inflammation in PD. Furthermore, in Porphyromonas gingivalis (Pg)-treated leucine-rich repeat kinase 2 (LRRK2) R1441G mice, dopaminergic neurons in the SN were reduced, but serum IL-17A, brain IL-17 receptor A, and activated microglial cells were increased; these findings indicated that neuroinflammation might play an important role in the pathophysiology of LRRK2-associated PD [130]. A previous study showed that auricular vagus nerve stimulation (aVNS) treatment decreased Th17 cells, and reduced the levels of inflammatory cytokines, including TNF-α and IL-1β in 6-OHDA treats rats, indicating that aVNS could suppress the evolution of inflammation and modulating innate immune responses to play a neuroprotective role against dopaminergic damage [131]. In PD mice, administration of purified bee venom (BV) phospholipase A2 (bvPLA2) inhibited loss of dopaminergic neurons within the SN in a dose-dependent manner, and this concentration-dependent action appeared to be related to the inhibition Th17 polarization; these results suggest that standardized bvPLA2 may have a neuroprotective effect against PD through neuroinflammation modulation [132]. JKAP, the regulator of immunity and inflammation, was also found to be correlated with Th17 cells and disease severity in PD [133]. Repetitive transcranial magnetic stimulation (rTMS) was proved to have therapeutic effects on neuroinflammation via reducing the production of pro-inflammatory cytokines IFNγ and IL-17A [134].
Microglia activation
Addition of IL-17A to co-cultures of microglia and neurons led to activation of microglia cells and TH+ neuronal cell death. Interestingly, IL-17A exacerbated dopaminergic neuronal loss only in the presence of microglia. Furthermore, the inhibition of the IL-17A receptor on microglia was sufficient to attenuate these effects [68]. A network of communication may exist between glial cells and Th17 cells, a greater understanding of this interaction may provide a novel therapeutic approach [135]. A previous study found that High mobility group protein B1 (HMGB1) A box inhibited the activation of microglia-mediated by HMGB1, inhibited the infiltration of Th17 cells, and decreased the proportion of Th17 in CD4+ T cells, indicating that HMGB1 A box may play a different role in protecting neurons in PD via influencing the activation of microglia cells, the infiltration of Th17 cells, and the differentiation of T cells to Th17 [136].
Alteration of gut microbiota
Altered gut microbiota was described in PD patients, and it also had strong potential to mediate motor deficits and neuroinflammation in PD model [137]. Furthermore, intestinal microbiota has the ability to induce Th17 differentiation [37]. Therefore, the specific Th17 cells and their role in directing against gut microbiota might inspire the development of gut immunomodulatory therapeutic approaches in PD patients [129].
Strategic therapy targeting on IL-17A
In the experimental phase, the anti-Th17 therapeutics in PD can be achieved by using nuclear receptor agonists, including peroxisome proliferator-activated receptor gamma (PPARγ) and liver X receptor (LXR), both of them are known to negatively regulate differentiation of Th17 cells [138, 139]. These agonists may have therapeutic prospects in PD because they effectively inhibit PD pathology [140]. Furthermore, an anti-IL-17A-neutralizing antibody proved to be effective in alleviating the PD manifestations in the PD rat model [68].
Th17 cells and IL-17A in ALS
ALS is a neurodegenerative disorder characterized by progressive degeneration of upper and lower motor neurons (MNs), resulting in muscle weakness and paralysis. The possible involvement of Th17 in ALS is indicated by circumstantial evidence. Studies had shown increased IL-17 levels in serum and CSF of ALS patients, and in the cell model, the IL-17 production was upregulated by cultured peripheral blood mononuclear cells [141, 142]. ALS patients had a higher expression of IL-17A in serum than controls, indicating a greater vulnerability of ALS patients to IL-17A-mediated damage. In ALS patients, the immune profile in peripheral blood was shifted towards a Th1/Th17 cell-mediated pro-inflammatory immune response, and Th1 and Th17 cells were moderate negatively correlated with disease severity, evaluated by forced vital capacity and ALS functional rating scale revised (ALSFRS-R) [143]. The spinal cords of ALS patients were found to be infiltrated by IL-17A-positive CD8 cells and IL-17A-positive mast cells. Mononuclear cells treated with aggregated superoxide dismutase-1 (SOD-1) protein could induce the expression of IL-6, IL-23, and IL-1β, which may be responsible for the induction of IL-17A [144]. IL-17A may be involved in chronic inflammation in ALS, and could be a new therapeutic approach by immune modulation of inflammatory cytokines.
Strategic therapy targeting on IL-17A
A recent study developed a co-culture system of human-induced pluripotent stem cells (hiPSCs)-derived MNs and Th17 cells, derived from ALS patients, MS patients, and healthy controls. They found that Th17 cells from MS patients induced severe degeneration of MNs, and IL-17A yielded a decline of viability and neurite length of MNs in a dose-dependent manner. Furthermore, neutralizing IL-17A and anti-IL-17A receptor treatment reverted this detrimental effect of IL-17A [143].
Conclusions
In 2021, we compared 761 age–gender matched healthy controls with 761 PD patients and found that the ratio of CD4/CD8 in PD patients was higher than that in healthy controls, and the percentage of CD4+ T cells was negatively correlated with the Hoehn and Yahr (H&Y) stage [145]. However, we did not compare the subtypes of CD4+ T cells. Although the function of TH17/IL-17A on AD or PD is still contradictory and the mechanism of TH17/IL-17A is still unclear, the results of the latest research on IL-17A targeted treatments are still valid, so the pathogenesis and targeted therapy of IL-17A in neurodegenerative diseases are still worth exploring.
Availability of data and materials
No.
Abbreviations
- AD:
-
Alzheimer’s disease
- PD:
-
Parkinson’s disease
- ALS:
-
Amyotrophic lateral sclerosis
- CNS:
-
Central nervous system
- TH17:
-
T helper 17
- IL-17A:
-
Interleukin-17A
- TGF-β:
-
Transforming growth factor-β
- ROR:
-
Retinoic orphan receptor
- CTLA:
-
Cytotoxic T-lymphocyte antigen
- TCR:
-
T-cell receptor
- NKT:
-
Natural killer T
- ILC3:
-
Group 3 innate lymphoid cells
- CXCL:
-
C-X-C motif ligand
- G-CSF:
-
Granulocyte colony-stimulating factor
- AS:
-
Ankylosing spondylitis
- RA:
-
Rheumatoid arthritis
- SLE:
-
Systemic lupus erythematosus
- IBD:
-
Inflammatory bowel disease
- MS:
-
Multiple sclerosis
- EAE:
-
Experimental autoimmune encephalomyelitis
- CSF:
-
The cerebral fluid
- BBB:
-
The blood–brain barrier
- Aβ:
-
Amyloid-β
- FTD:
-
Frontotemporal lobar degeneration
- APP/PS1:
-
Amyloid precursor protein/presenilin1
- LPS:
-
Lipopolysaccharide
- Tg:
-
Transgenic
- SAL:
-
Salidroside
- SAMP8:
-
Senescence-accelerated mouse prone 8
- TJ:
-
Tight junctions
- GM-CSF:
-
Granulocyte macrophage-colony stimulating factor
- TNF-α:
-
Tumor necrosis factor-alpha
- IFN-γ:
-
Interferon-gamma
- SD:
-
Sprague-Dawley
- JNK:
-
C-Jun N-terminal kinase
- JKAP:
-
C-Jun N-terminal kinase (JNK) pathway-associated phosphatase
- GAA:
-
Acid alpha-glucosidase
- BACE1:
-
Beta-site APP-cleaving enzyme 1
- DA:
-
Dopaminergic
- SNpc:
-
Substantia nigra pars compacta
- MPTP:
-
Mitochondrial permeability transition pore
- SN:
-
Substantia nigra
- REXO-C/ANP/S:
-
Rabies virus glycoprotein (RVG) peptide-modified exosome (EXO) curcumin/phenylboronic acid-poly(2-(dimethylamino)ethyl acrylate) nanoparticle/small interfering RNA targeting SNCA
- DRD2:
-
Dopamine 2 receptor
- NFκB:
-
Nuclear factor-kappa-B
- LFA-1/ICAM-1:
-
Lymphocyte function-associated antigen-1/intercellular adhesion molecule-1
- Pg:
-
Porphyromonas gingivalis
- LRRK2:
-
Leucine-rich repeat kinase 2
- aVNS:
-
Auricular vagus nerve stimulation
- bvPLA2:
-
Bee venom (BV) phospholipase A2
- rTMS:
-
Repetitive transcranial magnetic stimulation
- HMGB1:
-
High mobility group protein B1
- PPARγ:
-
Peroxisome proliferator-activated receptor gamma
- LXR:
-
Liver X receptor
- MNs:
-
Motor neurons
- ALSFRS-R:
-
Amyotrophic lateral sclerosis functional rating scale revised
- SOD-1:
-
Superoxide dismutase-1
- hiPSCs:
-
Human-induced pluripotent stem cells
- H&Y:
-
The Hoehn and Yahr
References
Hammond TR, Marsh SE, Stevens B. Immune signaling in neurodegeneration. Immunity. 2019;50(4):955–74. https://doi.org/10.1016/j.immuni.2019.03.016.
Ransohoff RM. How neuroinflammation contributes to neurodegeneration. Science. 2016;353(6301):777–83. https://doi.org/10.1126/science.aag2590.
Chen J, Liu X, Zhong Y. Interleukin-17A: the key cytokine in neurodegenerative diseases. Front Aging Neurosci. 2020;12:566922. https://doi.org/10.3389/fnagi.2020.566922 (Published 2020 Sep 29).
Harrington LE, Hatton RD, Mangan PR, et al. Interleukin 17-producing CD4+ effector T cells develop via a lineage distinct from the T helper type 1 and 2 lineages. Nat Immunol. 2005;6(11):1123–32. https://doi.org/10.1038/ni1254.
Park H, Li Z, Yang XO, et al. A distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17. Nat Immunol. 2005;6(11):1133–41. https://doi.org/10.1038/ni1261.
Lee JY, Hall JA, Kroehling L, et al. Serum Amyloid A proteins induce pathogenic Th17 cells and promote inflammatory disease [published correction appears in Cell. 2020;183(7):2036–9]. Cell. 2020;180(1):79-91.e16. https://doi.org/10.1016/j.cell.2019.11.026.
Bettelli E, Carrier Y, Gao W, et al. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441(7090):235–8. https://doi.org/10.1038/nature04753.
Mangan PR, Harrington LE, O’Quinn DB, et al. Transforming growth factor-beta induces development of the T(H)17 lineage. Nature. 2006;441(7090):231–4. https://doi.org/10.1038/nature04754.
Veldhoen M, Hocking RJ, Atkins CJ, Locksley RM, Stockinger B. TGFbeta in the context of an inflammatory cytokine milieu supports de novo differentiation of IL-17-producing T cells. Immunity. 2006;24(2):179–89. https://doi.org/10.1016/j.immuni.2006.01.001.
Zhou L, Ivanov II, Spolski R, et al. IL-6 programs T(H)-17 cell differentiation by promoting sequential engagement of the IL-21 and IL-23 pathways. Nat Immunol. 2007;8(9):967–74. https://doi.org/10.1038/ni1488.
Chung Y, Chang SH, Martinez GJ, et al. Critical regulation of early Th17 cell differentiation by interleukin-1 signaling. Immunity. 2009;30(4):576–87. https://doi.org/10.1016/j.immuni.2009.02.007.
Hirota K, Duarte JH, Veldhoen M, et al. Fate mapping of IL-17-producing T cells in inflammatory responses. Nat Immunol. 2011;12(3):255–63. https://doi.org/10.1038/ni.1993.
Komuczki J, Tuzlak S, Friebel E, et al. Fate-mapping of GM-CSF expression identifies a discrete subset of inflammation-driving T helper cells regulated by cytokines IL-23 and IL-1β. Immunity. 2019;50(5):1289-1304.e6. https://doi.org/10.1016/j.immuni.2019.04.006.
McGeachy MJ, Chen Y, Tato CM, et al. The interleukin 23 receptor is essential for the terminal differentiation of interleukin 17-producing effector T helper cells in vivo. Nat Immunol. 2009;10(3):314–24. https://doi.org/10.1038/ni.1698.
Ivanov II, McKenzie BS, Zhou L, et al. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell. 2006;126(6):1121–33. https://doi.org/10.1016/j.cell.2006.07.035.
Yang XO, Pappu BP, Nurieva R, et al. T helper 17 lineage differentiation is programmed by orphan nuclear receptors ROR alpha and ROR gamma. Immunity. 2008;28(1):29–39. https://doi.org/10.1016/j.immuni.2007.11.016.
Zhong Z, Wen Z, Darnell JE Jr. Stat3: a STAT family member activated by tyrosine phosphorylation in response to epidermal growth factor and interleukin-6. Science. 1994;264(5155):95–8. https://doi.org/10.1126/science.8140422.
Takeda K, Kaisho T, Yoshida N, Takeda J, Kishimoto T, Akira S. Stat3 activation is responsible for IL-6-dependent T cell proliferation through preventing apoptosis: generation and characterization of T cell-specific Stat3-deficient mice [published correction appears in J Immunol. 2015;194(7):3526]. J Immunol. 1998;161(9):4652–60.
Yang XO, Panopoulos AD, Nurieva R, et al. STAT3 regulates cytokine-mediated generation of inflammatory helper T cells. J Biol Chem. 2007;282(13):9358–63. https://doi.org/10.1074/jbc.C600321200.
Laurence A, Tato CM, Davidson TS, et al. Interleukin-2 signaling via STAT5 constrains T helper 17 cell generation. Immunity. 2007;26(3):371–81. https://doi.org/10.1016/j.immuni.2007.02.009.
Ghoreschi K, Laurence A, Yang XP, et al. Generation of pathogenic T(H)17 cells in the absence of TGF-β signalling. Nature. 2010;467(7318):967–71. https://doi.org/10.1038/nature09447.
Volpe E, Servant N, Zollinger R, et al. A critical function for transforming growth factor-beta, interleukin 23 and proinflammatory cytokines in driving and modulating human T(H)-17 responses. Nat Immunol. 2008;9(6):650–7. https://doi.org/10.1038/ni.1613.
McGeachy MJ, Cua DJ, Gaffen SL. The IL-17 family of cytokines in health and disease. Immunity. 2019;50(4):892–906. https://doi.org/10.1016/j.immuni.2019.03.021.
Rouvier E, Luciani MF, Mattéi MG, Denizot F, Golstein P. CTLA-8, cloned from an activated T cell, bearing AU-rich messenger RNA instability sequences, and homologous to a herpesvirus saimiri gene. J Immunol. 1993;150(12):5445–56.
Gaffen SL. Life before seventeen: cloning of the IL-17 receptor. J Immunol. 2011;187(9):4389–91. https://doi.org/10.4049/jimmunol.1102576.
Cua DJ, Tato CM. Innate IL-17-producing cells: the sentinels of the immune system [published correction appears in Nat Rev Immunol. 2010;10(8):611] [published correction appears in Nat Rev Immunol. 2010;10(7):following 489]. Nat Rev Immunol. 2010;10(7):479–89. https://doi.org/10.1038/nri2800.
Jin W, Dong C. IL-17 cytokines in immunity and inflammation. Emerg Microbes Infect. 2013;2(9):e60. https://doi.org/10.1038/emi.2013.58.
Reynolds JM, Angkasekwinai P, Dong C. IL-17 family member cytokines: regulation and function in innate immunity. Cytokine Growth Factor Rev. 2010;21(6):413–23. https://doi.org/10.1016/j.cytogfr.2010.10.002.
Hatfield JK, Brown MA. Group 3 innate lymphoid cells accumulate and exhibit disease-induced activation in the meninges in EAE. Cell Immunol. 2015;297(2):69–79. https://doi.org/10.1016/j.cellimm.2015.06.006.
Cosmi L, Maggi L, Santarlasci V, Liotta F, Annunziato F. T helper cells plasticity in inflammation. Cytometry A. 2014;85(1):36–42. https://doi.org/10.1002/cyto.a.22348.
Cosmi L, Santarlasci V, Maggi L, Liotta F, Annunziato F. Th17 plasticity: pathophysiology and treatment of chronic inflammatory disorders. Curr Opin Pharmacol. 2014;17:12–6. https://doi.org/10.1016/j.coph.2014.06.004.
Onishi RM, Gaffen SL. Interleukin-17 and its target genes: mechanisms of interleukin-17 function in disease. Immunology. 2010;129(3):311–21. https://doi.org/10.1111/j.1365-2567.2009.03240.x.
Gaffen SL, Jain R, Garg AV, Cua DJ. The IL-23-IL-17 immune axis: from mechanisms to therapeutic testing. Nat Rev Immunol. 2014;14(9):585–600. https://doi.org/10.1038/nri3707.
Conti HR, Gaffen SL. IL-17-mediated immunity to the opportunistic fungal pathogen Candida albicans. J Immunol. 2015;195(3):780–8. https://doi.org/10.4049/jimmunol.1500909.
Drummond RA, Lionakis MS. Organ-specific mechanisms linking innate and adaptive antifungal immunity. Semin Cell Dev Biol. 2019;89:78–90. https://doi.org/10.1016/j.semcdb.2018.01.008.
Naik S, Bouladoux N, Linehan JL, et al. Commensal-dendritic-cell interaction specifies a unique protective skin immune signature. Nature. 2015;520(7545):104–8. https://doi.org/10.1038/nature14052.
Ivanov II, Atarashi K, Manel N, et al. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell. 2009;139(3):485–98. https://doi.org/10.1016/j.cell.2009.09.033.
Kumar P, Monin L, Castillo P, et al. Intestinal interleukin-17 receptor signaling mediates reciprocal control of the gut microbiota and autoimmune inflammation. Immunity. 2016;44(3):659–71. https://doi.org/10.1016/j.immuni.2016.02.007.
Phuna ZX, Madhavan P. A closer look at the mycobiome in Alzheimer’s disease: fungal species, pathogenesis and transmission. Eur J Neurosci. 2022;55(5):1291–321. https://doi.org/10.1111/ejn.15599.
Maddur MS, Miossec P, Kaveri SV, Bayry J. Th17 cells: biology, pathogenesis of autoimmune and inflammatory diseases, and therapeutic strategies. Am J Pathol. 2012;181(1):8–18. https://doi.org/10.1016/j.ajpath.2012.03.044.
Chiricozzi A, Krueger JG. IL-17 targeted therapies for psoriasis. Expert Opin Investig Drugs. 2013;22(8):993–1005. https://doi.org/10.1517/13543784.2013.806483.
Baeten D, Sieper J, Braun J, et al. Secukinumab, an interleukin-17A Inhibitor, in ankylosing spondylitis. N Engl J Med. 2015;373(26):2534–48. https://doi.org/10.1056/NEJMoa1505066.
Shen H, Goodall JC, Hill Gaston JS. Frequency and phenotype of peripheral blood Th17 cells in ankylosing spondylitis and rheumatoid arthritis. Arthritis Rheum. 2009;60(6):1647–56. https://doi.org/10.1002/art.24568.
Pavelka K, Chon Y, Newmark R, Lin SL, Baumgartner S, Erondu N. A study to evaluate the safety, tolerability, and efficacy of brodalumab in subjects with rheumatoid arthritis and an inadequate response to methotrexate. J Rheumatol. 2015;42(6):912–9. https://doi.org/10.3899/jrheum.141271.
Yang J, Chu Y, Yang X, et al. Th17 and natural Treg cell population dynamics in systemic lupus erythematosus. Arthritis Rheum. 2009;60(5):1472–83. https://doi.org/10.1002/art.24499.
Zenewicz LA, Antov A, Flavell RA. CD4 T-cell differentiation and inflammatory bowel disease. Trends Mol Med. 2009;15(5):199–207. https://doi.org/10.1016/j.molmed.2009.03.002.
Manel N, Unutmaz D, Littman DR. The differentiation of human T(H)-17 cells requires transforming growth factor-beta and induction of the nuclear receptor RORgammat. Nat Immunol. 2008;9(6):641–9. https://doi.org/10.1038/ni.1610.
Lock C, Hermans G, Pedotti R, et al. Gene-microarray analysis of multiple sclerosis lesions yields new targets validated in autoimmune encephalomyelitis. Nat Med. 2002;8(5):500–8. https://doi.org/10.1038/nm0502-500.
Schofield C, Fischer SK, Townsend MJ, et al. Characterization of IL-17AA and IL-17FF in rheumatoid arthritis and multiple sclerosis. Bioanalysis. 2016;8(22):2317–27. https://doi.org/10.4155/bio-2016-0207.
Hedegaard CJ, Krakauer M, Bendtzen K, Lund H, Sellebjerg F, Nielsen CH. T helper cell type 1 (Th1), Th2 and Th17 responses to myelin basic protein and disease activity in multiple sclerosis [published correction appears in Immunology. 2008;125(3):438]. Immunology. 2008;125(2):161–9. https://doi.org/10.1111/j.1365-2567.2008.02837.x.
Brucklacher-Waldert V, Stuerner K, Kolster M, Wolthausen J, Tolosa E. Phenotypical and functional characterization of T helper 17 cells in multiple sclerosis. Brain. 2009;132(Pt 12):3329–41. https://doi.org/10.1093/brain/awp289.
Durelli L, Conti L, Clerico M, et al. T-helper 17 cells expand in multiple sclerosis and are inhibited by interferon-beta. Ann Neurol. 2009;65(5):499–509. https://doi.org/10.1002/ana.21652.
Setiadi AF, Abbas AR, Jeet S, et al. IL-17A is associated with the breakdown of the blood-brain barrier in relapsing-remitting multiple sclerosis. J Neuroimmunol. 2019;332:147–54. https://doi.org/10.1016/j.jneuroim.2019.04.011.
Waisman A, Hauptmann J, Regen T. The role of IL-17 in CNS diseases. Acta Neuropathol. 2015;129(5):625–37. https://doi.org/10.1007/s00401-015-1402-7.
Huppert J, Closhen D, Croxford A, et al. Cellular mechanisms of IL-17-induced blood-brain barrier disruption. FASEB J. 2010;24(4):1023–34. https://doi.org/10.1096/fj.09-141978.
Kebir H, Kreymborg K, Ifergan I, et al. Human TH17 lymphocytes promote blood-brain barrier disruption and central nervous system inflammation. Nat Med. 2007;13(10):1173–5. https://doi.org/10.1038/nm1651.
Tahmasebinia F, Pourgholaminejad A. The role of Th17 cells in auto-inflammatory neurological disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2017;79(Pt B):408–16. https://doi.org/10.1016/j.pnpbp.2017.07.023.
Prajeeth CK, Kronisch J, Khorooshi R, et al. Effectors of Th1 and Th17 cells act on astrocytes and augment their neuroinflammatory properties. J Neuroinflamm. 2017;14(1):204. https://doi.org/10.1186/s12974-017-0978-3 (Published 2017 Oct 16).
Murphy AC, Lalor SJ, Lynch MA, Mills KH. Infiltration of Th1 and Th17 cells and activation of microglia in the CNS during the course of experimental autoimmune encephalomyelitis. Brain Behav Immun. 2010;24(4):641–51. https://doi.org/10.1016/j.bbi.2010.01.014.
Langrish CL, Chen Y, Blumenschein WM, et al. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J Exp Med. 2005;201(2):233–40. https://doi.org/10.1084/jem.20041257.
Tzartos JS, Friese MA, Craner MJ, et al. Interleukin-17 production in central nervous system-infiltrating T cells and glial cells is associated with active disease in multiple sclerosis. Am J Pathol. 2008;172(1):146–55. https://doi.org/10.2353/ajpath.2008.070690.
Segal BM. Th17 cells in autoimmune demyelinating disease. Semin Immunopathol. 2010;32(1):71–7. https://doi.org/10.1007/s00281-009-0186-z.
Komiyama Y, Nakae S, Matsuki T, et al. IL-17 plays an important role in the development of experimental autoimmune encephalomyelitis. J Immunol. 2006;177(1):566–73. https://doi.org/10.4049/jimmunol.177.1.566.
Havrdová E, Belova A, Goloborodko A, et al. Activity of secukinumab, an anti-IL-17A antibody, on brain lesions in RRMS: results from a randomized, proof-of-concept study. J Neurol. 2016;263(7):1287–95. https://doi.org/10.1007/s00415-016-8128-x.
Sun J, Zhang S, Zhang X, Zhang X, Dong H, Qian Y. IL-17A is implicated in lipopolysaccharide-induced neuroinflammation and cognitive impairment in aged rats via microglial activation. J Neuroinflamm. 2015;12:165. https://doi.org/10.1186/s12974-015-0394-5 (Published 2015 Sep 15).
Cristiano C, Volpicelli F, Lippiello P, et al. Neutralization of IL-17 rescues amyloid-β-induced neuroinflammation and memory impairment. Br J Pharmacol. 2019;176(18):3544–57. https://doi.org/10.1111/bph.14586.
Sommer A, Marxreiter F, Krach F, et al. Th17 lymphocytes induce neuronal cell death in a human iPSC-based model of Parkinson’s disease [published correction appears in Cell Stem Cell. 2019 Jun 6;24(6):1006]. Cell Stem Cell. 2018;23(1):123-131.e6. https://doi.org/10.1016/j.stem.2018.06.015.
Liu Z, Qiu AW, Huang Y, et al. IL-17A exacerbates neuroinflammation and neurodegeneration by activating microglia in rodent models of Parkinson’s disease. Brain Behav Immun. 2019;81:630–45. https://doi.org/10.1016/j.bbi.2019.07.026.
Liu Z, Huang Y, Cao BB, Qiu YH, Peng YP. Th17 cells induce dopaminergic neuronal death via LFA-1/ICAM-1 interaction in a mouse model of parkinson’s disease. Mol Neurobiol. 2017;54(10):7762–76. https://doi.org/10.1007/s12035-016-0249-9.
Jin M, Akgün K, Ziemssen T, Kipp M, Günther R, Hermann A. Interleukin-17 and Th17 lymphocytes directly impair motoneuron survival of wildtype and FUS-ALS mutant human iPSCs. Int J Mol Sci. 2021;22(15):8042. https://doi.org/10.3390/ijms22158042 (Published 2021 Jul 27).
Yan XZ, Lai L, Ao Q, Tian XH, Zhang YH. Interleukin-17A in Alzheimer’s disease: recent advances and controversies. Curr Neuropharmacol. 2022;20(2):372–83. https://doi.org/10.2174/1570159X19666210823110004.
Taipa R, das Neves SP, Sousa AL, et al. Proinflammatory and anti-inflammatory cytokines in the CSF of patients with Alzheimer’s disease and their correlation with cognitive decline. Neurobiol Aging. 2019;76:125–32. https://doi.org/10.1016/j.neurobiolaging.2018.12.019.
Doecke JD, Laws SM, Faux NG, et al. Blood-based protein biomarkers for diagnosis of Alzheimer disease. Arch Neurol. 2012;69(10):1318–25. https://doi.org/10.1001/archneurol.2012.1282.
Hu WT, Chen-Plotkin A, Grossman M, et al. Novel CSF biomarkers for frontotemporal lobar degenerations. Neurology. 2010;75(23):2079–86. https://doi.org/10.1212/WNL.0b013e318200d78d.
Zenaro E, Pietronigro E, Della Bianca V, et al. Neutrophils promote Alzheimer’s disease-like pathology and cognitive decline via LFA-1 integrin. Nat Med. 2015;21(8):880–6. https://doi.org/10.1038/nm.3913.
Browne TC, McQuillan K, McManus RM, O’Reilly JA, Mills KH, Lynch MA. IFN-γ Production by amyloid β-specific Th1 cells promotes microglial activation and increases plaque burden in a mouse model of Alzheimer’s disease. J Immunol. 2013;190(5):2241–51. https://doi.org/10.4049/jimmunol.1200947.
Mohammadi Shahrokhi V, Ravari A, Mirzaei T, Zare-Bidaki M, Asadikaram G, Arababadi MK. IL-17A and IL-23: plausible risk factors to induce age-associated inflammation in Alzheimer’s disease. Immunol Invest. 2018;47(8):812–22. https://doi.org/10.1080/08820139.2018.1504300.
Yin Y, Wen S, Li G, Wang D. Hypoxia enhances stimulating effect of amyloid beta peptide (25–35) for interleukin 17 and T helper lymphocyte subtype 17 upregulation in cultured peripheral blood mononuclear cells. Microbiol Immunol. 2009;53(5):281–6. https://doi.org/10.1111/j.1348-0421.2009.00120.x.
Machhi J, Yeapuri P, Lu Y, et al. CD4+ effector T cells accelerate Alzheimer’s disease in mice. J Neuroinflamm. 2021;18(1):272. https://doi.org/10.1186/s12974-021-02308-7 (Published 2021 Nov 19).
Sun L, Ju T, Wang T, et al. Decreased Netrin-1 and correlated Th17/Tregs balance disorder in Aβ1–42 induced alzheimer’s disease model rats. Front Aging Neurosci. 2019;11:124. https://doi.org/10.3389/fnagi.2019.00124 (Published 2021 Nov 19).
Knopp RC, Baumann KK, Wilson ML, Banks WA, Erickson MA. Amyloid Beta pathology exacerbates weight loss and brain cytokine responses following low-dose lipopolysaccharide in aged female Tg2576 mice. Int J Mol Sci. 2022;23(4):2377. https://doi.org/10.3390/ijms23042377 (Published 2022 Feb 21).
Milovanovic J, Arsenijevic A, Stojanovic B, et al. Interleukin-17 in chronic inflammatory neurological diseases. Front Immunol. 2020;11:947. https://doi.org/10.3389/fimmu.2020.00947 (Published 2020 Jun 3).
Wang X, Zhang M, Liu H. LncRNA17A regulates autophagy and apoptosis of SH-SY5Y cell line as an in vitro model for Alzheimer’s disease. Biosci Biotechnol Biochem. 2019;83(4):609–21. https://doi.org/10.1080/09168451.2018.1562874.
Xie Z, Lu H, Yang S, et al. Salidroside attenuates cognitive dysfunction in senescence-accelerated mouse prone 8 (SAMP8) mice and modulates inflammation of the gut-brain axis. Front Pharmacol. 2020;11:568423. https://doi.org/10.3389/fphar.2020.568423 (Published 2020 Dec 9).
Derkow K, Krüger C, Dembny P, Lehnardt S. Microglia induce neurotoxic IL-17+ γδ T cells dependent on TLR2, TLR4, and TLR9 activation. PLoS ONE. 2015;10(8):e0135898. https://doi.org/10.1371/journal.pone.0135898 (Published 2015 Aug 19).
Gu Y, Wu Z, Zeng F, et al. Systemic exposure to lipopolysaccharide from porphyromonas gingivalis induces bone loss-correlated Alzheimer’s disease-like pathologies in middle-aged mice. J Alzheimers Dis. 2020;78(1):61–74. https://doi.org/10.3233/JAD-200689.
Zhang J, Ke KF, Liu Z, Qiu YH, Peng YP. Th17 cell-mediated neuroinflammation is involved in neurodegeneration of ab1-42-induced Alzheimer’s disease model rats. PLoS ONE. 2013;8:e75786. https://doi.org/10.1371/journal.pone.0075786.
St-Amour I, Bosoi CR, Paré I, et al. Peripheral adaptive immunity of the triple transgenic mouse model of Alzheimer’s disease. J Neuroinflamm. 2019;16(1):3. https://doi.org/10.1186/s12974-018-1380-5 (Published 2019 Jan 5).
Lemprière S. T cells on patrol in Alzheimer disease. Nat Rev Neurol. 2020;16(3):128–9. https://doi.org/10.1038/s41582-020-0317-7.
Saresella M, Calabrese E, Marventano I, et al. Increased activity of Th-17 and Th-9 lymphocytes and a skewing of the post-thymic differentiation pathway are seen in Alzheimer’s disease. Brain Behav Immun. 2011;25(3):539–47. https://doi.org/10.1016/j.bbi.2010.12.004.
Oberstein TJ, Taha L, Spitzer P, et al. Imbalance of circulating Th17 and regulatory T cells in Alzheimer’s disease: a case control study. Front Immunol. 2018;9:1213. https://doi.org/10.3389/fimmu.2018.01213 (Published 2018 Jun 4).
Saksida T, Koprivica I, Vujičić M, et al. Impaired IL-17 production in gut-residing immune cells of 5xFAD mice with Alzheimer’s Disease pathology. J Alzheimers Dis. 2018;61(2):619–30. https://doi.org/10.3233/JAD-170538.
McManus RM, Higgins SC, Mills KH, Lynch MA. Respiratory infection promotes T cell infiltration and amyloid-β deposition in APP/PS1 mice. Neurobiol Aging. 2014;35(1):109–21. https://doi.org/10.1016/j.neurobiolaging.2013.07.025.
Ahuja M, Buabeid M, Abdel-Rahman E, et al. Immunological alteration & toxic molecular inductions leading to cognitive impairment & neurotoxicity in transgenic mouse model of Alzheimer’s disease. Life Sci. 2017;177:49–59. https://doi.org/10.1016/j.lfs.2017.03.004.
Zeng J, Liu J, Qu Q, Zhao X, Zhang J. JKAP, Th1 cells, and Th17 cells are dysregulated and inter-correlated, among them JKAP and Th17 cells relate to cognitive impairment progression in Alzheimer’s disease patients [published online ahead of print, 2021 Sep 30]. Ir J Med Sci. 2021. https://doi.org/10.1007/s11845-021-02749-2.
Zhang Y, Wang X, Yang X, Yang X, Xue J, Yang Y. Ganoderic acid A to alleviate neuroinflammation of Alzheimer’s disease in mice by regulating the imbalance of the Th17/Tregs axis. J Agric Food Chem. 2021;69(47):14204–14. https://doi.org/10.1021/acs.jafc.1c06304.
Chen Y, Qi Z, Qiao B, Lv Z, Hao Y, Li H. Oxymatrine can attenuate pathological deficits of Alzheimer’s disease mice through regulation of neuroinflammation. J Neuroimmunol. 2019;334:576978. https://doi.org/10.1016/j.jneuroim.2019.576978.
Fragoulis A, Siegl S, Fendt M, et al. Oral administration of methysticin improves cognitive deficits in a mouse model of Alzheimer’s disease. Redox Biol. 2017;12:843–53. https://doi.org/10.1016/j.redox.2017.04.024.
Katayama H. Anti-interleukin-17A and anti-interleukin-23 antibodies may be effective against Alzheimer’s disease: role of neutrophils in the pathogenesis. Brain Behav. 2020;10(1):e01504. https://doi.org/10.1002/brb3.1504.
Marciani DJ. Alzheimer’s disease vaccine development: a new strategy focusing on immune modulation. J Neuroimmunol. 2015;287:54–63. https://doi.org/10.1016/j.jneuroim.2015.08.008.
Kubick N, Flournoy PCH, Enciu AM, Manda G, Mickael ME. Drugs modulating CD4+ T cells blood-brain barrier interaction in Alzheimer’s disease. Pharmaceutics. 2020;12(9):880. https://doi.org/10.3390/pharmaceutics12090880.
Yang J, Kou J, Lalonde R, Fukuchi KI. Intracranial IL-17A overexpression decreases cerebral amyloid angiopathy by upregulation of ABCA1 in an animal model of Alzheimer’s disease. Brain Behav Immun. 2017;65:262–73. https://doi.org/10.1016/j.bbi.2017.05.012.
Tfilin M, Turgeman G. Interleukine-17 administration modulates adult hippocampal neurogenesis and improves spatial learning in mice. J Mol Neurosci. 2019;69(2):254–63. https://doi.org/10.1007/s12031-019-01354-4.
Eriksen JL, Wszolek Z, Petrucelli L. Molecular pathogenesis of Parkinson disease. Arch Neurol. 2005;62(3):353–7. https://doi.org/10.1001/archneur.62.3.353.
Schapira AH, Jenner P. Etiology and pathogenesis of Parkinson’s disease. Mov Disord. 2011;26(6):1049–55. https://doi.org/10.1002/mds.23732.
Kalia LV, Lang AE. Parkinson’s disease. Lancet. 2015;386(9996):896–912. https://doi.org/10.1016/S0140-6736(14)61393-3.
Dehay B, Bourdenx M, Gorry P, et al. Targeting α-synuclein for treatment of Parkinson’s disease: mechanistic and therapeutic considerations. Lancet Neurol. 2015;14(8):855–66. https://doi.org/10.1016/S1474-4422(15)00006-X.
More SV, Kumar H, Kim IS, Song SY, Choi DK. Cellular and molecular mediators of neuroinflammation in the pathogenesis of Parkinson’s disease. Mediators Inflamm. 2013;2013:952375. https://doi.org/10.1155/2013/952375.
McGeer PL, McGeer EG. Inflammation and neurodegeneration in Parkinson’s disease. Parkinsonism Relat Disord. 2004;10(Suppl 1):S3–7. https://doi.org/10.1016/j.parkreldis.2004.01.005.
Kustrimovic N, Comi C, Magistrelli L, et al. Parkinson’s disease patients have a complex phenotypic and functional Th1 bias: cross-sectional studies of CD4+ Th1/Th2/T17 and Treg in drug-naïve and drug-treated patients. J Neuroinflamm. 2018;15(1):205. https://doi.org/10.1186/s12974-018-1248-8 (Published 2018 Jul 12).
Niwa F, Kuriyama N, Nakagawa M, Imanishi J. Effects of peripheral lymphocyte subpopulations and the clinical correlation with Parkinson’s disease. Geriatr Gerontol Int. 2012;12(1):102–7. https://doi.org/10.1111/j.1447-0594.2011.00740.x.
Cook DA, Kannarkat GT, Cintron AF, et al. LRRK2 levels in immune cells are increased in Parkinson’s disease. NPJ Parkinsons Dis. 2017;3:11. https://doi.org/10.1038/s41531-017-0010-8 (Published 2017 Mar 28).
Chen Y, Qi B, Xu W, et al. Clinical correlation of peripheral CD4+-cell sub-sets, their imbalance and Parkinson’s disease. Mol Med Rep. 2015;12(4):6105–11. https://doi.org/10.3892/mmr.2015.4136.
Yang F, Li B, Li L, Zhang H. The clinical significance of the imbalance of Th17 and Treg cells and their related cytokines in peripheral blood of Parkinson’s disease patients. Int J Clin Exp Med. 2016;9:17946–51.
Cen L, Yang C, Huang S, et al. Peripheral lymphocyte subsets as a marker of Parkinson’s disease in a Chinese population. Neurosci Bull. 2017;33(5):493–500. https://doi.org/10.1007/s12264-017-0163-9.
Yang L, Guo C, Zhu J, et al. Increased levels of pro-inflammatory and anti-inflammatory cellular responses in Parkinson’s disease patients: search for a disease indicator. Med Sci Monit. 2017;23:2972–8. https://doi.org/10.12659/msm.904240 (Published 2017 Jun 18).
Storelli E, Cassina N, Rasini E, Marino F, Cosentino M. Do Th17 lymphocytes and IL-17 contribute to Parkinson’s disease? A systematic review of available evidence. Front Neurol. 2019;10:13. https://doi.org/10.3389/fneur.2019.00013 (Published 2019 Jan 24).
Rocha NP, Assis F, Scalzo PL, et al. Reduced activated T lymphocytes (CD4+CD25+) and plasma levels of cytokines in Parkinson’s disease. Mol Neurobiol. 2018;55(2):1488–97. https://doi.org/10.1007/s12035-017-0404-y.
Álvarez-Luquín DD, Arce-Sillas A, Leyva-Hernández J, et al. Regulatory impairment in untreated Parkinson’s disease is not restricted to Tregs: other regulatory populations are also involved. J Neuroinflamm. 2019;16(1):212. https://doi.org/10.1186/s12974-019-1606-1 (Published 2019 Nov 11).
Liu L, Li Y, Peng H, et al. Targeted exosome coating gene-chem nanocomplex as “nanoscavenger” for clearing α-synuclein and immune activation of Parkinson’s disease. Sci Adv. 2020;6(50):eaba3967. https://doi.org/10.1126/sciadv.aba3967 (Published 2020 Dec 11).
Hirsch EC, Vyas S, Hunot S. Neuroinflammation in Parkinson’s disease. Parkinsonism Relat Disord. 2012;18(Suppl 1):S210–2. https://doi.org/10.1016/S1353-8020(11)70065-7.
Kortekaas R, Leenders KL, van Oostrom JC, et al. Blood-brain barrier dysfunction in parkinsonian midbrain in vivo. Ann Neurol. 2005;57(2):176–9. https://doi.org/10.1002/ana.20369.
Liu Z, Zhai XR, Du ZS, et al. Dopamine receptor D2 on CD4+ T cells is protective against neuroinflammation and neurodegeneration in a mouse model of Parkinson’s disease. Brain Behav Immun. 2021;98:110–21. https://doi.org/10.1016/j.bbi.2021.08.220.
Elgueta D, Contreras F, Prado C, et al. Dopamine receptor D3 expression is altered in CD4+ T cells from Parkinson’s disease patients and its pharmacologic inhibition attenuates the motor impairment in a mouse model. Front Immunol. 2019;10:981. https://doi.org/10.3389/fimmu.2019.00981 (Published 2019 May 1).
Hewison M. An update on vitamin D and human immunity. Clin Endocrinol (Oxf). 2012;76(3):315–25. https://doi.org/10.1111/j.1365-2265.2011.04261.x.
Ooi JH, Chen J, Cantorna MT. Vitamin D regulation of immune function in the gut: why do T cells have vitamin D receptors? Mol Aspects Med. 2012;33(1):77–82. https://doi.org/10.1016/j.mam.2011.10.014.
Cantorna MT, Snyder L, Lin YD, Yang L. Vitamin D and 1,25(OH)2D regulation of T cells. Nutrients. 2015;7(4):3011–21. https://doi.org/10.3390/nu7043011 (Published 2015 Apr 22).
Reynolds AD, Stone DK, Hutter JA, Benner EJ, Mosley RL, Gendelman HE. Regulatory T cells attenuate Th17 cell-mediated nigrostriatal dopaminergic neurodegeneration in a model of Parkinson’s disease. J Immunol. 2010;184(5):2261–71. https://doi.org/10.4049/jimmunol.0901852.
Prots I, Winner B. Th17 cells: a promising therapeutic target for Parkinson’s disease? Expert Opin Ther Targets. 2019;23(4):309–14. https://doi.org/10.1080/14728222.2019.1590336.
Feng YK, Wu QL, Peng YW, et al. Oral P gingivalis impairs gut permeability and mediates immune responses associated with neurodegeneration in LRRK2 R1441G mice. J Neuroinflamm. 2020;17(1):347. https://doi.org/10.1186/s12974-020-02027-5 (Published 2020 Nov 19).
Jiang Y, Cao Z, Ma H, et al. Auricular vagus nerve stimulation exerts antiinflammatory effects and immune regulatory function in a 6-OHDA model of Parkinson’s disease. Neurochem Res. 2018;43(11):2155–64. https://doi.org/10.1007/s11064-018-2639-z.
Kim KH, Lee SY, Shin J, Hwang JT, Jeon HN, Bae H. Dose-dependent neuroprotective effect of standardized bee venom phospholipase A2 against MPTP-induced Parkinson’s disease in mice. Front Aging Neurosci. 2019;11:80. https://doi.org/10.3389/fnagi.2019.00080 (Published 2019 Apr 5).
Yang Q, Zhuang J, Cai P, Li L, Wang R, Chen Z. JKAP relates to disease risk, severity, and Th1 and Th17 differentiation in Parkinson’s disease. Ann Clin Transl Neurol. 2021;8(9):1786–95. https://doi.org/10.1002/acn3.51420.
Aftanas LI, Gevorgyan MM, Zhanaeva SY, et al. Therapeutic effects of repetitive transcranial magnetic stimulation (rTMS) on neuroinflammation and neuroplasticity in patients with Parkinson’s disease: a placebo-controlled study. Bull Exp Biol Med. 2018;165(2):195–9. https://doi.org/10.1007/s10517-018-4128-4.
MacMahon Copas AN, McComish SF, Fletcher JM, Caldwell MA. The pathogenesis of Parkinson’s disease: a complex interplay between astrocytes, microglia, and T lymphocytes? Front Neurol. 2021;12:666737. https://doi.org/10.3389/fneur.2021.666737 (Published 2021 May 26).
Tian Y, Cao Y, Chen R, et al. HMGB1 A box protects neurons by potently inhibiting both microglia and T cell-mediated inflammation in a mouse Parkinson’s disease model. Clin Sci (Lond). 2020;134(15):2075–90. https://doi.org/10.1042/CS20200553.
Sampson TR, Debelius JW, Thron T, et al. Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson’s disease. Cell. 2016;167(6):1469-1480.e12. https://doi.org/10.1016/j.cell.2016.11.018.
Cui G, Qin X, Wu L, et al. Liver X receptor (LXR) mediates negative regulation of mouse and human Th17 differentiation. J Clin Invest. 2011;121(2):658–70. https://doi.org/10.1172/JCI42974.
Klotz L, Burgdorf S, Dani I, et al. The nuclear receptor PPAR gamma selectively inhibits Th17 differentiation in a T cell-intrinsic fashion and suppresses CNS autoimmunity [published correction appears in J Exp Med. 2009 Dec 21;206(13):3159. Novak, Natalija [corrected to Nowak, Nina]]. J Exp Med. 2009;206(10):2079–89. https://doi.org/10.1084/jem.20082771.
Carta AR. PPAR-γ: therapeutic prospects in Parkinson’s disease. Curr Drug Targets. 2013;14(7):743–51. https://doi.org/10.2174/1389450111314070004.
Rentzos M, Rombos A, Nikolaou C, et al. Interleukin-17 and interleukin-23 are elevated in serum and cerebrospinal fluid of patients with ALS: a reflection of Th17 cells activation? Acta Neurol Scand. 2010;122(6):425–9. https://doi.org/10.1111/j.1600-0404.2010.01333.x.
Saresella M, Piancone F, Tortorella P, et al. T helper-17 activation dominates the immunologic milieu of both amyotrophic lateral sclerosis and progressive multiple sclerosis. Clin Immunol. 2013;148(1):79–88. https://doi.org/10.1016/j.clim.2013.04.010.
Jin M, Günther R, Akgün K, Hermann A, Ziemssen T. Peripheral proinflammatory Th1/Th17 immune cell shift is linked to disease severity in amyotrophic lateral sclerosis. Sci Rep. 2020;10(1):5941. https://doi.org/10.1038/s41598-020-62756-8 (Published 2020 Apr 3).
Fiala M, Chattopadhay M, La Cava A, et al. IL-17A is increased in the serum and in spinal cord CD8 and mast cells of ALS patients. J Neuroinflamm. 2010;7:76. https://doi.org/10.1186/1742-2094-7-76 (Published 2010 Nov 9).
Chen X, Feng W, Ou R, et al. Evidence for peripheral immune activation in Parkinson’s disease. Front Aging Neurosci. 2021;13:617370. https://doi.org/10.3389/fnagi.2021.617370 (Published 2021 Apr 30).
Acknowledgements
Thank the authors of the references.
Funding
This study was supported by grant from National key Research and development program of China (Grant No. 2017YFC09007703), grant from science and technology planning project in Sichuan Province (Grant No. 2020YJ0281), grant from 1·3·5 project for disciplines of excellence West China Hospital Sichuan University (Grant No. ZYJC18038), and the grant from cadres health care project in Sichuan Province (Grant No. 2019-112).
Author information
Authors and Affiliations
Contributions
All authors participated in drafting the article or revising it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors agreed to be published.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fu, J., Huang, Y., Bao, T. et al. The role of Th17 cells/IL-17A in AD, PD, ALS and the strategic therapy targeting on IL-17A. J Neuroinflammation 19, 98 (2022). https://doi.org/10.1186/s12974-022-02446-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-022-02446-6